Published online Nov 27, 2012. doi: 10.4240/wjgs.v4.i11.256
Revised: September 20, 2012
Accepted: November 17, 2012
Published online: November 27, 2012
AIM: To investigate the efficacy of the anal fistula plug (AFP) compared to the mucosa advancement flap (MAF), considered the best procedure for patients with a complex anal fistula.
METHODS: The literature search included PubMed, EMBASE, Cochrane Library and OVID original studies on the topic of AFP compared to MAF for complex fistula-in-ano that had a deadline for publication by April 2011. Randomized controlled trials, controlled clinical trials and prospective cohort studies were included in the review. After information collection, a meta-analysis was performed using data on overall success rates as well as incidence of incontinence and morbidity. The quality of postoperative life was also included with the clinical results.
RESULTS: Six studies involving 408 patients (AFP = 167, MAF = 241) were included in the meta-analysis. The differences in the overall success rates and incidence of fistula recurrence were not statistically significant between the AFP and MAF [risk difference (RD) = -0.12, 95%CI: -0.39 - 0.14; RD = 0.13; 95%CI: -0.18 - 0.43, respectively]. However, for the AFP, the risk of postoperative impaired continence was lower (RD = -0.08, 95%CI: -0.15 - -0.02) as was the incidence of other complications (RD = -0.06, 95%CI: -0.11 - -0.00). The postoperative quality of life, for patients treated using the AFP was superior to that of the MAF patients. Patients treated with the AFP had less persistent pain of a shorter duration and the healing time of the fistula and hospital stay were also reduced.
CONCLUSION: The AFP is an effective procedure for patients with a complex anal fistula; it has the same success rate but a lower risk of complications than the MAF and may also be associated with an improved postoperative quality of life. Additional evidence is needed to confirm these findings.
- Citation: Leng Q, Jin HY. Anal fistula plug vs mucosa advancement flap in complex fistula-in-ano: A meta-analysis. World J Gastrointest Surg 2012; 4(11): 256-261
- URL: https://www.wjgnet.com/1948-9366/full/v4/i11/256.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i11.256
Fistula-in-ano is a common condition. It has an incidence of 5.6 per 100 000 in women and 12.3 per 100 000 in men[1]. This disorder is reported to occur predominantly during the third and fourth decades of life[2]; most cases are of cryptoglandular origin[3]. Parks et al[4] developed a classification system in which the fistulas are divided into the following: Intersphincteric fistula, transsphincteric fistula, suprasphincteric fistula and extrasphincteric fistula. Intersphincteric fistulas and low transsphincteric fistulas (which account for less than one third of the external sphincter complex) are easy to treat by fistulotomy and have a high success rate. Treatment of high tanssphincteric fistulas continues to be a challenge.
Conventional surgery includes the fistulotomy, with loose and cutting setons. All of such techniques have disappointing success rates and a high risk of incontinence. Therefore, some sphincter preservation procedures have been developed. The mucosa advancement flap (MAF), recently considered the best available treatment option for complex fistulas, results in a success rate of about 60%[5,6]. This procedure is technically demanding and may affect continence[7]. Use of fibrin glue is an alternative to the MAF; however, the long-term closure rates are low[8-12].
Johnson et al[13] first described the anal fistula plug (AFP) in 2006; the plug is made of lyophilized porcine intestinal submucosa. Since then, several studies on the AFP have been reported with variable results. A systematic review, based on observational studies, reported that the AFP has a moderate success rate of 35%-87% for complex fistula-in-ano[14]. In the present report, we performed a meta-analysis comparing the AFP and the MAF with the objective of evaluating the efficacy of the AFP for the treatment of patients with a complex fistula-in-ano.
A fistula was considered “complex” when the fistula was high [suprasphicteric, extrasphincteric or high-trans-sphincteric (track crosses > 30%-50% of external sphincter)], was anterior in a female, had multiple tracts, or the patient had pre-existing incontinence, a history of local irradiation, or Crohn’s disease. Fistulas with multiple tracts were defined as a fistula with a single primary and multiple secondary openings.
Plug extrusion was present when there was partial or complete displacement of the plug during the postoperative period. The outcome studied was treatment success, which was defined as clinical healing of the fistula in the anal tract. For the patients with multiple tracts, the procedure was considered successful only if all of the tracts were closed.
A search was performed using: PubMed, EMBASE, Cochrane Library and OVID with a deadline publication date of April 2011. The keywords used for the search were: anal fistula, perianal fistula, fistula in anal, AFP, fistula plug, MAF and advancement flap. In addition to computer browsing, review and original papers were also scanned in the reference section to identify additional data. No language restrictions were applied.
All randomized controlled trials (RCTs), controlled clinical trials and prospective cohort studies that compared the efficacy of AFP to MAF in patients with a complex anal fistula were included. Studies without enough data and animal trials were excluded.
Data on the type of trial, total number of patients treated, follow-up period, overall success rates with the AFP and MAF, recurrent disease, sepsis/abscess formation in the postoperative period, plug extrusion rate, total number of patients with incontinence and postoperative quality of life were extracted by two independent reviewers from the studies included. Discrepancies were resolved by discussion between reviewers.
The primary outcome measured was the success rates of the two procedures for the treatment of the anal fistula. The secondary outcome measured was the plug extrusion rate, abscess formation/sepsis rate, incontinence rate and quality of life after the operation.
Statistical analysis was carried out using Review Manager (version 5.1) provided by The Cochrane Collaboration. Dichotomous data are presented as the risk difference (RD) and continuous outcomes as the weighted mean difference, both with 95%CI. The overall effect was tested using Z scores and significance was set at P < 0.05. The meta-analysis was performed using fixed-effect or random-effect methods, depending on the absence or presence of significant heterogeneity[15]. Statistical heterogeneity between trials was evaluated by the χ2 and I2 tests and significance was set at P < 0.10. In the absence of statistically significant heterogeneity, the fixed-effect method was used to combine the results. When heterogeneity was confirmed (P≤ 0.10), the random-effect method was used. No sensitivity analysis was performed.
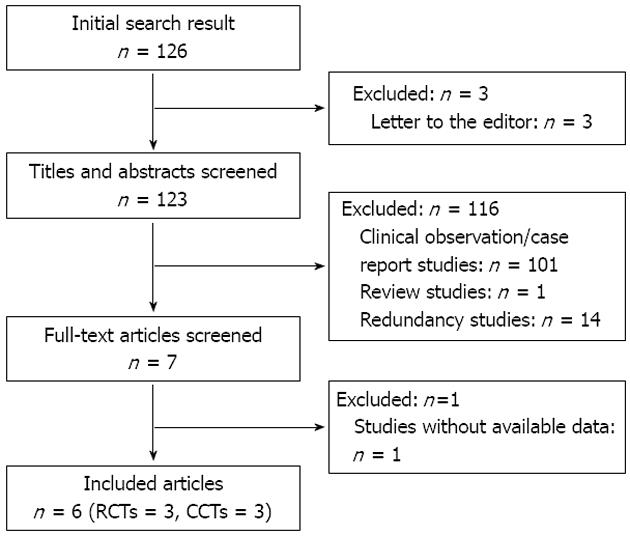
The searches identified a total of 126 studies. Three “Letters to the Editor” were excluded from the analysis. By scanning titles and abstracts, 116 redundant publications, reviews and case reports were excluded. After reviewing full texts, one study without available data was removed from consideration. A total of six studies that involved 408 patients were included in the meta-analysis (Figure 1).
The characteristics of the six included studies are shown in Table 1. Three of the trials were randomized using computer randomization[16-18]. Two of the RCTs[16,17] described the method of allocation concealment and blinding. During the follow-up, one study[18] had one patient lost (one patient in the AFP group), and the other studies[16,17] had no patient lost to follow-up. One study[16] described the method used for data recording and analysis. Two of the trials[19,20] were retrospective studies, and one of the trials[21] compared the healing and complication rates of a prospective cohort of AFP patients to a retrospective cohort of patients that underwent the endo-anal advancement flap procedure.
| Ref. | Study design | Patients (n) | Follow-up | Success rates n (%) | |||
| AFP | MAF | AFP | MAF | AFP | MAF | ||
| Christoforidis et al[19] | Retrospective | 37 | 43 | 14M | 56M | 12/37 (32.4) | 27/43 (62.8) |
| Ortiz et al[18] | RCT | 15 | 16 | 1Y | 1Y | 3/15 (20.0) | 14/16 (87.5) |
| Chung et al[20] | Retrospective | 27 | 96 | 24W | 12W | 19/27 (70.4) | 58/96 (60.4) |
| Adamina et al[21] | Cohort study | 12 | 12 | 28.1W | 14.1W | 6/12 (50.0) | 4/12 (33.3) |
| A ba-bai-ke-re et al[16] | RCT | 45 | 45 | 5.7M | 6.1M | 37/45 (82.2) | 29/45 (64.4) |
| Van Koperen et al[17] | RCT | 31 | 29 | 11M | 11M | 9/31 (29.0) | 14/29 (48.3) |
All the trials excluded patients with recto-vaginal fistulas, recto-urethral fistulas, sepsis, patients that were human immunodeficiency virus positive, and those with fistulas related to Crohn’s disease, ulcerative colitis, tuberculosis, prior surgery and malignancies. Patients with severe cardiovascular disease, diabetes or a pregnancy were also excluded.
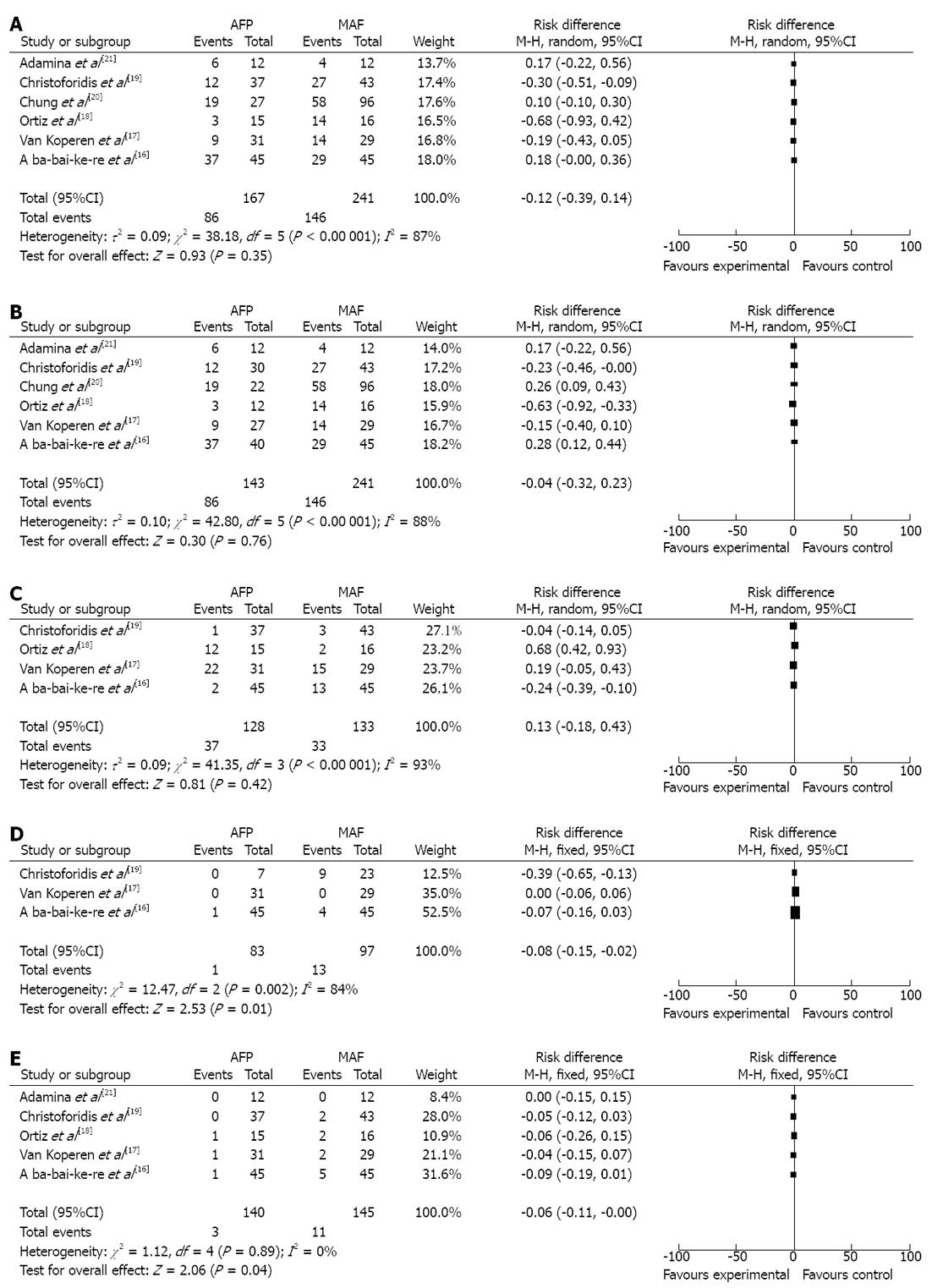
Assessment of overall success rate: The healing rates at the end of follow-up for the AFP in patients with complex anal fistulas are shown in Table 1. For the six studies[16-21], statistically significant heterogeneity was detected (τ2 = 0.09, χ2 = 38.18, df = 5, P < 0.00001, I2 = 87%), using the random-effect method for the meta-analysis. The combined result indicated no statistically significant difference in the overall healing rate between the AFP and MAF procedures (RD = -0.12, 95%CI: -0.39 - 0.14) (Figure 2A).
Plug extrusion was a common finding during the early postoperative period. In the studiesincluded, plug extrusion ranged from 11.1% to 18.9%. Including these patients for analysis could decrease the success rate of the AFP. After excluding those patients that had the plug extruded, a modified analysis was performed and no statistically significant difference was found (RD = -0.004, 95%CI: -0.32 - 0.23) (Figure 2B).
Comparison of fistula recurrence: Four studies[16-19] reported on the fistula recurrence rates during the follow-up. The RD for the AFP compared to the MAF in patients with complex fistulas was 0.13 (95%CI: -0.18 - 0.43). Statistical heterogeneity of the trials was found (τ2 = 0.09, χ2 = 41.35, df = 3, P < 0.00001, I2 = 93%), allowing the use of the random-effect method for the meta-analysis. The result revealed that there was no significant difference in rate of fistula recurrence between the AFP and the MAF (RD = 0.13, 95%CI: -0.18 - 0.43) (Figure 2C).
Comparisons of postoperative complications: Three studies[16,17,19] reported on postoperative incontinence rates. One study[16] used the Wexner score and Vaizey scale[22] to evaluate continence, at the same time, another study[17] used colorectal functional outcomes[23]. Yet another study[19] assessed continence using the Cleveland Clinic Florida-Fecal Incontinence score. According to the results of the heterogeneity analysis (χ2 = 0.29, df = 1, P = 0.66, I2 = 0%), the random-effect method was used. The findings indicated that the rate of postoperative incontinence was lower with the AFP than the MAF procedure (RD = -0.08, 95%CI: -0.15 - -0.02) (Figure 2D).
Five studies[16-19,21] reported other complications including abscess formation and bleeding. According to the results of the heterogeneity analysis (χ2 = 0.47, df = 3, P = 0.93, I2 = 0%), the fixed-effect method was used. The results indicated that other complications were fewer with the AFP compared to the MAF procedure (RD = -0.06, 95%CI: -0.11 - 0.00) (Figure 2E).
Quality of postoperative life: The Life quality scale system[24] was used in one study[16]. The score for the postoperative quality of life was higher in the AFP group (85.9 ± 5.3 vs 65.3 ± 8.9, P = 0.000). Postoperative pain was less (visual analogue scale score 3 ± 3 vs 4 ± 2.5, P = 0.14) on day one[17] and persisted for a shorter period of time (1.5 ± 0.5 d vs 7.5 ± 1.8 d, P = 0.0000)[16]. In addition, the fistula tract healing time was reduced (7.5 ± 3.5 d vs 24.5 ± 5.5 d, P = 0.0000)[16] and the hospital stay was shortened (1 d vs 2.5 d, P = 0.002)[21].
The main objective of surgery for an anal fistula is to eradicate the fistula tract while maintaining anal continence[25]. A simple laying open procedure is effective for low or simple fistulas[26]. However, treatment of complex anal fistulas is challenging because internal and external sphincters are involved in the fistulous track and fecal continence could be impaired after surgery[27,28]. Seton placement has been the standard approach to complex anal fistulas and has been recommended to reduce postoperative incontinence[29-31]. However, continence impairment is variable ranging from 0% to 70%[29,32-35]. Recently, more attention has been focused on sphincter-preserving approaches for complex fistulas where conventional surgery may result in a high incontinence rate. The MAF is considered to be the best available treatment for complex fistulas; however, it is a demanding technique and may affect continence. Using the AFP, with biological material, to close the fistula tracts seems to cause less damage and may have better outcomes.
According to the results of the present meta-analysis, the difference in the overall healing rate between the AFP and the MAF in patients with a complex anal fistula was not statistically significant (RD = -0.12, 95%CI: -0.39 - 0.14). At the end of the follow-up, the recurrence rate for the AFP group was from 2.7% to 80.0%, and was from 7.0% to 51.7% in the MAF group, the difference was not statistically significant (P = 0.42). Although it is routine to secure the AFP, at the internal opening, with absorbable sutures, plug extrusion, which ranges from 4% to 41%, is a common occurrence. In the studies included, the plug extrusion rate was from 11.1% to 18.9%. If the plug-extruded cases are excluded, the patient cure rate range increases to 25.0% to 92.5%. However, the success rates of the two treatments still showed no statistically significant difference (RD = -0.004, 95%CI: -0.32 - 0.23).
Impairment of continence is the main complication after surgical treatment of anal fistulas. The MAF is associated with a higher morbidity and significant risk of worsening incontinence (0%-52%)[36-39]. The AFP is associated with less damage. After flushing the fistula tract with hydrogen peroxide, the AFP is inserted through the tract with the wide end of the plug wedged firmly in the internal opening of the fistula tract. This procedure, with less potential damage to the sphincter muscle, is likely to have a better outcome. The data from the studies included shows that both morbidity (RD = -0.06, 95%CI: -0.11 - -0.00) and incontinence (RD = -0.08, 95%CI: -0.15 - -0.02) were lower in the AFP group.
Avalos-González et al[40] reported that a fibrin sealant could reduce the closure time of stable enterocutaneous fistulas. The AFP, which is made of lyophilized porcine intestinal submucosa, has the same effect on an anal fistula. With the AFP, the healing time of an anal fistula tract was reduced from 24.5 ± 5.5 d to 7.5 ± 3.5 d. The AFP could also improve the quality of life, postoperatively. Both the postoperative pain score and the persistence of pain were lower in the AFP group. After treatment with the AFP, the hospital stay was shortened and patients could return to work earlier.
In summary, this meta-analysis clearly supports the AFP as an effective treatment for patients with complex anal fistulas. The success rate was the same and the complications were lower compared to the MAF. In addition, the AFP may be associated with a better postoperative quality of life. However, these results are based on a few small controlled studies with limited follow-up. Additional data is needed to confirm these findings.
Fistula-in-ano is a common condition. It has an incidence of 5.6 per 100 000 in women and 12.3 per 100 000 in men. This disorder is reported to occur predominantly during the third and fourth decades of life; most cases are of cryptoglandular origin. Treatment of high tanssphincteric fistulas continues to be a challenge.
This study aims to investigate the efficacy of the anal fistula plug (AFP) compared to the mucosa advancement flap (MAF), considered the best procedure for patients with a complex anal fistula.
A search was performed using: PubMed, EMBASE, Cochrane Library and OVID with a deadline publication date by April 2011. The keywords used for the search were: anal fistula, perianal fistula, fistula in anal, AFP, fistula plug, MAF and advancement flap. In addition to computer browsing, review and original papers were also scanned in the reference section to identify additional data. No language restrictions were applied.
The authors found that the AFP is an effective procedure for patients with a complex anal fistula; it has the same success rate but a lower risk of complications than the MAF and may also be associated with an improved postoperative quality of life. Additional evidence is needed to confirm these findings.
This is a well conducted meta-analysis of AFP vs mucosal advancement flap for complex anal fistula.
