Published online Aug 27, 2011. doi: 10.4240/wjgs.v3.i8.128
Revised: June 6, 2011
Accepted: June 15, 2011
Published online: August 27, 2011
Duplications of the alimentary tract (ATD) are rare congenital anomalies often found early in life. They may occur anywhere in the intestinal tract but the ileum is the most frequently affected site. Clinical presentation of ATD in adults is variable and because these lesions occur so infrequently they are rarely suspected. In the present report we describe a case of ileal duplication in a 61-year-old patient with Crohn’s disease. Despite various radiological investigations and medical consultations, the diagnosis was only made on the surgical specimen.
- Citation: Fiorani C, Scaramuzzo R, Lazzaro A, Biancone L, Palmieri G, Gaspari AL, Sica G. Intestinal duplication in adulthood: A rare entity, difficult to diagnose. World J Gastrointest Surg 2011; 3(8): 128-130
- URL: https://www.wjgnet.com/1948-9366/full/v3/i8/128.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i8.128
Duplications of the alimentary tract (ATD) are rare congenital anomalies. Eighty percent of ATD are diagnosed in children before the age of 2 years. They may occur anywhere in the intestinal tract but the ileum is the most frequent affected site[1-3].
Due to the infrequency of ATD and its major relevance in the pediatric population, the analyses of patient characteristics and clinical manifestations in the adult are limited.
In the present report we describe a case of ileal duplication in a 61-year-old patient with Crohn’s disease.
A 61-year-old Caucasian patient with a 5-mo history of intermittent diffuse abdominal pain associated with nausea, vomiting and weight loss was referred to our Gastroenterology Unit with a diagnosis of ileal Crohn’s disease. A small bowel follow through (SBFT) showed an ileal stricture associated with dilation above a stenosis and a suspected entero-enteric fistula at about 30 cm from the ileo-cecal valve (Figure 1). However, no radiological evidence of mucosal lesions, including ulcers, was detectable. Steroid treatment was given, followed by incomplete remission.
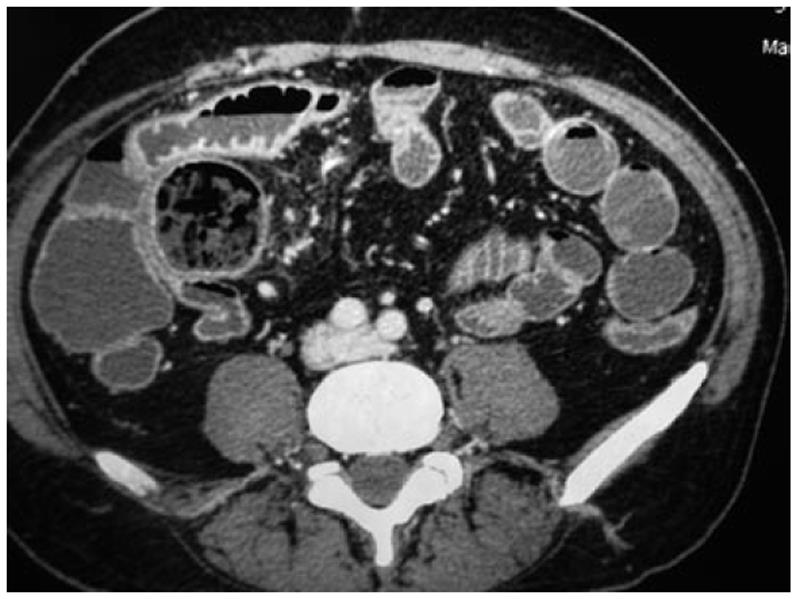
Clinical examination and blood tests at admission were normal. The patient had no family history of inflammatory bowel disease (IBD) and there were no abdominal masses, cutaneous fistulas or other stigmata of Crohn’s disease. A Small Bowel Contrast Ultrasonography (SICUS) was performed that showed findings comparable to SBFT. Oral budesonide (9 mg/d) was given with temporary and partial benefit. Entero-computed tomography (CT) scan confirmed the ileal stenosis associated with dilation above the stricture but it also visualized a blind loop of the intestine close to the stenosis (resembling a diverticulum) and enlarged mesenteric lymph-nodes (Figure 2). At this point, a differential diagnosis between CD and intestinal lymphoma was made in a symptomatic patient, giving an indication for an explorative laparotomy.
At surgery, an inflammatory mass was found in the right iliac fossa. The terminal and pre-terminal ileum, the cecum and the great omentum were involved. Tight adhesions were found between the above mentioned structures and both the terminal ileum and regional mesentery. The intestine at this level was thickened and a pre-stenotic dilation was present. A standard ileo-cecal resection was performed and the surgeon described the intra-operative findings compatible with an inflammatory mass of unknown origin. The patient made an uneventful recovery and was discharged home within a week.
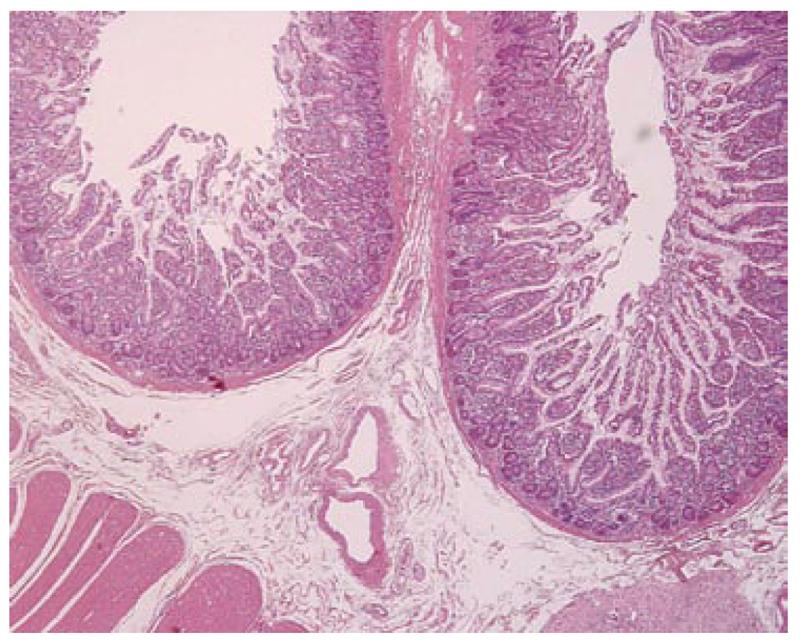
Macroscopic examination showed a tubular structure communicating with the ileal lumen that measured 5.5 cm × 2.5 cm × 2 cm. The cut surface was morphologically indistinguishable from the normal ileal wall. Light microscopy (Figure 3) highlighted the four layered organization of the ATD wall, including a mucosa with an intestinal-type epithelial lining and a muscularis propria, with an inner circular and outer longitudinal smooth muscle layers. A myenteric plexus was present between the two muscle coats.
The mucosa showed patchy features of ischemic injury. A diagnosis of ileal duplication was finally made.
ATD are congenital anomalies of the intestine, first described by Fitz[4]. They can be spherical or tubular and can be attached or adherent to the ATD. These conditions are rare (1/10 000 live births), usually encountered in the ileum[1,2] and the vast majority are found in infants[5,6]. The differential diagnosis is with mesenteric cysts and true and false diverticula. However, a duplication shares a portion of its wall with the adjacent small intestine, usually sharing a common blood supply. The epithelial lining is always of some part of the ATD and may include heterotopic gastric mucosa. Malignant degeneration has been described in the adult series[7].
According to the review published by Johnson et al[8] in 1994, cancer was found in 3 (23%) of 13 reported cases of ileal duplications in adults (2 adenocarcinoma and 1 squamous cell carcinoma). This evidence of epithelial instability might suggest a tendency toward malignant transformation in long standing duplications. This also supports complete resection of the duplication as the most appropriate method of treatment.
Clinical presentation of ATD in adults is variable and, because these lesions occur so infrequently, they are not suspected. A palpable mass can be found in approximately one half of patients; abdominal pain is often present but the most common clinical presentations include intestinal obstruction and bleeding[1,9-11]. It is worthwhile to highlight that the clinical presentation is strictly related to the site and type of ATD. In cases of ATD of the hindgut, the diagnosis is often made within the first years of life and the most frequent symptom is biliary vomits. These malformations are usually cystic and localized on the mesenteric border of the first or second duodenum. In the jejunum, the most frequent aspect includes a tubular duplication with a common lumen, whilst in the ileum ADT can resemble a diverticulum. Ileal duplication affecting the distal part of the intestine should be distinguished from a Meckel’s diverticulum, even though this is present on the anti-mesenteric border of the intestine. Complications of ATD include volvulus, invagination, bleeding, perforation and malignancy.
