Published online Sep 27, 2011. doi: 10.4240/wjgs.v3.i9.138
Revised: July 26, 2011
Accepted: August 5, 2011
Published online: September 27, 2011
Blunt isolated pancreatic trauma is uncommon, accounting for 1%-4% of high impact abdominal injuries. In addition, its diagnosis can be difficult; physical signs may be poor and laboratory findings nonspecific, resulting in delayed treatment. Preserving the spleen during distal pancreatectomy (DP) is controversial. One of the spleen’s functions regards immunity; complications following splenectomy include leukocytosis, thrombocytosis, overwhelming post splenectomy sepsis and some degree of immunodeficiency. This is why many authors favor its preservation. We describe a case of a young man with an isolated pancreatic trauma due to a blunt abdominal trauma with a delayed presentation who was treated with spleen-preserving DP and we discuss the value of this procedure with reference to the literature.
- Citation: Fonseca AZ, Jr MAFR, Contrucci O, Pompeo A, Orsetti A, Neto HA. Spleen preserving distal pancreatectomy in an isolated blunt pancreatic trauma. World J Gastrointest Surg 2011; 3(9): 138-141
- URL: https://www.wjgnet.com/1948-9366/full/v3/i9/138.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i9.138
Blunt isolated pancreatic trauma is uncommon[1], accounting for 1%-4% of high impact blunt abdominal injuries[2]. In addition, its diagnosis can be difficult; physical signs may be poor and laboratory findings nonspecific[1], resulting in delayed treatment[3]. In many instances, the injury only becomes apparent after the development of complications[4]. Due to this, the management of these kinds of injuries is not easy and few surgeons and institutes have the necessary experience[1].
Several treatment modalities have been described, from non-surgical to open drainage and even duodenopancreatectomy[3], depending on the grade of the lesion. Major duct injury is the most important factor related to the outcome in these patients[3]. When present (incidence near to 1.3%), pancreaticojejunostomy and distal pancreatectomy (DP), with or without splenectomy, can be performed, the latter being preferred[3].
Preserving the spleen during DP is controversial. Some authors found no significant difference with or without splenectomy[5]; the majority believe that the maintenance of the organ brings more benefits to the patient, as shown in their reports[6-12]. One of the spleen’s functions is immunity; complications following splenectomy include leukocytosis, thrombocytosis, overwhelming post splenectomy sepsis and some degree of immunodeficiency[9]. These are the most common arguments made by authors favoring spleen preservation.
The spleen can be preserved in two different ways while performing a DP. Firstly, the splenic vessels are maintained, assuring adequate blood supply to the organ. Secondly, these vessels are ligated, preserving the short gastric vessels for perfusion. In the latter technique, macroscopic inspection of the spleen has been shown to be efficient and reliable[7,11].
We describe the case of a young man with an isolated pancreatic trauma due to a blunt abdominal trauma with a delayed presentation who was treated with spleen-preserving DP and we discuss the value of this procedure with reference to the literature.