Peer reviewers: Francis Seow-Choen, Colorectal Surgery, Professor, Medical Director, Fortis Colorectal Hospital, 290 Orchard Road Paragon No. 06-06, Singapore 238859, Singapore; Giulio Aniello Santoro, Professor, I Department of Surgery, Regional Hospital, Via Isola di Mezzo, n.16, 31100 Treviso, Italy
S- Editor Wen LL L- Editor Hughes D E- Editor Zheng XM
| 1. | Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73:219-224. [PubMed] |
| 2. | Marks CG, Ritchie JK. Anal fistulas at St Mark's Hospital. Br J Surg. 1977;64:84-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 90] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Seow-Choen F, Nicholls RJ. Anal fistula. Br J Surg. 1992;79:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 82] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1072] [Cited by in RCA: 928] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 5. | Ortíz H, Marzo J. Endorectal flap advancement repair and fistulectomy for high trans-sphincteric and suprasphincteric fistulas. Br J Surg. 2000;87:1680-1683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 103] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | van der Hagen SJ, Baeten CG, Soeters PB, van Gemert WG. Long-term outcome following mucosal advancement flap for high perianal fistulas and fistulotomy for low perianal fistulas: recurrent perianal fistulas: failure of treatment or recurrent patient disease? Int J Colorectal Dis. 2006;21:784-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Schouten WR, Zimmerman DD, Briel JW. Transanal advancement flap repair of transsphincteric fistulas. Dis Colon Rectum. 1999;42:1419-122; discussion 1419-122;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 157] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Buchanan GN, Bartram CI, Phillips RK, Gould SW, Halligan S, Rockall TA, Sibbons P, Cohen RG. Efficacy of fibrin sealant in the management of complex anal fistula: a prospective trial. Dis Colon Rectum. 2003;46:1167-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 160] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | Ellis CN, Clark S. Fibrin glue as an adjunct to flap repair of anal fistulas: a randomized, controlled study. Dis Colon Rectum. 2006;49:1736-1740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Sentovich SM. Fibrin glue for anal fistulas: long-term results. Dis Colon Rectum. 2003;46:498-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 132] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Williams JG, Farrands PA, Williams AB, Taylor BA, Lunniss PJ, Sagar PM, Varma JS, George BD. The treatment of anal fistula: ACPGBI position statement. Colorectal Dis. 2007;9 Suppl 4:18-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 12. | Gisbertz SS, Sosef MN, Festen S, Gerhards MF. Treatment of fistulas in ano with fibrin glue. Dig Surg. 2005;22:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Johnson EK, Gaw JU, Armstrong DN. Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas. Dis Colon Rectum. 2006;49:371-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 210] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 14. | Garg P, Song J, Bhatia A, Kalia H, Menon GR. The efficacy of anal fistula plug in fistula-in-ano: a systematic review. Colorectal Dis. 2010;12:965-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 15. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 25804] [Article Influence: 1121.9] [Reference Citation Analysis (0)] |
| 16. | A ba-bai-ke-re MM, Wen H, Huang HG, Chu H, Lu M, Chang ZS, Ai EH, Fan K. Randomized controlled trial of minimally invasive surgery using acellular dermal matrix for complex anorectal fistula. World J Gastroenterol. 2010;16:3279-3286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | van Koperen PJ, Bemelman WA, Gerhards MF, Janssen LW, van Tets WF, van Dalsen AD, Slors JF. The anal fistula plug treatment compared with the mucosal advancement flap for cryptoglandular high transsphincteric perianal fistula: a double-blinded multicenter randomized trial. Dis Colon Rectum. 2011;54:387-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Ortiz H, Marzo J, Ciga MA, Oteiza F, Armendáriz P, de Miguel M. Randomized clinical trial of anal fistula plug versus endorectal advancement flap for the treatment of high cryptoglandular fistula in ano. Br J Surg. 2009;96:608-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 19. | Christoforidis D, Pieh MC, Madoff RD, Mellgren AF. Treatment of transsphincteric anal fistulas by endorectal advancement flap or collagen fistula plug: a comparative study. Dis Colon Rectum. 2009;52:18-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 74] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Chung W, Kazemi P, Ko D, Sun C, Brown CJ, Raval M, Phang T. Anal fistula plug and fibrin glue versus conventional treatment in repair of complex anal fistulas. Am J Surg. 2009;197:604-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Adamina M, Hoch JS, Burnstein MJ. To plug or not to plug: a cost-effectiveness analysis for complex anal fistula. Surgery. 2010;147:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 963] [Cited by in RCA: 973] [Article Influence: 37.4] [Reference Citation Analysis (1)] |
| 23. | Bakx R, Sprangers MA, Oort FJ, van Tets WF, Bemelman WA, Slors JF, van Lanschot JJ. Development and validation of a colorectal functional outcome questionnaire. Int J Colorectal Dis. 2005;20:126-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 24. | Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC. Fecal Incontinence Quality of Life Scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum. 2000;43:9-16; discussion 16-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 929] [Cited by in RCA: 842] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 25. | Joy HA, Williams JG. The outcome of surgery for complex anal fistula. Colorectal Dis. 2002;4:254-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Shouler PJ, Grimley RP, Keighley MR, Alexander-Williams J. Fistula-in-ano is usually simple to manage surgically. Int J Colorectal Dis. 1986;1:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 59] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Pescatori M, Maria G, Anastasio G, Rinallo L. Anal manometry improves the outcome of surgery for fistula-in-ano. Dis Colon Rectum. 1989;32:588-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Lunniss PJ, Kamm MA, Phillips RK. Factors affecting continence after surgery for anal fistula. Br J Surg. 1994;81:1382-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 118] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Williams JG, MacLeod CA, Rothenberger DA, Goldberg SM. Seton treatment of high anal fistulae. Br J Surg. 1991;78:1159-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 143] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | Cirocco WC, Rusin LC. Simplified Seton management for complex anal fistulas: a novel use for the rubber band ligator. Dis Colon Rectum. 1991;34:1135-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Walfisch S, Menachem Y, Koretz M. Double seton--a new modified approach to high transsphincteric anal fistula. Dis Colon Rectum. 1997;40:731-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | García-Aguilar J, Belmonte C, Wong DW, Goldberg SM, Madoff RD. Cutting seton versus two-stage seton fistulotomy in the surgical management of high anal fistula. Br J Surg. 1998;85:243-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 115] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 33. | Gurer A, Ozlem N, Gokakin AK, Ozdogan M, Kulacoglu H, Aydin R. A novel material in seton treatment of fistula-in-ano. Am J Surg. 2007;193:794-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Hamel CT, Marti WR, Oertli D. Simplified placement and management of cutting setons in the treatment of transsphincteric anal fistula: technical note. Int J Colorectal Dis. 2004;19:354-36; discussion 354-36;. [PubMed] |
| 35. | Theerapol A, So BY, Ngoi SS. Routine use of setons for the treatment of anal fistulae. Singapore Med J. 2002;43:305-307. [PubMed] |
| 36. | Mizrahi N, Wexner SD, Zmora O, Da Silva G, Efron J, Weiss EG, Vernava AM, Nogueras JJ. Endorectal advancement flap: are there predictors of failure? Dis Colon Rectum. 2002;45:1616-1621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 203] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 37. | Zimmerman DD, Briel JW, Gosselink MP, Schouten WR. Anocutaneous advancement flap repair of transsphincteric fistulas. Dis Colon Rectum. 2001;44:1474-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 71] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Wedell J, Meier zu Eissen P, Banzhaf G, Kleine L. Sliding flap advancement for the treatment of high level fistulae. Br J Surg. 1987;74:390-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 66] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 39. | Wang D, Yamana T, Iwadare J. Long-term results and quality-of-life outcomes in patients with transsphincteric fistulas after muscle-filling procedure. Dis Colon Rectum. 2002;45:1011-1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Avalos-González J, Portilla-deBuen E, Leal-Cortés CA, Orozco-Mosqueda A, Estrada-Aguilar Mdel C, Velázquez-Ramírez GA, Ambriz-González G, Fuentes-Orozco C, Guzmán-Gurrola AE, González-Ojeda A. Reduction of the closure time of postoperative enterocutaneous fistulas with fibrin sealant. World J Gastroenterol. 2010;16:2793-2800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |