Published online Jun 27, 2010. doi: 10.4240/wjgs.v2.i6.224
Revised: March 31, 2010
Accepted: April 7, 2010
Published online: June 27, 2010
Natural orifice translumenal endoscopic surgery (NOTES) training is unique in that it crosses specialty lines and most practitioners do not possess both the knowledge and skill to perform the procedures in their current form. The learning process becomes even more complex because the field is in constant evolution with advances in technology and technique being introduced almost daily! The challenges of learning NOTES illustrates a larger problem in all procedurally based medical specialties today-the pace of change has become so rapid that a practicing physician’s technical skills become out of date within five to ten years of completing residency or fellowship training. As a result, practicing physicians must develop a strategy to rapidly learn about a new technique or technology and introduce it safely into their practice while satisfying the concerns of their hospital’s credentialing committee. This chapter will explore the options for learning new procedures and discuss the rapidly expanding armamentarium of education institutes and the developing technology to measure procedural competence.
- Citation: Dunkin BJ. Natural orifice transluminal endoscopic surgery: Educational challenge. World J Gastrointest Surg 2010; 2(6): 224-230
- URL: https://www.wjgnet.com/1948-9366/full/v2/i6/224.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v2.i6.224
In 1989 Dr. Eddie Joe Reddick became the first surgeon in the US to remove a diseased gallbladder from a patient using a miniaturized camera system, long narrow instruments and four half inch incisions in the abdominal wall. This new technique of laparoscopic surgery would revolutionize abdominal and thoracic surgery forever. Within three years nearly all general surgeons in the US would move from performing gallbladder surgery using an open technique (a term never used before the era of laparoscopy) to laparoscopic surgery. Most had never even seen a laparoscopic procedure before, much less used the technique to perform a complex operation. This created an unprecedented demand for new procedure training in surgery. Nearly overnight practicing surgeons needed to learn an entirely new set of surgical skills and offer them to their patients in a safe manner. As predicted, there was significant variation in the types of training experiences offered and, unfortunately, some patients suffered complications from undergoing operations by inadequately prepared surgeons.
In 2004, Kalloo et al[1] reported on a series of transgastric peritoneoscopies done in a porcine model-a procedure to be later termed natural orifice translumenal endoscopic surgery (NOTES). That same year Reddy and Rao presented a video of the first human transgastric appendectomy at the Annual Conference of the Society of Gastrointestinal Endoscopy of India[2]. As with the laparoscopy revolution, the introduction of NOTES caused a stir among general surgeons and many scrambled to learn more in anticipation of the next possible wave of minimally invasive surgery. Interestingly, a subgroup of advanced therapeutic gastroenterologists was also intrigued by this new field and equally interested in learning more. By 2005 the first NOTES hands-on training course was conducted at Case Western Reserve School of Medicine in Cleveland, Ohio despite the fact that only one human case had been done in the world! Multiple courses followed both in the US and Europe.
NOTES training is unique in that it crosses specialty lines (general and thoracic surgery, gynecology, gastroenterology) and most practitioners do not possess both the knowledge and skill to perform the procedures in their current form. The flexible endoscopy instruments used in NOTES are not familiar to most surgeons while surgical technique and procedures are not familiar to most gastroenterologists. Adding unique points of access such as transvaginal, transcolonic or transesophageal further adds to the learning curve and the whole process becomes even more complex because the field is in constant evolution with advances in technology and technique being introduced almost daily!
The challenges of learning NOTES illustrates a larger problem in all procedurally based medical specialties today-the pace of change has become so rapid that a practicing physician’s technical skills become out of date within five to ten years of completing residency or fellowship training. As a result, practicing physicians must develop a strategy to rapidly learn about a new technique or technology and introduce it safely into their practice while satisfying the concerns of their hospital’s credentialing committee. This chapter will explore the options for learning new procedures and discuss the rapidly expanding armamentarium of education institutes and the developing technology to measure procedural competence.
The introduction of laparoscopic cholecystectomy fostered the development of a myriad of educational programs focused on helping practicing surgeons to learn this new technique and begin performing these procedures. The experience from course to course was variable but a model of presenting didactic material coupled with live demonstration of technique followed by rehearsal in an inanimate or animate model was established. With time and standardization of the laparoscopic cholecystectomy technique, surgeons successfully transitioned to this new mode of surgery.
Training to learn NOTES is different from laparoscopy. When laparoscopic cholecystectomy was introduced, surgeons had expert knowledge about the disease process they were treating and the goals of the surgical procedure. Even the laparoscopic instruments looked like long extensions of open ones. Thus they only had to focus on the technical aspects of this new mode of entry into the abdominal cavity. In a NOTES cholecystectomy, the surgeon again has expert knowledge of the disease process but use of the flexible endoscopic tools is more challenging than in laparoscopy. Now, not only does the surgeon have to learn about the variety of flexible tools but he must also master advanced flexible endoscopy just to deliver these tools to their target location. The tools and the endoscope are also linked which makes manipulation of both difficult to coordinate and results in relying on an assistant more than with most procedures. If transvaginal access is added to the procedure, a whole new understanding of anatomy must be mastered as well.
The gastroenterologist is equally challenged by NOTES. He or she has an advantage when manipulating the endoscope and flexible tools but does not have mastery of surgical principles, technique and anatomy which may have a longer learning curve than the technical issues facing a surgeon. In addition, the gastroenterologist is unaccustomed to working under sterile conditions in the operating room environment and potentially spending a number of hours to perform a single procedure. Alternative access points-such as the transvaginal route-are as equally unfamiliar as they are to the general surgeon.
Finally, both surgeons and gastroenterologists are handicapped in learning NOTES because of the rapid pace of change in the field. Laparoscopic cholecystectomy was disseminated to the majority of general surgeons once the technique had become standardized. In fact, the natural evolution of minimally invasive procedures is to standardize the technique which often results in eventually moving them out of a surgical environment and into another procedure area in the hospital. Percutaneous endoscopic gastrostomy (PEG) tube placement is an excellent example of this evolution having first been performed in the operating room but now done in the endoscopy unit or even at the patient’s bedside. The technology and technique of NOTES is evolving so quickly that it is impossible to settle on a standard approach for a particular procedure. As a result, what is learned and even mastered today may not apply tomorrow.
Having identified the challenges for a practicing surgeon to learn a new technique or technology, let us review current options for accomplishing this. The first option is to attend a “continuing medical education (CME)-type” event. CME programs are learning opportunities designed to enhance the knowledge and skills of practicing physicians in their care of patients. A surgeon attending such a program is granted CME credits. These credits document the number of hours the surgeon committed to the activity and are designed to track this type of effort for purposes of reporting to credentialing bodies such as state licensing boards and medical specialty boards. While CME requirements are a motivational element to encourage surgeons to continually update their knowledge and skills, they are a poor mechanism for gaining procedural competence. The credits usually reflect attendance only and are not an accurate measure of knowledge or skill. There is also variable acceptance of CME credits alone as an indication of procedural competence by hospital credentialing bodies.
As a result, many surgeons follow attendance of a CME-type activity with a preceptorship. A preceptor is a coach in an educational relationship who structures the learning process to achieve a set of formally identified skills. A role model and teacher, the preceptor operates in an environment that closely resembles the normal work setting for the learner. There are three types of preceptorships[3]. The first is an experience where the preceptor comes to the learner’s institution to help perform the operation. This is the most efficient method of transferring skill because the preceptor can help guide the learner surgeon through the procedure on their own patient working with their own operative team and in their own hospital. The entire operative team learns during this experience and system-based barriers to the procedure can be identified and corrected. It is also convenient for the patient. Despite these advantages, there are significant barriers to this type of preceptorship. First, the preceptor may be limited in his or her ability to direct or even take over the procedure. This is because of potential limitations in gaining privileges at the host institution to “scrub-in” to the case. Such a limitation is more concerning when the legal community may view the preceptor as the most qualified person in the operating room and thus responsible for the outcome of the procedure which in turn leads to questions of malpractice liability. Also, many institutions require state licensure for even temporary privileges-a process that can take many months and significant commitment to accomplish. Finally, the ability for a preceptor to teach at institutions outside of their own is limited and disruptive to their own surgical practice.
A second type of preceptorship involves the learner visiting the preceptor’s institution. This has the advantage of allowing the preceptor complete control of the case without exposing them to unusual privileging, licensing or malpractice issues. The down side is that most of the challenges put on the preceptor in the first model are now shifted to the learner. There are also issues about patient travel if the learner wants to operate on his own case, and ensuring continuity of the postoperative follow-up.
The third and most effective method of preceptorship is a mini fellowship. Such fellowships offer the most structured experience with time for the preceptor to monitor progress and ensure successful transfer of skills. The obvious disadvantage is that the learner must leave their practice for a significant period of time. There are also obstacles with licensing, privileging and malpractice. Finally, the learner may interfere with the training of residents and fellows at the preceptor’s institution.
What are most needed in surgical training are objective measures of procedural competence. A practicing surgeon would benefit most by being able to spend a short, concentrated, well structured period of time at an educational institute learning a new procedure and walk away from the experience with a validated objective measure of his or her skills that could be used to convince a credentialing body that they are now prepared to perform that procedure at their home institution. A number of developments are occurring to move surgical education closer to this goal.
One of the most basic advances in surgical training is the development of a new classification system which will give credentialing bodies a better understanding of the type of educational activity in which a surgeon has engaged. The American College of Surgeons developed the System for Verification of Knowledge and Skills which has five levels. A Level I educational event simply requires verification of attendance-much like CME. Level II requires verification of satisfactory completion of course objectives usually done by having the learner take a didactic examination. Level III requires verification of knowledge and skills which, to date, has been accomplished by using a combination of a written examination coupled with evaluation of skills by an expert proctor in a hands-on laboratory experience. Level IV requires verification of a preceptorial experience and Level V requires verification of satisfactory patient outcomes. This classification system clarifies the degree of training and will help credentialing bodies better understand a surgeons credentials and set standards for allowing a performance of new procedures.
Another advance in surgical training is the development of objective measures of knowledge and skill in basic laparoscopy. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has developed a program called the fundamentals of laparoscopic surgery (FLS) which is a training and verification program for laparoscopic surgery. FLS includes on-line didactic material covering the fundamental knowledge-base required for any surgeon performing laparoscopy or thoracoscopy. It also entails a written examination as well as a hands-on skills test using the McGill Inanimate System for Training and Evaluation of Laparoscopic Skills (MISTELS) physical laparoscopy simulator. The MISTELS simulator consists of five exercises performed in a trainer box. A camera and LED lighting system provide visualization and the surgeon works through two trocars placed in fixed positions through an opaque cover on top of the box (Figure 1). The system was designed to be inexpensive and easily portable so that it could be used at home for practice. FLS has gone through extensive testing to prove reliability and validity and is the first commercially available program which provides a benchmark for knowledge and skills in a surgical technique[4]. Because of the validation work that has been done on FLS, it has withstood the scrutiny of a high stakes exam and is now required by the American Board of Surgery (ABS) to become Board certified. SAGES has partnered with the American College of Surgeons and industry to provide FLS testing at no charge for every graduating general surgery resident in the US.
Following closely on the heels of FLS is another SAGES program called the Fundamentals of Endoscopic Surgery (FES). FES is modeled after FLS as a validated training and testing program of knowledge and skills in flexible gastrointestinal (GI) endoscopy. Like FLS, FES consists of web-based didactic material covering the fundamental knowledge required to perform flexible endoscopy as well as a written exam and a hands-on skills test. Because there is no equivalent of the MISTELS trainer for flexible endoscopy, the FES task force chose to use a computer based simulation platform for the hands-on skills test. There are five skills sets for FES including endoscope navigation, loop reduction, mucosal evaluation and targeting. FES is currently undergoing rigorous reliability and validity testing and will be rolled out at the SAGES annual meeting in April 2010. Once validated, it is expected that FES will take its place alongside FLS as another requirement by the American Board of Surgery to become certified.
While validated simulator training and testing is important, meaningful measures of real clinical performance are crucial to verifying that a practicing surgeon has the skills that he or she say they have. Validated clinical measures of procedure performance are also required to demonstrate that simulator training has a positive effect on clinical performance. Such an effect is called predictive validity in that performance on the simulator predicts performance in the real clinical domain. Predictive validity is the “Holy Grail” of simulation technology but is missing for almost all current surgical simulators. While developing FES it was envisioned that predictive validity would be a crucial component to its evaluation. As a result, the FES Task Force developed and validated a clinical assessment tool for GI endoscopy called GAGES-the Global Assessment of Gastrointestinal Endoscopic Skills. GAGES was developed by expert endoscopists and educators who defined the fundamental skills required to perform flexible GI endoscopy and then distilled the evaluation of these skills into 2 global assessments: GAGES Upper Endoscopy (GAGES-UE) and GAGES Colonoscopy (GAGES-C). A multi-institutional trial was then conducted to establish the validity of GAGES proving that experts and novices achieved different scores when evaluated by expert observers. This exciting work provided the first validated clinical assessment tool for performing flexible endoscopy and may replace the practice of using procedure numbers as a surrogate for procedural competence.
In 2002 the American College of Surgeons (ACS) established its Division of Education which is pursuing a spectrum of educational programs to promote patient safety and help surgeons meet the requirements for Maintenance of Certification (MOC) while addressing core competencies[5]. One of the visions of this Division was the creation of a network of accredited simulation centers that could offer educational support to practicing surgeons on a local and regional level to enhance the quality of surgical care. Some have even suggested that in the future, surgeons may be required by their specialty board to intermittently take a sabbatical during their career and go to an educational institute like that envisioned by the ACS to update their knowledge and skills. In 2005 the ACS began accrediting simulation centers based on strict criteria defined by the Division of Education. These centers are now known as Accredited Education Institutes (AEIs) of which there are currently 46. Most are located in North America, but there are also Institutes in Sweden, Greece and the United Kingdom. Recently the ACS has added to the power of the AEI network by forming the Research and Development Committee of the Consortium of ACS-Accredited Education Institutes. The charge of this Committee is to facilitate and govern the conceptualization, development and implementation of multi-institutional research programs across the AEIs. Such collaboration will foster the development of validated metrics of skills acquisition in a manner that has not been possible before.
While the establishment of a coordinated network of AEIs is a unique ACS program, the concept of providing procedurally based medical training in a comprehensive education institute is not. In 1994 the European Institute of Telesurgery (EITS) was established in Strasbourg, France. This institute has become a model of procedural training in minimally invasive surgery and is responsible for the education of thousands of practicing surgeons over the last 15 years. In 2008 EITS exported their training model to Taiwan with the formation of the Asian Institute of Telesurgery (AITS) which is already having a significant impact on surgeons in Asia. World class institutes have been established in other parts of the world as well including the Minimal Access Therapy Training Unit (MATTU) in Surrey, England and the Advanced Mini Invasive Surgery Academy (AIMS) in Milan, Italy which are a contemporary of EITS having been developed around the same concept and responsible for training many surgeons across multiple specialties in minimally invasive surgical techniques.
So, now surgeons and gastroenterologists have a growing world wide network of education institutes to help them learn new procedures and technologies in an efficient manner. As more validated metrics of procedural competence develop, they will be incorporated into the training of these institutes so that meaningful measures of technical proficiency can be given to credentialing bodies for hospital privileging, state and board licensure and MOC.
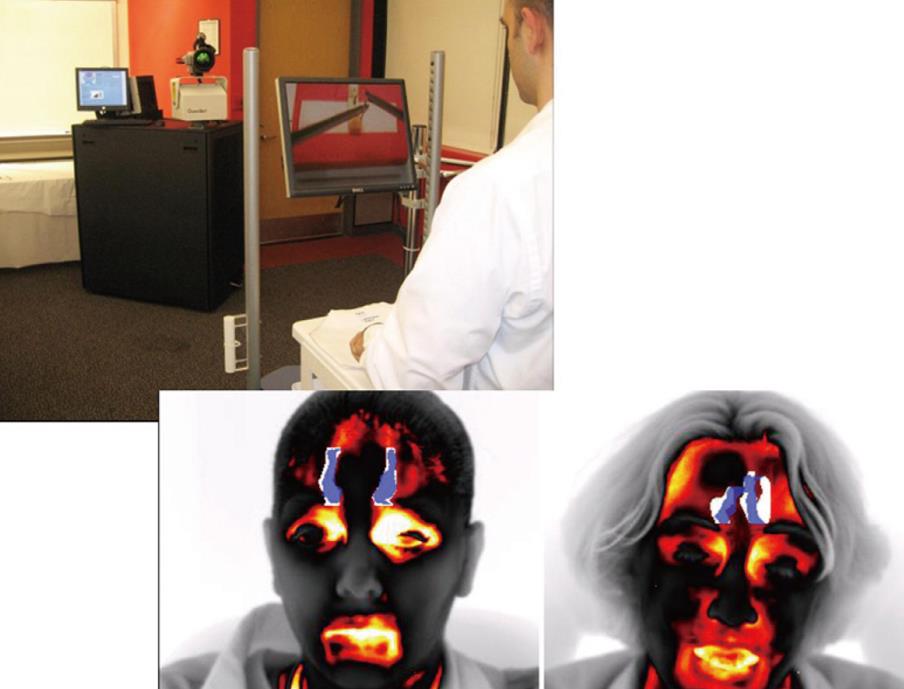
Exciting developments are on the horizon for verifying procedural competence in medical procedures and supporting physicians through the early part of their learning curve with these new techniques. One example comes from the Methodist Institute for Technology, Innovation and Education (MITIE) in Houston, Texas. MITIE has teamed up with the computer science department at the University of Houston (UH) to develop a novel method of measuring procedural competence using thermal imaging of the face (Figure 2). The UH team had developed a method of quantitatively measuring stress by monitoring the thermal signature of the face and other parameters such as perspiration build-up on the upper lip and intercantonal fold distance. When the MITIE team saw this technology, they hypothesized that expert surgeons should be less stressed while performing complex surgical tasks when compared to a novices and will thus have different thermal signatures. It was proposed to use this technology to monitor novice and expert surgeons while performing laparoscopic drills in a FLS trainer. Preliminary data indicates that these groups can be differentiated by their thermal monitoring. These results are exciting because such a monitoring device is unobtrusive and independent of the actual procedure being performed. Perhaps in the future, a credentialing body will ask for a surgeon’s thermal signature before granting privileges for a new procedure!
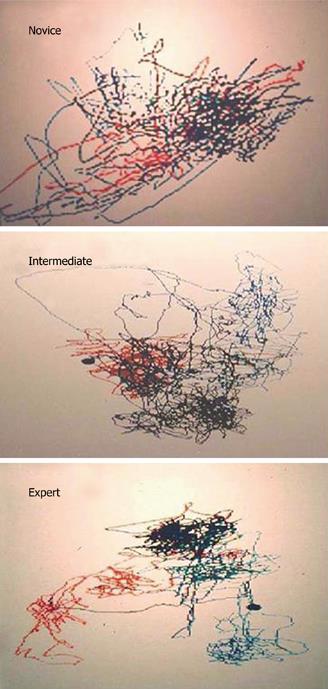
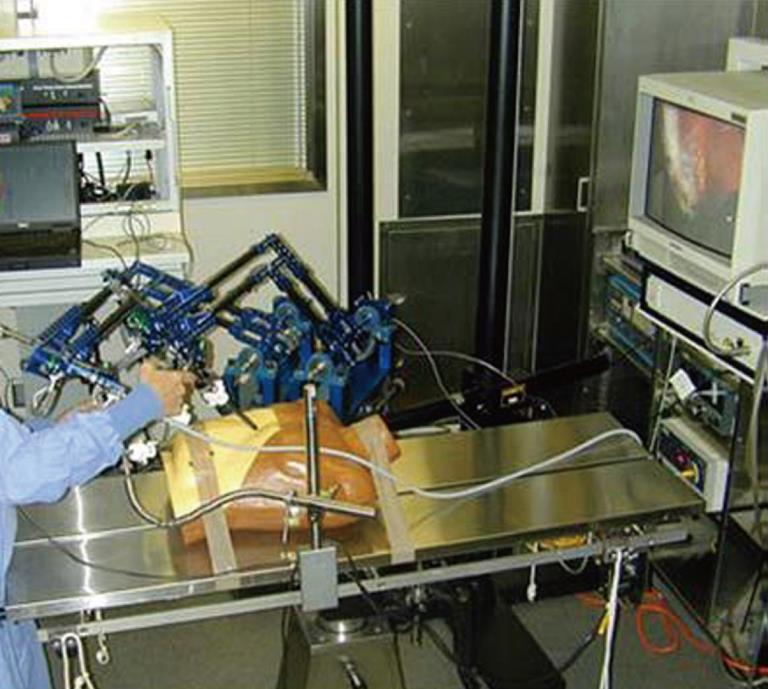
Other recent innovations in simulation include motion tracking of the hands. At the Imperial College in London, Datta et al[6] have used magnetic trackers in the Imperial College Surgical Assessment Device (ICSAD) to demonstrate that it is possible to quantitatively track the motion of a surgeon’s hands and generate a ‘‘motion signature’’ which has a different pattern in experts versus novices (Figure 3). A similar approach has been taken by Rosen et al[7] at the University of Washington using real laparoscopic instruments with a mechanical device called the Blue Dragon (Figure 4). Noble et al, working in MITIE, are using motion capture camera technology like that used for video games to monitor orthopedic surgeons during joint replacement surgery (Figure 5). Not only are the tools used by the orthopedic surgeon tracked in space but also the joint prosthesis themselves and the patient’s boney surfaces. Using this type of tracking, a surgeon can receive feedback about whether or not their surgical performance fell within acceptable parameters and, if not, what elements require correction. Another advance in simulation on the immediate horizon is termed patient specific simulation. This type of simulation allows for real clinical imaging data sets from specific patients to be programmed into a simulator for the purposes of rehearsing a procedure prior to its actual clinical performance. In this way, surgical teams may rehearse procedures using real patient data for their planning, running scenarios over and over until a satisfactory outcome is achieved. Such simulators are already available in endovascular surgery.
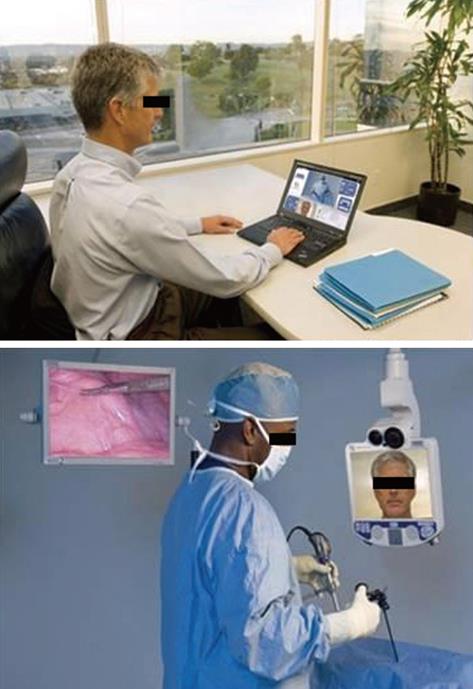
To maximize procedural adoption, it is imperative that a surgeon receives support from a preceptor after returning to their own hospital. This support during the early part of the learning curve is imperative to ensure smooth procedural adoption while maximizing patient safety. In an effort to address the challenges faced by traveling preceptors outlined earlier in this paper, some have turned to telecommunications as a means of providing support without requiring the preceptor to travel. Telemedicine has certainly gained acceptance in a number of areas but has been difficult to effectively implement in the operating room. Ideally, for teleproctoring to be effective, a meaningful linkage to the OR could be established at a moment’s notice when the operating surgeon desires a real time consultation. Until recently, this type of communication has not been available. However, In Touch Health Inc., a leader in medical telepresence via the wide area network (WAN) and a remotely manipulated robot, has partnered with Karl Storz Endoscopy to develop the VisitOR1TM telecommunications platform (Figure 6). This platform allows a preceptor working from a laptop computer to link into a VisitOR1TM operating room and manipulate a video monitor with built-in camera and laser pointer. By remotely controlling the camera and video platform the proctor can see what the surgeon sees, point to areas on the operating field, telestrate on the video monitor and push pre-recorded content out to the operative field. With this type of communication an experienced surgeon working through the early part of their learning curve for a new procedure could be guided safely to deliver quality care in a short period of time with excellent outcomes.
If NOTES progresses to become a common surgical approach, multiple types of NOTES training environments will be created. Ideally, these environments will incorporate the above elements in order to confirm procedural competence. For example, once the learner has prepared for a hands-on training experience, they would come to an accredited training institute to work in a simulated environment. This environment would reproduce patient specific anatomy and pathology for accurate pre-procedure rehearsal. The surgeon’s performance would also be closely monitored with both thermal imaging and motion tracking to ensure proper technique. Finally, when the surgeon has been deemed competent in this simulated environment, they would return to their own hospital where telemedicine technology could allow a mentor surgeon to join them remotely and counsel them through their first procedures.
In the end, the real question is not who is going to be performing NOTES – gastroenterologists or surgeons? The real question is how do practicing health care professionals learn new techniques and technology and introduce them safely into their practice to optimize patient care? NOTES is an example of the ever quickening pace of change in medical technology putting unprecedented pressure on health care providers to stay current. The advent of an international network of educational institutes coupled with the development of validated metrics of procedural competence will help procedurally based physicians adopt new techniques safely with maximum patient benefit. In this way surgery continues to move away from an apprentice model of skills acquisition to a criterion-based one. Such a move is required to address the fast pace of change in health care.
Peer reviewer: Rungsun Rerknimitr, MD, Division of Gastroenterology, Internal Medicine, King Chulalongkorn Memorial Hospital, Rama IVC Rd Lumpini, Bangkok 10310, Thailand
S- Editor Wang JL L- Editor Roemmele A E- Editor Yang C
| 1. | Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114-117. |
| 3. | Sachdeva AK. Acquiring skills in new procedures and technology: the challenge and the opportunity. Arch Surg. 2005;140:387-389. |
| 4. | Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG. Proving the value of simulation in laparoscopic surgery. Ann Surg. 2004;240:518-525; discussion 525-528. |
| 5. | Sachdeva AK, Pellegrini CA, Johnson KA. Support for simulation-based surgical education through American College of Surgeons--accredited education institutes. World J Surg. 2008;32:196-207. |
| 6. | Datta V, Mackay S, Mandalia M, Darzi A. The use of electromagnetic motion tracking analysis to objectively measure open surgical skill in the laboratory-based model. J Am Coll Surg. 2001;193:479-485. |
| 7. | Rosen J, Brown JD, Barreca M, Chang . L, Hannaford B, Sinanan M. The Blue DRAGON–a system for monitoring the kinematics and the dynamics of endoscopic in minimally invasive surgery for objective laparoscopic skill assessment. Stud Health Technol Inform. 2002;85:412-418. |