INTRODUCTION
Meckel’s diverticulum (MD) is the most common congenital abnormality of the gastrointestinal tract, occurring in 1% to 2% of the population[1]. It is usually asymptomatic and becomes evident when complicated. Although MD appears equally in both sexes, it causes complications more frequently in males[2,3]. Lower gastrointestinal bleeding, obstruction and inflammation are the most common complications which usually occur in children under 10 years old. Occasionally, inversion of MD into the lumen of the bowel can cause intussusception, ischemia and infarction[4].
The incidence of intussesception attributed to an inversion of MD accounts for 4% of all cases presenting with intestinal obstruction due to intussusception[5]. It occurs when the MD sags into the bowel lumen and then serves as a lead point to allow telescoping of the small intestine, first into the distal ileum and then in to the large intestine, causing ileo-ileal and ileocolic type of intussusceptions. The vast majority of cases with ileocolic intussusception is idiopathic and has a tendency to appear in children under 2 years of age[1,6]. The incidence of MD complications has been reported to decrease with advancing age. However, intussusception attributed to an inversion of MD may appear in older ages[2].
Regarding the physiognomy of this occurrence, we report two cases of intussusception due to inverted Meckel’s diverticulum in 15 and 80 years old females.
CASE REPORT
Patient 1
A 15-year-old female presented to the emergency room complaining of abdominal pain and vomiting for the last 12 h. She had no significant past medical history or previous abdominal surgery. There was no family history of any hereditary illnesses.
On admission she had normal vital signs and a temperature of 37.3°C. Physical examination showed a slightly distended abdomen with hyperactive bowel sounds. The patient had moderate abdominal tenderness without guarding. No masses or hernias were identified. Laboratory tests revealed increased white blood cells (WBC) of 13 200 μ/L with shift to the left.
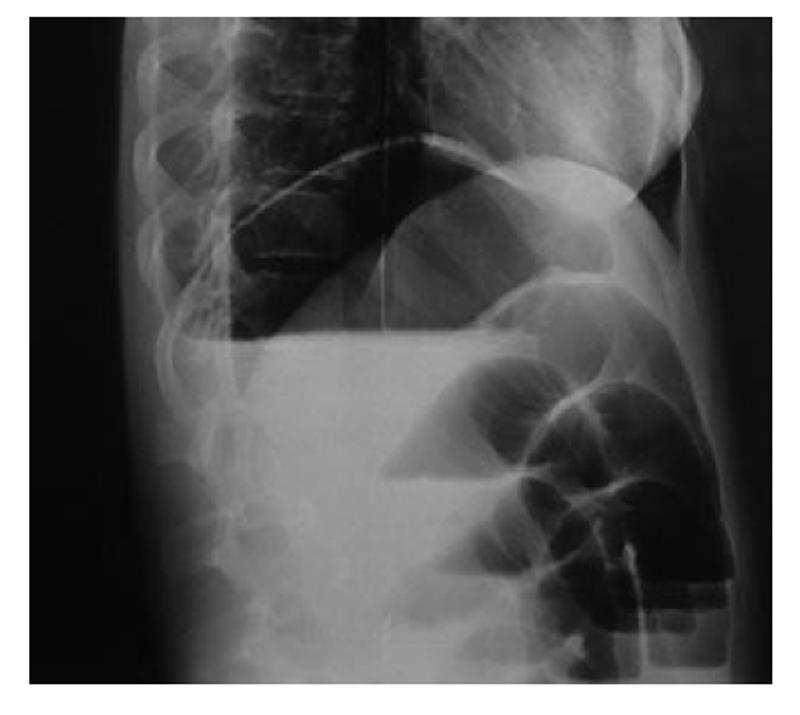
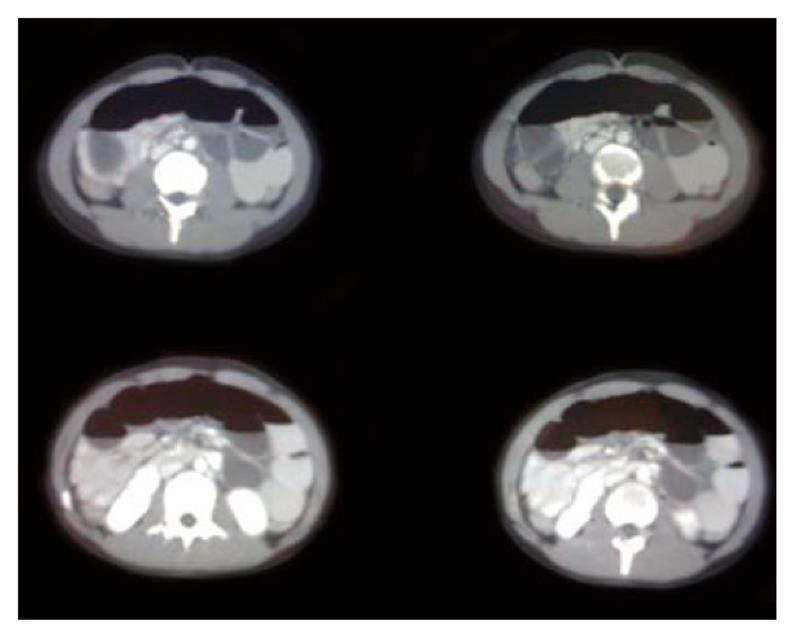
Plain abdominal X-ray demonstrated air fluid levels of the small bowel (Figure 1). Computed tomography (CT) revealed distension of the small intestine, especially of the jejunum and ileus. Furthermore, a mass lesion with concentric rings of fat and soft tissue attenuation was identified (Figure 2). These findings were consistent with a bowel obstruction secondary to an enteric intussusception.
Figure 1 Plain abdominal X-ray demonstrated air fluid levels of the small bowel.
Figure 2 Computed tomography revealed distention of the small intestine at the level of jejunum and ileus.
A mass lesion was identified with concentric rings of fat and soft- tissue attenuation.
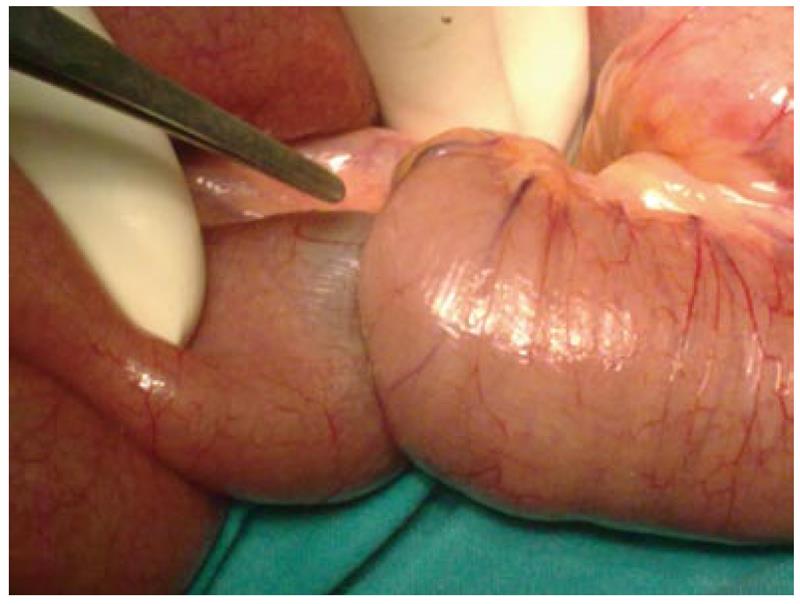
A decision to operate was made based on the above findings. A midline laparotomy was carried out. The intra operative findings were distention of the small bowel and intussusception of ileus due to an inverted MD located 20 cm from the ileocecal valve. The bowel was deployed and examined for signs of ischemia. No ischemic loop was identified. A diverticulectomy was performed using a TA stapler in parallel with the longitudinal axon of the bowel lumen (Figure 3). The operating time was 45 min. Histopathology revealed MD measuring 4 cm × 2 cm × 0.7 cm without ectopic mucosa or malignancy.
Figure 3 Intussuscepted portion of ileus attributed to inverted Meckel’s diverticulum.
The postoperative period was uneventful and after 6 d the patient was discharged. At the 12 mo follow-up, the patient had no evidence of complications.
Patient 2
An 80-year-old female with no previous laparotomies presented to the emergency room complaining of colicky abdominal pain, relieved after vomiting for the last 24 h. Her past medical history identified symptoms of anorexia for the past year, weight loss, repeated episodes of small bowel obstruction and readmissions for the last 3 mo. She had been investigated for these symptoms with a colonoscopy that was negative. Her family history was free of any hereditary illnesses.
On admission she had normal vital signs and a temperature of 37°C. Physical examination showed a distended abdomen with normal bowel sounds. The patient had moderate abdominal tenderness without concomitant peritoneal irritation. No masses or hernias were identified. Laboratory tests revealed increased WBC of 14 500 μ/L with shift to the left.
Plain abdominal X-ray demonstrated air fluid levels of small bowel. CT with contrast revealed distension of the small intestine and wall thickening. She was managed conservatively for the first 24 h but the patient did not respond well to the analgesics and severe distention was observed.
After a surgical consultation, the patient was admitted to the operating room. A midline laparotomy was carried out. The intra operative findings were distention of the small bowel and intussusception of ileus due to an inverted MD located 70 cm from the ileocecal valve (Figure 4). The free diverticulum acted as a lead point for intussusception. Extensive fibrosis of the adjacent mesentery and thickening of jejunal mucosa were also identified. No ischemic loop was identified. A segmental small bowel resection and hand-sewn anastomosis was performed. The operating time was 50 min. Histopathology distinguished MD measuring 3.5 cm × 2.5 cm × 1 cm and no signs of malignancy. The postoperative period was uneventful and after 7 d the patient was discharged. At 6 mo follow-up, the patient remains asymptomatic and without recurrence.
Figure 4 Intraoperative image of a free diverticulum located at an approximate distance of 70 cm from ileocecal valve.
DISCUSSION
There is a paucity of data regarding the true incidence of intussusception due to MD. Only a few cases have been reported in the literature[7-13]. Epidemiological data confirm that the chronic clinical course paces patients with inverted MD to the operating room in older ages[14-16]. However, the presented first case occurred in a young patient 15 years old. The second case occurred in an 80-year-old female who had multiple admissions for partial bowel obstruction. That implies that ileo-ileal intussusception can be observed in any age group.
Preoperative clinical diagnosis for adults remains a challenge as the classic triad of childhood intussusception occurs in only 15%-20% of cases[17]. The usual concept embraces long lasting symptoms of partial obstruction[18,19].
Therefore, several clinical characteristics such as history of previous attacks, the chronic course of disease with vomiting and possibly rectal bleeding and a palpable mass have been identified to distinguish the intussusception from an inverted Meckel diverticulum[20]. However, our first patient did not have any of these features and presented acutely, whereas our second patient had had readmissions for a long time.
CT is the most sensitive imaging modality for diagnosis of bowel obstruction with reported accuracy of 58%-100%[21]. In the early stage, the characteristic point is the target lesion, described as enveloped, eccentrically located areas of low density, which represents the intussuscepted bowel viewed in cross section[22]. That was identified only in our first case. However, this imaging stamp is noticed in intussusceptions caused by other pathological lesions, which limit the sensitivity and specificity of CT to identify the cause of intussusception[23]. CT enteroclysis and magnetic resonance enteroclysis are up-to-date alternative studies for successful diagnosis of MD[24]. Other findings, such as vascular compromise, layering or stratification effect to bowel wall thickening and amorphous mass recognized later in the natural history of unrelieved intussusception were not revealed in our cases[22]. Thus, CT is recommended not only as a strong diagnostic tool but also as a determinator of progression and severity of this process.
Referring to the location, MD is usually found within 100 cm of the ileocecal valve[2]. In our two cases, the distance was calculated as 20 and 70 cm respectively.
Concerning the surgical treatment, the available techniques reported in the literature are classified based on the location of MD and the progression and the severity of the process. Simple diverticulectomy or segmental resection is preferred for the small bowel, since the malignancy rate is low (17%)[25-27]. Diverticulectomy is predicated as a simple, minimal and cost effective technique which can resolve the problem[19].
Resection with anastomosis is clearly indicated in cases of inflammation and ischemia of ileum and is also recommended in edematous, inflamed or perforated base of MD. Laparoscopy represents an alternative method of treatment with techniques varied from segmental resection of MD[28] to reduction of intussusception, diverticulectomy and intracorporeal anastomosis[29].
The authors preferred the open approach due to the uncertainty of the diagnosis. Laparoscopy seems to be safe and effective as a treatment option in emergency surgery for small bowel obstruction. However, in routine practice there are obstacles such as proper instrumentation and facilities available in the setting of emergency surgery. Moreover, there is an absence of level I evidence knowledge to support the proper treatment options[30].
Intra operatively, the intussuscepted bowel was deployed and examined for ischemia. There is no doubt that in case of transmural ischemia, the bowel needs to be resected along with the diverticulum. Intussusception due to MD is an absolute indication for MD resection. In one of the cases, simple diverticulectomy was performed using a TA stapler. There is currently a lack of strong evidence to support the use of a stapler for the MD diverticulectomy. The morbidity and leak rates seem to be equivalent or even better than that reported in a hand-sewn technique[31]. Few published series have addressed the results from this surgical technique. More specifically, Vadalà et al[32] described his experience in treating seven cases of diverticulectomies in the emergency setting with the use of staplers, emphasizing the reduction of operative time and the decreased postoperative complications. Additionally, Patsner et al[33] reported diverticulectomies in sixteen patients during gynecological cancer surgery without morbidity.
In our study, we report two cases of successful management of adult ileus intussusception due to inverted MD. The novel information is that this uncommon entity can be observed even in extreme adult ages, since the first patient was only 15 years old while the second patient was 80 years old. Age might be a predictor factor for the type of the operation although this needs to be further investigated.
In adult cases there are usually previous episodes or even readmissions. It could be assumed that age may influence the clinical course along with the surgical treatment. A long life period with multiple episodes of partial obstruction seems to be related to structural effects in the wall of the small bowel and the adjustment structures, as confirmed in the elderly patient. That predisposes the severity of the intraoperative findings and the type of the proper surgical procedure since only diverticulectomy was adequate for the very young patient and a wider resection was considered necessary for the old patient.
In conclusion, adult intussusception caused by inverted MD may be observed in any age. Diverticulectomy vs bowel resection are the standard treatment. Age should be considered as a predictive factor for the surgical strategy.