Published online Oct 27, 2011. doi: 10.4240/wjgs.v3.i10.142
Revised: September 20, 2011
Accepted: September 26, 2011
Published online: October 27, 2011
While laparoscopic colon surgery has been established to some degree over this decade, laparoscopic rectal surgery is not standard yet because of the difficulty of making a clear surgical field, the lack of precise anatomy of the pelvis, immature procedures of rectal transaction and so on. On the other hand, maintaining a clear surgical field via the magnified laparoscopy may allow easier mobilization of the rectum as far as the levetor muscle level and may result less blood loss and less invasiveness. However, some unique techniques to keep a clear surgical field and knowledge about anatomy of the pelvis are required to achieve the above superior operative outcomes. This review article discusses how to keep a clear operative field, removing normally existing abdominal structures, and how to transact the rectum and restore the discontinuity based on anatomical investigations. According to this review, laparoscopic rectal surgery will become a powerful modality to accomplish a more precise procedure which has been technically impossible so far, actually entering a new era.
- Citation: Fukunaga Y. Superiority of laparoscopic rectal surgery: Towards a new era. World J Gastrointest Surg 2011; 3(10): 142-146
- URL: https://www.wjgnet.com/1948-9366/full/v3/i10/142.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i10.142
Since its advent in 1991[1], laparoscopic colonic resection has drawn much interest worldwide and many modifications and improvements have been reported[2-7], yielding great benefits for the patients involved. Over the last decade, several reports on randomized controlled trials have been published around the world which provide evidence for equivalence between laparoscopic and open surgery in the treatment of colon cancer[8-13]. However, all of these studies were limited to the colon, sigmoid colon or right side of the colon, with none comparing these techniques for cancer of the rectum. On the other hand, recent studies have focused on laparoscopic surgery for rectal cancer. While some of these studies have investigated laparoscopic surgery for colon cancer, a number of single-institute, cohort studies have focused on the advantages of this technique in rectal surgery[14-17]. Evidence for the visual superiority that this technique affords through the use of optical instruments, however, has so far been based on the experience of individual surgeons and none from multicenter, randomized, control trials is yet available. Rectal surgery must be considered in relationship to oncological care, regardless of the technique used, and much attention now is paid to increasing operative safety and outcomes in terms of such care. For a long time now, much effort has gone into improving techniques so as to avoid impairment of urinary, sexual and anal function following rectal cancer surgery[18-23].
Preservation of the anus is the biggest hope of most rectal cancer patients, making this the biggest priority among surgeons too. One purely surgical development in this respect is the indication for intersphincteric resection in cases of very low rectal cancer located close to the dentate line[24-26]. Neoadjuvant chemo-radio therapy is also used to preserve the anus and for local control[27,28]. In this editorial, I would like to consider the potential of laparoscopic surgery in overcoming such difficulties and providing improved outcomes.
Laparoscopy offers superb visualization of the pelvis. However, there is still a need for new procedures for removal of the small bowel, sigmoid colon, ovary and uterus. The Trendelenburg position is necessary for removal of the small bowel and a variety of techniques are required for retraction of the sigmoid colon. The magnification offered by the laparoscope allows the surgeon a clear view of the inner regions of the pelvis. There is no doubt that this enhanced view in combination with fundamental investigation allows more precise anatomical recognition, as will be described later. A number of reports have been published on the relationship between the anatomy of the pelvis and rectal surgery. Kinugasa et al[29-31] investigated surgical planes in the anterior and posterior aspects of the pelvis using fresh cadaver specimens. While some later studies concurred with Kinugasa regarding the posterior plane, others did not and the matter remains controversial[32,33]. In a study on the fascial structures posterolateral to the rectum, Kinugasa reported the existence of a provisionally termed “pre-HGN fascia” between the fascia propria of the rectum (FPR) and the parietal presacral fascia covering HGN. This pre-HGN fascia lies very close to the FPR and is so thin that it appears almost contiguous with the FPR at the third and fourth sacral vertebrae. He also stated that use of a surgical plane on the parietal presacral fascia runs the risk of injury to the pelvic plexus, presacral vein and other structures. This hypothesis, however, remains unverified and in the procedure for total mesorectal excision advocated by Heald et al[34], mobilization on this plane is the norm due to difficulties in separating the FPR and pre-HGN fascia. Separation of these planes would result in injury to the FPR, making this unacceptable in terms of oncological safety.
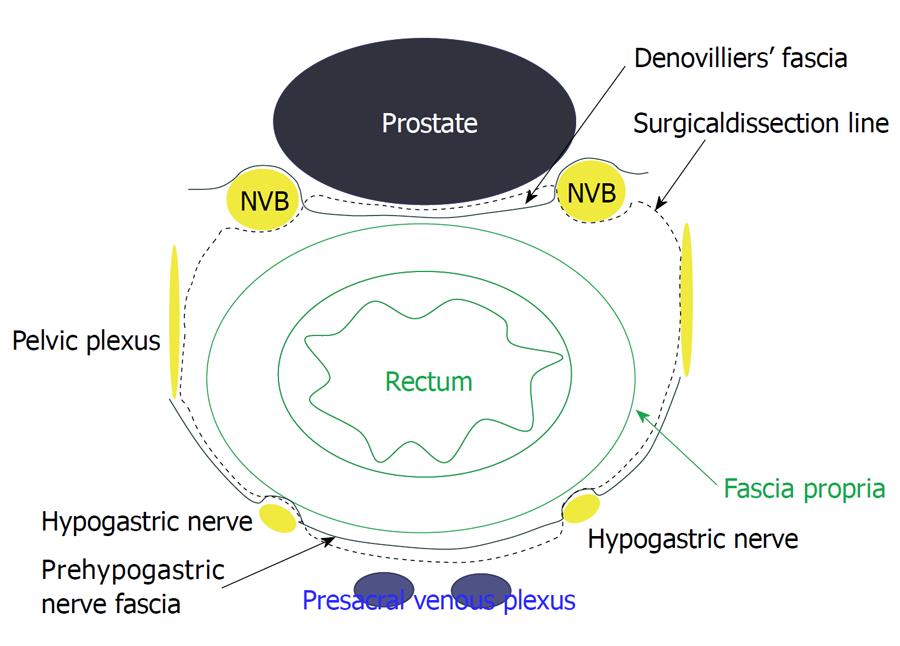
In contrast, anterior to the rectum, the structures of Denonvillier’s fascia and its relationship with the FPR have been investigated in many studies[32,33]. Although Denonvillier’s fascia is used in descriptions of operative surgery, confusion exists with regard to the precise relationship between Denonvillier’s fascia and the FPR. Lindsey et al[32] proposed three possible surgical planes for anterior resection in total mesorectal excision according to circumferential tumor location. He also stated that the Denonvilliers’ fascia should be left on the prostate and seminal vesicles during routine anatomic anterior resection. In some cases in which the tumor is located on the anterior or circumferential rectum, this plane should be resected with the specimen. Kinugasa et al[29] also advocated leaving Denonvilliers’ fascia on the prostate and seminal vesicles, citing improved safety in terms of preservation of autonomic nerves in the pelvis. When the surgical dissection plane is placed anterior to the Denonvilliers’ fascia, this plane continues anterior to the neurovascular bundles and pelvic plexus (Figure 1).
Double stapling technique is now the standard method for reconstruction after rectal resection and most low rectal cancer patients are candidates for anus-preserving surgery using this technique[35]. Even in open surgery, anastomotic leakage is the most feared and difficult complication for both surgeon and patient. Generally speaking, the rate of anastomotic leakage with double stapling technique in open rectal surgery is 8%-10%[36,37]. Nobody knows how this compares with the leakage rate with laparoscopic surgery in such cases. However, during the early days of laparoscopic surgery, it has to be admitted that inexperience with this approach may have meant that rectal transaction was not carried out in a satisfactory environment in many cases. The use of multiple stapling cartridges for transaction implies that the rectum is divided, resulting in poor sealing and compromised vascular supply to the stump[17]. Some studies have reported the experiences of individual surgeons and the techniques employed for transaction of the rectum with less than two cartridges[38,39]. Conventional devices employed in open surgery have been used for transaction of the rectum under pneumoperitoneum[38,40]. Some recent reports advocate the use of an endostapler in pure laparoscopic surgery for transaction of the rectum[39,41]. A number of studies, not limited to laparoscopic surgery, have reported risk factors for anastomotic leakage in rectal cancer surgery[42-47] and these have included the degree of anastomosis, age, male sex, smoking, diabetes, cardiovascular disease, obesity and preoperative radiochemotherapy among others. It has yet to be shown that laparoscopic surgery yields a lower rate of anastomotic leakage than open surgery. However, there is no doubt that laparoscopic rectal surgery provides a magnified field of view, allowing a more accurate and finer technique, even in the very narrow and deep confines of the pelvis, resulting in more favorable outcomes than open surgery.
Rectal washout before transaction to avoid increase in anastomotic recurrence is another issue related to this technique. Maeda et al[48] reported the importance of rectal wash out before transaction of the rectum in cancer patients. On the other hand, some reports have argued against rectal wash out, even in cancer patients[49-51]. Despite no objective evidence that rectal wash out decreases anastomotic recurrence, this entity after double stapling technique has been approved. Rectal wash out before transaction may even be possible with new and unique laparoscopic procedures, even for very low level tumors[38,52].
Recent studies have reported intersphincteric resection for low rectal cancer, even in cases where hand-sewn anastomosis via the anus is necessary. This technique was reported in the early 1990s in open surgery[24-26]. Since then, short-term outcomes, including anal function, and long-term outcomes, according to the spread of indications for advanced cancer, have been discussed. How far partial or total intersphincteric resection is required from the anal verge may influence postoperative bowel habits. Such factors may play an important role from an oncological viewpoint as well. This operation has been tried laparoscopically in recent studies[53-58]. Magnification of the lower pelvis allows safe and easy mobilization of the rectum as far as the levator muscle or the intersphincteric space from the abdominal side. Once this ultra-low mobilization of the rectum has been carried out from the anterior side, per-anum dissection of the rectum can easily performed while partially preserving the internal or external sphincter. Local recurrence is another factor that must be taken into consideration with this procedure, especially with the laparoscopic approach. The rate of local recurrence after this operation has been reported to be approximately 2.5%[59] to 10%[60], and may be influenced by the stage of the primary rectal cancer. Is the laparoscopic approach for this operation beneficial? Some authors maintain that abdominal laparoscopic dissection of the rectum via the abdomen allows better magnification of the surgical field than anal dissection[61,62].
In using this technique for advanced rectal cancer, especially by laparoscopy, rate of local recurrence remains an unsolved issue. Saito et al[60] reported that most cases of local recurrence were histological T3.
Laparoscopic rectal surgery is now entering a new era and many case-matched control studies and new technical trials are under way. To achieve technically safe and oncologically sufficient outcomes, the magnification of anatomy that laparoscopy allows will play an important role in the further development of surgical expertise.
Peer reviewer: Zenichi Morise, MD, PhD, Department of Surgery, Fujita Health University School of Medicine, 1-98 Dengakugakubo Kutsukakecho, Toyoake Aichi 470-1192, Japan
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
| 1. | Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1:144-150. [PubMed] |
| 2. | Wexner SD, Johansen OB, Nogueras JJ, Jagelman DG. Laparoscopic total abdominal colectomy. A prospective trial. Dis Colon Rectum. 1992;35:651-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 158] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Van Ye TM, Cattey RP, Henry LG. Laparoscopically assisted colon resections compare favorably with open technique. Surg Laparosc Endosc. 1994;4:25-31. [PubMed] |
| 4. | Franklin ME, Rosenthal D, Norem RF. Prospective evaluation of laparoscopic colon resection versus open colon resection for adenocarcinoma. A multicenter study. Surg Endosc. 1995;9:811-816. [PubMed] |
| 5. | Milsom JW, Okuda J, Kim SH, Shore GI, Wilson JE. Atraumatic and expeditious laparoscopic bowel handling using a new endoscopic device. Dis Colon Rectum. 1997;40:1394-1395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Konishi F, Okada M, Nagai H, Ozawa A, Kashiwagi H, Kanazawa K. Laparoscopic-assisted colectomy with lymph node dissection for invasive carcinoma of the colon. Surg Today. 1996;26:882-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Lacy AM, García-Valdecasas JC, Delgado S, Sabater L, Grande L, Fuster J, Visa J. Unusual intraoperative complication in laparoscopic sigmoidectomy. Surg Endosc. 1998;12:448-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA. 2002;287:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 540] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 9. | Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1901] [Cited by in RCA: 1816] [Article Influence: 79.0] [Reference Citation Analysis (0)] |
| 10. | Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363:1187-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 707] [Cited by in RCA: 656] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 11. | Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2517] [Article Influence: 119.9] [Reference Citation Analysis (0)] |
| 12. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2298] [Article Influence: 114.9] [Reference Citation Analysis (0)] |
| 13. | Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1112] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 14. | Morino M, Parini U, Giraudo G, Salval M, Brachet Contul R, Garrone C. Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg. 2003;237:335-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 221] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 15. | Hartley JE, Mehigan BJ, Qureshi AE, Duthie GS, Lee PW, Monson JR. Total mesorectal excision: assessment of the laparoscopic approach. Dis Colon Rectum. 2001;44:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 141] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Leroy J, Jamali F, Forbes L, Smith M, Rubino F, Mutter D, Marescaux J. Laparoscopic total mesorectal excision (TME) for rectal cancer surgery: long-term outcomes. Surg Endosc. 2004;18:281-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 281] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 17. | Kim SH, Park IJ, Joh YG, Hahn KY. Laparoscopic resection of rectal cancer: a comparison of surgical and oncologic outcomes between extraperitoneal and intraperitoneal disease locations. Dis Colon Rectum. 2008;51:844-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Sugihara K, Moriya Y, Akasu T, Fujita S. Pelvic autonomic nerve preservation for patients with rectal carcinoma. Oncologic and functional outcome. Cancer. 1996;78:1871-1880. [PubMed] |
| 19. | Havenga K, Enker WE, McDermott K, Cohen AM, Minsky BD, Guillem J. Male and female sexual and urinary function after total mesorectal excision with autonomic nerve preservation for carcinoma of the rectum. J Am Coll Surg. 1996;182:495-502. [PubMed] |
| 20. | Nesbakken A, Nygaard K, Bull-Njaa T, Carlsen E, Eri LM. Bladder and sexual dysfunction after mesorectal excision for rectal cancer. Br J Surg. 2000;87:206-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 198] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 21. | Quah HM, Jayne DG, Eu KW, Seow-Choen F. Bladder and sexual dysfunction following laparoscopically assisted and conventional open mesorectal resection for cancer. Br J Surg. 2002;89:1551-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 213] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 22. | Jayne DG, Brown JM, Thorpe H, Walker J, Quirke P, Guillou PJ. Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg. 2005;92:1124-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 277] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 23. | Asoglu O, Matlim T, Karanlik H, Atar M, Muslumanoglu M, Kapran Y, Igci A, Ozmen V, Kecer M, Parlak M. Impact of laparoscopic surgery on bladder and sexual function after total mesorectal excision for rectal cancer. Surg Endosc. 2009;23:296-303. [PubMed] |
| 24. | Braun J, Treutner KH, Winkeltau G, Heidenreich U, Lerch MM, Schumpelick V. Results of intersphincteric resection of the rectum with direct coloanal anastomosis for rectal carcinoma. Am J Surg. 1992;163:407-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Schiessel R, Karner-Hanusch J, Herbst F, Teleky B, Wunderlich M. Intersphincteric resection for low rectal tumours. Br J Surg. 1994;81:1376-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 320] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 26. | Teramoto T, Watanabe M, Kitajima M. Per anum intersphincteric rectal dissection with direct coloanal anastomosis for lower rectal cancer: the ultimate sphincter-preserving operation. Dis Colon Rectum. 1997;40:S43-S47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731-1740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4342] [Cited by in RCA: 4462] [Article Influence: 212.5] [Reference Citation Analysis (1)] |
| 28. | Madoff RD. Chemoradiotherapy for rectal cancer--when, why, and how? N Engl J Med. 2004;351:1790-1792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Kinugasa Y, Murakami G, Uchimoto K, Takenaka A, Yajima T, Sugihara K. Operating behind Denonvilliers' fascia for reliable preservation of urogenital autonomic nerves in total mesorectal excision: a histologic study using cadaveric specimens, including a surgical experiment using fresh cadaveric models. Dis Colon Rectum. 2006;49:1024-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Kinugasa Y, Murakami G, Suzuki D, Sugihara K. Histological identification of fascial structures posterolateral to the rectum. Br J Surg. 2007;94:620-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 31. | Kinugasa Y, Niikura H, Murakami G, Suzuki D, Saito S, Tatsumi H, Ishii M. Development of the human hypogastric nerve sheath with special reference to the topohistology between the nerve sheath and other prevertebral fascial structures. Clin Anat. 2008;21:558-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Lindsey I, Warren BF, Mortensen NJ. Denonvilliers' fascia lies anterior to the fascia propria and rectal dissection plane in total mesorectal excision. Dis Colon Rectum. 2005;48:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Zhai LD, Liu J, Li YS, Yuan W, He L. Denonvilliers' fascia in women and its relationship with the fascia propria of the rectum examined by successive slices of celloidin-embedded pelvic viscera. Dis Colon Rectum. 2009;52:1564-1571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982;69:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1985] [Cited by in RCA: 1935] [Article Influence: 45.0] [Reference Citation Analysis (1)] |
| 35. | Feinberg SM, Parker F, Cohen Z, Jamieson CG, Myers ED, Railton RH, Langer B, Stern HS, McLeod RS. The double stapling technique for low anterior resection of rectal carcinoma. Dis Colon Rectum. 1986;29:885-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Vignali A, Fazio VW, Lavery IC, Milsom JW, Church JM, Hull TL, Strong SA, Oakley JR. Factors associated with the occurrence of leaks in stapled rectal anastomoses: a review of 1,014 patients. J Am Coll Surg. 1997;185:105-113. [PubMed] |
| 37. | Detry RJ, Kartheuser A, Delriviere L, Saba J, Kestens PJ. Use of the circular stapler in 1000 consecutive colorectal anastomoses: experience of one surgical team. Surgery. 1995;117:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Fukunaga Y, Higashino M, Tanimura S, Takemura M, Fujiwara Y, Osugi H. New technique for rectal division in laparoscopic anterior resection--with video. World J Surg. 2008;32:2095-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Yamaguchi T, Muto T. Standardized technique of laparoscopic intracorporeal rectal transection and anastomosis for low anterior resection. Surg Endosc. 2008;22:557-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 40. | Ishii Y, Hasegawa H, Nishibori H, Endo T, Kitajima M. The application of a new stapling device for open surgery (Contour Curved Cutter Stapler) in the laparoscopic resection of rectal cancer. Surg Endosc. 2006;20:1329-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Ito M, Sugito M, Kobayashi A, Nishizawa Y, Tsunoda Y, Saito N. Relationship between multiple numbers of stapler firings during rectal division and anastomotic leakage after laparoscopic rectal resection. Int J Colorectal Dis. 2008;23:703-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 201] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 42. | Konishi T, Watanabe T, Kishimoto J, Nagawa H. Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg. 2006;202:439-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 201] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 43. | Lipska MA, Bissett IP, Parry BR, Merrie AE. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006;76:579-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 201] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 44. | Jung SH, Yu CS, Choi PW, Kim DD, Park IJ, Kim HC, Kim JC. Risk factors and oncologic impact of anastomotic leakage after rectal cancer surgery. Dis Colon Rectum. 2008;51:902-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 192] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 45. | Law WI, Chu KW, Ho JW, Chan CW. Risk factors for anastomotic leakage after low anterior resection with total mesorectal excision. Am J Surg. 2000;179:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 268] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 46. | Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM, Tang R. Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg. 2005;241:9-13. [PubMed] |
| 47. | Xiao L, Zhang WB, Jiang PC, Bu XF, Yan Q, Li H, Zhang YJ, Yu F. Can transanal tube placement after anterior resection for rectal carcinoma reduce anastomotic leakage rate? A single-institution prospective randomized study. World J Surg. 2011;35:1367-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 48. | Maeda K, Maruta M, Hanai T, Sato H, Horibe Y. Irrigation volume determines the efficacy of "rectal washout". Dis Colon Rectum. 2004;47:1706-1710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 49. | Agaba EA. Does rectal washout during anterior resection prevent local tumor recurrence? Dis Colon Rectum. 2004;47:291-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 50. | Terzi C, Unek T, Sağol O, Yilmaz T, Füzün M, Sökmen S, Ergör G, Küpelioğlu A. Is rectal washout necessary in anterior resection for rectal cancer? A prospective clinical study. World J Surg. 2006;30:233-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 51. | Constantinides VA, Cheetham D, Nicholls RJ, Tekkis PP. Is rectal washout effective for preventing localized recurrence after anterior resection for rectal cancer? Dis Colon Rectum. 2008;51:1339-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 52. | Fukunaga Y, Higashino M, Tanimura S, Nishiguchi Y, Kishida S, Nishikawa M, Ogata A, Osugi H. A novel laparoscopic technique for stapled colon and rectal anastomosis. Tech Coloproctol. 2003;7:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 53. | Watanabe M, Teramoto T, Hasegawa H, Kitajima M. Laparoscopic ultralow anterior resection combined with per anum intersphincteric rectal dissection for lower rectal cancer. Dis Colon Rectum. 2000;43:S94-S97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 80] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 54. | Rullier E, Sa Cunha A, Couderc P, Rullier A, Gontier R, Saric J. Laparoscopic intersphincteric resection with coloplasty and coloanal anastomosis for mid and low rectal cancer. Br J Surg. 2003;90:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 133] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 55. | Uchikoshi F, Nishida T, Ueshima S, Nakahara M, Matsuda H. Laparoscope-assisted anal sphincter-preserving operation preceded by transanal procedure. Tech Coloproctol. 2006;10:5-9; discussion 9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 56. | Orsenigo E, Di Palo S, Vignali A, Staudacher C. Laparoscopic intersphincteric resection for low rectal cancer. Surg Oncol. 2007;16 Suppl 1:S117-S120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 57. | Sakakura C, Nishio M, Miyagawa K, Miyashita A, Nagata H, Kin S, Fukuda K, Nakase Y, Hagiwara A, Nakanishi M. Laparoscope-assisted superlow anterior resection combined with inter sphincteric rectal dissection for very low advanced rectal cancers combined with preoperative chemotherapy. Hepatogastroenterology. 2009;56:692-695. [PubMed] |
| 58. | Fujimoto Y, Oya M, Kuroyanagi H, Ueno M, Yamaguchi T, Muto T. Laparoscopic assisted intersphincteric resection following preoperative chemoradiation therapy for locally advanced lower rectal cancer: report of a case. Hepatogastroenterology. 2009;56:378-380. [PubMed] |
| 59. | Yamada K, Ogata S, Saiki Y, Fukunaga M, Tsuji Y, Takano M. Long-term results of intersphincteric resection for low rectal cancer. Dis Colon Rectum. 2009;52:1065-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 60. | Saito N, Sugito M, Ito M, Kobayashi A, Nishizawa Y, Yoneyama Y, Nishizawa Y, Minagawa N. Oncologic outcome of intersphincteric resection for very low rectal cancer. World J Surg. 2009;33:1750-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 61. | Elshazly WG, Farouk M, Samy M. Preoperative concomitant radiotherapy with oral capecitabine in advanced rectal cancer within 6 cm from anal verge. Int J Colorectal Dis. 2009;24:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 62. | Weiser MR, Quah HM, Shia J, Guillem JG, Paty PB, Temple LK, Goodman KA, Minsky BD, Wong WD. Sphincter preservation in low rectal cancer is facilitated by preoperative chemoradiation and intersphincteric dissection. Ann Surg. 2009;249:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 183] [Article Influence: 11.4] [Reference Citation Analysis (0)] |