Published online Apr 27, 2011. doi: 10.4240/wjgs.v3.i4.49
Revised: April 3, 2011
Accepted: April 11, 2011
Published online: April 27, 2011
AIM: To globally approach the clinical entity of small bowel diverticulosis and, at the same time, set out the treatment options.
METHODS: We analysed 77 cases of diverticula located in the duodenum, jejunum and ileum that were treated in our department, evaluating the symptoms, diagnostic approach and offered treatment.
RESULTS: Almost half of the diverticula (46.7%) were incidentally discovered and Meckel’s diverticula represented the majority (43%) that were actually the only true diverticula. A high complication rate (53%) which included inflammation with or without perforation (22%), bleeding (10%) or obstructive ileus (12%) due to small bowel diverticulosis was reported. The preoperative diagnosis was often impossible (44% of complicated cases).
CONCLUSION: Although small bowel diverticulosis has a low incidence, it should be in the clinician’s mind in order to avoid misdiagnosis.
- Citation: Mantas D, Kykalos S, Patsouras D, Kouraklis G. Small intestine diverticula: Is there anything new? World J Gastrointest Surg 2011; 3(4): 49-53
- URL: https://www.wjgnet.com/1948-9366/full/v3/i4/49.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i4.49
Small bowel diverticula were first reported on autopsy by Cooper in 1907. In 1920, Case illustrated the lesion on X-ray. The first resection of diverticula was performed by Hunt and Cook 1 year later[1]. This outpouching deformity of the small bowel is usually asymptomatic but can also lead to various partial and serious complications. The management of this clinical entity should be a matter of concern for clinicians.
This report is presented as a continued study of a previous retrospective analysis[2], incorporating new cases of small bowel diverticula recorded in our department during the last decade so that the reference period extends from 1980 to 2009. There are now 77 cases.
This series includes both acquired and congenital diverticula from the duodenum to the ileum. The mean age of the patients, 45 males and 32 females, was 54.4 years and, in particular, 59 years (36-72 years), 64 years (28-87 years) and 24 years (16-36 years) for duodenal, ileal and Meckel’s diverticula respectively.
The clinical presentation, diagnostic method, number and site of the diverticula, treatment and postoperative complications were evaluated. Histopathological examination revealed that the only true diverticula were the so-called Meckel's diverticula, while all others showed a protrusion of mucosal and submucosal layers through a defect of the muscular layer covered by serosa.
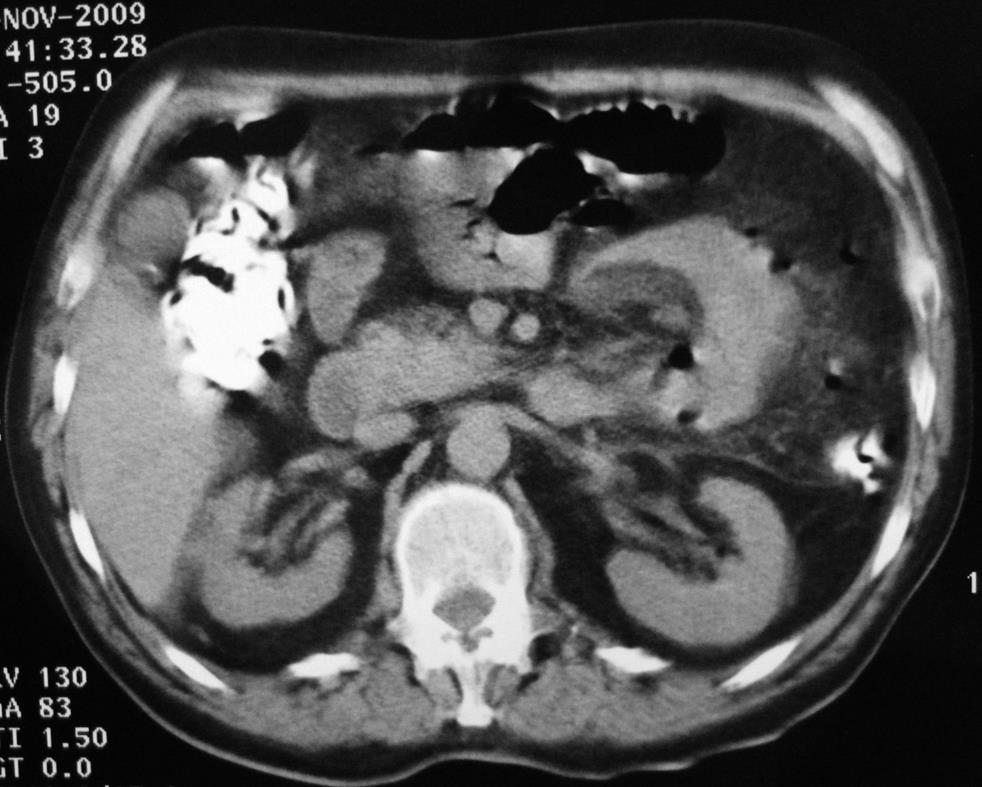
We would like to emphasize the case of a 68-year-old male patient who presented to us with abdominal pain in the left lower abdominal quadrant. He suffered from diabetes mellitus and myasthenia gravis and was treated by oral intake of cortisone and anticholinergic pills. He underwent an abdominal computed tomography (CT) scan that revealed sigmoid diverticulosis with concomitant pericolic fat opacity that affected the neighboring small bowel loops (Figure 1). The symptoms were attributed to a mild attack of sigmoid diverticulitis and the patient was treated conservatively. The first attempt of oral food intake after 4 d of fasting was accompanied by the recurrence of the symptoms, to the extent that the patient could not even tolerate water.
Capsule endoscopy was not indicated as a stricture could not be excluded. An enteroclysis was performed that revealed the presence of many small bowel diverticula without further signs of stricture, perforation or enteric fistula (Figure 2). As no sign of healing was seen, an explorative laparotomy was performed. The intraoperative findings were diffuse peritonitis caused by a perforated ileum diverticulum so a segmental enterectomy was performed and the patient was definitively treated. The coexistence of sigmoid diverticula had led to a false first diagnosis, delaying the operative intervention.
Diabetes mellitus and regular cortisone intake also covered the normally tumultuous clinical signs. Finally, we should connect myasthenia gravis and its therapy with the development of the small bowel diverticula in this patient. Although no direct correlation between myasthenia gravis and SBD has been established so far, there are several studies that implicate neurological diseases with the generation of SBD. A strong relationship with myasthenia gravis is also assumed with inflammatory bowel disease and neoplasia[3,4]. Furthermore, anticholinesterase drugs are responsible for vigorous peristaltic contractions and for an increase of the intraluminal pressure due to muscarinic effects on the smooth muscle of the small and large intestine[5,6].
There were 33 cases with Meckel’s diverticula, 19 cases with diverticula located in the duodenum and in the remaining 25 cases, diverticula were located in the jejunum and ileum. Multiple diverticula were discovered in 19 patients (Table 1).
| Meckel | 33 |
| Duodenal | 19 |
| Jejunum | 9 (6 multiple) |
| Ileum | 5 (2 multiple) |
| Both | 11 |
| Total | 77 |
The clinical signs and symptoms of all cases are presented in Table 2. Thirty-six cases of incidental SBD were discovered during laparotomy or upper G-I endoscopy. More than half of the cases (19 of 36) were a Meckel’s diverticulum while 12 were located in the duodenum and 5 in the jejunum and ileum (Table 3).We should point out that the widespread use of diagnostic gastroscopy and ERCP in our department has revealed 14 cases of duodenal diverticula, 11 of which were asymptomatic and required no further treatment.
| Asymptomatic-incidental | 36 | Only Meckel’s were treated |
| Symptomatic | 41 | |
| Bleeding | 8 | Pre-Op estimated 5 (Tc-scan 3, angiography 2) during OP estimated 3 |
| Fever | 17 | |
| Pain-discomfort | 24 | |
| Obstruction | 9 | |
| Diarrhea | 1 | |
| Jaundice | 2 | |
| Malabsorption | 1 |
| Meckel | 19 |
| Duodenal | 12 |
| Jejunum | 2 |
| Ileum | 1 |
| Both | 2 |
| Total | 36 |
The complication rate in our study group was as high as 53% (41 cases), with common complications of inflammation, perforation, bleeding and obstructive ileus.
The diagnosis of complicated SB diverticulosis was preoperatively established in 23 of the 41 total cases by using all the available diagnostic tools (Table 4).
| Asymptomatic | 15 |
| Bleeding | 6 |
| Inflammation | 7 |
| Obstruction | 5 |
| Total | 33 |
Enteroclysis and ERCP showed the presence of complicated diverticula in eight and three cases respectively. Abdominal CT revealed eight cases of Meckel diverticula, while Tc-99m scintigraphy and digital angiography proved useful in cases of bleeding. Enteroclysis remains an important diagnostic procedure for small bowel disorders. In our series, enteroclysis proved helpful in detecting 13 cases of SBD, four, five and two of which were located in duodenum, jejunum and ileum respectively. The two further cases were confined in the jejunum and ileum.
Diverticulitis or perforation with associated peritonitis led to an urgent operation in 14 cases but duodenal diverticulum was not found to be responsible for this complication. 50% of the cases were caused by Meckel’s diverticula, while jejunal diverticula were much more common than ileal (five against two cases respectively). The perforation was limited by the omentum and the neighbouring small bowel loops in most of the cases so generalized peritonitis was rare in our series.
The diagnosis of bleeding diverticula was preoperatively established in five of the eight cases presented to us. Bleeding scintigraphy and digital angiography revealed the lesion in three and two cases respectively. In the other three cases, the diagnosis was set through an explorative laparotomy for rectal bleeding of unknown origin as all diagnostic methods had failed to discover the true source. Meckel’s diverticula were the source in six of the bleeding cases (75%).
We treated 33 cases of Meckel’s diverticula (Table 5), 15 of which were asymptomatic and incidentally identified. In five patients, the diverticulum caused obstructive ileus of the small bowel due to invagination and volvulus. In all six cases of a bleeding Meckel’s diverticulum, a segmental enterectomy instead of a simple diverticulectomy was performed because the bleeding site was located mostly in the ileum adjacent to diverticulum. All the other non-bleeding Meckel’s diverticula, including seven cases of inflammation, were excised.
| Incidental findings | 19 |
| Emergency operation | 18 |
| Enteroclysis | 13 |
| Tc-scan | 3 |
| Angiography | 2 |
| Abdomen CT | 8 |
| Gastroscopy-ERCP | 14 |
| Total | 77 |
Most duodenal diverticula were incidentally discovered but two of them were associated with jaundice and abdominal discomfort. A further diverticulum of the third portion of the duodenum was in contact with a 3-cm large GIST of intermediate dignity. That patient was treated with local excision of the lesions. Furthermore, a patient with jejunal and ileal diverticula presented with malabsorption due to blind loop syndrome. The patient had megaloblastic anemia as the bacterial overgrowth led to B12 consumption and concomitant deficiency. Relief of symptoms was only noted after treatment with broad-spectrum oral antibiotics.
In our series, every symptomatic and complicated SBD, as well as all Meckel’s diverticula, were treated surgically, reaching the number of 60 operated cases. No late complications and no short bowel syndrome have been referred during our long follow-up period among our operated patients and all were completely relieved from the initial symptoms.
Small bowel diverticula is a clinical entity with special features as it usually remains silent. The site of protrusion is that of the entry points of the bowel vascular supply through the mesentery. This anatomical preference often makes them difficult to detect as they are located in the mesenteric leaves[7]. In some cases, the incoming vessel runs over the diverticulum dome. This close relationship is responsible for the complication of hemorrhage that results from diverticula[8].
Duodenal diverticula are the most common acquired diverticula of SB, with an incidence rate of 15% in autopsy studies. Most of them are located periampullary, projecting from the medial wall of the duodenum. Obstructions of the biliary or pancreatic duct, bleeding, perforation or blind loop syndrome are rare complications[9].
The presence of small bowel diverticula ranges from 0.1 to 1.5% in autopsy series. The higher incidence of SBD in the jejunum compared to the ileum is attributed to the larger diameter of the penetrating jejunal arteries. Their acute complications include intestinal obstruction, bleeding, inflammation and perforation, with that rate reaching 15%[10,11] in most studies. Obscure bleeding, malabsorption, enterolith formation and abdominal discomfort are their chronic clinical manifestations. The total complication rate was significantly higher in our series (53%), as previously mentioned.
All asymptomatic and incidentally discovered SBD (Meckel’s excluded) should not be treated. Some authors favor surgical intervention, especially for large diverticula with dilated bowel loops that suggests a progressive form of the disease. On the other hand, in all complicated cases, a segmental enterectomy with primary anastomosis should be performed[12].
The clinical presentation of small bowel diverticulitis is that of an acute abdomen. Although the treatment is predominantly surgical, in cases of local and self-limited inflammation and in the absence of perforation, a conservative approach is a possible option[13].
Bleeding from SBD presents as melena or hematochesia and the diagnostic algorithm should be that of lower intestinal bleeding. As long as upper GI bleeding is ruled out, coloscopy, scintigram or angiography have their role in the identification of the bleeding source. 99mTc-bleeding scan and angiography can detect hemorrhage when the bleeding rate is in the range of 0.1 mL/min and 0.5 to 1.0 mL/min respectively. Capsule videoscopy is also a useful tool for the clinician but is contraindicated in obstruction or bowel motility disorders[14,15].
Greater emphasis will be given to Meckel’s diverticulum as it is one of the most common congenital anomalies of the small bowel with an incidence rate of about 2% of the population. It is a pure diverticulum located on the antimesenteric border of the terminal ileum (45-60 cm proximal to the ileocecal valve) and is actually a rudiment of the omphalomesenteric duct. Although it is usually incidentally discovered, it is associated with many complications such as bleeding, diverticulitis, bowel obstruction or even neoplasms formation[16]. The intestinal obstruction occurs as a result of intussusception, volvulus or incarceration in a Littre’s hernia.
Although the treatment of choice of an incidentally discovered Meckel’s diverticulum in children is its resection, the recommendations for adults are controversial[17]. The tendency is to remove them as long as the patient’s age and the conditions in the abdomen allow it[18,19].
In conclusion, many diagnostic examinations such as enteroclysis, CT, Tc-99m scintigraphy and a video capsule are helpful to verify the existence and location of SBD. The appropriate approach (surgical or not) lies, as analyzed above, on their location and the symptoms or complications that they may generate.
Small bowel diverticula were first reported on autopsy by Cooper in 1907. In 1920, Case illustrated the lesion on X-ray. The first resection of diverticula was performed by Hunt and Cook 1 year later. This outpouching deformity of the small bowel is usually asymptomatic but can also lead to various partial and serious complications.
This report is presented as a continued study of a previous retrospective analysis, incorporating new cases of small bowel diverticula recorded in our department during the last decade so that the reference period extends from 1980 to 2009.
The complication rate in authors study group was as high as 53% (41 cases), with common complications of inflammation, perforation, bleeding and obstructive ileus. The diagnosis of complicated SB diverticulosis was preoperatively established in 23 of the 41 total cases by using all the available diagnostic tools.
The authors concluded that many diagnostic examinations such as enteroclysis, computed tomography, Tc-99m scintigraphy and a video capsule are helpful to verify the existence and location of SBD. The appropriate approach (surgical or not) lies, as analyzed above, on their location and the symptoms or complications that they may generate.
In general the paper is well written and covers many of the basic points of a case report and review of the literature. This is descriptive paper and could be discussed as a “lessons learned manuscript”.
Peer reviewer: Scott Steele, MD, FACS, FASCRS, Chief, Colon and Rectal Surgery, Department of Surgery, Madigan Army Medical Center, Fort Lewis, WA 98431, United States
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
| 1. | Herrington JL Jr. Perforation of acuired diverticula of the jejunum and ileum. Analysis of reported cases. Surgery. 1962;51:426-433. |
| 2. | Kouraklis G, Glinavou A, Mantas D, Kouskos E, Karatzas G. Clinical implications of small bowel diverticula. Isr Med Assoc J. 2002;4:431-433. |
| 3. | Martin RW, Shah A. Myasthenia gravis coexistent with Crohn's disease. J Clin Gastroenterol. 1991;13:112-113. |
| 4. | Lossos A, River Y, Eliakim A, Steiner I. Neurologic aspects of inflammatory bowel disease. Neurology. 1995;45:416-421. |
| 5. | Bassotti G, Imbimbo BP, Betti C, Erbella GS, Pelli MA, Morelli A. Edrophonium chloride for testing colonic contractile activity in man. Acta Physiol Scand. 1991;141:289-293. |
| 6. | Li Destri G, Scilletta B, Latino R, Di Cataldo A. [Myasthenia gravis and intestinal resection: is dehiscence likely to occur?]. Minerva Chir. 2006;61:525-528. |
| 7. | Garrett JP, Nolan DJ. Diverticula of the terminal ileum. Clin Radiol. 1989;40:178-179. |
| 8. | Evers BM. Small intenstine. Sabiston Textbook of Surgery. Philadelphia: Saunders 2008; 1318-1323. |
| 9. | Schnueriger B, Vorburger SA, Banz VM, Schoepfer AM, Candinas D. Diagnosis and management of the symptomatic duodenal diverticulum: a case series and a short review of the literature. J Gastrointest Surg. 2008;12:1571-1576. |
| 10. | Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology. 1983;85:538-547. |
| 11. | Wilcox RD, Shatney CH. Surgical implications of jejunal diverticula. South Med J. 1988;81:1386-1391. |
| 12. | Liu D, Chen L. Management of the total bowel diverticular disease. Hepatogastroenterology. 2009;56:1679-1682. |
| 13. | Veen M, Hornstra BJ, Clemens CH, Stigter H, Vree R. Small bowel diverticulitis as a cause of acute abdomen. Eur J Gastroenterol Hepatol. 2009;21:123-125. |
| 14. | Barnert J, Messmann H. Diagnosis and management of lower gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2009;6:637-646. |
| 15. | Rodriguez HE, Ziauddin MF, Quiros ED, Brown AM, Podbielski FJ. Jejunal diverticulosis and gastrointestinal bleeding. J Clin Gastroenterol. 2001;33:412-414. |
| 16. | Yahchouchy EK, Marano AF, Etienne JC, Fingerhut AL. Meckel's diverticulum. J Am Coll Surg. 2001;192:658-662. |
| 17. | Zani A, Eaton S, Rees CM, Pierro A. Incidentally detected Meckel diverticulum: to resect or not to resect? Ann Surg. 2008;247:276-281. |
| 18. | Zulfikaroglu B, Ozalp N, Zulfikaroglu E, Ozmen MM, Tez M, Koc M. Is incidental Meckel's diverticulum resected safely? N Z Med J. 2008;121:39-44. |
| 19. | Robijn J, Sebrechts E, Miserez M. Management of incidentally found Meckel's diverticulum a new approach: resection based on a Risk Score. Acta Chir Belg. 2006;106:467-470. |