INTRODUCTION
Diverticulosis is a common condition in Western countries, affecting approximately 30%-50% of adults over the age of 60 and 67% over 80 years[1,2]. It is defined as a pocket of mucosa bounded by muscularis mucosa which herniates through areas of weakness in the muscularis propria, usually at vascular entry sites[3]. Complications of diverticulosis include diverticulitis, bleeding, abscess formation, fistula, stricture formation and free perforation. Approximately 10% of patients with diverticulosis will eventually develop acute diverticulitis and other complications[4]. Occasionally acute diverticulitis will involve the female organs, especially the left ovary which lies in close proximity to the sigmoid colon where diverticula are most commonly located[8]. In such cases, the usual predominantly bowel symptoms of diverticulitis, such as localized lower abdominal pain, constipation or diarrhea and increased flatulence, may be minimal or absent[10]. We present a case of diverticulitis causing a tubo-ovarian abscess which was unrecognized due to atypical symptoms. Additionally, two abdominal-pelvic computerized tomography scans failed to demonstrate diverticula, eventually resulting in a free peritoneal perforation of the colon.
CASE REPORT
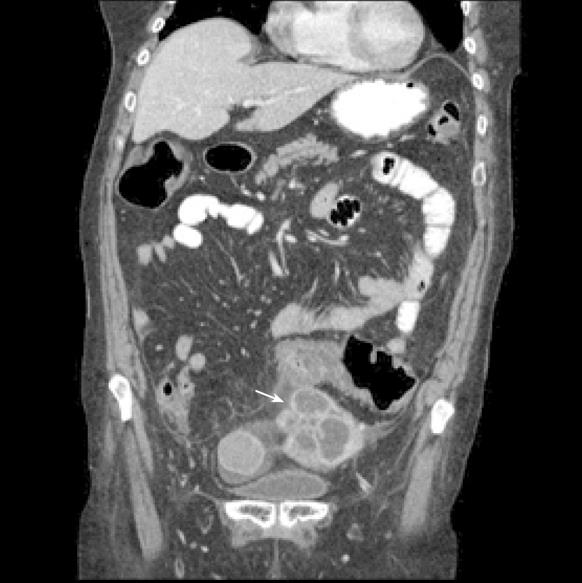
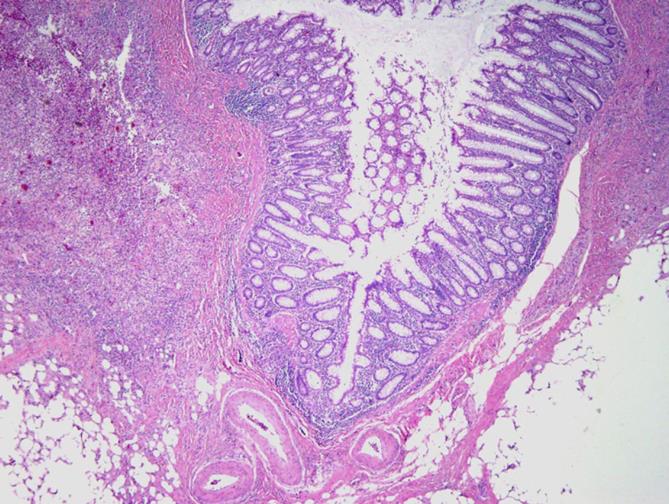
A 63-year old woman presented to her gastroenterologist with vague persistent abdominal cramps. A subsequent work-up consisting of an abdominal ultrasound demonstrated a complex left ovarian cystic mass and elective surgery was recommended by gynecology due to the suspicion of ovarian cancer. The patient, however, deferred surgery. She presented to the New York Presbyterian Hospital Emergency Department one month later because of increased abdominal discomfort and the new onset of diarrhea. On physical examination, she appeared to be well nourished, well developed and in no acute distress. Vital signs were all normal, including a temperature of 36.7 degrees centigrade. Her examination was only remarkable for mild distention with left upper quadrant, right lower quadrant and suprapubic tenderness, without rebound tenderness. Laboratory data was significant for hypokalemia (2.9 mmol/L), leukocytosis (18 500 uL) and hypoalbuminemia (2.3 g/dL). An abdominal-pelvic CT scan confirmed the presence of a complex cystic left adnexal mass with surrounding inflammatory changes and mild ascites. The sigmoid colon adjacent to the pelvic mass contained a long segment of wall thickening, without diverticula seen (Figure 1). The patient was treated with levaquin and metronidazole antibiotics for a presumed tubo-ovarian abscess. Evaluation of the patient’s diarrhea with stool examination revealed evidence of fecal leukocytes but no pathogenic bacteria, parasites or Clostridium difficile toxin. A subsequent flexible sigmoidoscopy was limited to only 30 cm from the anal verge due to severe narrowing. Biopsies of the sigmoid colon demonstrated non-specific inflamed colonic mucosa. On the ninth hospital day, the patient’s abdomen became more distended and a repeat abdominal-pelvic CT scan showed free intraperitoneal air but with a stable enhancing left pelvic mass inseparable from the adjacent sigmoid colon. The patient was taken to the operating room on the same day. The pelvic mass together with adherent sigmoid colon was removed. A subsequent pathological examination of the resected specimen revealed a 7-cm mass encompassing the left fallopian tube and ovary adherent to a perforated diverticulum of the sigmoid colon which contained features of organization and a striking fibroinflammatory response (Figure 2).
Figure 1 Tubo-ovarian abscess with adjacent sigmoid colon.
Figure 2 Perforated diverticulum with adjacent peri-colonic abscess.
(HE stain, x 40)
DISCUSSION
Postmenopausal tubo-ovarian abscesses may occur due to pelvic inflammatory disease but this is uncommon and most often the abscess is associated with a gynecological malignancy[6,7]. Often the possibility of acute diverticulitis is not considered pre-operatively. A series of seventeen patients with diagnoses of ovarian cancer or twisted ovarian cysts were proven at surgery to have acute diverticulitis as the cause of their symptoms and pre-operative findings[15]. In another series, five patients with the preoperative diagnoses of either twisted ovarian cyst, ovarian abscess or ectopic pregnancy were discovered post-operatively to be misdiagnosed and actually had acute diverticulitis[16]. In a larger series of 69 women who underwent surgery for what was believed to be gynecological disease, 38% were found to have acute diverticulitis[13]. Another case has been reported in the literature of a 31-year old woman who underwent the surgical resection of a tubo-ovarian abscess but required another operation shortly afterwards because of a recurrent pelvic abscess due to diverticulitis that was unrecognized at the time of the first operation[14]. This illustrates the importance of recognizing acute diverticulitis which may present as a gynecological problem, even at a young age. Diverticulitis with abscess formation can be very insidious and reports of presentation as only chronic diarrhea[11] or even an isolated brain abscess[12] have been described.
Early recognition of tubo-ovarian abscess resulting from diverticulitis and prompt treatment is crucial for prevention of further complications[9]. Appropriate surgical treatment with possible pre-operative percutaneous abscess drainage can avoid further complications such as stricture or fistula formation and free perforation[5]. The discovery of a pelvic mass together with any bowel symptoms should arouse suspicion of possible diverticulitis with abscess. Diverticula may be absent on x-ray examination as a consequence of intense peri-colonic inflammation secondary to the diverticulitis. The finding of a thickened loop of sigmoid colon adherent to the pelvic mass, even without diverticulosis, visualized on x-ray, is suggestive of possible diverticulitis as the underlying pathology. Prompt recognition of this condition early in the patient’s course will greatly improve the chances of a full and uncomplicated recovery.
Peer reviewers: Yoshihiro Moriwaki, MD, PhD, Department of Critical Care and Emergency Center, Yokohama City University Medical Center, 4-57, Urafune-cho, Minami-ku, Yokohama 232-0024, Japan; Theodoros E Pavlidis, MD, PhD, Professor, Department of Surgery, University of Thessaloniki, Hippocration Hospital, A Samothraki 23, Thessaloniki 54248, Greece
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng L