Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.102998
Revised: December 21, 2024
Accepted: January 20, 2025
Published online: March 27, 2025
Processing time: 112 Days and 2.5 Hours
In recent years, the use of ultrafine choledochoscopy has gradually increased in the treatment of cholelithiasis. However, stone incarceration and residual spasm of the sphincter of Oddi may be inevitable when an ultrafine choledochoscope is used alone.
To investigate the safety and feasibility of ultrafine choledochoscopy combined with low-dose atropine in the treatment of Oddi intersphincter stones.
Seventeen patients with Oddi intersphincter stones were retrospectively analyzed. The perioperative clinical data and follow-up information were collected.
Among the 17 patients, 3 were male and 14 were female. The mean age was 40.6 ± 13.9 years, and the mean diameter of the common bile duct was 7.8 ± 1.3 mm. All patients successfully underwent Oddi intersphincter stone removal using a combination of ultrafine choledochoscopy and low-dose atropine. No serious complications, such as postoperative hemorrhage, pancreatitis or bile leakage occurred in the 17 patients. During the one-year follow-up, none of the patients experienced stone recurrence.
Ultrafine choledochoscopy combined with low-dose atropine is safe and feasible for the treatment of Oddi intersphincter stones.
Core Tip: The application of ultrafine choledochoscopy has gradually been used in the treatment of cholelithiasis. However, stone incarceration with residual stones and spasm of the sphincter of Oddi may still occur. We investigated the safety and feasibility of an ultrafine choledochoscope combined with low-dose atropine for the treatment of Oddi intersphincter stones. All 17 patients successfully underwent Oddi intersphincter stone removal using a combination of ultrafine choledochoscopy and low-dose atropine. No serious complications, such as postoperative hemorrhage, pancreatitis or bile leakage occurred. None of the patients experienced stone recurrence during follow-up. Therefore, ultrafine choledochoscopy combined with low-dose atropine is safe and feasible for the treatment of Oddi intersphincter stones.
- Citation: Hu XS, Wang Y, Pan HT, Zhu C, Zhou S, Chen SL, Liu HC, Pang Q, Jin H. Initial experience with ultrafine choledochoscopy combined with low-dose atropine for the treatment of Oddi intersphincter stones. World J Gastrointest Surg 2025; 17(3): 102998
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/102998.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.102998
Choledocholithiasis is a common disease of the biliary system that can cause serious complications such as biliary obstruction, cholangitis and pancreatitis[1,2]. Oddi intersphincter stones represent a special type of choledocholithiasis that is located in the sphincter of Oddi at the terminal common bile duct. Owing to the special anatomical site, it is relatively difficult to remove Oddi intersphincter stones. Traditional treatment methods include endoscopic retrograde cholangiopanchography combined with sphincterotomy and mechanical basket lithotomy under choledoscopy[3,4]. However, the above strategies may result in several problems, such as substantial surgical trauma, high rates of complications and incomplete stone removal[5,6].
In recent years, with the rapid progression of minimally invasive technology, the application of ultrafine choledo
Atropine, an anticholinergic drug, can relax smooth muscle, relieve spasm, and is widely used to treat gastrointestinal spasm. It has also been shown that atropine can relax the sphincter of Oddi[8], facilitating stone removal and improving the success rate of the operation. On the basis of the above theories and techniques, in recent years, we have innovatively applied the combination of an ultrafine choledochoscope and low-dose atropine in the treatment of Oddi intersphincter stones. In this study, we retrospectively analyzed the clinical data of 9 patients who were treated with combination therapy and explored its effectiveness and safety. This information may provide new ideas and methods for clinical treatment.
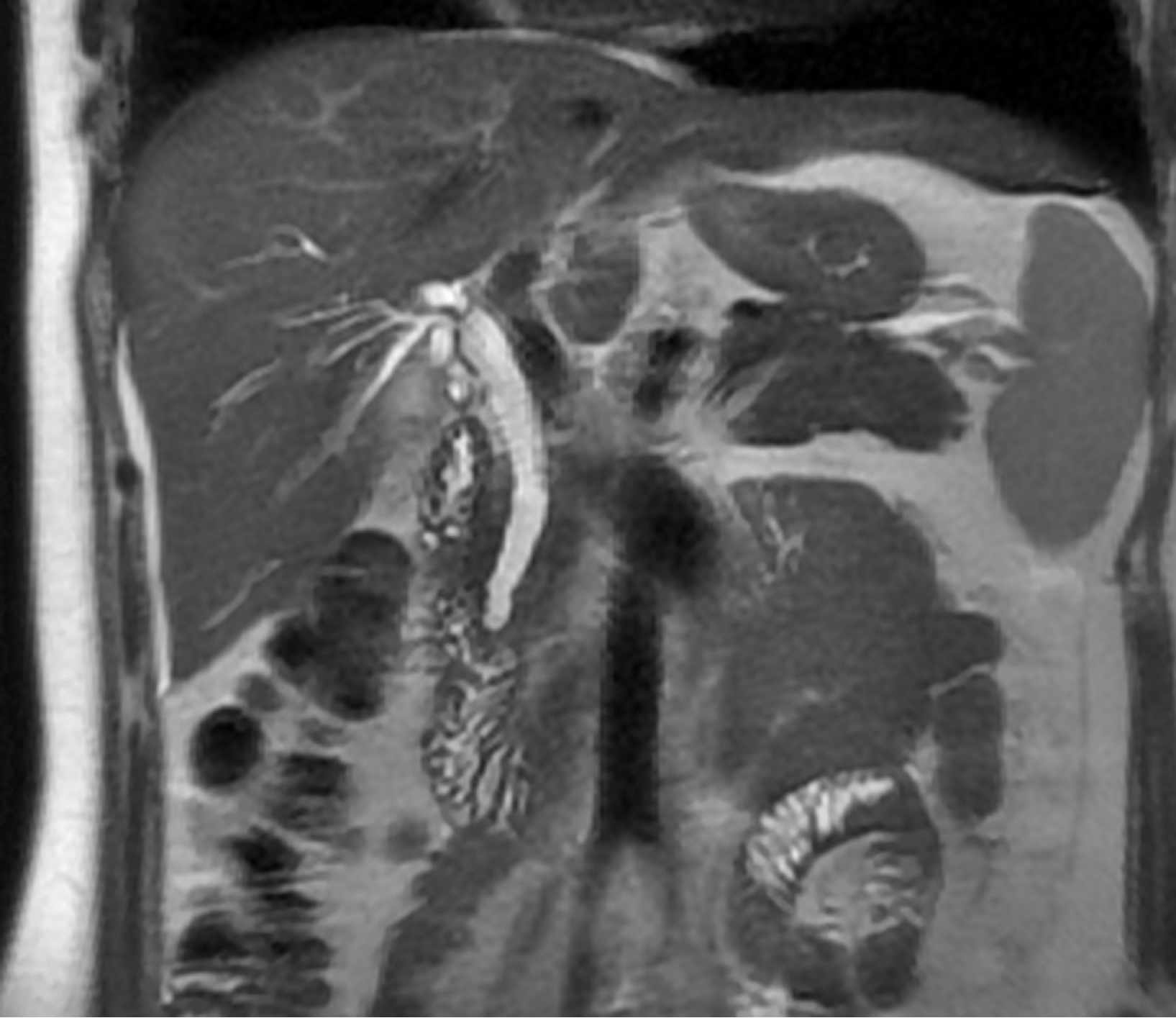
Clinical data and surgical videos of patients with Oddi intersphincter stones admitted to the Department of Hepatopancreatobiliary, Anhui No. 2 Provincial People’s Hospital from April 2021 to July 2024 were retrospectively analyzed. The inclusion criteria were as follows: (1) Aged between 18 and 75 years; (2) Terminal common bile duct stones were diagnosed using preoperative imaging, such as magnetic resonance cholangiopancreatography (Figure 1), computed tomography, and ultrasound, and Oddi intersphincter stones were further confirmed with intraoperative exploration; and (3) No obvious clinical symptoms, such as jaundice or cholangitis, were detected. The exclusion criteria were as follows: (1) Patients had serious cardiopulmonary disease, hepatic insufficiency, or renal insufficiency; (2) Patients were allergic to or contraindicated atropine; (3) Patients were pregnant or lactating; (4) Patients had uncontrolled biliary tract infection before the operation; and (5) Patients were lost to follow-up or lacked complete clinical data. Our study was reported in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Anhui No. 2 Provincial People’s Hospital. All patients signed informed consent before surgery.
The ultrafine choledochoscope and related equipment were provided by Micro-Tech Co., Ltd. (host model: BS-W-150; disposable ultrafine choledochoscope model: CDS22004, diameter: 2.8 mm; disposable endoscopic lithotomy basket model: CEB01013, shape: Four-wire spiral). The amount of atropine sulfate used for injection was 0.5 mg per tablet.
Preoperative routine examinations, including routine blood tests, liver and kidney function tests, coagulation function tests and electrocardiograms, were performed. The patients were deprived of food for 4 hours and water for 2 hours before surgery. Antibiotics were administered 30 minutes before surgery to prevent infection.
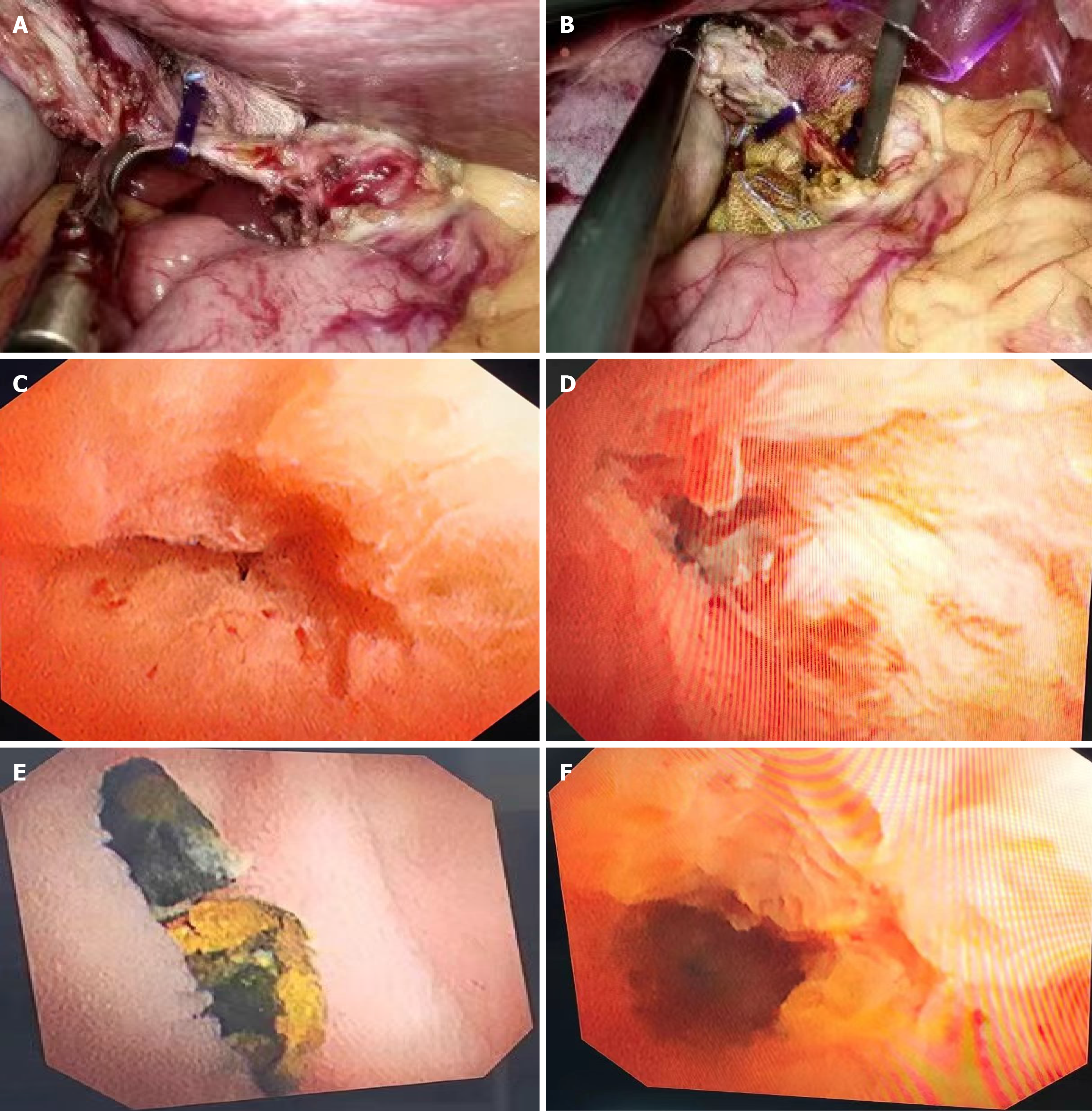
General anesthesia was used, and breathing was maintained by intubation. The patients were subsequently placed in the supine position. Retrograde cholecystectomy was first performed, and the gallbladder duct was not severed. The anterior wall of the gallbladder duct was incised longitudinally at a distance of 0.5 mm from the common bile duct, and the ultrafine choledochoscope was inserted through the gallbladder duct to explore the common bile duct (Figure 2A and B). Then, under direct visual inspection using an ultrafine choledochoscope, the common bile duct was carefully examined to detect and locate Oddi intersphincter stones (Figure 2C and D). The stone was subsequently removed using a special lithotomy basket for an ultrafast choledochoscope or by being pushed into the intestinal cavity of the duodenum (Figure 2E). The common bile duct was explored once again to confirm that the stone was removed thoroughly (Figure 2F). Finally, the opening of the gallbladder duct was closed.
Before stone removal, 0.5 mg of atropine was administered intravenously, and relaxation of the Oddi sphincter was observed. If necessary, the dose was increased by 0.5 mg, and the maximum dose was 1.0 mg.
The vital signs of patients were routinely observed after the operation, with special attention given to changes in breathing and heart rate. The patients were deprived of food and water for 6 hours after the operation and then gradually resumed a normal diet. Antibiotics were used continually to prevent infection. Low-dose dexamethasone (5 mg) and 654-2 (10 mg) were used in combination for 3 days. Routine blood, liver function and imaging results were reexamined at 3 days postsurgery.
The criteria for surgical success were defined as complete removal of Oddi intersphincter stone, an unblocked biliary tract, and no serious complications. The operation time was defined as the total time from the insertion of an ultrafine choledochoscope into the common bile duct to the confirmation of stone removal. Postoperative bleeding, cholangitis, pancreatitis, bile leakage, and other complications were recorded within 30 days. Patients were followed up by outpatient and telephone visits at 1, 3, 6 and 12 months after surgery. Symptom remission, stone recurrence and complications were recorded.
The Shapiro-Wilk test for normality was performed on all the data using SPSS 26.0 software. The normally distributed data are expressed as the mean ± SD. The nonnormally distributed data are expressed as the median (minimum-maximum). The categorical data are expressed as the number of cases.
A total of 17 patients were recruited, including 3 males and 14 females. The mean age of the patients was 40.6 ± 13.9 years, and the mean BMI was 22.1 ± 2.8 kg/m2. The mean diameters of the common bile duct and gallbladder duct were 7.8 ± 1.3 mm and 3.8 ± 0.4 mm, respectively. The median maximum diameter of choledocholithiasis was 3 (2–5) mm, and 2 patients had multiple bile duct stones. The median preoperative TBIL level was 18 (8–51) µmol/L, and 10 patients had elevated TBIL levels. All the patients had varying degrees of symptoms, such as biliary colic, jaundice and fever. The basic information of the included patients is shown in Table 1.
| Variables | Total |
| Gender (male/female) | 3/14 |
| Age (yeas) | 40.6 ± 13.9 |
| BMI (kg/m2) | 22.1 ± 2.8 |
| Hypertension (yes/no) | 4/13 |
| Diabetes (yes/no) | 5/12 |
| Common bile duct diameter (mm) | 7.8 ± 1.3 |
| Gallbladder duct diameter (mm) | 3.8 ± 0.4 |
| Maximum diameter of choledocholithiasis (mm) | 5 (1-7) |
| Number of bile duct stones (single/multiple) | 12/5 |
| ALT (U/L) | 61 (10-447) |
| AST (U/L) | 49 (13-800) |
| ALP (U/L) | 76 (42-339) |
| GGT (U/L) | 246 (9-627) |
| TBIL (µmol/L) | 18 (8-51) |
The stones were removed successfully in all 17 patients, with a surgical success rate of 100%. Among these patients, 12 were successfully removed through the lithotomy basket using a combination of ultrafine choledochoscopy and low-dose atropine. In 5 patients, as the lithotomy basket failed to open, the stones were pushed into the intestinal cavity using a combination of ultrafine choledochoscopy and low-dose atropine.
The average operation time was 19.4 ± 7.8 minutes. Overall, the operation time was short, and the operation was simple. Intraoperative blood loss was 26.3 ± 7.4 mL. The postoperative durations of activity, diet, and extubation were 6.7 ± 2.0, 9.0 ± 3.4, and 1.9 ± 0.6 hours, respectively. None of the patients had postoperative jaundice (Table 2).
| Variables | Total |
| Operation time (minute) | 19.4 ± 7.8 |
| Intraoperative blood loss (mL) | 26.3 ± 7.4 |
| Postoperative activity time (hour) | 6.7 ± 2.0 |
| Postoperative feeding time (hour) | 9.0 ± 3.4 |
| Postoperative extubation time (hour) | 1.9 ± 0.6 |
| Postoperative ALT (U/L) | 56 (12-137) |
| Postoperative AST (U/L) | 24 (12-46) |
| Postoperative ALP (U/L) | 88 (38-218) |
| Postoperative GGT (U/L) | 56 (7-432) |
| Postoperative TBIL (µmol/L) | 19 (7-34) |
| Elevated serum amylase (yes/no) | 0/17 |
| Bile leakage (yes/no) | 0/17 |
| Biliary tract infection (yes/no) | 0/17 |
| Biliary stricture (yes/no) | 0/17 |
| Residual stone (yes/no) | 0/17 |
| Postoperative occult blood in stool (yes/no) | 0/17 |
| Stone recurrence (yes/no) | 0/17 |
| Postoperative symptom relief (yes/no) | 17/0 |
No serious complications, including postoperative hemorrhage, pancreatitis, bile leakage, biliary tract infection, biliary stricture, or residual stone, occurred in any of the 17 patients.
All patients were followed up regularly after surgery. During the follow-up period, none of the patients had preoperative symptoms such as biliary colic, jaundice or fever. The symptom remission rate was 100%. During the follow-up period, none of the patients experienced stone recurrence. No patients developed other surgery-related complications during the follow-up period.
In this study, we first demonstrated that the treatment of Oddi intersphincter stones using ultrafine choledochoscopy combined with low-dose atropine had a high success rate, a short operation time and a low incidence of postoperative complications. In addition, patient symptoms were significantly relieved, and the risk of stone recurrence was low after surgery.
An intersphincter stone is a special type of choledocholithiasis. Under traditional choledochoscopy, intermittent water injection into the common bile duct is typically applied to increase biliary pressure. The diastolic space of the Oddi sphincter was opened, and a mesh basket was used to remove the stone. Traditional choledochoscopy has an effect on upper sphincter intermuscular stones. However, owing to disturbances, the sphincter of Oddi is prone to spasms, which affect the stone removal success rate. In addition, as a traditional choledochoscope is too thick to enter the sphincter, stones located between the middle and lower sphincter are likely overlooked; therefore, the success rate of stone removal is relatively low. In addition, blindly pushing stones with mesh baskets easily causes complications such as aggravation of stone incarceration or intestinal injury. Owing to the advantages of a small diameter, flexible operation and clear vision, the ultrafast choledochoscope can better enter the Oddi intersphincter area and accurately detect and remove stones. The sphincter of Oddi is relaxed by atropine, allowing the ultrafine choledochoscope to be further extended into the intestinal lumen, which further increases the success rate of stone removal.
In this study, Oddi intersphincter stones were successfully removed in all 17 patients by using an ultrafine choledochoscope combined with low-dose atropine, yielding a success rate of 100%. This result is consistent with a recent finding by Nie et al[9] that ultrafine choledochoscopy has a high success rate in the treatment of biliary stones. The complication rate of choledochoscopic surgery is approximately 7%-10%[10]. Traditional ERCP combined with sphincterotomy or mechanical lithotomy also has several shortcomings in the treatment of Oddi intersphincter stones, including large surgical trauma, high complication rates and incomplete stone removal[11]. As an anticholinergic drug, atropine relaxes smooth muscles and relieves spasms. During biliary surgery, atropine relaxes the sphincter of Oddi and improves the patency of the biliary tract, facilitating stone removal. Moreover, atropine reduces spasm reactions in the Oddi sphincter during surgery, facilitates the extraction of stones, reduces intraoperative difficulties, improves the success rate of surgery, and reduces the risk of postoperative complications[12,13]. Moreover, the dosage of atropine is controlled within a small range (0.5–1 mg), which effectively prevents adverse effects. For patients with more severe incarcerated stones, the use of intraoperative lithotripsy devices improves the removal success rate. In this study, no serious complications, such as postoperative hemorrhage, pancreatitis or bile leakage, were noted in any of the patients after surgery, suggesting that ultrafine choledochoscopy combined with low-dose atropine is safe for the treatment of Oddi inter
Although the present study results indicate that ultrafine choledochoscopy combined with low-dose atropine has a satisfactory effect on the treatment of Oddi intersphincter stones, the sample size of the study was relatively small, and a control group was lacking. It is necessary to increase the sample size and establish a control group to further verify the effectiveness and safety of this technology. In addition, the optimal dosage and timing of atropine should be further explored to optimize the treatment regimen.
In conclusion, this study suggests that ultrafine choledochoscopy combined with low-dose atropine is effective and safe for the treatment of Oddi intersphincter stones, with a high surgical success rate, a low incidence of postoperative complications, and a low risk of stone recurrence. This method provides new ideas and choices for the minimally invasive treatment of biliary calculi and has good clinical application prospects.
| 1. | Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017;66:765-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 255] [Article Influence: 31.9] [Reference Citation Analysis (1)] |
| 2. | Gupta V, Abhinav A, Vuthaluru S, Kalra S, Bhalla A, Rao AK, Goyal MK, Vuthaluru AR. The Multifaceted Impact of Gallstones: Understanding Complications and Management Strategies. Cureus. 2024;16:e62500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Fu K, Yang YY, Chen H, Zhang GX, Wang Y, Yin Z. Effect of endoscopic sphincterotomy and endoscopic papillary balloon dilation endoscopic retrograde cholangiopancreatographies on the sphincter of Oddi. World J Gastrointest Surg. 2024;16:1726-1733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Li L, Wang J, Tong CC, He CY. Risk factors of recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2023;22:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Syrén EL, Sandblom G, Enochsson L, Eklund A, Isaksson B, Österberg J, Eriksson S. Outcome of ERCP related to case-volume. Surg Endosc. 2022;36:5339-5347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 6. | Lyu Y, Cheng Y, Li T, Cheng B, Jin X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc. 2019;33:3275-3286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 91] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 7. | Navaratne L, Al-Musawi J, Vutipongsatorn K, Isla AM. Leveraging access to technology and enhanced surgical technique (LATEST) in laparoscopic bile duct exploration (LBDE). Surg Endosc. 2023;37:2367-2378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Takenaga H, Magaribuchi T, Nakajima H. Effects of timepidium bromide, hyoscine-N-butylbromide and atropine on the isolated guinea pig gallbladder and sphincter of Oddi. Jpn J Pharmacol. 1980;30:317-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Nie H, Wang F, Xiong Q, Dong L, Fang J, Wang H, Zhao Q. Novel biliopancreatic duct endoscope combining optical coherence tomography with intraductal US for exploring the bile duct: a diagnostic study in a porcine model. Gastrointest Endosc. 2021;94:1136-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Al-Habbal Y, Reid I, Tiang T, Houli N, Lai B, McQuillan T, Bird D, Yong T. Retrospective comparative analysis of choledochoscopic bile duct exploration versus ERCP for bile duct stones. Sci Rep. 2020;10:14736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Ak Ç, Aykut H, Pala E, Sayar S, Tarikçi Kiliç E, Adali G, Kahraman R, Öztürk O, Özdil K. Post-ERCP Complication Analysis of an Experienced Center. Surg Laparosc Endosc Percutan Tech. 2022;32:707-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Dahlstrand C, Björck S, Edin R, Dahlström A, Ahlman H. Substance P in the control of extrahepatic biliary motility in the cat. Regul Pept. 1988;20:11-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Thune A, Baker RA, Saccone GT, Owen H, Toouli J. Differing effects of pethidine and morphine on human sphincter of Oddi motility. Br J Surg. 1990;77:992-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 36] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Navaratne L, Martinez Isla A. Transductal versus transcystic laparoscopic common bile duct exploration: an institutional review of over four hundred cases. Surg Endosc. 2021;35:437-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |