INTRODUCTION
The incidence of metastatic esophageal tumor (MET) is low, ranging from 0.3%-6.1% in autopsy series[1-3], with hepatocellular carcinoma (HCC) was accounting for less than 0.4% of primary lesions[4]. The majority of METs are associated with diffuse metastases or with mediastinal carcinomatosis, and thus are not candidates for aggressive local treatments. Recently, we performed a robot-assited local resection of an isolated partially obstructing MET using the da Vinci surgical system in a patient who had undergone liver transplantation for cirrhotic liver associated with HCC. The case is reported herein.
CASE REPORT
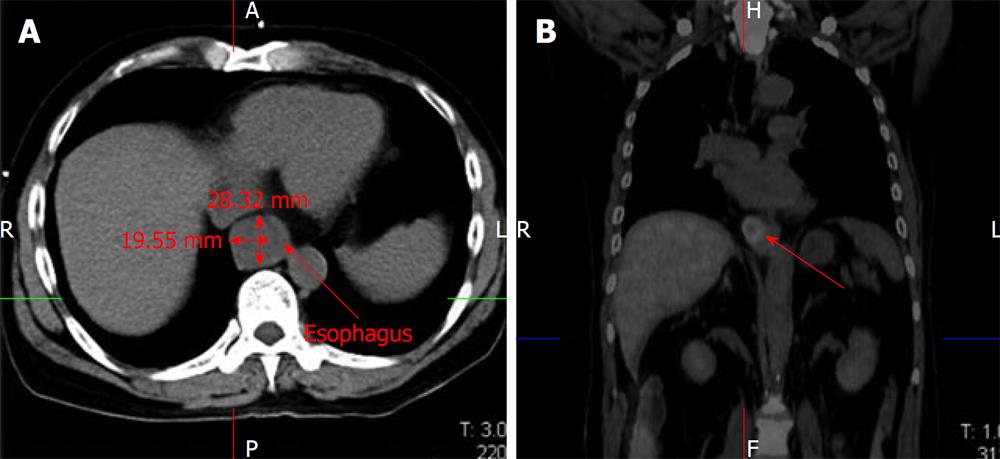
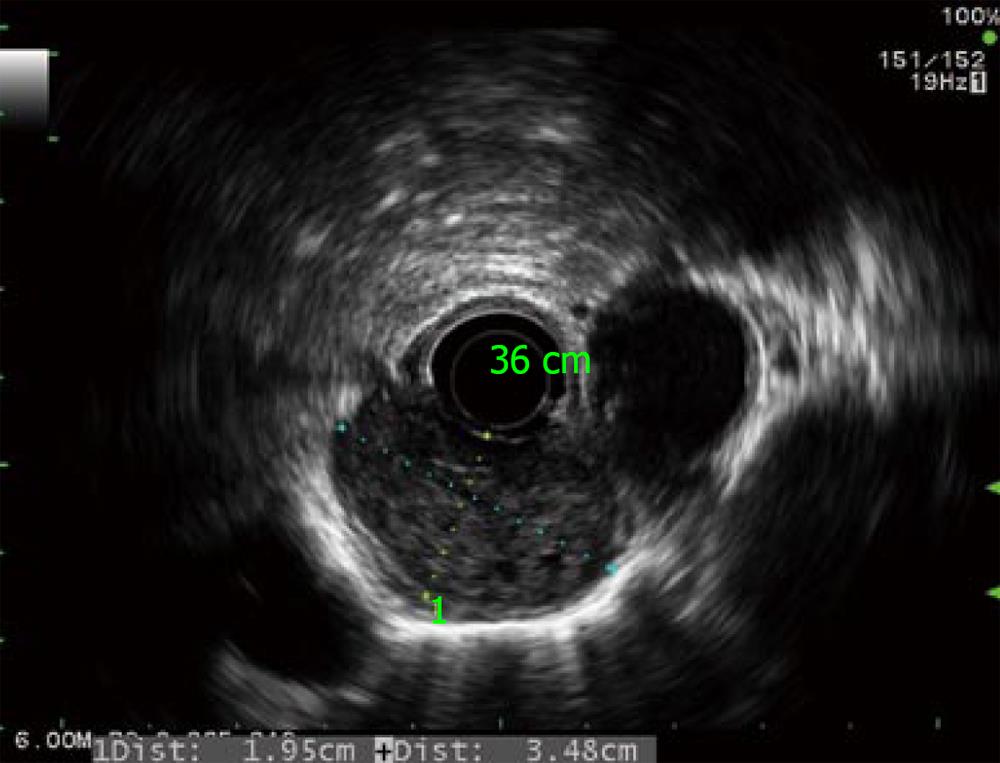
The patient was a 59-year-old man who underwent liver transplantation for cirrhotic liver associated with a solitary HCC. Three and a half years later, he developed progressive dysphagia. Esophagography showed severe narrowing of the distal esophagus. Computed tomography (CT) scan demonstrated marked thickening of the esophageal wall around the stricture (Figure 1A). Endoscopic study revealed an extrinsic compression at 35 cm from the incisors, causing severe stenosis but without any mucosal irregularity. Positron emission tomography (PET) scan showed marked uptake by the esophageal tumor without any recurrence of HCC at other sites (Figure 1B). Endoscopic ultrasonography revealed a large submucosal tumor of 1.9 cm × 3.5 cm. in diameter in the lower esophagus (Figure 2). Laboratory analysis revealed an elevated α-fetoprotein level of 510 ng/mL. The patients was diagnosed with MET from recurrent HCC. Since his general condition was excellent, we decided to perform surgical resection.
Figure 1 Computed tomography scan demonstrated marked thickening of the esophageal wall (A).
Positron emission tomography scan showed marked uptake by the esophageal lesion without any recurrence of hepatocellular carcinoma at other sites (B).
Figure 2 Radial echoendoscopy showed a heterogeneous submucosal tumor about 2 cm × 3.
5 cm in diameter without periesophageal lymph node.
Surgical technique
After induction of general anesthesia with a single-lumen endotracheal tube, the patient was placed in the lithotomy position. An arterial line, a central venous catheter, and a Foley catheter were placed. Pneumatic compression stockings were placed on both legs. Preoperative antibiotics were administered. The abdomen were prepared and draped in the usual sterile fashion. After placing the trocar, the abdomen was insufflated to 14 mmHg. The abdominal cavity was inspected for any evidence of carcinomatosis. Lysis adhesion was performed using standard laparoscopy. Part of the dense adhesion of the omentum was transected using endoGIA staples for prevention of intra-operative bleeding. Laparoscopic ultrasonography of the liver demonstrated no recurrence of HCC.
The da Vinci surgical system was then brought into position, cephalad to the patient, And the arms of the system were attached to the trocars. The robotic camera and the two operating robotic instruments were secured in their ports. Transabdominal dissection of the distal esophagus and stomach was started and continued in a cephalad direction along the circumferential borders of the esophagus. The articulated hook cautery was used for this maneuver, allowing precise circumferential dissection of the esophagus, and division of each individual periesophageal attachment with minimal blood loss and trauma. The tumor of the lower esophagus was mobilized so esophageal metastastectomy and esophagogastrostomy were performed using the robotic system (Figure 3). The esophagogastrostomy anastomosis was created by the robotic hand-sew technique with vicryl #3/0 interrupted stitches.
Figure 3 Intraoperative finding of the da Vinci S Robotic surgical system (A), the dense adhesion was resected using endoGIA staple (B).
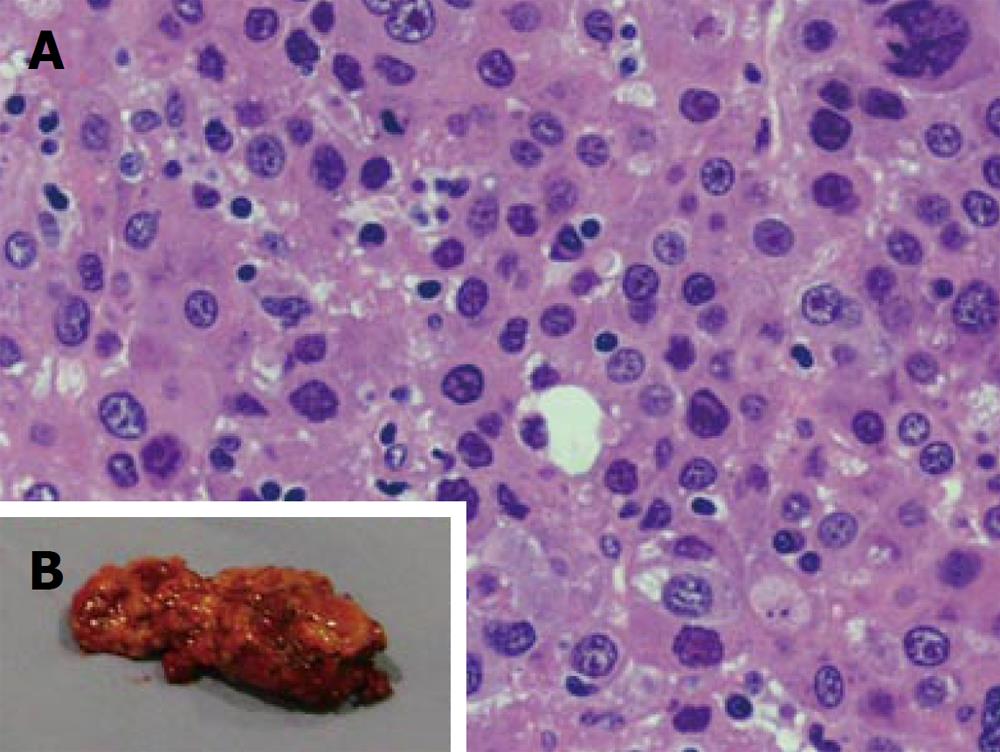
Pathological study confirmed the resected specimen was a HCC, suggesting metastatic lesions from the liver (Figure 4). The patient was discharged 14 d later with no apparent symptoms after the surgery. The α-fetoprotein level decreased to 30 ng/mL. Two months later, he developed anastomosis stricture causing dysphagia which was successfully treated by endoscopic esophageal dilatation.
Figure 4 Pathological result of the resected specimen confirmed metastasis from hepatocellular carcinoma.
DISCUSSION
Since Gross firstly reported a case of metastatic esophageal cancer from the prostate[5], many reports have shown the esophagus to be a frequent metastatic site from a variety of malignancies including breast[6], lung[7], ovary[8], liver[9], rectum[10] and others[11-14]. In autopsy studies, the overall incidence of esophageal metastases is 0.3%-6%[1-3]. The most common primary tumor-bearing organs are breast and lung[6,7]. Esophageal metastasis from HCC has only been described in one previous report[9]. Our case was diagnosed as an esophageal metastasis from HCC, which is extremely rare especially post liver transplantation.
The possible routes of esophageal involvement are direct extension from adjacent organs, mediastinal nodes or hematogenous spreading from a distant primary[15]. In this caseit is most likely that the HCC developed secondary metastasis in the esophageal wall through hematogenous spread.
METs are usually located in the submucosal layer and cause progressive dysphagia[3,16]. Esophagography and endoscopy show severe luminal stricture with normal overlying mucosa, often making histological diagnosis difficult[16]. CT scan demonstrates concentric thickening of the esophageal wall over the stricture without an apparent extrinsic mass[16,17]. In our patient, the diagnosis was confirmed by PET scan which showed marked uptake by the tumor (SUV - MAX = 4.5) an by an increase in α fetoprotein level to 510 ng/mL. Standard treatment for metastatic esophageal cancer has not yet been established. However, as the majority of such patients already have advanced malignant disease or metastases at multiple sites, systemic chemotherapy and/or local radiation are usually considered as the first choice of treatment. Unfortunately, when the symptoms appear, the majority of the patients already have distant metastases[9]. Therefore, treatment has been directed toward palliation, for which a variety of options exist, including endoscopic dilation and stent placement or esophagectomy[7]. As metastatic HCC shows poor response to chemo-radiation, we discussed with the patient that surgical removal is the optimal treatment. However, recent reports have shown that esophagectomy can provide excellent palliation and long-term survival in certain cases without metastases to other sites[3,6-8,11,18-21]. The prognosis varied from 7 mo to 14 years after esophagectomy, depending on the biological characteristics of the primary malignancy.
The use of the da Vinci Robotic Surgical System (Intuitive Surgical, Sunnyvale, California) provides the advantages of three-dimensional visualization through a stereo endoscope, tremor reduction, motion scaling, and wristed instrumentation with additional degrees of freedom compared to standard laparoscopic instruments[22,23]. It may be that advanced robotics will be reserved for only the most complex operations, such as esophagectomy and reconstruction. The system allows the surgeon to work in the narrow space of the mediastinum, overcoming spatial limitations experienced while using thoracoscopic or laparoscopic techniques. The robotic system is of tremendous help in accessing remote areas through a small esophageal hiatus. The extent of lymphadenectomy and the total operative time were not issues in this procedure, but might be improved on with further experience[24]. In authors’ opinion, robotic surgery can ameliorate the technical difficulties encountered laparoscopically and may allow surgeons to perform this and other delicate procedures without increased operative time, because of the maneuverability and increased length of the instruments as well as the excellent three-dimensional operative view. From our experience with this new robotic system, aggressive surgery might be considered as a therapeutic procedure for metastatic HCC of the esophagus, as long as the primary tumor is satisfactorily controlled.
In conclusion, we report a rare case of premortem-diagnosed esophageal metastasis from HCC in a patient who had previously undergone liver transplantation. We performed what is possibly the first reported successful esophageal metastatectomy and reconstruction esophagogastrostomy using the da Vinci robotic system.