Published online Feb 27, 2011. doi: 10.4240/wjgs.v3.i2.29
Revised: January 15, 2011
Accepted: January 21, 2011
Published online: February 27, 2011
A hiatal hernia can be classified as one of four types according to the position of the gastroesophageal (GE) junction and the extent of herniated stomach. Type I, or sliding hernias, account for up to 95% of all hiatal hernias and occur when the GE junction migrates into the posterior mediastinum through the hiatus. Type II occurs when the fundus herniates through the hiatus alongside a normally positioned GE junction. Type III is a combination of types I and II hernias with a displaced GE junction as well as stomach protruding through the hiatus. Type IV paraesophageal hernias are the rarest of the hiatal hernias. Usually, colon or small bowel is herniated within the mediastinum along with the stomach. We present a case of a paraesophageal hernia with the mid-body of the pancreas as part of the hernia contents.
- Citation: Coughlin M, Fanous M, Velanovich V. Herniated pancreatic body within a paraesophageal hernia. World J Gastrointest Surg 2011; 3(2): 29-30
- URL: https://www.wjgnet.com/1948-9366/full/v3/i2/29.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i2.29
A hiatal hernia can be classified as one of four types according to the position of the gastroesophageal (GE) junction and the extent of herniated stomach[1,2]. Type I, or sliding hernias, account for up to 95% of all hiatal hernias[3] and occur when the GE junction migrates into the posterior mediastinum through the hiatus. Types II-IV, paraesophageal hernias (PEH), together account for 5% of hiatal hernias[3]. Type II occurs when the fundus herniates through the hiatus alongside a normally positioned GE junction. Type III is a combination of types I and II hernias with a displaced GE junction as well as stomach protruding through the hiatus. Type IV is characterized by displacement of the stomach along with other organs into the chest.
We present an unusual case of a PEH containing the mid-body of the pancreas within the hernia sac.
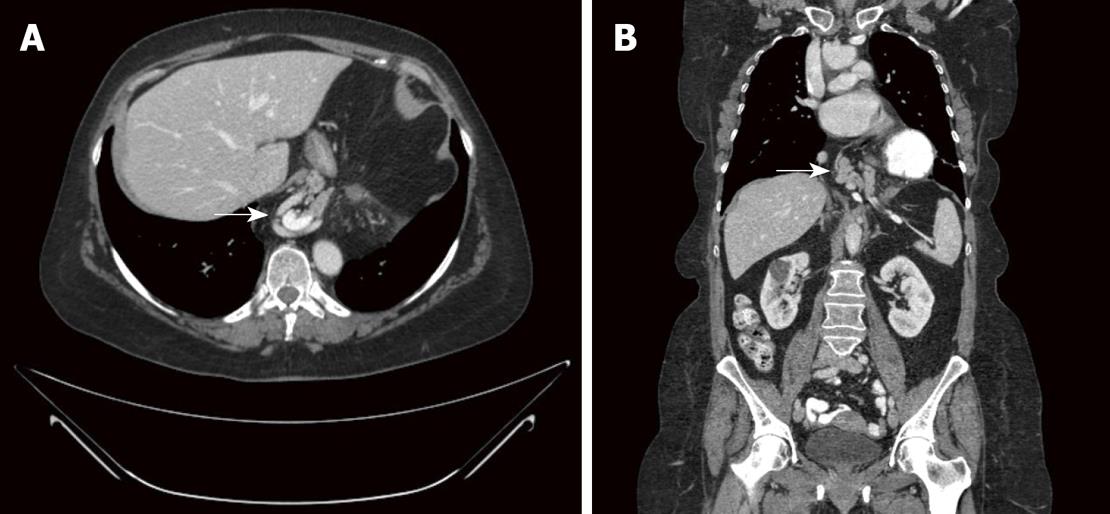
The patient is a 61-year old female with a past medical history of gastroesophageal reflux disease, peptic ulcer disease, breast cancer, and hyperthyroidism, who was referred to our clinic for elective repair of a paraesophageal hernia. She had symptoms of chest pressure and discomfort associated with occasional dysphagia, especially to solid foods, and occasional heartburn and regurgitation. This led to an initial evaluation with an upper endoscopy, which demonstrated a large paraesophageal hernia. A computed tomography scan showed an almost completely intrathoracic stomach with the mid-body of the pancreas herniated up through the hiatus (Figure 1A and B). The patient otherwise had no signs of gastric volvulus. Aside from mild epigastric tenderness on abdominal examination, her physical examination was normal.
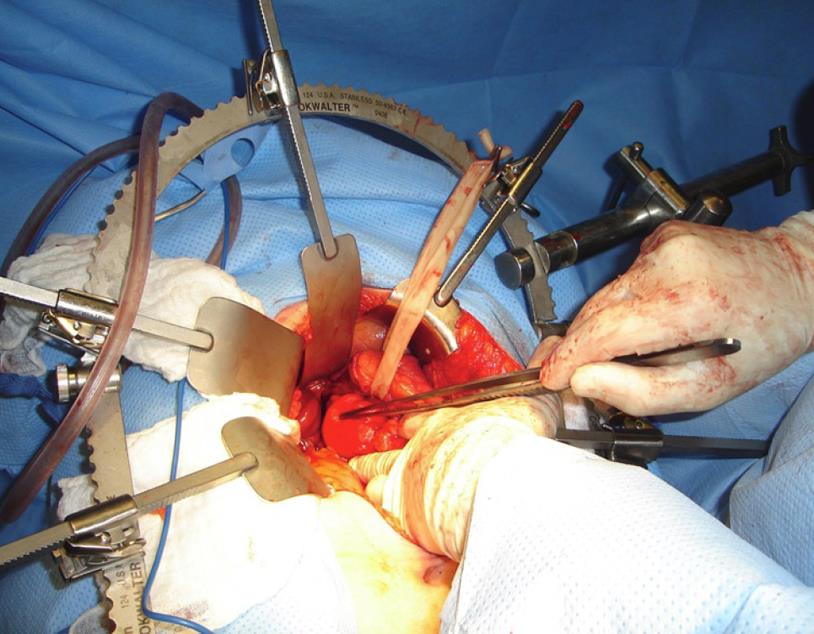
The patient was taken to the operating room for an elective paraesophageal hernia repair with Alloderm mesh and Nissen fundoplication. Upon exploration of the abdomen, a large paraesophageal hernia was found with the entire stomach rotated into the mediastinum in an organo-axial fashion. Posterior to the herniated stomach was the herniated pancreas (Figure 2). The hernia sac was dissected from the mediastinum and with this the stomach and pancreas were reduced into the abdomen and the hernia sac excised. The hiatal hernia was closed and the wrap performed.
The patient tolerated the procedure well. Her hospital course was uncomplicated. An esophagram on post-op day three was negative for leakage and the patient was put on a diet, which she tolerated. She was discharged home on post-op day four in good condition.
Type IV paraesophageal hernias are very rare, representing 5%-7% of all PEH[4]. The most cost common organ to accompany the stomach into the chest is the colon, most often the splenic flexure. Other more common organs include loops of the small bowel and omentum. It is extraordinarily rare for the pancreas to herniate in paraesophageal hernias, there being only five reported cases in the English literature. Most cases included the body and tail of the pancreas, with one case of the head of the pancreas herniating into the thorax. The majority were symptomatic[5-7]. Our case is unusual in that only the mid-body of the pancreas was herniated, not the tail and spleen.
It is controversial whether or not surgery is necessary for asymptomatic hiatal hernias, although it is agreed that surgery is the best choice for symptomatic PEH[3,8]. In asymptomatic patients, the potential risk of incarceration and strangulation is used by some as an indication for surgery[9]. Others claim that progression of symptoms is slow and seldom leads to emergency surgery, and therefore advocate a watchful approach for patients with large but asymptomatic PEH[10]. There is debate as to whether a transthoracic, transabdominal, or laparoscopic approach is best, but the underlying surgical principles for successful repair include reduction of hernia contents, removal of the hernia sac, closure of the hiatal defect, and an antireflux procedure.
Peer reviewers: Yan-Shen Shan, MD, PhD, Associate Professor, Department of Surgery, National Cheng Kung University Hospital, Sheng-Li Road 138, Tainan 70428, Taiwan, China; Shouji Shimoyama, MD, Gastrointestinal Unit, Settlement Clinic, 4-20-7, Towa, Adachi-ku, Tokyo 120-0003, Japan
S- Editor Wang JL L- Editor Hughes D E- Editor Liu N
| 1. | Mitiek M, Andrade R. Giant hiatal hernia. Ann Thorac Surg. 2010;89:S2168-S2173. |
| 2. | Awais O, Luketich JD. Management of giant paraesophageal hernia. Minerva Chir. 2009;64:159-168. |
| 3. | Shieman C, Grondin SC. Paraesophageal hernia: clinical presentation, evaluation, and management controversies. Thorac Surg Clin. 2009;19:473-484. |
| 4. | Grushka JR, Grenon SM, Ferri LE. A type IV paraesophageal hernia containing a volvulized sigmoid colon. Dis Esophagus. 2008;21:94-96. |
| 5. | Kafka N. Acute pancreatitis secondary to incarcerated paraesophageal hernia. Surgery. 1994;15:653-655. |
| 6. | Katz M. Asymptomatic diaphragmatic hiatal herniation of the pancreas. J Comput Assist Tomogr. 2002;26:524-525. |
| 7. | Chevallier P, Peten E, Pellegrino C, Souci J, Motamedi JP, Padovani B. Hiatal hernia with pancreatic volvulus: a rare case of acute pancreatitis. AJR. 2001;177:373-374. |
| 8. | Velanovich V, Karmy-Jones R. Surgical management of paraesophageal hernias: Outcome and quality of life analysis. Dig Surg. 2001;18:432-438. |
| 9. | Sihvo EI, Salo JA, Räsänen JV, Rantanen TK. Fatal complications of adult paraesophageal hernia: A population-based study. J Thorac Cardiovasc Surg. 2009;137:419-424. |