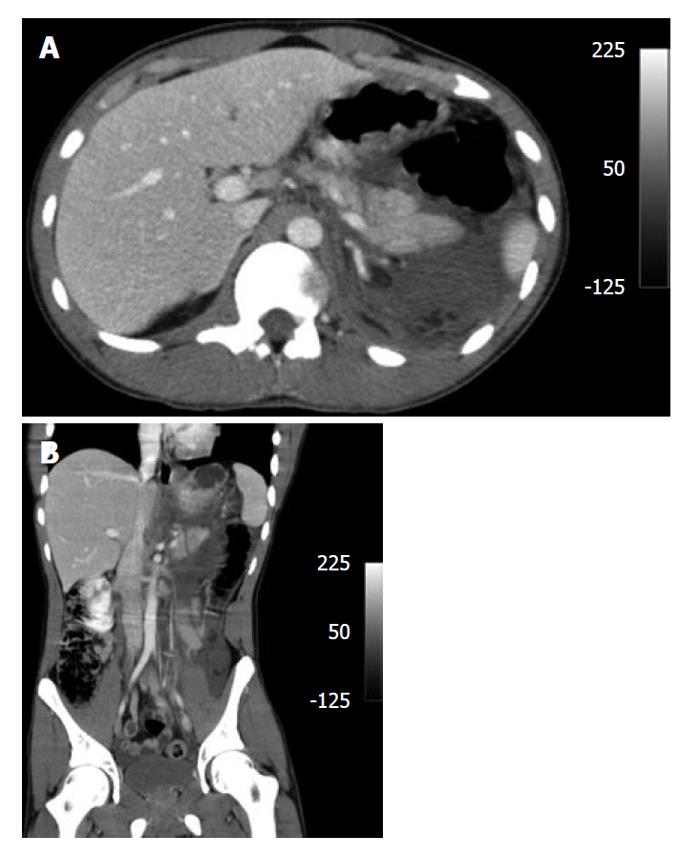
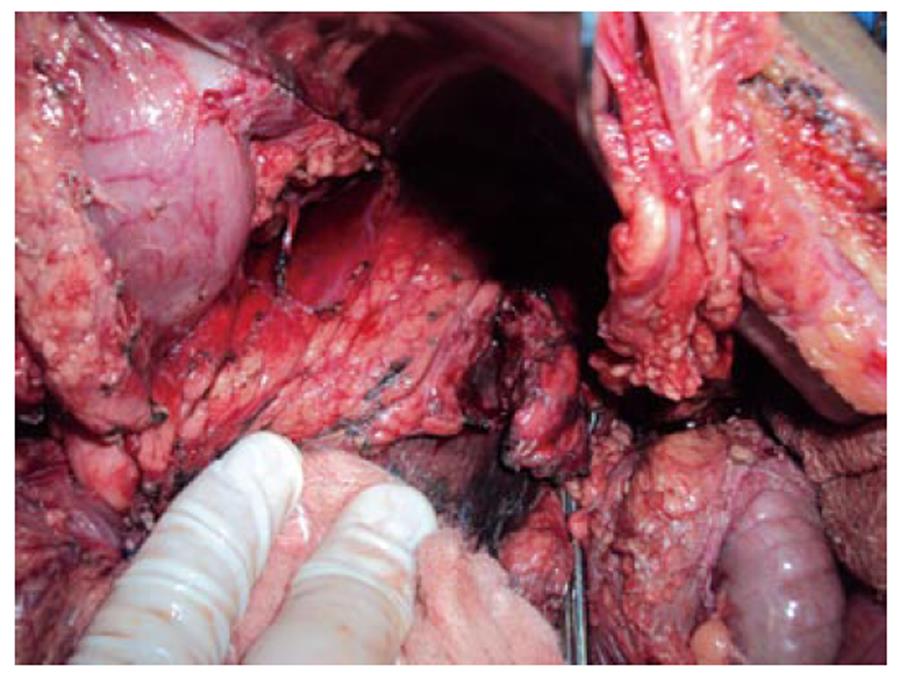
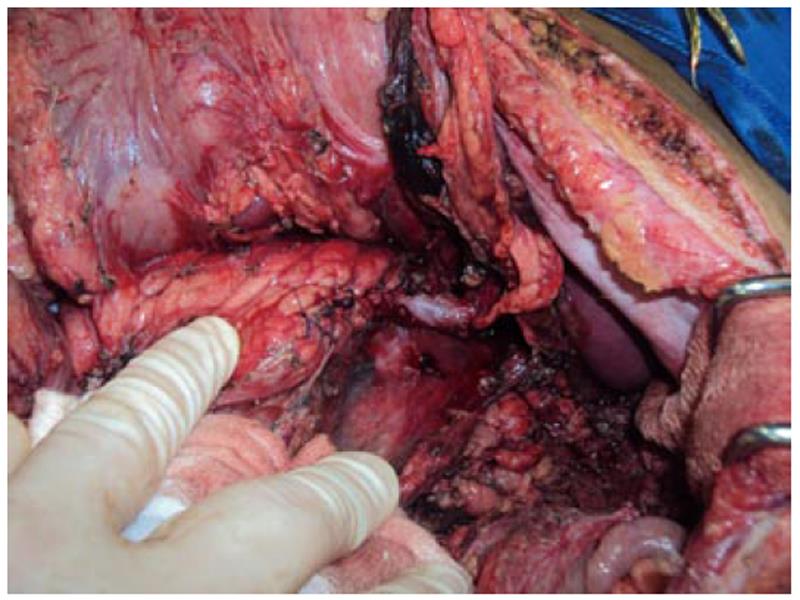
LHGJ, 18 years old, male, had a motorcycle accident 24 h earlier and presented with a blunt abdominal trauma. He decided to get medical attention due to abdominal pain and vomiting. He was hemodynamically stable (arterial pressure: 120 × 80 mmHg and heart rate: 110 bpm). On physical examination, abdominal palpation was painful with no signs of peritonitis. Laboratory tests and a computed tomography (CT) of the abdomen were carried out. Results: amylase: 1237 U/L; creatinine: 1.7mg/dL; glucose: 125 mg/dL; hemoglobin: 15.6. Abdominal CT: fluid in the upper abdomen, with a pancreatic trauma with transection of the main pancreatic duct. Other organs showed no signs of injuries (Figure 1A and B). Due to the high suspicion of main pancreatic injury, a laparotomy was performed. At surgery, the fracture with duct disruption was confirmed (Figure 2); a spleen-preserving DP maintaining the splenic vessels was performed. We carried out specific ligation of the main pancreatic duct and a hand sewn interrupted suture of the pancreatic stump (Figure 3). The patient recovered uneventfully and was discharged on postoperative day 5.
Trauma to the pancreas is a rare entity, especially when it is the only organ to be injured in an abdominal trauma[1,3,8,13]. This occurs due to its retroperitoneal location[3]. When it happens, physical examination can be poor and laboratory findings nonspecific[1], leading to delayed diagnosis and treatment. Thus, this injury has high rates of morbidity and mortality, with overall complications rates up to 62%[1,3], reaching 80% when diagnosis is made 24 h after injury[3]. The principal determinant of outcome in these patients is major duct involvement[1,3,14]. With the information above, one can understand why it is important to maintain a high suspicion in patients with unexplained abdominal signs after blunt trauma. Accurate and early diagnosis is imperative so that treatment can be offered as soon as possible.
CT has a low accuracy for diagnosis of pancreatic injury[15], with acceptable sensitivity ranging from 68%-71.4%[13,16,17]. Detecting major injury with CT is difficult, with low accuracy[1]. Findings on CT which may indicate pancreatic injury are intra/extra peritoneal fluid, fluid in the lesser sac, thickening of the left anterior renal fascia and, the most important one, fluid between the splenic vein and the pancreas, seen in 90% of cases. Findings on CT can be normal, despite the presence of duct disruption[15]. If transection of the pancreas is complete or laceration seen on CT is more than half of the organ, major duct injury should be suspected and surgery scheduled[3] or endoscopic retrogade pancreatography (ERP) performed if suitable. Besides CT, ERP and magnetic resonance pancreatography (MRP) can be performed. Since mortality and morbidity is strongly related to major duct injury, its integrity should be assessed. ERP can easily do this but is rarely available at the time of the trauma and only a few patients are suitable for the exam[3,17]. MRP is more available and easier to perform[3]. Another useful tool of ERP is ductal stenting. Lin et al[3] showed that the procedure helps in the management of pancreatic fistula but may be complicated by long term strictures. Attention must also be paid because stenting in the acute phase may lead to delay in necessary surgical and definitive treatment.
Surgery may be needed in almost all cases during the course of recovery. It may be indicated at admission or some time later to correct possible strictures. Choosing the right procedure depends on the extent of the injury and the presence or not of associated injuries. When distal duct disruption is present, pancreatic resection should be performed[3]; for proximal duct injury, closed suction drainage and distal resection can be selected, with duct stenting an option. A study from Taiwan showed that DP is a superior operative treatment for distal injuries when compared to pancreaticojejunostomy, which had a high complication rate of 60% due to anastomotic leakage[3]. The literature agrees that pancreatic fistula is responsible for high rates of morbidity and mortality in this kind of trauma, especially with delayed diagnosis[1,3,11,12].
When DP is indicated and there are no associated injuries, a controversial matter comes up: to preserve the spleen or not. Authors who advocate DP with splenectomy claim that this procedure increases blood loss, surgical time and demands great surgical skills. A small study with 40 patients conducted by Benoist in France suggested a better postoperative course when splenectomy is performed. He found significant differences in postoperative complications between the procedures for pancreatic fistula (12% vs 40%, P < 0.05) and subphrenic abscesses (4% vs 27%, P < 0.05), more frequent after spleen preservation. Due to this, hospital stay was longer in the preservation group. Despite their findings, they could not explain the difference in the rate of pancreatic fistula between the procedures[5]. Another possible disadvantage is that the displacement of the spleen may lead to an inherent risk of torsion or hemorrhage[6].
On the other hand, many authors accept and advocate the spleen preserving procedure[4,6,7,9-12]. The first ones to study and compare these two procedures and to favor spleen preservation were Richardson et al[17] and Aldridge et al[18]. Both groups consider DP with spleen preservation a safe and feasible procedure. Lin et al[3] found a 22% complication rate for spleen preserving against 72.7% for the splenectomy procedure (P < 0.05). The higher complication rate was, according to the authors, due to associated injuries, but not confirmed by others.
Shoup et al[12] discussed the main reasons for splenectomy: blood loss and surgical time. Patients whose spleen were preserved had less blood loss (350 mL vs 600 mL, P < 0.01). Surgical time tended to be longer in the splenectomy group, although significant difference was not reached. Another statistically significant finding was the incidence of infection; spleen preservation carried a 9% rate vs 28% in the splenectomy group (P = 0.07). In addition, complications in the latter group were more severe (P = 0.05), with an increased hospital stay (P < 0.01).
Carrère et al[11] also support the spleen preserving procedure. When splenectomy was performed, they found a significant difference for developing postoperative complications (13% vs 34%, P = 0.03), intra-abdominal infected collections (3% vs 18%, P = 0.02), infectious complications (8% vs 32%, P = 0.03). More reoperations were required in these patients, but this did not reach statistical significance. An interesting fact is that it did not happen due to associated injuries (P = 0.53). Univariate analysis showed that splenectomy was the only risk factor for postoperative complications (odds ratio: 3.2, 95% confidence interval: 1.1-10.2, P = 0.04).
Another study from Singapore[10] with 232 patients showed that splenectomy was associated with an increased risk of developing pancreatic fistula and non pancreatic fistula related complications. On univariate analysis, splenectomy was significantly associated with non pancreatic fistula related complications (P = 0.049). They suggest that splenic preservation does not decrease the occurrence of pancreatic fistula but may protect against its progression to infectious complications[10].
The same opinion is shared by Rodríguez et al[7]. In their paper, patients who had their spleen preserved had less blood loss (P < 0.0001), shorter operative time (P < 0.0001) and shorter hospitalization (P < 0.0001), consistent with other findings[10,12]. These factors were significant predictors of postoperative complications. Another issue discussed was that macroscopic inspection of the spleen is reliable, as mentioned in other papers[7,11], although some changes in the organ’s color may occur[7].
In conclusion, our group believe that DP with spleen preservation is feasible and safe. Although it is mentioned in the literature as a debatable matter, the majority of papers favor spleen preservation, with a decreased risk of complications and good outcomes. We also suggest that the spleen preserving procedure be done whenever possible.
Peer reviewers: Sonshin Takao, MD, PhD, Professor, Division of Advanced Medicine, Kagoshima University, Frontier Science Research Center, 8-35-1 Sakuragaoka, Kagoshima 890-8544, Japan; Alessandro Zerbi, MD, Department of Surgery, San Raffaele Hospital, Via Olgettina 60, Milano 20132, Italy
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
| 1. | Bradley EL, Young PR, Chang MC, Allen JE, Baker CC, Meredith W, Reed L, Thomason M. Diagnosis and initial management of blunt pancreatic trauma: guidelines from a multiinstitutional review. Ann Surg. 1998;227:861-869. |
| 2. | Beckingham IJ, Krige JE. ABC of diseases of liver, pancreas, and biliary system: Liver and pancreatic trauma. BMJ. 2001;322:783-785. |
| 3. | Lin BC, Chen RJ, Fang JF, Hsu YP, Kao YC, Kao JL. Management of blunt major pancreatic injury. J Trauma. 2004;56:774-778. |
| 4. | Thomas H, Madanur M, Bartlett A, Marangoni G, Heaton N, Rela M. Pancreatic trauma--12-year experience from a tertiary center. Pancreas. 2009;38:113-116. |
| 5. | Benoist S, Dugué L, Sauvanet A, Valverde A, Mauvais F, Paye F, Farges O, Belghiti J. Is there a role of preservation of the spleen in distal pancreatectomy? J Am Coll Surg. 1999;188:255-260. |
| 6. | Hirota M, Ichihara A, Furuhashi S, Tanaka H, Takamori H, Baba H. Spleen and gastrosplenic ligament preserving distal pancreatectomy under a minimum incision approach assisted by laparoscopy. J Hepatobiliary Pancreat Surg. 2009;16:792-795. |
| 7. | Rodríguez JR, Madanat MG, Healy BC, Thayer SP, Warshaw AL, Fernández-del Castillo C. Distal pancreatectomy with splenic preservation revisited. Surgery. 2007;141:619-625. |
| 8. | de Wilt JH, van Eijck CH, Hussain SM, Bonjer HJ. Laparoscopic spleen preserving distal pancreatectomy after blunt abdominal trauma. Injury. 2003;34:233-234. |
| 9. | Bruzoni M, Sasson AR. Open and laparoscopic spleen-preserving, splenic vessel-preserving distal pancreatectomy: indications and outcomes. J Gastrointest Surg. 2008;12:1202-1206. |
| 10. | Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, Chow PK, Soo KC, Wong WK, Ooi LL. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg. 2008;143:956-965. |
| 11. | Carrère N, Abid S, Julio CH, Bloom E, Pradère B. Spleen-preserving distal pancreatectomy with excision of splenic artery and vein: a case-matched comparison with conventional distal pancreatectomy with splenectomy. World J Surg. 2007;31:375-382. |
| 12. | Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002;137:164-168. |
| 13. | Lochan R, Sen G, Barrett AM, Scott J, Charnley RM. Management strategies in isolated pancreatic trauma. J Hepatobiliary Pancreat Surg. 2009;16:189-196. |
| 14. | Oláh A, Issekutz A, Haulik L, Makay R. Pancreatic transection from blunt abdominal trauma: early versus delayed diagnosis and surgical management. Dig Surg. 2003;20:408-414. |
| 15. | Brestas PS, Karakyklas D, Gardelis J, Tsouroulas M, Drossos C. Sequential CT evaluation of isolated non-penetrating pancreatic trauma. JOP. 2006;7:51-55. |
| 16. | Govaert MJ, Ponsen KJ, de Jonge L, de Wit LT, Obertop H. Fracture of the pancreas in two patients after a go-kart accident. HPB (Oxford). 2001;3:3-6. |