Twenty-seven cases of ileal duplications in adults are described in the world literature in over 100 years. In one of these cases, the correct diagnosis was made pre-operatively. In this case, clinical presentation and pre-operative studies supported a diagnosis of complicated CD. Biopsies were not taken because it was not possible to enter the ileo-cecal valve during diagnostic colonoscopy and the rest of colonic mucosa was normal. Laparotomy is also often indicated in these settings to make a differential diagnosis[12]. Abdominal scans such as SICUS, CT or MRI and conventional contrast x-ray studies are useful tools to detect ATD. The diagnostic problems arise from the extreme rarity of this entity in the adult population.
We hereby describe a case of an adult patient who underwent various radiological studies and was referred to different physicians during the year before the correct diagnosis was made. The patient had 3 previous admissions to A&E and was on oral steroids when referred to our Gastroenterology Unit. ATD was not suspected and the diagnosis was made on the surgical specimen.
In conclusion, ATD are congenital abnormalities that can arise at any level from the mouth to the anus. They are rare and often found early in life. A minority of cases may remain undiscovered until adulthood when they may give rise to different symptoms, depending on the location. The ileum is the most frequent affected site and abdominal pain is the most referred symptom. Diagnosis is difficult due to the rarity of this entity. Symptoms are not specific and intestinal duplication is not considered in differential diagnoses. We believe therefore that it is useful to report new cases and to review the most relevant aspects of this entity. Surgical correction is the treatment of choice and, in the adult, resection of the entire duplication should be undertaken due to the reported incidence of malignancy.
Peer reviewer: Jorg H Kleeff, MD, Department of General Surgery, Klinikum rechts der Isar, Technical University of Munich, Ismaningerstr 22, Munich 81675, Germany
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
| 1. | Hackam DJ, Zalev A, Burnstein M, Rotstein OD, Koo J. Enteric duplication in the adult, derived from the foregut, midgut and hindgut: presentation, patterns and literature review. Can J Surg. 1997;40:129-133. [PubMed] |
| 2. | Iyer CP, Mahour GH. Duplications of the alimentary tract in infants and children. J Pediatr Surg. 1995;30:1267-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 100] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Holcomb GW, Gheissari A, O'Neill JA, Shorter NA, Bishop HC. Surgical management of alimentary tract duplications. Ann Surg. 1989;209:167-174. [PubMed] |
| 4. | Fitz RH. Persistent omphalo-mesenteric remains; their importance in the causation of intestinal duplication, cyst-formation, and obstruction. Am J Med Sci. 1884;88:30-57. [RCA] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Ildstad ST, Tollerud DJ, Weiss RG, Ryan DP, McGowan MA, Martin LW. Duplications of the alimentary tract. Clinical characteristics, preferred treatment, and associated malformations. Ann Surg. 1988;208:184-189. [PubMed] |
| 6. | Bissler JJ, Klein RL. Alimentary tract duplications in children: case and literature review. Clin Pediatr (Phila). 1988;27:152-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Orr MM, Edwards AJ. Neoplastic change in duplications of the alimentary tract. Br J Surg. 1975;62:269-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 101] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Johnson JA, Poole GV. Ileal duplications in adults. Presentation and treatment. Arch Surg. 1994;129:659-661. [PubMed] |
| 9. | Mboyo A, Monek O, Massicot R, Martin L, Destuynder O, Lemouel A, Aubert D. Cystic rectal duplication: a rare cause of neonatal intestinal obstruction. Pediatr Surg Int. 1997;12:452-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Steiner Z, Mogilner J. A rare case of completely isolated duplication cyst of the alimentary tract. J Pediatr Surg. 1999;34:1284-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Grosfeld JL, O'Neill JA, Clatworthy HW. Enteric duplications in infancy and childhood: an 18-year review. Ann Surg. 1970;172:83-90. [PubMed] |
| 12. | Dignass A, Van Assche G, Lindsay JO, Lémann M, Söderholm J, Colombel JF, Danese S, D'Hoore A, Gassull M, Gomollón F. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Current management. J Crohns Colitis. 2010;4:28-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1118] [Cited by in RCA: 1032] [Article Influence: 68.8] [Reference Citation Analysis (1)] |