CASE REPORT
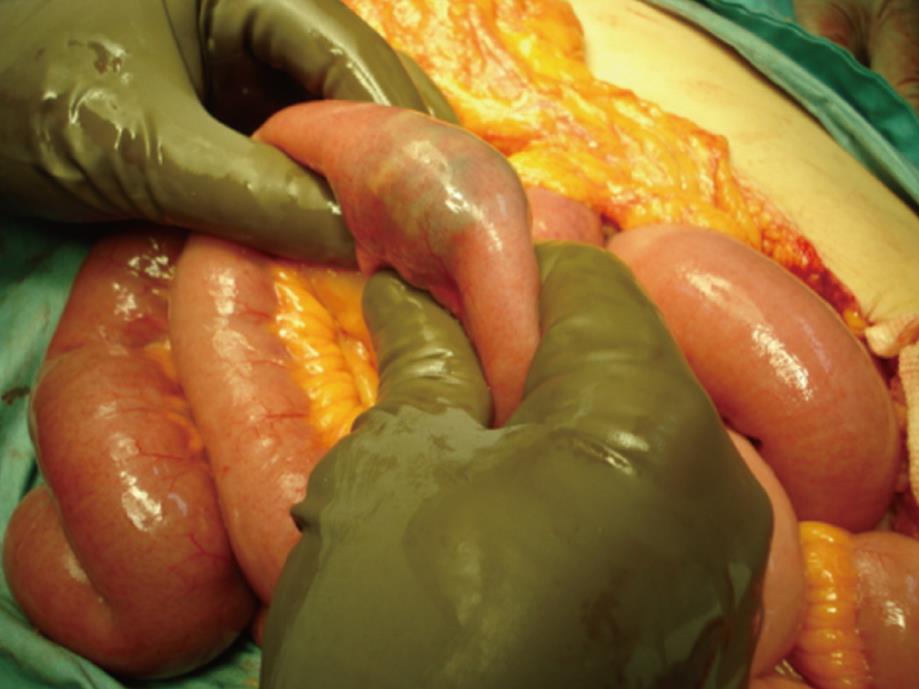
A 51-year-old female patient was referred to our hospital with 3 events of abdominal pain and distension, postprandial vomiting and pain relief after vomits, absence of transit of feces and flatus, during the previous 7 d. There was no previous history of gallstone disease. At admission, physical examination revealed a temperature of 37.2°C, a pulse of 98 beats per minute, a respiratory rate of 18 per minute and blood pressure of 100/75 mmHg. Bowel sounds were hyperactive, her abdomen was mildly distended, with tenderness, but no guarding or rebound. White blood cell count was 9400 per cubic millimeter, with 86% neutrophils. Other tests were unremarkable. Plain abdominal film demonstrated dilated bowel loops, air-fluid levels and a vague image of a stone in the inferior left quadrant (Figure 1). On the second day after admission, the patient presented transit to feces and gases, and vital signs normalized; white blood cell count was 6400 per cubic millimeter, with 80% neutrophils. Once stabilized, with a diagnosis of intestinal obstruction and its intermittent presentation, probably due to a gallstone ileus, the decision was made to perform a laparotomy. Generalized distention of jejunum and ileum was found proximal to a palpable stone, impacted 70 cm from the ileocecal valve (Figures 2 and 3). The gallbladder presented gallstones and a firm adhesion to the first portion of the duodenum, suggestive of a cholecystoduodenal fistula. No other gallstones were palpated. Due to her stable condition, enterolithotomy and ileal suture repair, repair of the cholecystoduodenal fistula, duodenorrhaphy and cholecystectomy were performed. At histopathology, the gallbladder showed cholelithiasis, acute and chronic inflammation and a fistulous tract walled by fibrous and granulation tissue. Following an uneventful recovery, the patient was discharged 10 d later. After a 6 mo follow-up, she remains in good health.
Figure 1 Plain abdominal film suggestive of intestinal obstruction and a calcified stone (arrow).
Figure 2 Site of stone impaction in ileum.
Figure 3 Enterostomy showing the obstructing gallstone.
DISCUSSION
Gallstone ileus is described as a mechanical intestinal obstruction due to impaction of one or more large gallstones within the gastrointestinal tract[1]. It represents an unusual cause of intestinal obstruction, accounting for 1%-4% of all cases, but accounts for 25% of nonstrangulated small bowel obstructions in those over the age of 65[3,7]. This condition is usually preceded by an event of acute cholecystitis, with its consequent adhesions and inflammation, facilitating the formation of a fistula with the small or large intestine, and allowing the passage of a gallstone[1,4]. It has been suggested as part of the natural history of Mirizzi syndrome, where continuous inflammation may not only involve the biliary tract but the adjacent viscera as well[8]. Cholecystoenteric fistulae complicate less than 1% of gallstone cases. Although it usually affects elderly patients, with a peak incidence between 65 and 75 years of age, the age range of reported cases has been from 13 to 91 years[2,9].
The most common fistula is between the gallbladder and duodenum in 60%-86% of the cases. If the stone is large enough, usually greater than 2-2.5 cm in diameter, it will impact causing intestinal obstruction; the reported range is from 2 to 5 cm[1,3,10-12]. Multiple stones are reported in 3%-40% of cases[10].
The clinical presentation of gallstone ileus is that of intestinal obstruction, usually depends on the site of impaction, and may be manifested as acute, intermittent or chronic episodes[2]. The vomiting of proximal intestinal material becoming dark and feculent is a process called “tumbling” obstruction to indicate the halting movement of the gallstone down the gastrointestinal tract[11,13]. Most common sites of stone impaction are the terminal ileum and the ileocecal valve (50%-75%), while less common are the proximal ileum and jejunum (20%-40%), stomach, duodenum (less than 10%) and colon[4,10].
The diagnosis of gallstone ileus is difficult, and is not made until laparotomy in 50% of cases. Plain abdominal films are diagnostic in about 50% of cases, although only 10% of gallstones may be visualized[10]. Classical findings include: (1) pneumobilia; (2) intestinal obstruction; (3) aberrant gallstone location; and (4) change in location of a previously observed stone[14]. The presence of two of the three first signs, or Rigler’s triad, has been considered pathognomonic of gallstone ileus and is encountered in 40% to 50% of cases[10]. Nevertheless, the reported rate of classic radiographic triad findings ranges from 0% to 87%[15]. The finding of two air fluid levels in the right upper quadrant, secondary to air in the gallbladder, has been described as a fifth sign[16].
Abdominal ultrasound is useful to confirm the presence of cholelithiasis, and may also identify the fistula[17]. When compared to plain abdominal film and ultrasound, CT scan has proved to be the most valuable technique in the diagnosis of gallstone ileus cases, particularly to identify mechanical bowel obstruction, pneumobilia, and an ectopic gallstone within the bowel lumen[18]. Helical single-detector and multi-detector computed tomography can also depict the biliary-enteric fistula, besides giving information on the exact number, size and location of ectopic stones as well as the site of intestinal obstruction and thereby improving diagnostic accuracy[19,20].
The main goal of treatment is prompt relief of intestinal obstruction by removing the offending gallstone, with surgical intervention remaining the treatment of choice. Preoperative stabilization of the patient’s condition is essential, with special attention being paid to fluid and electrolyte balance and management of comorbid conditions[1].
There is no consensus on the choice of surgical procedure. The current approaches are: (1) enterolithotomy alone; (2) enterolithotomy with cholecystectomy performed later (two-stage surgery); and (3) enterolithotomy, cholecystectomy and fistula closure (one-stage surgery).
Enterolithotomy has been the most reported surgical procedure. The belief that the cholecystoenteric fistula will close spontaneously in the presence of a patent cystic duct has been reported. Nevertheless, the prevalence of recurrent cholecystitis has been highlighted as well as an increased incidence of gallbladder carcinoma in patients with fistulas[21,22]. Although recurrence rates of gallstone ileus of less than 5% are reported with 10% of patients requiring reoperations for continued symptoms related to biliary tract, recurrence rates of 17% or even 33% have also occurred[3,10,23,24]. A review of series reporting recurrences shows a recurrent gallstone ileus risk of 8.2% in patients who survive enterolithotomy alone; 52% of recurrences occur within the first month, while the remainder present within 2 years, with an associated 12%-20% mortality rate[25]. With a one-stage procedure, further events of cholecystitis, cholangitis and recurrent gallstone ileus are prevented[11].
On the other hand, in addition to the low recurrence rates of gallstone ileus and of further biliary-complications, simple enterolithotomy has been associated with an 11.7% mortality compared to 16.9% for the one-stage procedure[3]. Moreover, in patients treated with enterolithotomy and subsequent cholecystectomy plus fistula repair, mortality as low as 0% has been reported, whereas a mortality rate of 19% has followed the one-stage procedure[2]. Consideration should be taken of the fact that the severity of each case has influence on the outcome of any particular surgical procedure, and that mortality is not an absolute consequence of the surgical procedure itself. In a non-random study of three surgical groups comprising the one-stage procedure, two-stage procedure or enterolithotomy only, comparable in terms of patient age, associated concomitant diseases and APACHE II score, operative mortality and morbidity rates did not differ significantly among the three therapeutic groups[10]. In a retrospective study, where 7 stable patients, classified as ASA I and II, underwent a one-stage surgery, while 6 out of 7 pre-operatively shocked patients with ASA III and IV underwent an enterolithotomy alone; no mortality occurred at 30 d after the surgery[26]. In a recent retrospective study, all five patients in Group 1 were hypertensive and diabetic including two patients who had a history of ischemic heart disease, and all were hemodynamically unstable, with an ASA score of three or more, whereas the five patients in Group 2 were hemodynamically stable, with ASA score of two, and only two were hypertensive. Patients in Group 1 underwent enterolithotomy alone while patients in Group 2 underwent a one-stage procedure. There was no operative mortality in either group[27].
Proponents of a one-stage procedure recommend palpation of the entire bowel as essential to prevent further obstruction by a gallstone. It is also necessary to palpate the gallbladder and common bile duct, in order to exclude gallstones, evidence of leakage, abscess or necrosis[1,10,11,28].
No randomized trial has compared these surgical options, probably due to the low rates of presentation and to possible ethical considerations.
Small bowel resection and anastomosis is a therapeutic option in patients with an impacted gallstone when irreversible ischemic bowel damage or perforation is found[12].
The prognosis of gallstone ileus is usually poor, with mortality rates of up to 20%, due mainly to delayed diagnosis and comorbid conditions[3,5]. The average period between the initial symptoms and the time of admission ranges from 1 to 8 d[6,10,11,29], reflecting the intermittent gallstone movement until impaction occurs. Mechanical intestinal obstruction with abdominal pain and vomiting is seen in 80% of cases[10]. Moreover, the range of time between admission and operation, (3 to 4.5 d)[2,10] could be attributed to delays in establishing diagnosis and patient stabilization. A preoperative diagnosis in 43% to 73% of the patients has been reported, while more than 50% of the cases have been discovered only at laparotomy[3,10]. The delay from initial symptoms to hospital admission, and to diagnosis and treatment, the presence of comorbid conditions such as cardiorespiratory and metabolic diseases, and the effect of postoperative complications, might be responsible for the high rate of mortality[15].
The patient herein reported had a 7 d background of intermittent intestinal obstruction, with a vague calcified image suggestive of a gallstone in the abdominal film, although no clear pneumobilia was visualized. Stabilization was possible; passage of gases and feces were regained, due the presence of a gallstone “tumbling” obstruction, as already described[11,13]. The patient’s general condition and the surgical findings justified a one-stage procedure.
Surgical management should be individualized. When the patient is too ill or dissection is of major risk and when biliary surgery is not advisable at the initial operation, an enterolithotomy is the best option. Cholecystectomy and fistula closure might be considered on an elective basis, and appears to be justifiable when there are biliary symptoms or residual cholelithiasis at ultrasonography. The one-stage procedure should be the offered to patients who have been adequately stabilized in the preoperative period, and when local and general conditions, such as good cardiorespiratory and metabolic reserve, permit a more prolonged surgical procedure. The exclusion of the presence of gallstones by palpation of the gallbladder, common bile duct and the entire bowel is of paramount importance when deciding on biliary surgery in either one-stage or two-stage surgery[1,3,4,10-12,30].