Published online Jan 27, 2010. doi: 10.4240/wjgs.v2.i1.26
Revised: October 24, 2009
Accepted: October 31, 2009
Published online: January 27, 2010
Jejunal diverticula are quite rare. Furthermore, small bowel diverticular disease resulting in enteroliths can lead to complications necessitating surgical intervention. In this manuscript, we report two presentations of jejunal diverticulum with complications from enteroliths followed by a review of the literature. The first case was that of a 79-year-old male who presented with abdominal pain and was found, on computed tomography (CT) scan, to have evidence of intestinal perforation. A laparotomy showed that he had perforated jejunal diverticulitis. The second case was that of an 89-year-old female who presented with recurrent episodes of bowel obstruction. A laparotomy showed that she had an enterolith impacted in her jejunum in the presence of significant diverticular disease. Although a rare entity, familiarity with jejunal diverticular disease, its complications, and its management, should be part of every surgeon’s base of knowledge when considering abdominal pathology.
- Citation: Chugay P, Choi J, Dong XD. Jejunal diverticular disease complicated by enteroliths: Report of two different presentations. World J Gastrointest Surg 2010; 2(1): 26-29
- URL: https://www.wjgnet.com/1948-9366/full/v2/i1/26.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v2.i1.26
First described by Somerling in 1794 and then by Sir Asley Cooper in 1807, jejunal diverticular disease is a rarely found pathology, noted only in approximately 5% of post-mortem examinations[1]. Despite being a rare pathology, there is a greater prevalence of jejunal diverticular disease in the older age population, making it a topic of discussion in older patients presenting with abdominal pain[2]. While diverticular disease of the jejunum might be asymptomatic, patients with jejunal diverticulitis typically present with epigastric pain that radiates down the left side of the abdomen. However, the location of the pain is not consistent, and patients have been known to present with left lower quadrant pain similar to cases of sigmoid diverticulitis or with pain in the right lower quadrant suspicious for appendicitis[3]. Cases of jejunal diverticulosis can be complicated not only by diverticulitis, but by hemorrhage, perforation, intussusception, volvulus, malabsorption[4-6], and even small bowel obstruction due to enteroliths formed and expelled from these diverticula[7-10].
Cases of jejunal diverticulosis complicated by enteroliths are indeed rare, but worth mentioning as they can produce an enterolith ileus or lead to perforation if it becomes impacted. The stones formed within small bowel diverticula can be either de novo or secondary to a piece of undigested food. Those that form de novo are comprised of choleic acid, the end product of bile salt metabolism, as their primary constituent. It is theorized that choleic acid enteroliths form within small bowel diverticula due to an acidic pH shift within diverticula[11]. On rare occasions, these enteroliths have calcium as one of their constituents, making it apparent on plain abdominal radiographs. When the enterolith is extruded from the diverticulum, it can pass downstream in the small bowel toward the ileocecal valve and lead to a “tumbling ileus” as seen with gallstone ilea. Those stones that are not extruded can sit within the diverticulum for an extended period of time and might eventually erode through the bowel wall leading to perforation. If this perforation occurs slowly over time, a localized abscess can form without causing the patient to become acutely ill. Conversely, the case of the patient who perforates acutely can lead to gross contamination of the abdomen with peritonitis[7].
When complications of jejunal diverticular disease present, operative intervention is typically the treatment of choice in the patient who can tolerate surgery. Resection of the involved segment of bowel is curative; however, as with colonic diverticular disease, there is a possibility of later recurrence. In the case of enteroliths causing enterolith ileus, the stone can be manually lysed and milked into the colon where it can be passed through the rectum, an enterotomy may be performed to extract the stone, or a resection of the bowel may be performed.
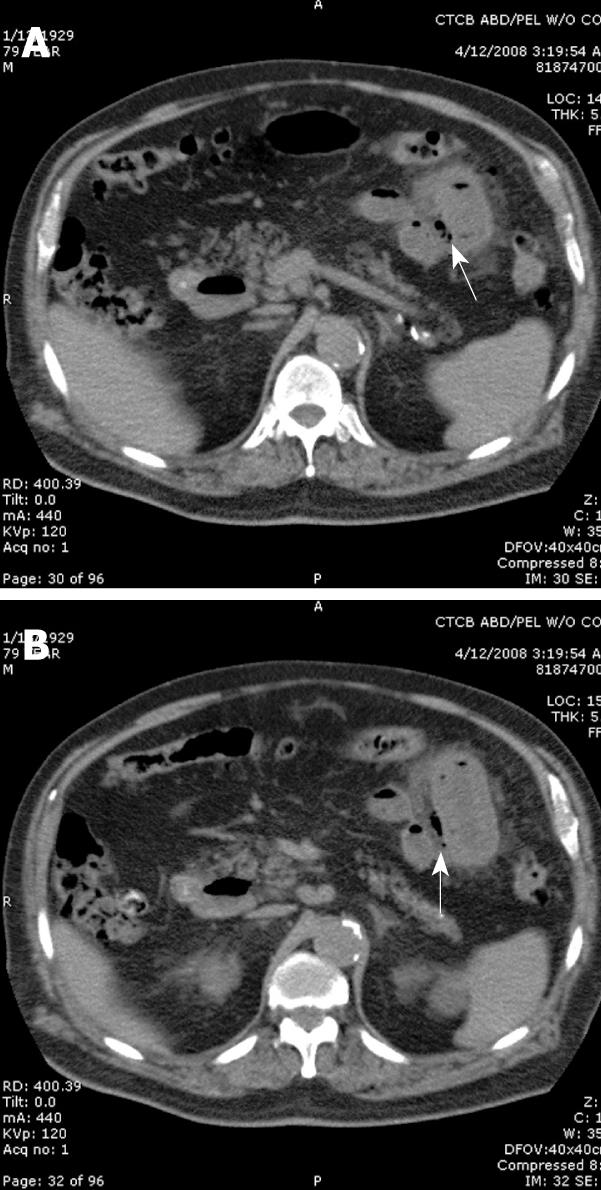
The first case is that of a 79-year-old Caucasian male who presented with a one day history of abdominal pain that was described as being diffuse and began after having a piece of coffee cake that contained nuts. The patient had associated nausea and vomiting. His past medical history was significant for diverticulitis, subdural hematoma, spinal disc herniation, and Alzheimer’s dementia. He had previously undergone a cholecystectomy, appendectomy, subdural hematoma evacuation, and spinal discectomy. Prior to surgical consultation, a computed tomography (CT) scan of the abdomen and pelvis was performed that demonstrated extensive inflammation of a segment of the small bowel on the left side of the abdomen (Figure 1A and B). There was also free air in the abdomen and pneumatosis of the mid jejunum, which was a concern for perforation. On physical examination, the patient was slightly tachycardic with a softly distended abdomen that was tender to palpation. During the operative exploration, the patient was noted to have turbid fluid on entering the abdomen. Intraoperative findings included the presence of extensive jejunal diverticula extending from the proximal to distal jejunum. A large impacted small bowel stone in the mid jejunum had significant associated inflammation along its path of migration, which led to pressure necrosis of the involved bowel wall. Approximately 100 cm of small bowel was resected, which contained two foci of necrosis, edematous jejunum, the impacted stone, and the segment of jejunum with the most extensive diverticular disease. After resection, the patient had bowel continuity re-established through a primary stapled anastomosis. After a 14-d hospital stay for management of peritonitis and postoperative adult respiratory distress syndrome, the patient had convalesced enough to be discharged to a short term nursing facility. At the time of discharge, he was tolerating diet, having activity levels back to baseline, and had no active abdominal pathology.
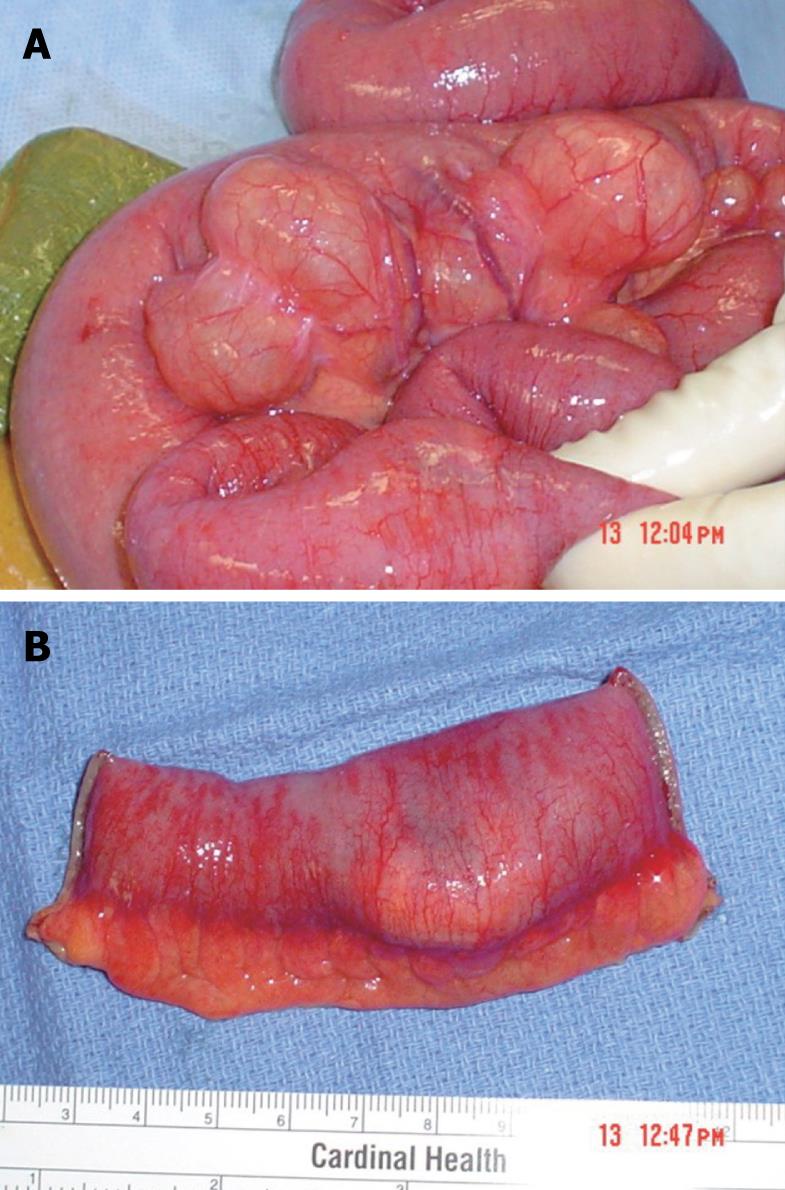
Our second case involves an eighty-nine year old Haitian female who presented to the emergency department complaining of a one-day history of generalized abdominal pain. The patient denied any nausea, vomiting, fever, chills, or genito-urinary symptoms. Her last bowel movement was three days prior to admission. Her past medical history was significant for hypertension, hypercholesterolemia, nephrolithiasis, diet controlled diabetes, diverticulosis, cholelithiasis, and arthritis. Her surgical history included a partial hysterectomy, ventral hernia repair, and carpal tunnel release. A CT scan of her abdomen and pelvis demonstrated pan-colonic diverticulosis and dilated loops of small bowel suggesting a partial bowel obstruction (Figure 2). An upper GI series with small bowel follow through, performed subsequently, demonstrated the presence of duodenal and jejunal diverticula (Figure 3).After failure of conservative management, we took the patient to the operating room for an exploratory laparotomy. Intraoperatively, we found multiple jejunal diverticula with dilated loops of small bowel (Figure 4A). On examination of the entire small bowel, an impacted stone was found in the distal jejunum (Figure 4B). A close inspection of the gallbladder ensured that our stone was not the result of a gallstone ileus. A primary small bowel resection encompassing the impacted stone was performed. Pathology confirmed a 3.5 cm × 3.0 cm × 1.5 cm tan calculus (Figure 5). The patient did well post operatively and was discharged without sequelae to a skilled nursing facility.
Small bowel diverticular disease is a pathological entity that is not easily diagnosed. However, it can be a source of abdominal pain, particularly in the elderly, and should be considered in the patient who has no other obvious pathology noted on physical examination or radiological evaluation. Diverticular disease of the small intestine is noted in the following distribution: 60%-70% duodenal, 20%-25% jejunal, and 5%-10% ileal[12]. The majority of cases of jejunal diverticulosis have been noted in patients in their sixth and seventh decades of life[13]. The literature estimates that jejunal diverticulosis has an incidence of 0.02% to 7.1%. Maglinte et al[14] described an incidence of small bowel diverticular disease of 2.3%, based on enteroclysis studies. In an autopsy series, Palder et al[15] described the incidence of jejunal diverticula to be 0.06% to 1.3%. Of interest, studies have been completed to determine the association between jejunal diverticular disease and diverticular disease elsewhere in the GI tract. In their research, Rankin and Palder discovered that synchronous colonic diverticulosis was present in 30%-61% of patients with jejunal diverticulosis and 22% had synchronous duodenal diverticula[15,16].
The pathogenesis of small bowel diverticular disease is akin to that of its counterpart in the large bowel. It is believed that intraluminal pressure is increased in a particular segment of bowel due to gut dysmotility, resulting in mucosal herniation along the mesenteric border of the bowel[17]. This makes the majority of jejunal diverticular disease a type of false diverticulosis, as there is no muscularis involved. With respect to the location of the diverticula, the mesenteric border of the bowel is more susceptible because there is an innate weakening of the wall due to entry of mesenteric blood vessels on that side. An association between small bowel diverticula and hereditary neuromuscular disorders such as Cronkhite-Canada syndrome has been noted, characterized by diffuse GI hamartoma polyps associated with malabsorption and diarrhea. There has also been an association between jejunal diverticulosis and lipid storage diseases such as Fabry’s disease, an X-linked recessive sphingolipidosis due to alpha-galactosidase deficiency.
In discussing jejunal diverticular disease, one must also discuss enterolith formation within the diverticula. De novo stone formation is theorized to form from choleic acid, the end product of bile salt metabolism. Deconjugation of bile salts by bacteria in the diverticula predisposes them to precipitate and result in stone formation due to the acidic pH within the proximal small bowel[13,17-20]. Another etiological basis for stone formation is stagnation of food particles from abnormal transit with resultant debris accumulation and stone formation. These stones can then remain within the diverticula and eventually lead to various complications.
Of the patients who do have jejunal diverticulosis, the majority is asymptomatic; however, 30% develop symptoms, and 10% may develop one of the associated complications that necessitate surgical intervention[17]. Edwards described the symptom complex seen in these patients as “flatulent dyspepsia” and noted that it consisted of epigastric pain, abdominal discomfort, and flatulence an hour or two after meals[9]. Patients can present with bleeding if there is erosion of the diverticulum into the mesenteric vessels that enter through the bowel wall immediately adjacent. They can also present with obstruction due to any of the following: enlargement of the diverticulum causing extrinsic compression of the bowel, enterolith ileus, or volvulus around the diverticulum[18]. These patients have also been known to present with malabsorptive signs and symptoms.
As the diagnosis of jejunal diverticular disease is not readily made on physical examination, one must rely on imaging and operative findings for a firm diagnosis. The literature has shown that CT scan has variable reliability, while barium swallows are the gold standard for diagnosis via radiographic imaging.
The treatment for diverticular disease of the jejunum is resection of the involved bowel segment. In a patient who is incidentally found to have diverticular disease of the small bowel on CT or intra-operatively, it is recommended that no action be taken. In the case of enteroliths causing obstruction, the patient should be taken to the operating room (OR) for exploration if there is no resolution of the obstruction. Once in the OR, digital or instrument fragmentation of the enterolith with milking into the distal intestine is the least invasive of operative interventions. It carries with it a success rate of 50% based on previously reported studies[19]. Complicated enteroliths will likely necessitate enterotomy. A caveat to the treatment of enterolith ileus is that one must be certain to evaluate for other stones within the bowel and the gallbladder.
Jejunal diverticulosis is typically a benign condition but might present as diverticulitis, gastrointestinal hemorrhage, obstruction, or frank perforation and should be considered particularly in the elderly population when there is no definitive source for pathology. Its management typically consists of resection of the involved segment of bowel. With respect to enteroliths complicating jejunal diverticulosis, one may see two very frequent presentations of this entity as described in the cases here: perforation or obstruction. In the case of perforation, the surgeon should perform an exploration of the abdomen with resection of the involved small bowel. In the case of partial bowel obstruction, the patient might be managed conservatively at first. However, non-resolution of the problem would mandate surgical intervention. Although jejunal diverticulosis and its complications are difficult to diagnose clinically, and even by conventional radiological means, it should be considered as a possible source of abdominal pain in the elderly patient when more common diagnoses have been excluded.
Peer reviewers: Grigory G Karmazanovsky, Professor, Department of Radiology, Vishnevsky Istitute of Surgery, B Serpukhovskaya street 27, Moscow 117997, Russia; Tatsuo Kanda, MD, PhD, Division of Digestive and General Surgery, Niigata University, Graduate School of Medical and Dental Sciences, Niigata 951-8510, Japan
S- Editor Li LF L- Editor Stewart GJ E- Editor Lin YP
| 1. | Cooper SA. The Anatomy and surgical treatment of abdominal hernia. Philadelphia: Lea and Blanchard 1844; . |
| 2. | Hayee B, Khan HN, Al-Mishlab T, McPartlin JF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003;9:883-884. |
| 3. | Silen W. Cope's Early Diagnosis of the Acute Abdomen, 21st ed. New York: Oxford University Press 2005; . |
| 4. | Chiu EJ, Shyr YM, Su CH, Wu CW, Lui WY. Diverticular disease of the small bowel. Hepatogastroenterology. 2000;47:181-184. |
| 6. | Williams RA, Davidson DD, Serota AI, Wilson SE. Surgical problems of diverticula of the small intestine. Surg Gynecol Obstet. 1981;152:621-626. |
| 7. | Slater NS. Perforation and obstruction by enterolith complicating jejunal diverticulosis; a report of three cases. Br J Surg. 1953;41:60-62. |
| 8. | Burkitt R. Intestinal obstruction due to enterolith complicating jejunal diverticulosis. Surgery. 1957;41:867-869. |
| 9. | Mortensen PB, Andersen JC. Acute obstruction by enterolith complicating jejunal diverticulosis. Case report. Acta Chir Scand. 1987;153:705-706. |
| 10. | Trésallet C, Renard-Penna R, Nguyen-Thanh Q, Cardot V, Chigot JP, Menegaux F. Intestinal obstruction by an enterolith from a perforated giant Meckel's diverticulum: diagnosis with CT reconstructed images. Int Surg. 2007;92:125-127. |
| 11. | Yang HK, Fondacaro PF. Enterolith ileus: a rare complication of duodenal diverticula. Am J Gastroenterol. 1992;87:1846-1848. |
| 12. | Crace PP, Grisham A, Kerlakian G. Jejunal diverticular disease with unborn enterolith presenting as a small bowel obstruction: a case report. Am Surg. 2007;73:703-705. |
| 13. | Lobo DN, Braithwaite BD, Fairbrother BJ. Enterolith ileus complicating jejunal diverticulosis. J Clin Gastroenterol. 1999;29:192-193. |
| 14. | Maglinte DD, Chernish SM, DeWeese R, Kelvin FM, Brunelle RL. Acquired jejunoileal diverticular disease: subject review. Radiology. 1986;158:577-580. |
| 17. | Harris LM, Volpe CM, Doerr RJ. Small bowel obstruction secondary to enterolith impaction complicating jejunal diverticulitis. Am J Gastroenterol. 1997;92:1538-1540. |
| 18. | Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997;184:383-388. |
| 19. | Steenvoorde P, Schaardenburgh P, Viersma JH. Enterolith ileus as a complication of jejunal diverticulosis: two case reports and a review of the literature. Dig Surg. 2003;20:57-60. |
| 20. | Liu CH, Huang KW, Mo YH, Yang PM. Enterolith ileus in a patient with jejunal diverticulosis: sonographic findings. J Clin Ultrasound. 2007;35:169-173. |