Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.103953
Revised: January 10, 2025
Accepted: January 21, 2025
Published online: March 27, 2025
Processing time: 81 Days and 15.8 Hours
In hemorrhoidal disease, despite the existence of numerous treatment options to alleviate symptoms, surgical intervention continues to be the gold standard. The advantages and disadvantages of many methods have been shown in numerous studies However, only a few studies have compared the effectiveness of combined methods.
To compare the results of a coloproctology clinic that switched to the Doppler-guided hemorrhoidal artery ligation (DG-HAL) + Ferguson hemorrhoidectomy (FH) technique from the FH in the treatment of hemorrhoidal disease.
In this retrospective cohort, data from a total of 45 patients who underwent DG-HAL + FH (n = 24) and FH (n = 21) for grade III hemorrhoidal disease between 2020 and 2022 were analyzed. Demographic and clinical data, surgical duration, intraoperative blood loss, hospital stay, postoperative analgesic consumption, pain scores using the Visual Analog Scale (VAS), complications, time to return to normal activities, and the recurrence rate were compared in both groups.
The study included 45 patients, with 75.6% (n = 34) male and 24.4% (n = 11) female. The rate of intraoperative blood loss was higher in the FH group (P < 0.05). The VAS scores and postoperative complication rates were similar in both groups. The need for postoperative analgesics was lower in the DG-HAL + FH group (2 vs 4 days, P < 0.05), while the FH group showed a shorter time to return to normal activities (9.5 vs 6.0 days, P = 0.02). The recurrence rate (16.7% vs 0%) and Clavien–Dindo Score-1 complications (20.8% vs 9.5%, P = 0.29) were higher in the DG-HAL + FH group but were insignificant.
Our study revealed that the addition of the DG-HAL to classical hemorrhoidectomy caused less intraoperative bleeding and a lower postoperative analgesia requirement.
Core Tip: In the contemporary treatment of hemorrhoidal disease, there is a broad spectrum of methods ranging from conservative treatments to stapled hemorrhoidectomy. The purpose of choosing combined therapy was to avoid undesirable complications such as pain and anal stenosis associated with conventional hemorrhoidectomies and to prevent potential tissue and sensory loss. We thought that non-invasive methods like Doppler or laser pexy might not be sufficient in some cases, while excision could be beneficial for prolapsed hemorrhoids. In this study, we compared the combined Ferguson approach [Ferguson + Doppler-guided hemorrhoidal artery ligation (DG-HAL)] with Ferguson hemorrhoidectomy only. We found that the duration of postoperative analgesic need was significantly lower in the DG-HAL + hemorrhoidectomy group, and the return to normal activity was quicker in Ferguson hemorrhoidectomy group.
- Citation: Eray IC, Topal U, Gumus S, Isiker K, Yavuz B, Aydin I. Comparative analysis of Ferguson hemorrhoidectomy combined with doppler-guided hemorrhoidal artery ligation and Ferguson hemorrhoidectomy in hemorrhoidal disease treatment. World J Gastrointest Surg 2025; 17(3): 103953
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/103953.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.103953
Hemorrhoids, identifiable as "vascular cushions" in the anorectal component contributing to the physiological continence mechanism, can expand due to various reasons, leading to hemorrhoidal disease characterized by symptoms such as bleeding, pain, and itching. Hemorrhoidal disease is a common and life quality-diminishing issue in society. Due to many cases being asymptomatic, its exact prevalence is unknown. The prevalence in the adult population varies from 4% to 45%, making hemorrhoidal disease the most frequent reason for proctology consultations, and it is found in up to 70% of the working population[1,2].
In hemorrhoidal disease, despite the existence of numerous treatment options to alleviate symptoms, surgical intervention continues to be the gold standard, particularly for grade 3-4 hemorrhoidal disease which is resistant to conservative treatment, according to the Goligher classification. Open hemorrhoidectomy (Milligan–Morgan) or closed hemorrhoidectomy (Ferguson) is one of the most commonly utilized operations[3-5]. However, this operation is as
Theoretically, Doppler-guided hemorrhoidal artery ligation (DG-HAL) is a procedure where hemorrhoidal arteries are ligated using a device aided by a Doppler-equipped anoscope. Through adding mucopexy, this technique aims to prevent prolapse of the hemorrhoidal and mucosal tissue. This technique is also called DG-HAL + recto anal repair. It has been proposed as an effective and painless technique for treating symptomatic grade 2 and 3 hemorrhoids with minimal mucosal prolapse[11].
Debates continue regarding the selection of a treatment for hemorrhoidal disease. The advantages and disadvantages of many methods have been shown in numerous studies[12-15]. However, only a few studies have compared the effectiveness of combined methods[3,5,16]. There is a lack of studies in the literature comparing the efficacy and outcomes of combined DG-HAL+ Ferguson hemorrhoidectomy (FH) vs FH alone.
This study compared the DG-HAL + FH vs the classic FH technique in treating hemorrhoidal disease.
This study was conducted by a National and International Board-certified coloproctologist in the colorectal surgery unit of a university hospital where more than 400 colorectal surgical procedures are performed annually. The ethics committee approval for writing the article was received from the Cukurova University Faculty of Medicine Ethics Committee in November 2023 (Approval No: 138).
The study included patients who applied to the coloproctology clinic between 01 January, 2020 and 30 December, 2022. The device/proctoscope with a Doppler converter (Angiodin-proctor by Comepa) began to be routinely used in our clinic on 15 June, 2021. Before this date (from 01 January, 2020 to 15 June, 2021), FH was performed routinely. Since the provision of the Doppler device, either DG-HAL or DG-HAL+FH have been routinely used for the treatment of grade 2 and 3 hemorrhoids.
Inclusion criteria: Patients aged between 18 and 65 years with grade 3 hemorrhoidal disease that did not respond to medical treatment or lifestyle changes were included in the study. Patients who underwent only FH or DG-HAL + FH were included in the study.
Exclusion criteria: Patients with a history of anorectal surgery or benign proctological diseases (e.g., perianal fistula, rectal prolapse, anal fissure, fecal incontinence, or anal stenosis) were excluded. Patients who underwent stapled hemorrhoidopexy, laser hemorrhoidopexy, or Milligan–Morgan hemorrhoidectomy were excluded from the study. Patients with grade 1-2-4 hemorrhoidal diseases were excluded. Patients who underwent only DG-HALs (without excisional hemorrhoidectomy) for grade 2 hemorrhoidal disease were also excluded from the study.
The patients were divided into groups based on the surgical treatment received: Group 1 (DG-HAL + FH) and group 2 (FH alone).
Preoperative colonoscopy or sigmoidoscopy was performed on patients in the colorectal screening age groups defined by the Turkish Ministry of Health and those suspected of having rectal cancer (due to age, presence of tenesmus, or a family history of colorectal cancer).
All patients received a phosphate enema approximately 3 hours before surgery. Antibiotic prophylaxis with 500 mg metronidazole was administered in the operating room.
All surgical procedures were performed by the same surgeon experienced in coloproctological surgery. The surgeries were performed under standard spinal anesthesia, with the patient in the lithotomy position.
FH was performed using the standard technique described in the literature, with the excision of the hemorrhoidal tissue carried out using electrocautery and closure of the excised hemorrhoidal tissue sites using absorbable sutures.
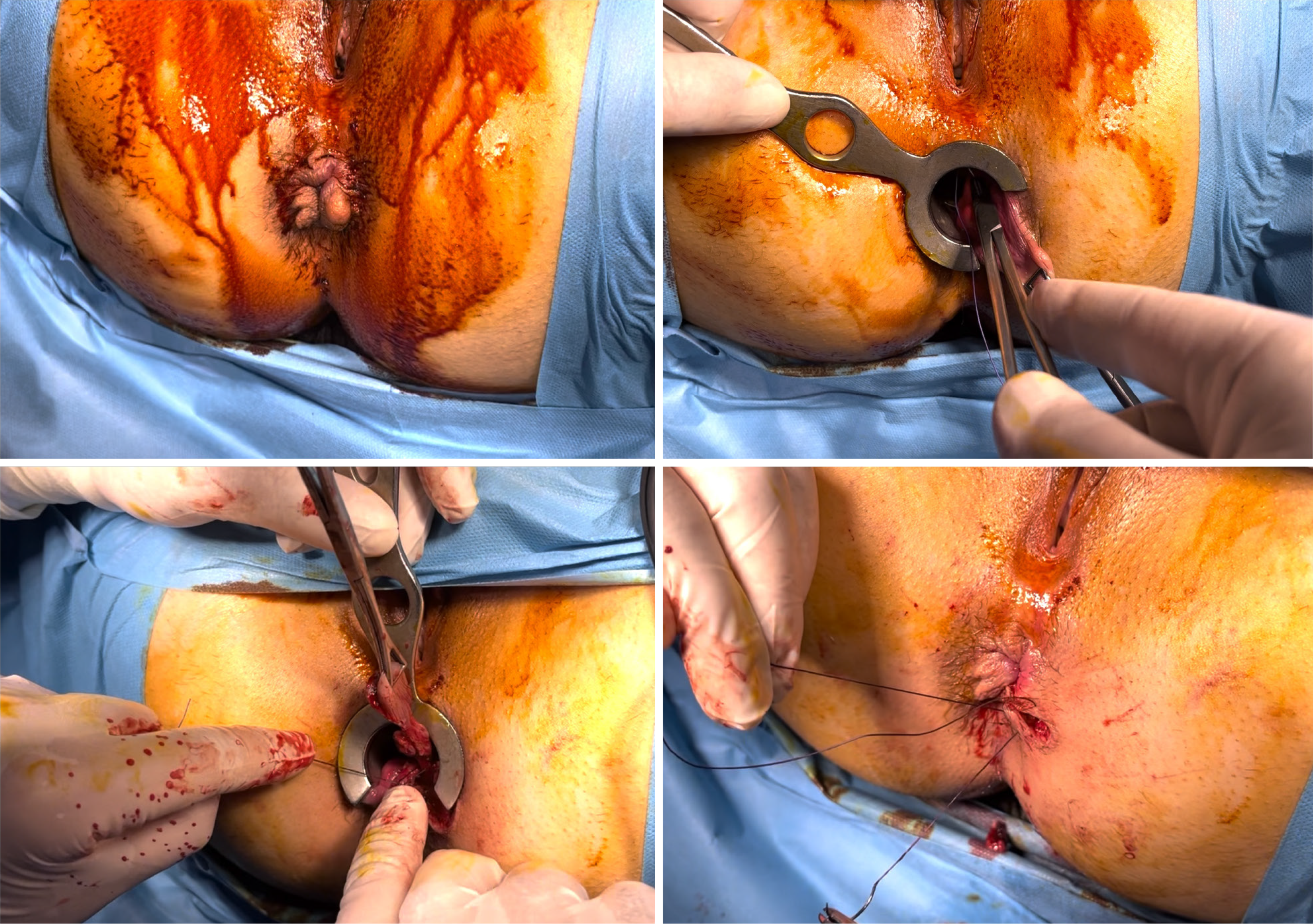
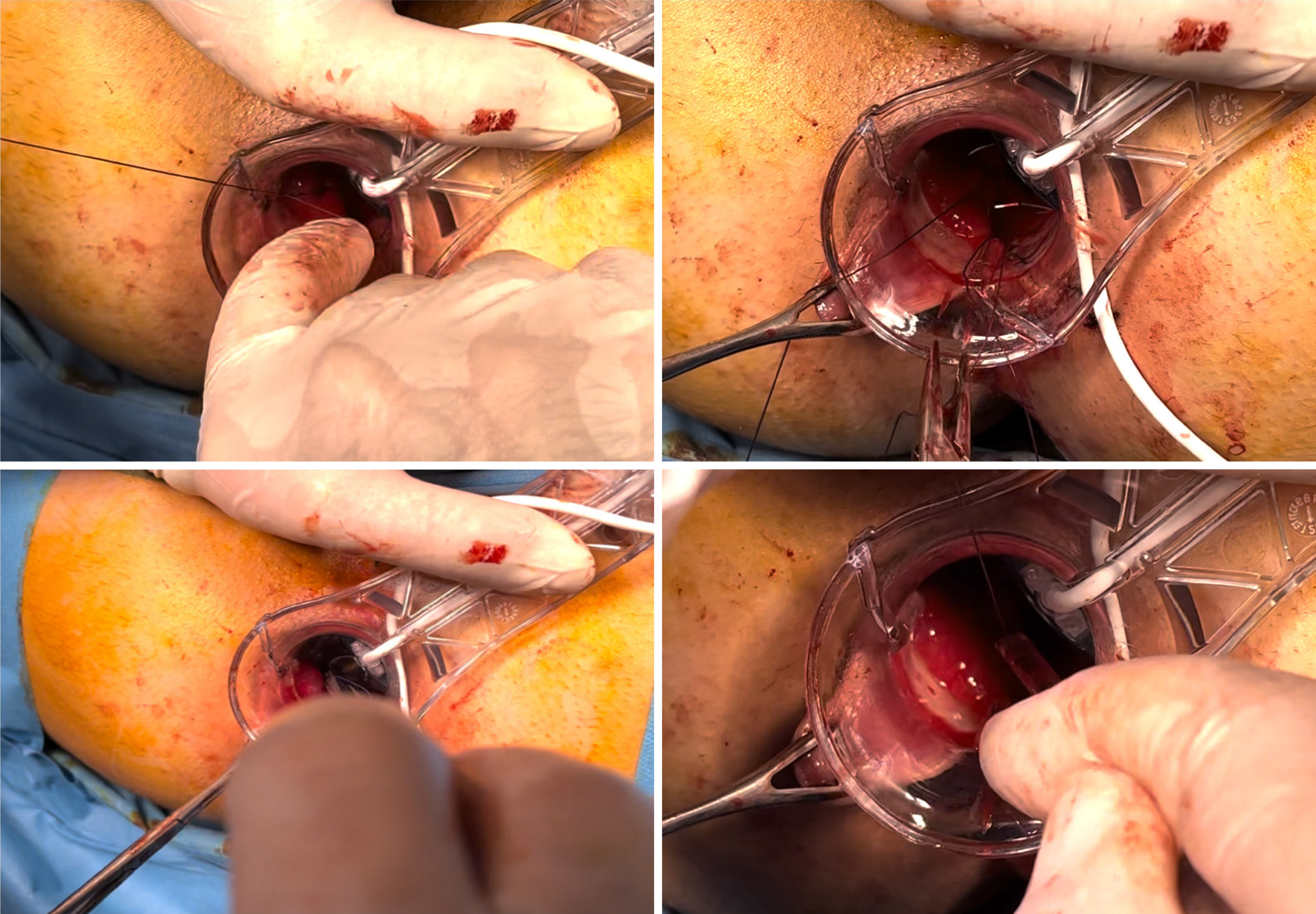
In the combined method (DG-HAL + FH), 1 or 2 dominant and prolapsed hemorrhoid piles were excised using the Ferguson technique (Figure 1), followed by DG-HAL on 1 or 2 piles. In cases where DG-HAL was performed as part of the combined procedure, the larger pile was designated as the dominant one and excised, while ligation was applied to the other piles. A maximum of three piles were treated for each patient in all groups. For DG-HAL, a special device/proctoscope with a Doppler converter was inserted into the anal canal and distal rectum (Figure 2). After placement, each branch was tied approximately 3-4 cm above the dentate line with a 2-0 absorbable polyglycolic acid suture, and the device was rotated clockwise to locate other arteries at that level. After a full rotation, the procedure was repeated up to 0.5-1 cm below the first series of sutures. Continuous sutures, becoming more superficial towards the dentate line, were placed, starting 3 cm proximal to the dentate line and ending 0.5 cm to the dentate line in patients with prolapsed hemorrhoids and/or rectal mucosal prolapse and tied to complete the mucopexy.
Post-discharge management included dietary modifications (e.g., stool softeners, adequate fluid intake with fiber supplements) and standard medical treatment. Venotonics were routinely prescribed.
After discharge, patients were routinely assessed on the 14th post-operative day in the outpatient clinic. Digital rectal examinations and/or rectoscopy were performed within 3-6 months to check for recurrences. Telephone interviews were conducted to assess the patients' last status one year after the surgery.
Demographic data such as age and gender were compared. Key performance indicators included intraoperative blood loss, length of hospital stay, postoperative analgesic requirement, and time to return to normal daily activities. Visual analog scale (VAS) scores were prospectively recorded after every procedure. The patients scored (0 = no pain, 10 = worse pain) the average pain and the pain after defecation. Early postoperative complications were classified according to the Clavien-Dindo (CD) scale. Urinary retention and tenesmus were classified as CD-1.
Statistical analysis was conducted using the SPSS v24 (IBM) software. Numerical variables are presented with their mean and standard deviation or median, minimum, and maximum values, while categorical variables are expressed in terms of counts and percentages. For group comparisons, the χ2 test was used to analyze categorical variables, while the Mann–Whitney U-test was applied for non-normally distributed continuous variables. Changes in VAS scores between days 1 and 7 within groups were evaluated using the Wilcoxon signed-rank test. A P value less than 0.05 was considered statistically significant.
A total of 45 consecutive patients were enrolled in the study. Of these patients, 75.6% (n = 34) were male, and 24.4% (n = 11) were female. In total, 53.3% (n = 24) of the patients underwent DG-HAL + FH, while 46.7% (n = 21) underwent FH. The demographic and clinical data are shown in Table 1.
| DG-HAL + hemorrhoidectomy (n = 24) | Ferguson hemorrhoidectomy (n = 21) | P value | ||
| Age | 51.9 ± 13.7 | 45.1 ± 14.1 | 0.08 | |
| Gender | Male | 18 (75.0) | 16 (76.2) | 0.63 |
| Female | 6 (25.0) | 5 (23.8) | ||
The rate of intraoperative blood loss was lower in the DG-HAL + FH group (10 vs 20 mL, P = 0.004), and the days needed for postoperative analgesics were lower (2 vs 4 days, P < 0.05). The first and seventh-day VAS scores were similar in both groups. Clavien-Dindo Score-1 complications were higher in the DG-HAL + FH group (20.8% vs 9.5%), and most of them were urinary retention (16.7% vs 4.8%), but these were not statistically significant. The time to return to normal activities was higher in the DG-HAL + FH group (9.5 vs 6 days, P < 0.05). Recurrence occurred in four of the DG-HAL + FH group, but there was no recurrence in the FH group. Operative and postoperative follow-up data are shown in Table 2. There was no anal stenosis or incontinence in follow-up.
| DG-HAL + hemorrhoidectomy (n = 24) | Ferguson hemorrhoidectomy (n = 21) | P value | ||
| Intraoperative blood loss (mL) | 10 (10-90) | 20 (20-80) | 0.004 | |
| Hospital stays duration (days) | 1 (1-3) | 1 (1-4) | 0.08 | |
| Day 1 VAS score | 2 (0-8)a | 2 (0-10)a | 0.06 | |
| Day 7 VAS score | 0 (0-8) | 0 (0-8) | 0.85 | |
| Postoperative analgesic need (days) | 2 (1-10) | 4 (2-12) | 0.02 | |
| Return to normal activity (days) | 9.50 (4.00-20.00) | 6.00 (1.00-20.00) | 0.02 | |
| Postoperative complications | Yes | 5 (20.8) | 2 (9.5) | 0.29 |
| No | 19 (79.2) | 19 (90.5) | ||
| Complication | Urinary retention | 4 (16.7) | 1 (4.8) | 0.45 |
| Tenesmus | 1 (4.2) | 1 (4.8) | ||
| None | 19 (79.2) | 19 (90.5) | ||
| Clavien-Dindo Score | 0 | 19 (79.2) | 19 (90.5) | 0.29 |
| 1 | 5 (20.8) | 2 (9.5) | ||
| Recurrence | Yes | 4 (16.7) | 0 (0) | 0.111 |
| No | 20 (83.3) | 21 (100) | ||
In the contemporary treatment of hemorrhoidal disease, there is a broad spectrum of methods ranging from conservative treatments to stapled hemorrhoidopexy. Excisional hemorrhoidectomy procedures are still the preferred treatment methods for grade 3-4 hemorrhoidal disease; however, they have specific adverse effects. Anal stenosis, incontinence, and postoperative pain, particularly after multiple excisions, can be troublesome for both the patient and the surgeon. Combined methods may help to prevent these undesirable side effects. Although limited literature studies have compared DG-HAL with stapled hemorrhoidopexy or mucopexy combinations, no study has compared DG-HAL + FH with FH. This study compared the reference close hemorrhoidectomy procedure Ferguson approach with combined DG-HAL + FH, and it was concluded that adding DG-HAL to FH resulted in less operative bleeding and a lower postoperative analgesic requirement.
Postoperative bleeding is a common and troublesome complication following hemorrhoidal surgery, typically categorized as either immediate or delayed [12,17,18]. A systematic review involving about 2000 patients showed that there was significantly less intra- and postoperative bleeding compared to the open technique[19]. Similarly, a meta-analysis comparing DG-HAL with stapled hemorrhoidectomy found a lower rate of postoperative bleeding in the DG-HAL group[20]. Another meta-analysis reported no significant difference in bleeding rates between DG-HAL and FH (OR: 0.41; 95%CI: 0.16, 1.05; Z = 1.87; P = 0.06)[21]. Therefore, incorporating interventions that have been proven beneficial in classical hemorrhoidectomy can reduce postoperative bleeding. In our series, we observed a significant difference in the rate of intraoperative bleeding between both groups.
The primary factor driving the search for alternative treatments following classical excision-based methods for hemorrhoidal disease is postoperative pain. Despite their cost, the development and preference for techniques such as DG-HAL are largely due to their ability to reduce pain[2]. Pain, although subjective and individual-specific, is often assessed using the validated VAS, a widely accepted method in current studies[22]. In a study by Lim et al[12], compared with the DG-HAL +/- laser hemorrhoidoplasty, no significant clinical or statistical difference was found in pain scores between the groups, as both are minimally invasive and non-excisional procedures. Poskus et al[13] have reported that both laser and mucopexy, when compared to excisional hemorrhoidectomy, were associated with lower postoperative pain scores. In a study by Long et al[5], when comparing the FH with the Milligan-Morgan Hemorrhoidectomy (MMH) + non-Doppler HAL, the MMH + non-Doppler HAL group had lower VAS scores at first defecation and at various postoperative intervals (12 hours, 1 day, 2 days, 3 days, and 7 days) and consumed fewer analgesics within 7 days compared to the FH group (P < 0.05), suggesting that MMH + NDG-HAL effectively alleviates surgical incision pain and reduces the need for analgesics. Based on these studies, it can be inferred that combined methods could potentially reduce pain. In our study, DG-HAL reduced the need for postoperative analgesia use compared to the FH group. This may be due to less surgical trauma in the DG-HAL group.
Another critical aspect in the selection of a treatment for hemorrhoidal disease is the time to return to daily activities, which is as important as pain and bleeding. While return-to-work times can extend up to a week following conventional methods, non-excisional procedures have reduced this period to as short as one day. The rapid return to work and quicker healing offered by minimally invasive methods compared to excisional methods are reasons for their preference[3,23]. The duration to resume daily activities is multifactorial, with postoperative pain and other complications being key factors prolonging this period. In a study by Abdelhamid et al[3], patients who underwent minimally invasive procedures such as combined hemorrhoidal artery ligation, returned to their daily activities sooner than those who had a FH. Similarly, Brusciano et al[24] showed this was associated with an earlier return to daily activities. Furthermore, Poskus et al[13] reported that both laser and mucopexy were associated with an earlier return to work compared to surgical excision. In contrast, our study did not show an early return-to-work advantage. This difference may be due to various factors, including the edema and/or inflammation in the rectal mucosal and submucosal layers caused by mucopexy, which can still be managed effectively with anti-inflammatory drugs and analgesics[24].
The most common postoperative complication is acute urinary retention, with rates up to 20%[25-27]. In our study, the urinary retention rate was similar in both groups. Adding DG-HAL to FH created a minimal increase in urinary retention but did not create a statistical difference. This may be due to the slightly longer operative duration of the DG-HAL + FH procedure or larger anoscope diameter, which may result in more significant sympathetic–parasympathetic nerve discordance. However, it is not easy to provide evidence to confirm this. This needs to be further investigated in more extensive patient series.
The effect of choosing combined methods on the long-term results should also be discussed. We observed more recurrences in the combined method. A randomized controlled trial by Aigner et al. compared DG-HAL with suture mastopexy vs suture mucopexy alone in treating grade III hemorrhoids. They examined 40 patients in two groups and found that patients who received DG-HAL had less pain but a higher long-term recurrence rate (10% vs 5%; P = 0.274)[28]. This was similar to the results of our study. On the other hand, there are contrary data about the recurrence rate, such as the randomized study which compared open hemorrhoidectomy with Doppler-guided hemorrhoid dearterialization and mucopexy; the results after a 1-year follow-up did not show any difference in relapse between the two groups[25].
The purpose of choosing the combined treatment was to avoid the unwanted complications of conventional hemorrhoidectomies, such as pain and anal stenosis, and to prevent unnecessary tissue and sensory loss. As the literature suggests that methods such as DG-HAL alone may be insufficient for grade 4 hemorrhoids, we have not yet started routinely applying them to grade 4, but we choose minimally invasive procedures in lower stages (DG-HAL alone for grade 2 disease and DG-HAL + FH for grade 3). As our case series grows, new results may lead us to return to the classical surgical method or suggest standardization of combined methods. In any case, developing new techniques or procedures in treating hemorrhoidal disease is essential due to the lack of a standardized technique.
Our study, being single-centered and retrospective, has its limitations. Retrospective studies are inherently prone to bias as confounding variables may not be equally distributed across groups. However, we believe that the scarcity of data in the existing literature making the same comparisons as our research is a significant advantage in our favor. According to Goligher, internal hemorrhoidal disease is divided into four stages. However, the fact that hemorrhoidal disease can be seen in different stages in the same patient may limit the standardization of surgical techniques. The findings from this study should be interpreted in the context of the limitations mentioned in the Discussion. They should be verified in future studies with larger sample sizes and randomized controlled trials.
Our study concluded that combining DG-HAL with FH may result in less intraoperative bleeding and less postoperative analgesia use.
| 1. | Carvajal López F, Hoyuela Alonso C, Juvany Gómez M, Troyano Escribano D, Trias Bisbal MA, Martrat Macià A, Ardid Brito J. Prospective Randomized Trial Comparing HAL-RAR Versus Excisional Hemorrhoidectomy: Postoperative Pain, Clinical Outcomes, and Quality of Life. Surg Innov. 2019;26:328-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Boerhave NHP, Klicks RJ, Dogan K. The efficacy of laser haemorrhoidoplasty (LHP) in the treatment of symptomatic haemorrhoidal disease: An observational cohort study. Colorectal Dis. 2023;25:1202-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Abdelhamid AF, Elsheikh MM, Abdraboh OH. Laser hemorrhoidoplasty combined with blind hemorrhoidal artery ligation compared to Milligan–Morgan hemorrhoidectomy in patients with second and third degree piles; a prospective randomized study. Egypt J Surg. 2023;42:669-675. [DOI] [Full Text] |
| 4. | De Schepper H, Coremans G, Denis MA, Dewint P, Duinslaeger M, Gijsen I, Haers P, Komen N, Remue C, Roelandt P, Somers M, Surmont M, Van de Putte D, Van den Broeck S, Van Kemseke C, De Looze D. Belgian consensus guideline on the management of hemorrhoidal disease. Acta Gastroenterol Belg. 2021;84:101-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Long Q, Wen Y, Li J. Milligan-Morgan hemorrhoidectomy combined with non-doppler hemorrhoidal artery ligation for the treatment of grade III/IV hemorrhoids: a single centre retrospective study. BMC Gastroenterol. 2023;23:293. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Bhatti MI, Sajid MS, Baig MK. Milligan-Morgan (Open) Versus Ferguson Haemorrhoidectomy (Closed): A Systematic Review and Meta-Analysis of Published Randomized, Controlled Trials. World J Surg. 2016;40:1509-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Tan VZZ, Peck EW, Sivarajah SS, Tan WJ, Ho LML, Ng JL, Chong C, Aw D, Mainza F, Foo FJ, Koh FH. Systematic review and meta-analysis of postoperative pain and symptoms control following laser haemorrhoidoplasty versus Milligan-Morgan haemorrhoidectomy for symptomatic haemorrhoids: a new standard. Int J Colorectal Dis. 2022;37:1759-1771. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Gambardella C, Brusciano L, Brillantino A, Parisi S, Lucido FS, Del Genio G, Tolone S, Allaria A, Di Saverio S, Pizza F, Sturiale A, Docimo L. Mid-term efficacy and postoperative wound management of laser hemorrhoidoplasty (LHP) vs conventional excisional hemorrhoidectomy in grade III hemorrhoidal disease: the twisting trend. Langenbecks Arch Surg. 2023;408:140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 9. | Plapler H, Hage R, Duarte J, Lopes N, Masson I, Cazarini C, Fukuda T. A new method for hemorrhoid surgery: intrahemorrhoidal diode laser, does it work? Photomed Laser Surg. 2009;27:819-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Longchamp G, Liot E, Meyer J, Toso C, Buchs NC, Ris F. Non-excisional laser therapies for hemorrhoidal disease: a systematic review of the literature. Lasers Med Sci. 2021;36:485-496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Ram E, Bachar GN, Goldes Y, Joubran S, Rath-Wolfson L. Modified Doppler-guided laser procedure for the treatment of second- and third-degree hemorrhoids. Laser Ther. 2018;27:137-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Lim SY, Rajandram R, Roslani AC. Comparison of post-operative bleeding incidence in laser hemorrhoidoplasty with and without hemorrhoidal artery ligation: a double-blinded randomized controlled trial. BMC Surg. 2022;22:146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Poskus T, Danys D, Makunaite G, Mainelis A, Mikalauskas S, Poskus E, Jotautas V, Dulskas A, Jasiunas E, Strupas K. Results of the double-blind randomized controlled trial comparing laser hemorrhoidoplasty with sutured mucopexy and excisional hemorrhoidectomy. Int J Colorectal Dis. 2020;35:481-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 14. | Watson AJ, Hudson J, Wood J, Kilonzo M, Brown SR, McDonald A, Norrie J, Bruhn H, Cook JA; eTHoS study group. Comparison of stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease (eTHoS): a pragmatic, multicentre, randomised controlled trial. Lancet. 2016;388:2375-2385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 15. | Brown SR, Tiernan JP, Watson AJM, Biggs K, Shephard N, Wailoo AJ, Bradburn M, Alshreef A, Hind D; HubBLe Study team. Haemorrhoidal artery ligation versus rubber band ligation for the management of symptomatic second-degree and third-degree haemorrhoids (HubBLe): a multicentre, open-label, randomised controlled trial. Lancet. 2016;388:356-364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 121] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 16. | Yanar F, Abbasov A, Ilhan B, Ozcınar B, Yanar H. The New Technique in Hemorrhoid Disease: A Combination of Laser Hemorrhoidoplasty and Ferguson Hemorrhoidectomy. 2022 Preprint. [DOI] [Full Text] |
| 17. | Moult HP, Aubert M, De Parades V. Classical treatment of hemorrhoids. J Visc Surg. 2015;152:S3-S9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Ng KS, Holzgang M, Young C. Still a Case of "No Pain, No Gain"? An Updated and Critical Review of the Pathogenesis, Diagnosis, and Management Options for Hemorrhoids in 2020. Ann Coloproctol. 2020;36:133-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Lakmal K, Basnayake O, Jayarajah U, Samarasekera DN. Clinical Outcomes and Effectiveness of Laser Treatment for Hemorrhoids: A Systematic Review. World J Surg. 2021;45:1222-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Song Y, Chen H, Yang F, Zeng Y, He Y, Huang H. Transanal hemorrhoidal dearterialization versus stapled hemorrhoidectomy in the treatment of hemorrhoids: A PRISMA-compliant updated meta-analysis of randomized control trials. Medicine (Baltimore). 2018;97:e11502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Xu L, Chen H, Lin G, Ge Q, Qi H, He X. Transanal hemorrhoidal dearterialization with mucopexy versus open hemorrhoidectomy in the treatment of hemorrhoids: a meta-analysis of randomized control trials. Tech Coloproctol. 2016;20:825-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Farrar JT, Berlin JA, Strom BL. Clinically important changes in acute pain outcome measures: a validation study. J Pain Symptom Manage. 2003;25:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 336] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 23. | Song SG, Kim SH. Optimal treatment of symptomatic hemorrhoids. J Korean Soc Coloproctol. 2011;27:277-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Brusciano L, Gambardella C, Terracciano G, Gualtieri G, Schiano di Visconte M, Tolone S, Del Genio G, Docimo L. Postoperative discomfort and pain in the management of hemorrhoidal disease: laser hemorrhoidoplasty, a minimal invasive treatment of symptomatic hemorrhoids. Updates Surg. 2020;72:851-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 25. | Elmér SE, Nygren JO, Lenander CE. A randomized trial of transanal hemorrhoidal dearterialization with anopexy compared with open hemorrhoidectomy in the treatment of hemorrhoids. Dis Colon Rectum. 2013;56:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Giordano P, Tomasi I, Pascariello A, Mills E, Elahi S. Transanal dearterialization with targeted mucopexy is effective for advanced haemorrhoids. Colorectal Dis. 2014;16:373-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Ratto C, Parello A, Litta F, De Simone V. Dearterialization of Hemorrhoids and Mucopexy: Techniques and Results. In: Ratto C, Parello A, Litta F, editors. Hemorrhoids. Cham: Springer, 2018. [DOI] [Full Text] |
| 28. | Aigner F, Kronberger I, Oberwalder M, Loizides A, Ulmer H, Gruber L, Pratschke J, Peer S, Gruber H. Doppler-guided haemorrhoidal artery ligation with suture mucopexy compared with suture mucopexy alone for the treatment of Grade III haemorrhoids: a prospective randomized controlled trial. Colorectal Dis. 2016;18:710-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |