Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.98947
Revised: December 10, 2024
Accepted: January 17, 2025
Published online: March 27, 2025
Processing time: 229 Days and 11.2 Hours
Complications associated with stomas—including parastomal hernia (PSH), pro
To analyze the existing data regarding the efficacy of EPC compared to TPC in reducing stoma-related complications post-colostomy.
PubMed, Google Scholar, EMBASE, MEDLINE, and the Cochrane Library were adopted to uncover pertinent papers in which EPC and TPC approaches were compared. We then conducted a meta-analysis using RevMan 5.4.1.
Both laparoscopic (Lap) and open approaches showed a reduced incidence of PSH in EPC relative to TPC (P < 0.00001 and P = 0.02 respectively). In addition, Lap EPC depicted a lesser incidence of prolapse, mucocutaneous separation, and stoma retraction (P = 0.007, P = 0.03, and P = 0.01, respectively) compared to Lap TPC. However, EPC and TPC did not differ with respect to operation time, blood loss, edema, ischemia, necrosis, or infection after the LAP approach.
The extraperitoneal approach may provide benefits in minimizing some stoma-related problems such as PSH, pro
Core Tip: The study provides an inclusive meta-analysis comparing extraperitoneal (EPC) and transperitoneal (TPC) routes in colostomy surgery, emphasizing significant reductions in parastomal hernia, prolapse, stoma retraction, and mucocutaneous separation with the EPC approach. Despite previous studies suggesting benefits, newer evidence from 1973 patients highlights methodological improvements and the inclusion of previously overlooked cohort studies. Findings indicate comparable operative outcomes between EPC and TPC routes, challenging previous assertions. The study underscores EPC's potential to enhance postoperative quality of life by minimizing specific complications.
- Citation: Isah AD, Wang X, Shaibu Z, Yuan X, Dang SC. Systematic review and meta-analysis comparing extraperitoneal and transperitoneal routes of colostomy-related complications. World J Gastrointest Surg 2025; 17(3): 98947
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/98947.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.98947
Colorectal cancer constitutes approximately 10% of newly diagnosed malignancies and cancer-related fatalities globally each year, and ranks as the third most prevalent cancer in men and the second most prevalent in women worldwide[1,2]. Conventional surgical techniques, including abdominoperineal resection (APR) and sigmoidectomy, are regarded as safe and effective interventions for these individuals[3,4]. However, even with the progress in surgical instrumentation and methodologies, some patients with low rectal cancer still require sigmoidostomy, which entails a significant risk of com
A colostomy requires creating a hole in the large intestine by pulling the healthy segment through an incision in the abdominal wall, thus establishing an alternate route for waste excretion[7]. This aperture, along with the connected sto
Regarding the prolonged use of these techniques, a consensus on the efficacy of permanent sigmoidostomy in avoiding parastomal hernia (PSH) remains unclear. The European Hernia Society contends that there are inadequate data to demonstrate the advantage of EPC over TPC in decreasing the incidence of PSH[7]. However, prior meta-analyses of open surgical techniques indicate that colostomies formed by the EPC route show a reduced incidence of PSH relative to those constructed via the TPC route[9]. Although studies on laparoscopic APR have revealed that the laparoscopic EPC approach reduces the rate of PSH[10], performing an EPC colostomy during laparoscopic APR is more challenging due to the technical complexities[11]. Deciding whether to pursue an open or laparoscopic extraperitoneal or transperitoneal route for a permanent stoma placement remains a point of perplexity for many surgeons. It is thus crucial to carefully consider the feasibility of each approach based on the specific patient’s condition, anatomy, and potential risks and benefits associated with the procedure. We herein assessed the impact of open and laparoscopic EPC vs TPC routes on colostomy-related complications.
In this meta-analysis we evaluated the EPC and TPC approaches using randomized controlled trials (RCTs) and retro
We conducted an extensive search of the PubMed, MEDLINE, Google Scholar, Cochrane Library, and Web of Science databases for publications published between 1976 and 2024. This investigation focused on research that compared the EPC and TPC approaches for individuals having an end colostomy due to cancer or other ailments. A search was imple
The following criteria were considered for inclusion.
Participants: Adult patients undergoing colonic surgery that comprised either an end colostomy or APR.
Interventions: EPC and TPC.
Comparison: EPC vs TPC.
Outcomes: PSH, prolapse, necrosis, infections, retraction, ischemia, and mucocutaneous separation.
The following criteria were considered for exclusion. Studies that lacked specifically targeted data. Incomplete papers. Case reports and meta-analyses. Non-English language papers
Two reviewers individually assessed the search results, and all concerns regarding inclusiveness were addressed via dialogue. Publications were included using standardized forms that recorded data from studies, including study design, EPC or TPC colostomy, author, country, year of publication, surgical method (whether open or laparoscopic), period of follow-up, and patient number as outlined in Table 1.
| Ref. | Country | Year | Approach (open/lap) | Study design | Group EPC/TPC | Number of patients EPC/TPC | Follow-up month |
| Heiying et al[13] | China | 2014 | Lap | RCTs | EPC/TPC | 18/18 | 17 (12-24) |
| Whittaker et al[14] | England | 1976 | Open | RS | EPC/TPC | 89/162 | - |
| Madoka et al[15] | Japan | 2012 | Lap | RS | EPC/TPC | 22/15 | 23/14 |
| Leroy et al[16] | Taiwan | 2012 | Lap | RS | EPC/TPC | 12/10 | 22.25/36.3 |
| Hino et al[17] | Japan | 2017 | Lap | RS | EPC/TPC | 30/29 | 21 (2-95) |
| Xiao et al[18] | China | 2023 | Both | RS | EPC/TPC | 103/202 | 17-46 |
| Zhang et al[19] | China | 2024 | Lap | RS | EPC/TPC | 37/37 | 36 |
| Ota et al[20] | Japan | 2022 | Lap | RS | EPC/TPC | 105/222 | 38.0/45.5 |
| Xiao et al[21] | China | 2022 | Lap | RS | EPC/TPC | 83/50 | 6 |
| Wang et al[22] | China | 2018 | Lap | RS | EPC/TPC | 108/123 | 24 |
| Yao et al[23] | China | 2023 | Lap | RS | EPC/TPC | 30/30 | 6 |
| Wang et al[24] | China | 2024 | Lap | RS | EPC/TPC | 37/46 | 32/28 |
| Dong et al[25] | China | 2012 | Lap | RCTs | EPC/TPC | 66/62 | 6-60 |
| Marks et al[26] | United States | 2005 | Open | RS | EPC/TPC | 37/190 | 60 |
Postoperative outcomes—including operation time and blood loss—were included. Additionally, problems associated with colostomy (such as PSH, prolapse, edema, mucocutaneous separation, infection, necrosis, ischemia, and stoma retraction) were documented as shown in Table 2.
| Ref. | Operation time | Blood loss | Edema | Necrosis | Ischemia | Stoma retraction | Infection | Prolapse | Mucocutaneous separation | Parastomal hernia |
| EPC/TPC Lap | ||||||||||
| Heiying et al[13] | 14.7 ± 6.4/25.3 ± 8.5 | - | 0/6 | - | 1/1 | 0/0 | - | 1/0 | - | 2/0 |
| Whittaker et al[14] | 361 ± 64/308 ± 80 | 182 ± 118/203 ± 254 | - | 2/0 | - | - | 4/1 | - | 2/6 | 1/5 |
| Madoka et al[15] | ||||||||||
| Leroy et al[16] | 320.83 ± 65.84/350 ± 64.8 | - | 0/2 | - | - | 0/1 | 0/0 | - | 0/4 | |
| Hino et al[17] | 291 ± 120/ 306 ± 102.25 | 43 ± 172.5/66 ± 203.25 | - | - | 0/2 | 0/3 | 1/0 | 1/4 | 0/1 | 4/12 |
| Xiao et al[18] | 209.47 ± 24.23/ 210.00 ± 24.42 | 90.67 ± 116.42/ 84.43 ± 41.92 | - | - | - | - | 3/7 | 6/10 | 0/2 | 7/31 |
| Zhang et al[19] | 205± 10.75 /205± 12.5 | - | - | 0/0 | - | 0/0 | - | 0/3 | - | 6/5 |
| Ota et al[20] | 289± 156.75/345.5± 192.5 | 50± 143.75/60 ± 407.5 | - | - | - | - | 17/46 | - | - | 2/38 |
| Xiao et al[21] | 23.1± 6/21.4 ± 4 | - | - | - | - | - | - | - | - | 0/4 |
| Wang et al[22] | 168.0 ± 21.2/ 170.2 ± 21.2 | 167.1 ± 73.7/179.1 ± 76.3 | 10/5 | 1/2 | - | 0/6 | 1/3 | 0/6 | - | 5/22 |
| Yao et al[23] | 26.64 ± 2.45/24.86 ± 2.78 | - | - | - | - | 1/1 | - | 0/2 | - | 0/4 |
| Wang et al[24] | 155.8 ± 38.2/158.5 ± 32.4 | 119.4 ± 81.3/108.7 ± 74.7 | 13/7 | - | 0/1 | 2/4 | - | 0/6 | - | 1/9 |
| Dong et al[25] | 21.3 ± 3.5/30.4 ± 4.2 | - | - | 1/1 | - | 1/3 | - | 0/2 | - | 0/5 |
| EPC/TPC open | ||||||||||
| Marks and Ritchie et al[26] | - | - | - | - | - | - | - | - | 1/22 | |
| Whittaker et al[14] | - | - | 9/16 | - | - | - | 11/23 | 2/10 | 7/17 | 8/28 |
We conducted our analysis using Review Manager (RevMan) version 5.4.1, applying the Mantel-Haenszel method for statistical evaluation. Both dichotomous and continuous data were assessed to calculate odds ratios (ORs) with 95%CI, which provided insights into the statistical differences between the outcomes of EPC and TPC colostomies. Our findings are presented through forest plots. Statistical heterogeneity was evaluated using the I2 statistic, with heterogeneity categorized as follows: 0%–30% (low), 30%–60% (moderate), 50%–90% (substantial), and 75%–100% (considerable). A significance threshold of P < 0.05 was employed for all models.
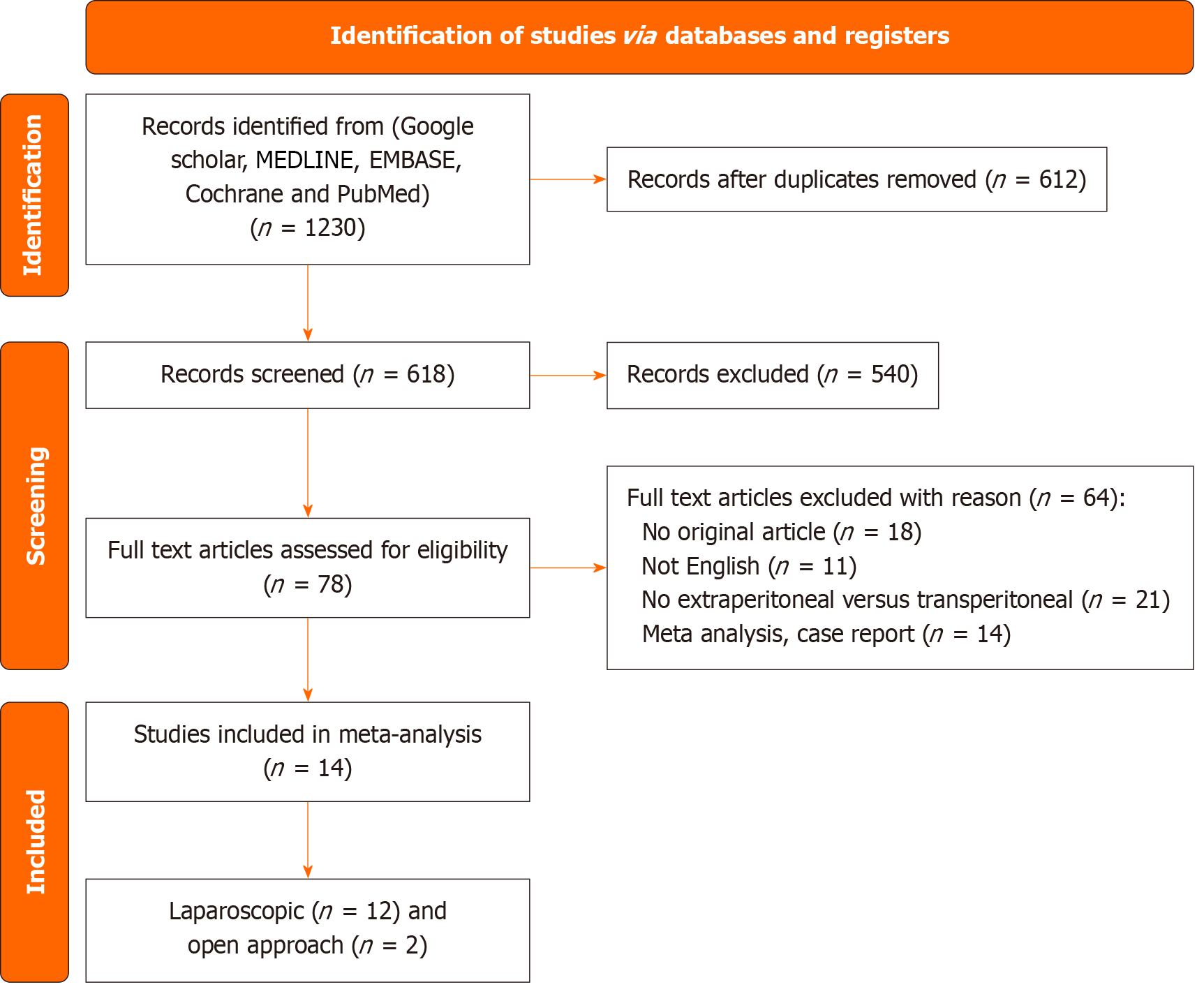
Our initial search identified 1230 articles, with 612 remaining after duplicate removal. Following the screening process, 78 articles were selected for full-text review. Of these, 14 studies met the inclusion criteria and were included in the final analysis: 12 focused on laparoscopic procedures, and 2 examined open procedures, as shown in Figure 1.
The included studies consisted of two RCT and 12 RS that involved a total of 1973 patients. Of these, 1495 patients underwent laparoscopic procedures (651 with EPC and 844 with TPC), and 478 patients underwent open procedures (126 with EPC and 352 with TPC).
The studies represented a geographically diverse sample, including data from Asia, Europe, and the United States; and offered a comprehensive perspective on the topic (detailed characteristics of the included studies are summarized in Table 1).
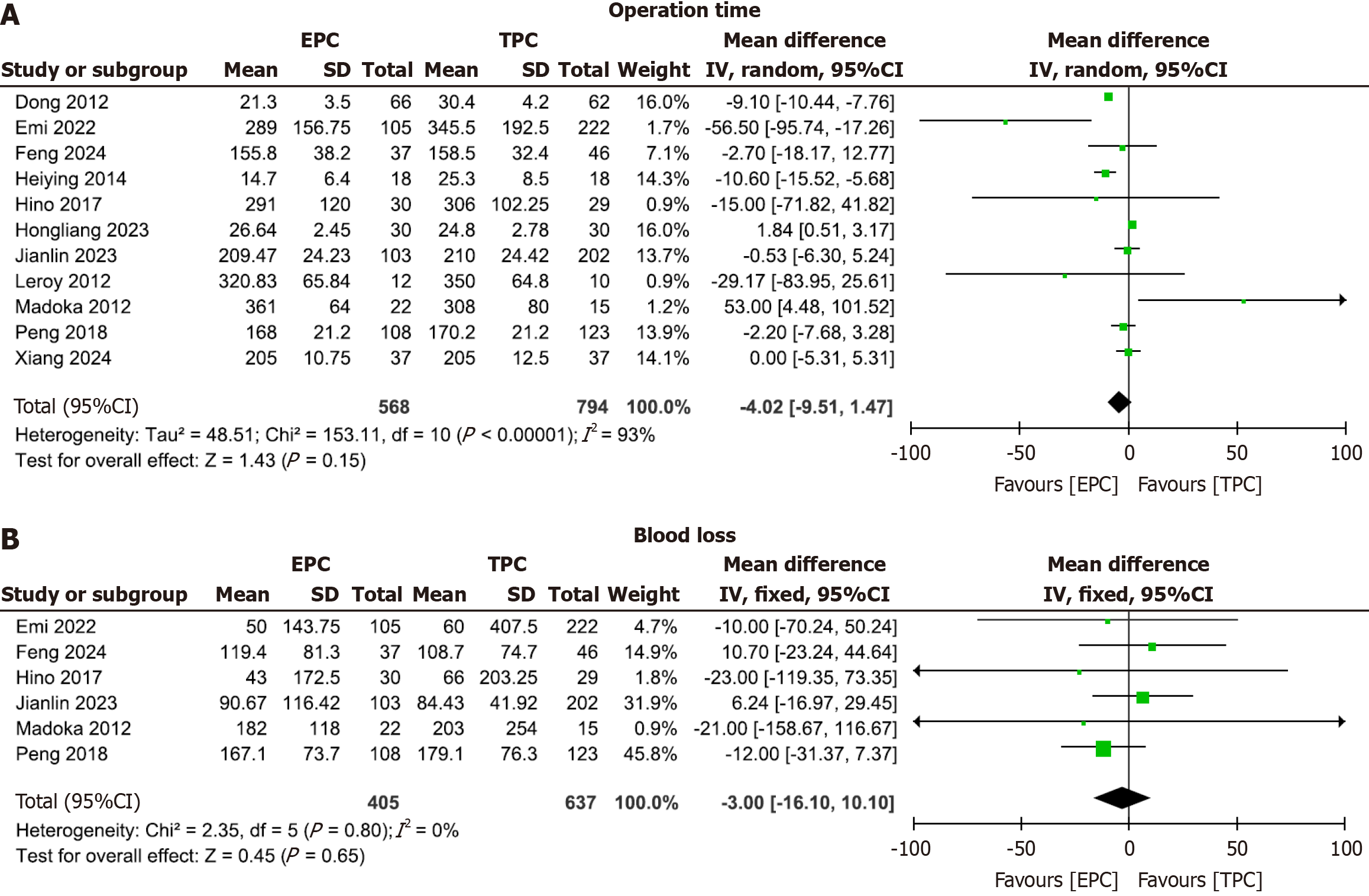
Several studies[13-25] collectively encompassed 1362 patients, comprising 568 patients in the EPC and 794 patients in the TPC groups. The analysis of operation time, as depicted in Figure 2A, indicated no statistically significant difference between the two groups. The mean difference was −4.02 (95%CI: −9.51-1.47), with an I2 of 93% and P = 0.15.
Six studies[15,17,18,20,22,24] collectively comprised 1042 patients, with 405 patients in the EPC group and 637 patients in the TPC group. The analysis of blood loss, as depicted in Figure 2B, indicated no statistically significant difference between the two groups. The mean difference was −3.00 (95%CI: −16.10–10.10), with an I2 of 0% and P = 0.65.
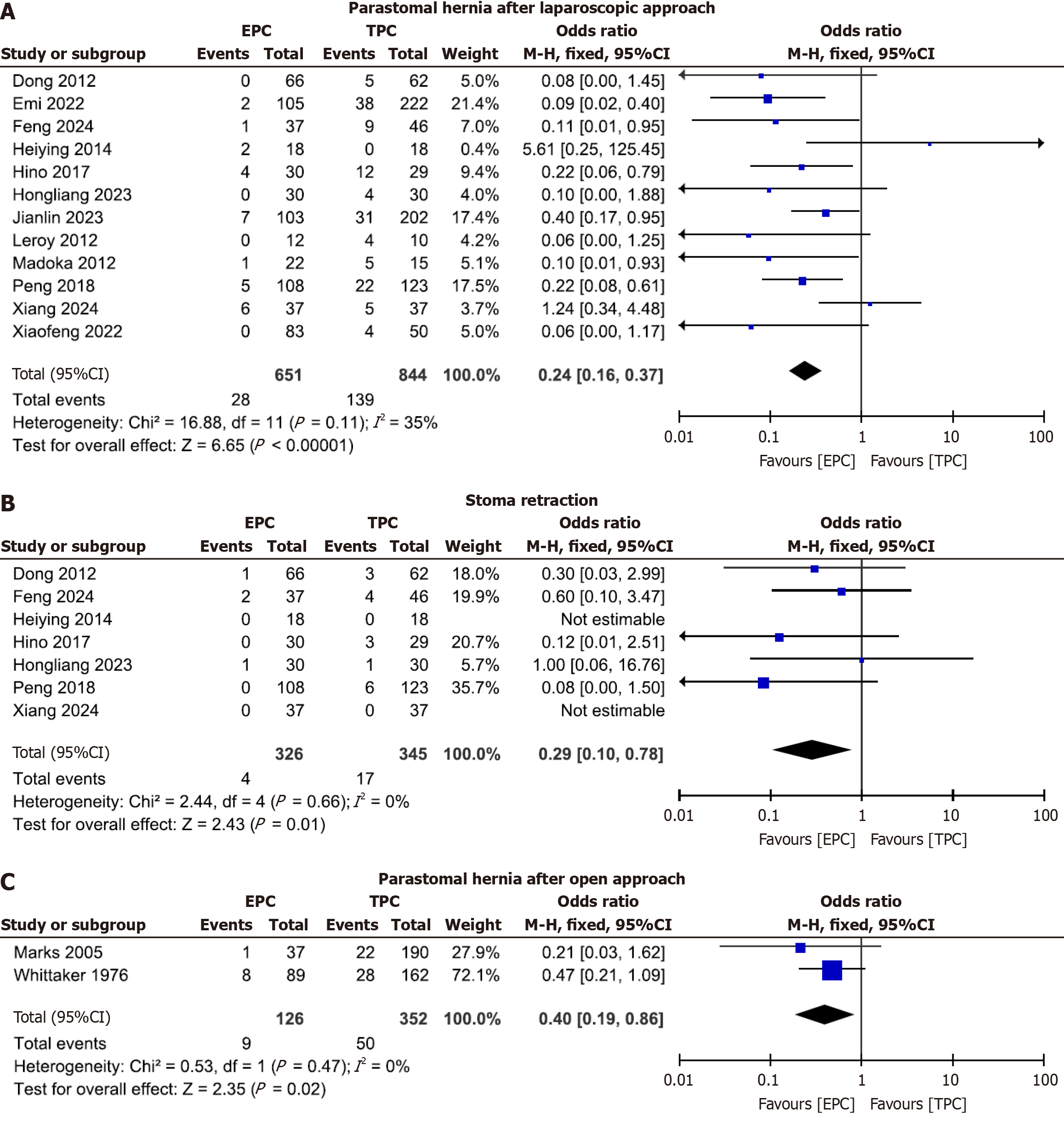
Twelve studies[13,15-25] collectively included 1495 patients, with 651 in the EPC group and 844 in the TPC group. Analysis of PSH rates (shown in Figure 3A) revealed a statistically significant difference favoring the EPC group. The PSH rate was 4.3% in the EPC group (28 of 651 patients) compared to 16.4% in the TPC group (139 of 844 patients). The OR was 0.24 (95%CI: 0.16–0.37), with an I2 of 35% and P < 0.00001.
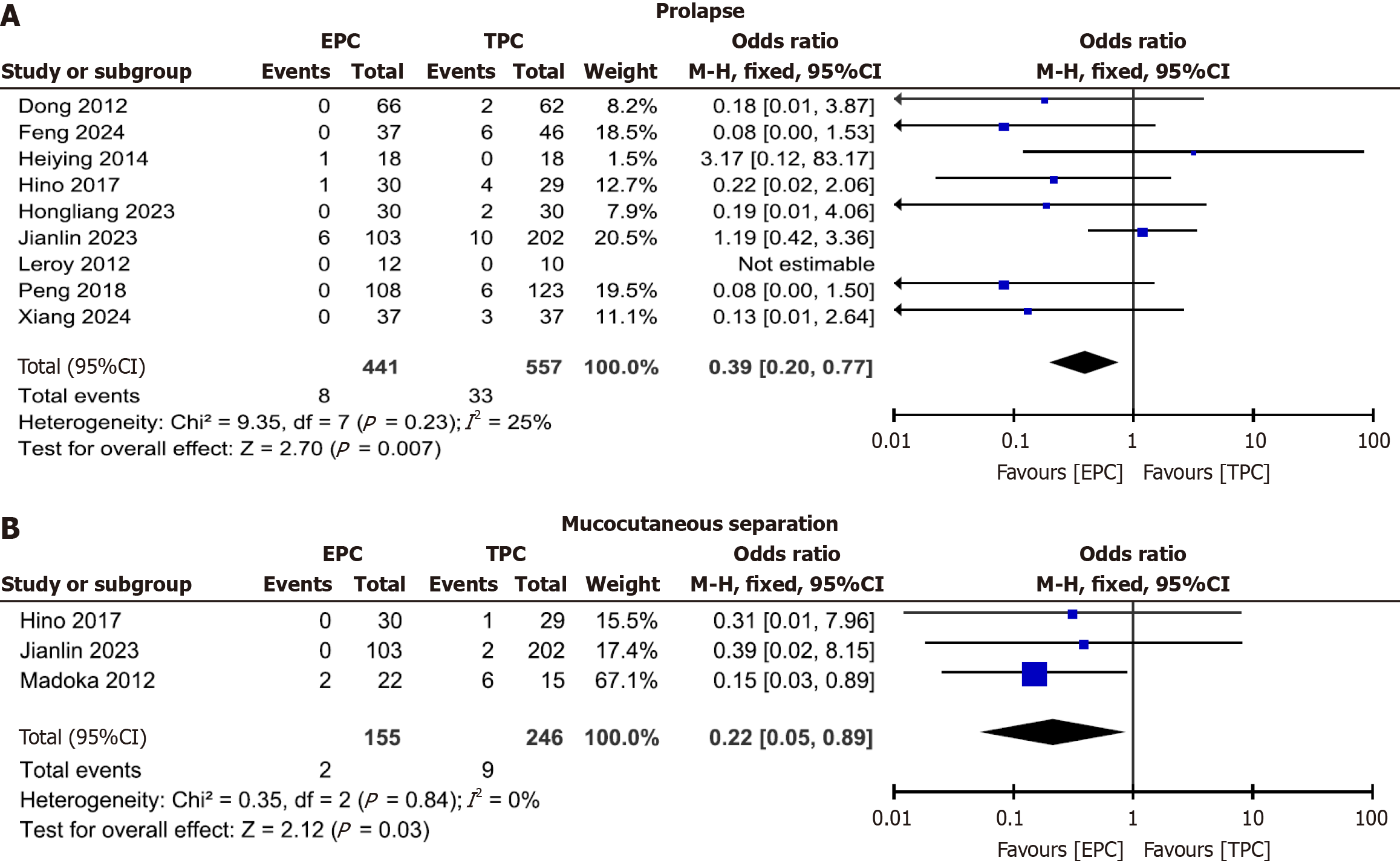
Nine studies[13,16-19,22-25] were collectively composed of 998 patients, with 441 in the EPC group and 557 in the TPC group. As illustrated in Figure 4A, the analysis of prolapse rates revealed a statistically significant difference that favored the EPC group. The prolapse rate was 1.8% in the EPC group (eight of 441 patients) compared to 5.9% in the TPC group (33 of 557 patients). The calculated OR was 0.39 (95%CI: 0.20–0.77), with an I2 value of 25% (indicating low heterogeneity), and a significance level of P = 0.007.
In three studies[15,17,18] that totaled 401 patients (155 in the EPC and 246 in the TPC groups), we analyzed the rate of mucocutaneous separation; and as shown in Figure 4B, there was a statistically significant difference in favor of the EPC group. The mucocutaneous separation rate was 1.3% (two of 155) in the EPC group compared to 3.6% (nine of 246) in the TPC group. The OR was 0.21 (95%CI: 0.05–0.84), with an I2 of 0% and P = 0.03.
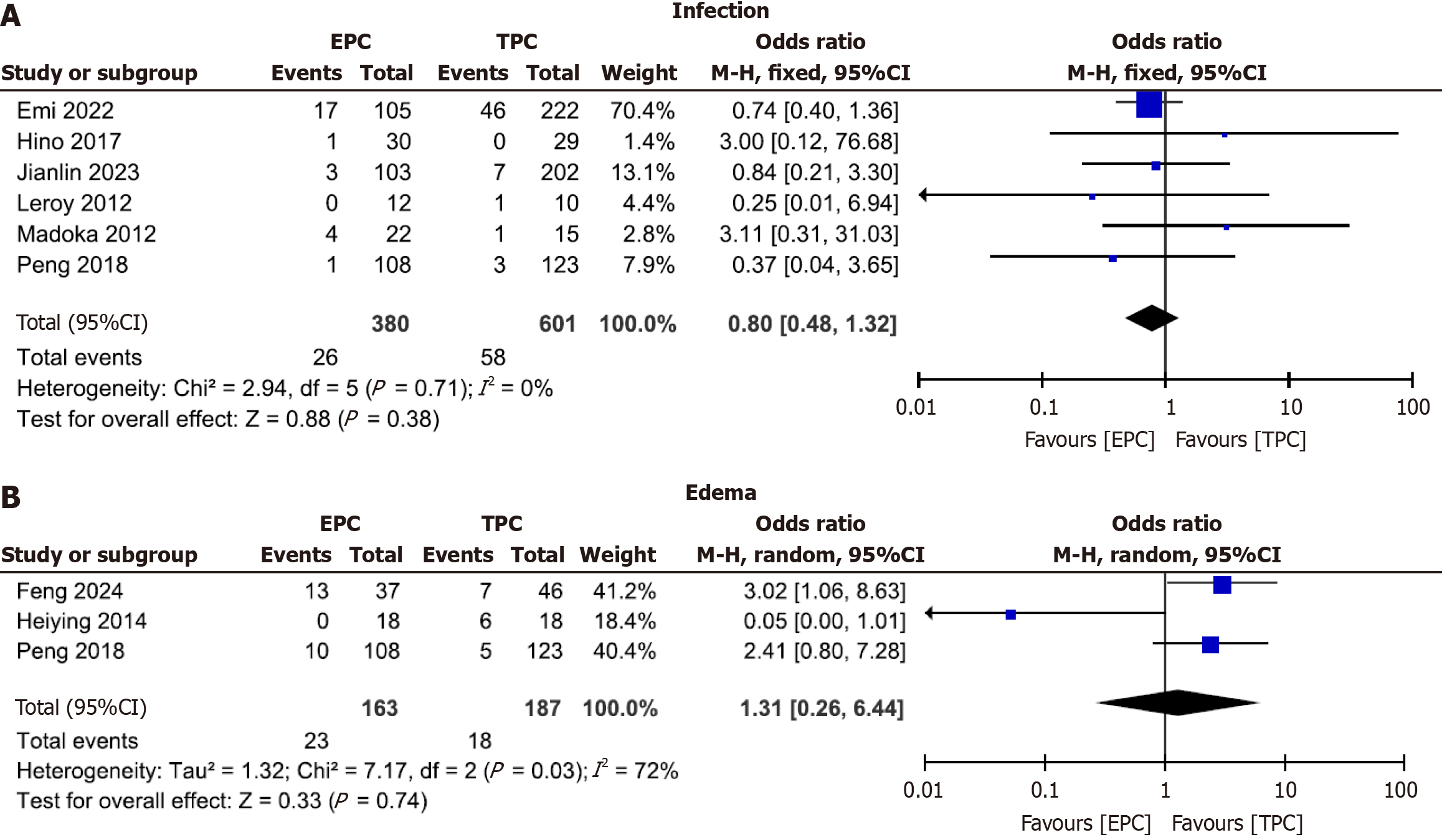
Six studies[15-18,20,22] collectively included 981 patients, with 380 in the EPC and 601 in the TPC groups; and our analysis of infection rates (shown in Figure 5A) did not reveal any difference between the groups. The infection rate was 6.8% (26/380) for EPC and 9.6% (58/601) for TPC, with an OR of 0.79 (95%CI: 0.48–1.32), I2 of 0%, and P = 0.38.
Three studies[13,22,24] consisted of 350 patients, 163 in the EPC and 187 in the TPC groups, and when we analyzed these for edema rates, we uncovered no difference between the groups (Figure 5B). The EPC group possessed an edema rate of 14.1% (23 of 163) vs 9.6% in the TPC group (18 of 187), for an OR of 1.31 (95%CI: 0.26–6.44), with an I2 of 72% and P = 0.74.
Seven studies[13,17,19,22-25] entailed 671 patients, with 326 in the EPC group and 345 in the TPC group. As shown in Figure 3B, analysis of stoma retraction showed a statistically significant difference that favored the EPC group. The stoma retraction rate was 1.2% (4 of 326 patients) in the EPC group, compared to 4.9% (17 of 345) in the TPC group, for an OR of 0.29 (95%CI: 0.10–0.78), an I2 of 0%, and P = 0.01.
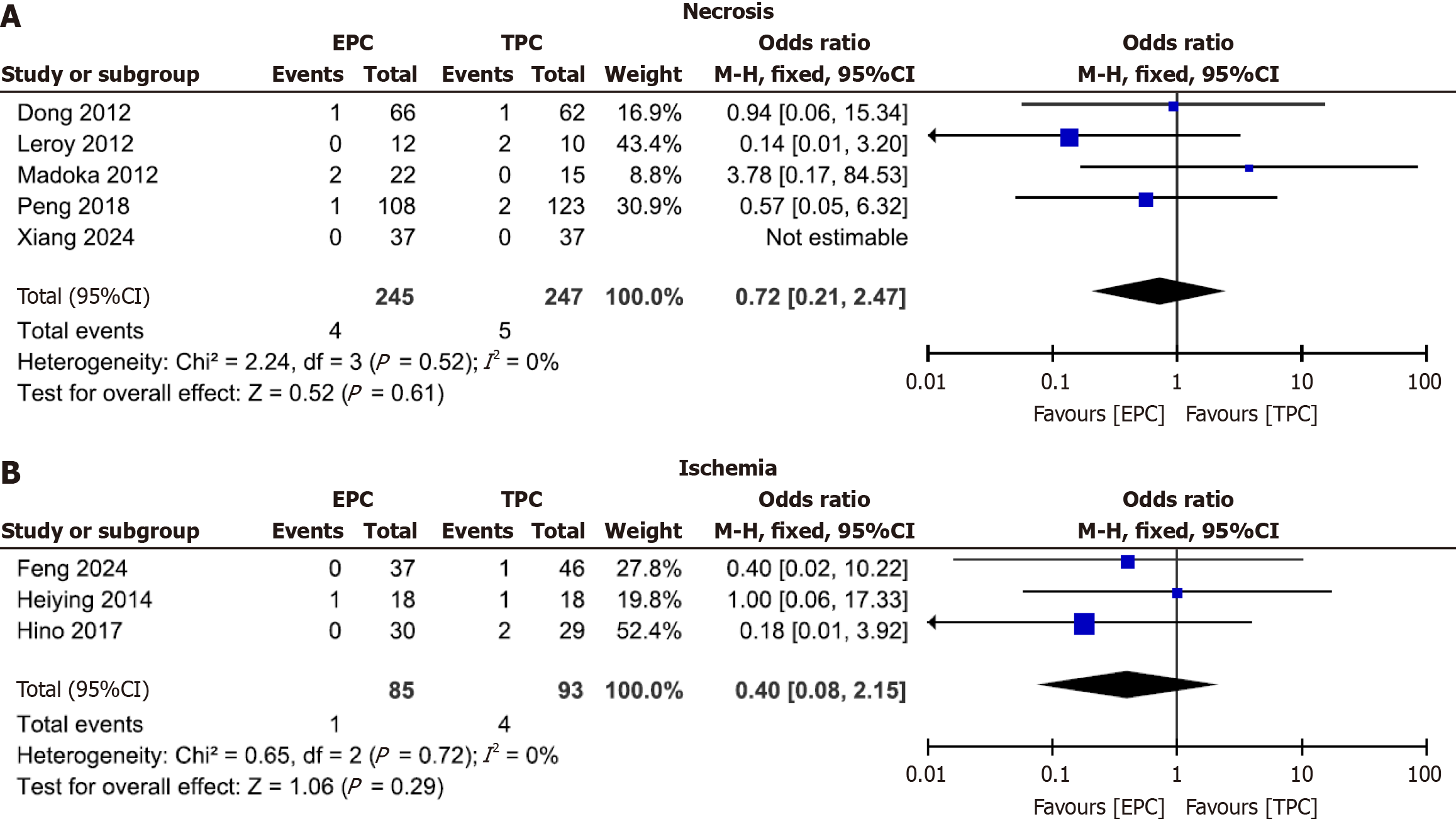
When we analyzed five studies of 492 patients for necrosis[15,16,19,22,25] (245 in the EPC group and 247 in the TPC group), we found no difference between the two groups (Figure 6A). The necrosis rate was 1.6% (4 of 245) in the EPC group and 2.0% (5 of 247) in the TPC group; the calculated OR was 0.72 (95%CI: 0.21–2.47), with an I2 value of 0% and P = 0.61.
Three studies[13,17,24] that encompassed a total of 178 patients (85 patients in the EPC group and 93 in the TPC group) were analyzed, and we found that the groups did not differ with respect to ischemia (Figure 6B). The ischemia rate was 1.2% in the EPC group (one case of 85) and 4.3% in the TPC group (four cases of 93), for an OR of 0.40 (95%CI: 0.08–2.15),
We analyzed the incidence of PSH in two studies[14,26] that encompassed 478 patients (126 with EPC and 352 with TPC) (Figure 3C), and our results indicated a statistically significant difference favoring the extraperitoneal group. The PSH rate was 7.1% in the EPC (9 of 126 patients) vs 14.2% in the TPC (50 of 352 patients), for an OR of 0.40 (95%CI: 0.19–0.86), an I2 of 0%, and P = 0.02.
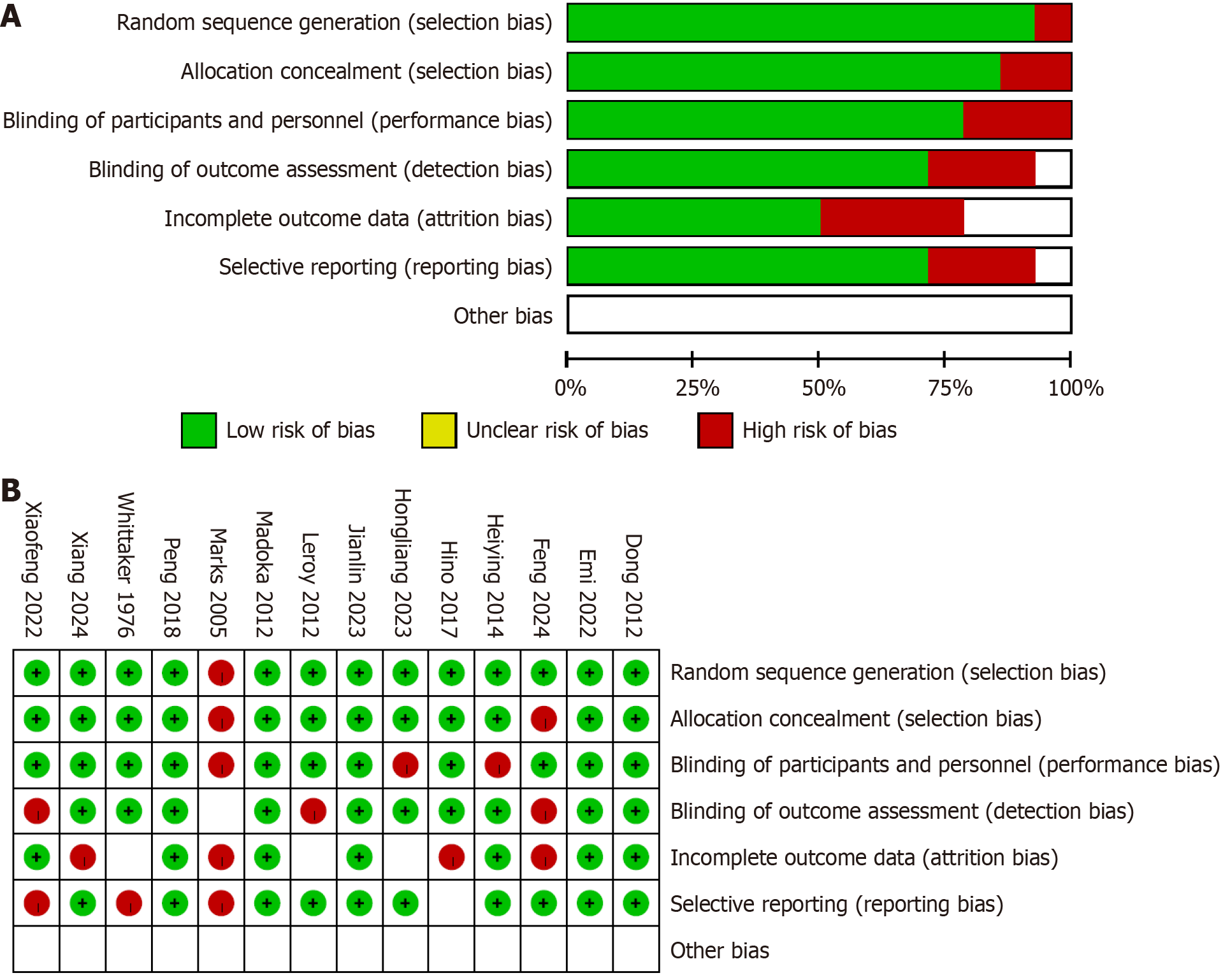
This study adhered to the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions (version 6.3) to objectively evaluate the quality of the included trials using the risk-of-bias tool. The assessment focused on several key domains: (1) Random sequence generation; (2) Allocation concealment; (3) Blinding; (4) Incomplete outcome data; (5) Selective reporting; and (6) Other relevant biases.
Trials were classified as “high risk” if bias was identified in one or more critical domains, trials with low risk of bias across all critical domains were categorized as “low risk”, and studies that did not clearly fall into either category were designated as “unclear” (the classification outcomes are illustrated in Figure 7). Any discrepancies among researchers were resolved through discussions involving the corresponding author.
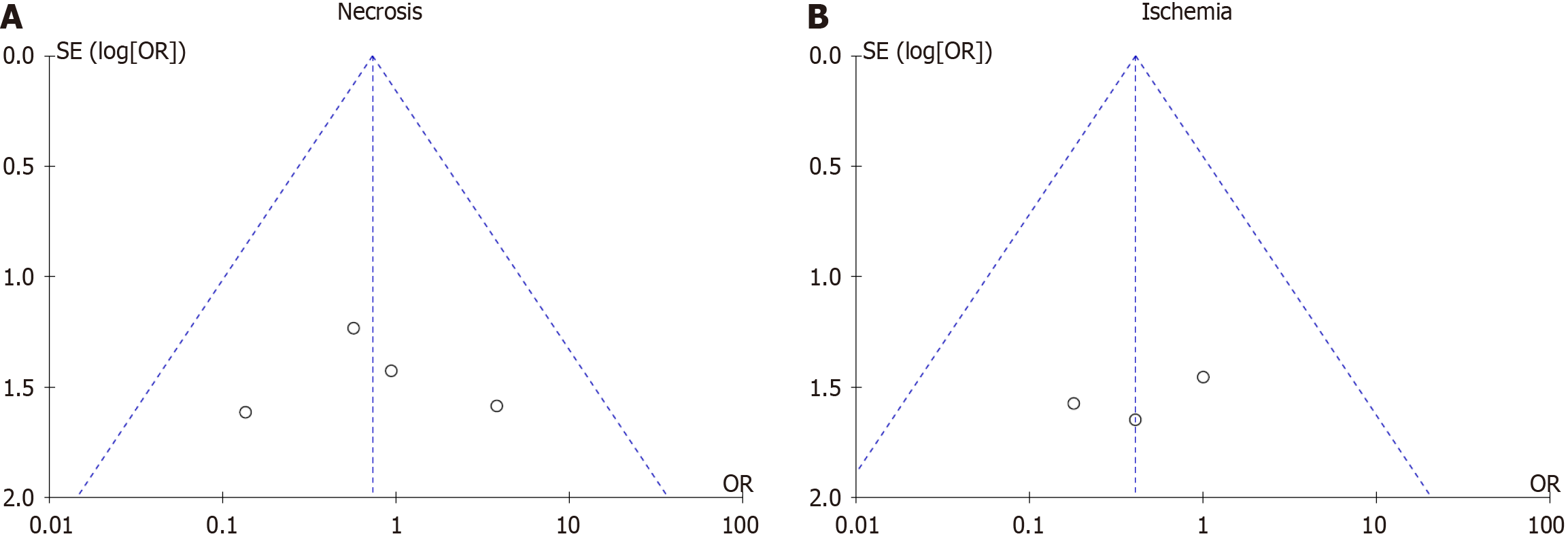
We detected no evidence of publication bias, as all studies fell within the 95%CI boundaries. The symmetry of the funnel plot was statistically assessed using the Egger test and confirmed the absence of bias. For necrosis, the analysis yielded an OR of 0.72 (95%CI: 0.21–2.47; P = 0.61; I2 = 0%); while for ischemia, the OR was 0.40 (95%CI: 0.08–2.15; P = 0.29; I2 = 0%), demonstrating no significant evidence of bias as shown in Figure 8.
Colostomy complications include mucocutaneous separation, stoma retraction, infection, ischemia, necrosis, edema, prolapse, and PSH; with the most common of these being PSH. Traditional treatment has been effective for most PSH, but surgical intervention often results in suboptimal outcomes; thus, prevention is considered the best course of action. While previous investigations have shown that extraperitoneal stoma formation exerts beneficial effects[19], evidence-based medical data remain limited.
Although authors of previous meta-analyses attempted to address the limitations of small-scale studies and reported findings that differ from those of the current study, our analysis remains crucial. This importance stems from the sig
Laparoscopic colostomy performed via the EPC route is often considered more technically demanding compared to the TPC route. However, congruent with findings from previous studies[15,16], our analysis did not reveal any differences in operative time or blood loss between the two approaches during laparoscopic surgery. Similarly, the authors of a separate meta-analysis also reported no notable differences between the techniques[10]. While Heiying et al[13] observed that the median operative time for the EPC route was approximately 10 min longer than for the TPC route, this difference was minimal and was deemed to be acceptable. This conclusion may be attributed to advancements in surgical techniques, procedural standardization, optimized patient selection, skilled surgical teams, and adherence to established clinical guidelines.
Recent developments have addressed the technical challenges associated with the EPC approach. For example, studies[29,30] have highlighted the use of a trocar-cannula system to create the extraperitoneal tunnel, simplifying the procedure by improving visualization and allowing for controlled tissue dissection. This technique reduces operative time and facilitates efficient creation of an EPC while maintaining satisfactory outcomes. Improved surgical skills and equipment, along with the selection of suitable patients and adherence to established protocols, likely contribute to the efficient per
In the present study, the incidence of PSH was significantly lower with the EPC route compared to the TPC route in both laparoscopic and open surgical approaches (P < 0.00001 and P = 0.02, respectively), with our findings consistent with those of previous studies[27,28]. A primary contributing factor to PSH is the insufficient structural density at the junction between the colon and the abdominal wall that can compromise integrity and result in herniation. Supporting these results, a meta-analysis of 1048 patients revealed that the EPC route was associated with a lower incidence of PSH[9], congruent with our findings. However, other investigators reported no significant differences between the two routes[26,31], potentially due to variations in surgical techniques or differences in follow-up durations. The literature presents varying perspectives on the clinical relevance of the EPC. While some authors argued that it exerted minimal impact on PSH incidence[32], others advocated for it as the preferred method for patients who required a permanent iliac colostomy[33]; in a more recent study, the authors continued to consider EPC as a viable option for such cases[34].
Although we did not uncover any differences in the rates of necrosis (P = 0.61), ischemia (P = 0.29), edema (P = 0.74), or infection (P = 0.38), the EPC group demonstrated significantly lower incidences of prolapse (P = 0.007), stoma retraction
Impaired blood supply during stoma formation can lead to ischemia and necrosis, complications that are more com
The limitations we identified in our study include a predominance of RS over RCT, potentially limiting the power to adequately compare complications with low incidence rates. Additionally, there was variability in the selection of colo
In conclusion, the extraperitoneal route emerges as a promising strategy that can be implemented to mitigate specific stoma-related complications such as PSH and other related complications in colostomy surgery. By considering the extraperitoneal route, healthcare providers may be able to minimize the incidence of these complications, and this will ultimately lead to improved patient outcomes and quality of care. However, further research and ongoing assessment are necessary to confirm and build upon these findings, to improve patient care and treatment outcomes in the area of colo
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55735] [Article Influence: 7962.1] [Reference Citation Analysis (132)] |
| 2. | Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1570] [Cited by in RCA: 2986] [Article Influence: 497.7] [Reference Citation Analysis (3)] |
| 3. | Simillis C, Baird DL, Kontovounisios C, Pawa N, Brown G, Rasheed S, Tekkis PP. A Systematic Review to Assess Resection Margin Status After Abdominoperineal Excision and Pelvic Exenteration for Rectal Cancer. Ann Surg. 2017;265:291-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | van der Linden YT, Boersma D, Bosscha K, Lips DJ, Prins HA. Use of a multi-instrument access device in abdominoperineal resections. J Minim Access Surg. 2016;12:248-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Gopall J, Shen XF, Cheng Y. Current status of laparoscopic total mesorectal excision. Am J Surg. 2012;203:230-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Eftaiha SM, Pai A, Sulo S, Park JJ, Prasad LM, Marecik SJ. Robot-Assisted Abdominoperineal Resection: Clinical, Pathologic, and Oncologic Outcomes. Dis Colon Rectum. 2016;59:607-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Antoniou SA, Agresta F, Garcia Alamino JM, Berger D, Berrevoet F, Brandsma HT, Bury K, Conze J, Cuccurullo D, Dietz UA, Fortelny RH, Frei-Lanter C, Hansson B, Helgstrand F, Hotouras A, Jänes A, Kroese LF, Lambrecht JR, Kyle-Leinhase I, López-Cano M, Maggiori L, Mandalà V, Miserez M, Montgomery A, Morales-Conde S, Prudhomme M, Rautio T, Smart N, Śmietański M, Szczepkowski M, Stabilini C, Muysoms FE. European Hernia Society guidelines on prevention and treatment of parastomal hernias. Hernia. 2018;22:183-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 245] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 8. | Brandsma HT, Hansson BM, Aufenacker TJ, van Geldere D, van Lammeren FM, Mahabier C, Steenvoorde P, de Vries Reilingh TS, Wiezer RJ, de Wilt JH, Bleichrodt RP, Rosman C. Prophylactic mesh placement to prevent parastomal hernia, early results of a prospective multicentre randomized trial. Hernia. 2016;20:535-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Lian L, Wu XR, He XS, Zou YF, Wu XJ, Lan P, Wang JP. Extraperitoneal vs. intraperitoneal route for permanent colostomy: a meta-analysis of 1,071 patients. Int J Colorectal Dis. 2012;27:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Wang FB, Pu YW, Zhong FY, Lv XD, Yang ZX, Xing CG. Laparoscopic permanent sigmoid stoma creation through the extraperitoneal route versus transperitoneal route. A meta-analysis of stoma-related complications. Saudi Med J. 2015;36:159-163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Hamada M, Nishioka Y, Nishimura T, Goto M, Furukita Y, Ozaki K, Nakamura T, Fukui Y, Taniki T, Horimi T. Laparoscopic permanent sigmoid stoma creation through the extraperitoneal route. Surg Laparosc Endosc Percutan Tech. 2008;18:483-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11206] [Cited by in RCA: 11011] [Article Influence: 688.2] [Reference Citation Analysis (0)] |
| 13. | Heiying J, Yonghong D, Xiaofeng W, Hang Y, Kunlan W, Bei Z, Jinhao Z, Qiang L. A study of laparoscopic extraperitoneal sigmoid colostomy after abdomino-perineal resection for rectal cancer. Gastroenterol Rep (Oxf). 2014;2:58-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Whittaker M, Goligher JC. A comparison of the results of extraperitoneal and intraperitoneal techniques for construction of terminal iliac colostomies. Dis Colon Rectum. 1976;19:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Hamada M, Ozaki K, Muraoka G, Kawakita N, Nishioka Y. Permanent end-sigmoid colostomy through the extraperitoneal route prevents parastomal hernia after laparoscopic abdominoperineal resection. Dis Colon Rectum. 2012;55:963-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Leroy J, Diana M, Callari C, Barry B, D'Agostino J, Wu HS, Marescaux J. Laparoscopic extraperitoneal colostomy in elective abdominoperineal resection for cancer: a single surgeon experience. Colorectal Dis. 2012;14:e618-e622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Hino H, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, Numata M, Furutani A, Suzuki T, Torii K. Relationship between stoma creation route for end colostomy and parastomal hernia development after laparoscopic surgery. Surg Endosc. 2017;31:1966-1973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Xiao J, Shen Y, Yang X, Zeng H, Wei M, Meng W, Wang Z. The same parastomal hernia repairs rate in the different approaches to colostomy. J Surg Oncol. 2023;128:304-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Zhang X, Li X, Cheng Z, Wang K, Dai Y, Wang Y. Modified Approach for Extraperitoneal Colostomy Creation in Laparoscopic Abdominoperineal Resection. Dis Colon Rectum. 2024;67:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 20. | Ota E, Yamaguchi T, Nagasaki T, Fukuoka H, Mukai T, Hiyoshi Y, Konishi T, Akiyoshi T, Fukunaga Y. Laparoscopic extraperitoneal colostomy has a lower risk of parastomal hernia and bowel obstruction than transperitoneal colostomy. Int J Colorectal Dis. 2022;37:1429-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Liao X, Li X, Cheng J, Zhang Y, Ding K, Li X. Extraperitoneal colostomy after laparoscopic abdominoperineal resection using a cannula for tunnel creation through a trocar port. Surg Endosc. 2022;36:3178-3182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Wang P, Liang J, Zhou H, Wang Z, Shi L, Zhou Z. Extraperitoneal sigmoidostomy: a surgical approach with less complications and better functions for abdominoperineal resection of rectal cancer. Int J Colorectal Dis. 2018;33:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Yao HL, Liu JP, Sun CH, Wang CJ, Li Y, Li L, Zhao B, Liu J. Application of Pelvic Peritoneum Closure Combined with Extraperitoneal Colostomy in Laparoscopic Surgery for Low Rectal Cancer. Proc Anticancer Res. 2023;7:29-37. [DOI] [Full Text] |
| 24. | Wang F, Sun X, Nie S, Fei J. Extraperitoneal sigmoidostomy after laparoscopic abdominoperineal resection: A single-center 6-year experience. Asian J Surg. 2024;47:2214-2215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Dong LR, Zhu YM, Xu Q, Cao CX, Zhang BZ. Clinical evaluation of extraperitoneal colostomy without damaging the muscle layer of the abdominal wall. J Int Med Res. 2012;40:1410-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Marks CG, Ritchie JK. The complications of synchronous combined excision for adenocarcinoma of the rectum at St Mark's Hospital. Br J Surg. 1975;62:901-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 41] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Kroese LF, de Smet GH, Jeekel J, Kleinrensink GJ, Lange JF. Systematic Review and Meta-Analysis of Extraperitoneal Versus Transperitoneal Colostomy for Preventing Parastomal Hernia. Dis Colon Rectum. 2016;59:688-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Luo J, Singh D, Zhang F, Yang X, Zha X, Jiang H, Yang L, Yang H. Comparison of the extraperitoneal and transperitoneal routes for permanent colostomy: a meta-analysis with RCTs and systematic review. World J Surg Oncol. 2022;20:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 29. | Li Z, Tian L, Liu R, Zheng B, Wang B, Zhao X, Quan P, Qiu J. A technique for laparoscopic extraperitoneal colostomy with an intact posterior sheath of rectus. BMC Surg. 2022;22:239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 30. | Akamoto S, Imura S, Fujiwara Y, Habu K, Konishi Y, Fukuhara T, Nakagawa K. Extraperitoneal colostomy in robotic surgery for rectal cancer using a tip-up fenestrated grasper. Asian J Endosc Surg. 2021;14:636-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Williams JG, Etherington R, Hayward MW, Hughes LE. Paraileostomy hernia: a clinical and radiological study. Br J Surg. 1990;77:1355-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Zhang T, Yang D, Sun G, Zhang D. Modified technique of extraperitoneal colostomy without incision of the posterior rectus sheath. Sci Rep. 2021;11:2857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Seyfried S, Lucas V, Galata C, Reißfelder C, Weiß C, Kienle P, Hardt J. Incisional hernia rate after ileostomy closure in lateral pararectal stoma versus transrectal stoma placement: follow-up of the randomized PATRASTOM trial. Colorectal Dis. 2020;22:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Fairclough E, Segar J, Breeman S, Smith A, Myers J, Reid F. Does variation of surgical technique affect native tissue anterior pelvic organ prolapse repair outcomes? Int Urogynecol J. 2024;35:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 35. | Krishnamurty DM, Blatnik J, Mutch M. Stoma Complications. Clin Colon Rectal Surg. 2017;30:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 36. | GOLIGHER JC. Extraperitoneal colostomy or ileostomy. Br J Surg. 1958;46:97-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 37. | Shellito PC. Complications of abdominal stoma surgery. Dis Colon Rectum. 1998;41:1562-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 183] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 38. | Arumugam PJ, Bevan L, Macdonald L, Watkins AJ, Morgan AR, Beynon J, Carr ND. A prospective audit of stomas--analysis of risk factors and complications and their management. Colorectal Dis. 2003;5:49-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 227] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 39. | Park JJ, Del Pino A, Orsay CP, Nelson RL, Pearl RK, Cintron JR, Abcarian H. Stoma complications: the Cook County Hospital experience. Dis Colon Rectum. 1999;42:1575-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 211] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 40. | Franklyn J, Varghese G, Mittal R, Rebekah G, Jesudason MR, Perakath B. A prospective randomized controlled trial comparing early postoperative complications in patients undergoing loop colostomy with and without a stoma rod. Colorectal Dis. 2017;19:675-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 41. | Miyo M, Takemasa I, Ikeda M, Tujie M, Hasegawa J, Ohue M, Kato T, Mizushima T, Doki Y, Mori M. The influence of specific technical maneuvers utilized in the creation of diverting loop-ileostomies on stoma-related morbidity. Surg Today. 2017;47:940-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 42. | Sung YH, Kwon I, Jo S, Park S. Factors affecting ostomy-related complications in Korea. J Wound Ostomy Continence Nurs. 2010;37:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 43. | Abd El-Aal W, Saied A, Hosny Bendary S, Mohammed Abdul-mohaymen A. Complications of colostomy after colorectal surgery. Al-Azhar Med J. 2020;49:1561-1970. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 44. | Kann BR. Early stomal complications. Clin Colon Rectal Surg. 2008;21:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 45. | Benedek Z, Kocsis L, Bauer O, Suciu N, Sorlea S, Crăciun C, Georgescu R, Coroș MF. Stoma-Related Complications: A Single-Center Experience and Literature Review. J Interdiscip Med. 2022;7:31-37. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |