Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.100321
Revised: December 1, 2024
Accepted: January 9, 2025
Published online: March 27, 2025
Processing time: 136 Days and 1.1 Hours
Liver transplantation, as an effective therapy for patients with liver cancer, plays an important role in improving the quality of life of patients. However, the com
Core Tip: This paper discusses the effect of early postoperative nutritional intervention on patients with liver cancer and liver transplantation, and combined with its mechanism of action, can better understand the effectiveness of intervention, and provide reference for the development of scientific and reasonable nutritional support programs in clinical practice.
- Citation: Deng SS, Zhu YP, Chen ZT, Li W. Application progress of early nutrition intervention in patients with hepatocellular carcinoma after liver transplantation. World J Gastrointest Surg 2025; 17(3): 100321
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/100321.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.100321
As a highly malignant tumor of the digestive system, liver cancer has a hidden onset, rapid development and high degree of malignancy, which often leads to the diagnosis of patients in the middle and late stage. For these patients, liver transplantation, as an effective treatment, can significantly prolong the survival of patients and improve their quality of life. However, liver transplant patients often have a severely impaired liver function and are unable to compensate themselves before undergoing surgery[1]. At the same time, many uncertain factors such as the trauma of the operation itself and the anesthesia treatment during the operation will further aggravate the metabolic pressure of the body, resulting in insufficient nutrition of the patients. If timely intervention measures are not taken, patients will not only face significant weight loss, hypoproteinemia, but also lead to severe consequences such as cachexia, which to some extent seriously affect the recovery of patients’ liver function after surgery. Therefore, many domestic authoritative experts have reached a consensus and advocated the implementation of early and active nutritional support strategies for patients after liver transplantation[2].
With the rapid development of nutrition science, clinical medicine and surgical technology, the field of postoperative nutrition intervention has also made remarkable breakthroughs and progress. From the previous parenteral nutrition auxiliary means, the gradual transition to the popularization and application of enteral nutrition, and then to the customization of personalized nutrition plans, the nutrition intervention strategy has been further improved[3]. On the one hand, this series of development has built a more scientific nutritional security system for liver cancer patients with liver transplantation, and on the other hand, it also provides a new perspective and way to promote the postoperative recovery process and optimize the quality of life of patients. Based on this, this paper aims to review the nutritional status of patients with liver cancer and the influence of nutritional intervention on liver transplantation, focusing on the me
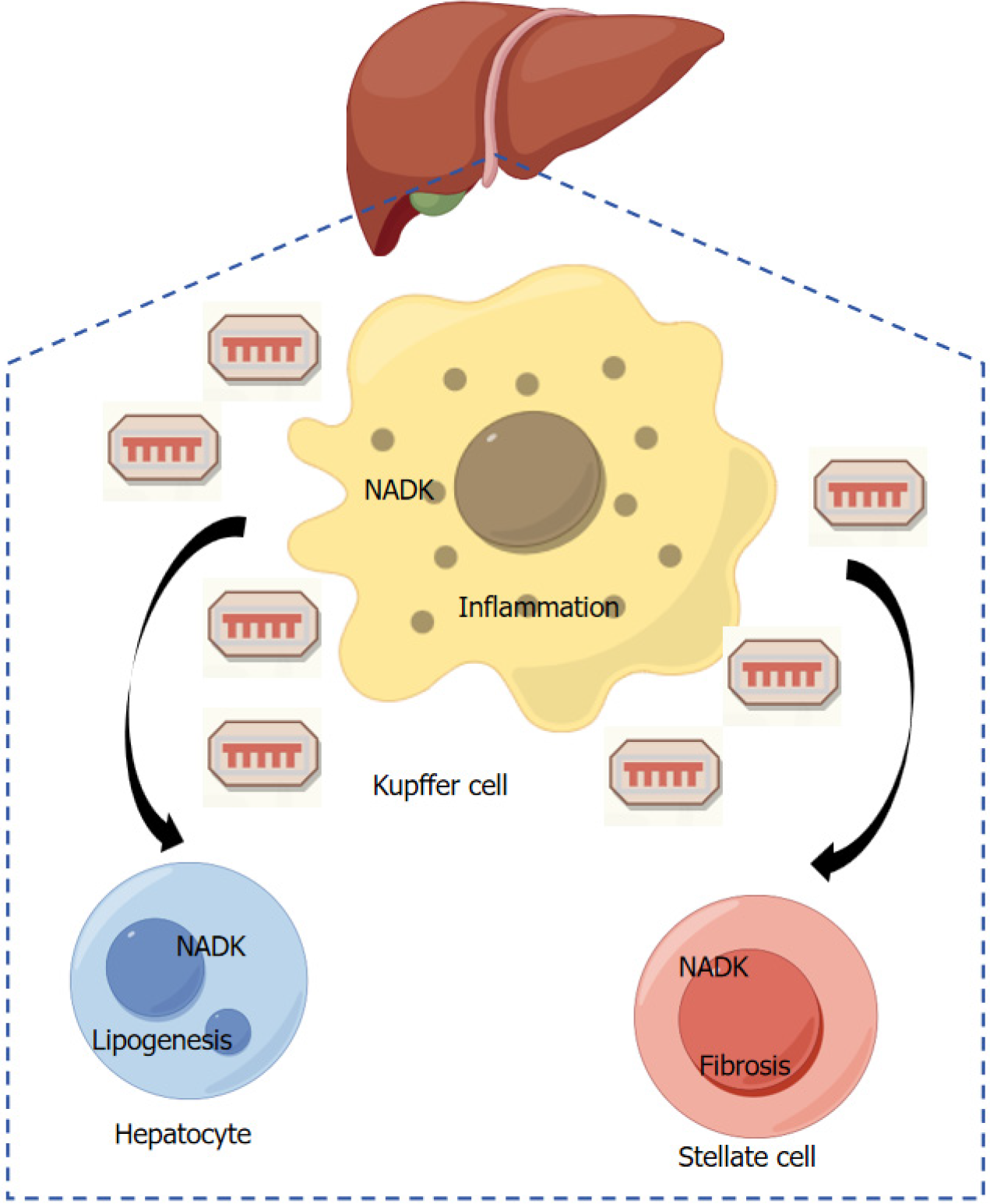
According to relevant studies, liver (Figure 1) is the main metabolic organ of the human body, and its lesions will inevitably increase the risk of malnutrition in patients[4]. Stachowska et al[5] reported in a meta-analysis that fiber supplementation was associated with favorable changes in body mass index (BMI), insulin homeostasis, and liver-related biomarkers in patients with nonalcoholic liver disease. Moreover, Lai et al[6] found that the severity of cirrhosis was related to the decreased activity of glutathione and its related enzymes. Among the global malignant tumors, liver cancer is the second deadliest, and the pathogenesis of this disease involves the individual health status of patients, environmental exposure and other aspects. Studies have revealed that the main reasons promoting the occurrence of liver cancer involve obesity and type 2 diabetes, etc., and after further investigation, it is found that nutrition status can become a key factor affecting the tumor process to a certain extent, especially in patients with advanced malignant tumors[7]. Therefore, the nutritional status of patients with malignant tumors has been paid more and more attention by clinicians. Zhang et al[8] found in their study that the risk of malnutrition was significantly higher in liver cancer patients receiving transarterial chemoembolization (TACE) treatment, and the risk of malnutrition was significantly positively correlated with their symptom groups. At the same time, studies have found that with the increasing age of patients, their liver function gradually declines, which, coupled with chronic diseases, may cause malnutrition to a certain extent[9]. In addition, in the study of Xi et al[10], it was further found that the progression of tumor-node-metastasis stages, the severity of anemia and the activity status of viral hepatitis B all affected the digestive and absorption functions of patients to varying degrees, thus further accelerating the occurrence of malnutrition in tumor patients.
Studies have shown that stress conditions such as anesthesia and surgical trauma will trigger the body to enter a highly decomposed abnormal metabolic state, among which postoperative insulin resistance is particularly significant, which not only limits the effective use of glucose to a certain extent, but also may lead to a series of metabolic disorders. Thus, the malnutrition of patients is further aggravated and their liver function is seriously damaged[11]. The core of individualized nutrition nursing strategy is to accurately assess the nutritional risk of patients in advance, and comprehensively consider their current nutritional status, personal eating habits and energy needs and other factors, so as to develop targeted diet management programs for them. To some extent, this intervention can effectively improve the nutritional status of patients while at the same time, further promote the overall recovery process of patients[12].
Menozzi et al[13] conducted structured interviews with pancreatic cancer surgery patients by means of a 24-hour dietary recall aimed at evaluating the intake of all foods, beverages, and oral nutritional supplements consumed in the last 24 hours, in conjunction with muscle mass measurements to provide a comprehensive nutritional assessment for pancreatic surgery. This study points to the importance of a multidimensional, comprehensive preoperative nutritional assessment and appropriate perioperative nutritional interventions for patients undergoing major cancer surgery in improving tolerance and clinical outcomes of antitumor therapy. Personalized nutritional care played an active role in patients undergoing hepatectomy for hepatocellular carcinoma. It can not only significantly improve the nutritional status of patients to a certain extent, but also promote the metabolism and absorption efficiency of nutrients, thus further enhancing the immune function of patients and conducive to postoperative rehabilitation. At the same time, Sun et al[14] used patient subjective global assessment to develop a personalized nutritional intervention plan and selection of nutritional pathways after TACE for hepatocellular carcinoma. Patients were given oral nutritional solution for energy supplementation or intravenous nutrition for energy supplementation as needed with close monitoring of nutritional risk and electrolyte changes, and it was found that the incidence of gastrointestinal complications as well as electrolyte disorders were significantly reduced in the nutritional intervention group. The study concluded that for elderly patients with primary liver cancer, early enteral nutritional support was provided to them after TACE, and the results showed that this measure effectively improved the nutritional status of the patients, and also enhanced the liver function and immune function of the patients to a certain extent, which ultimately improved the prognosis of the patients. In addition, other studies have found that preoperative nutritional risk screening (NRS) and targeted nutritional supplementation based on the assessment results can, on the one hand, successfully solve the problem of nutritional imbalance[15]; on the other hand, postoperative complications can be significantly reduced, thus minimizing the length of hospitalization and enabling patients to recover more quickly. In addition, Yap et al[16] also confirmed through systematic analysis that perioperative nutritional intervention could effectively reduce postoperative infection, ascites, length of hospital stay, and increase body weight in patients undergoing hepatocellular cancer resection.
Anthropometric indicators: When evaluating the physical condition of liver transplant candidates, BMI, upper arm circumference, hand grip strength and other indicators should be measured, and effective comprehensive evaluation should be carried out[17]. However, for most patients, these indicators may interfere with the measurement results due to the presence of peripheral edema and abdominal fluid. The accuracy of BMI in cancer patients may be reduced, so the accuracy of BMI can be improved to a certain extent by scientifically estimating and subtracting the amount of abdominal fluid and other body fluid accumulation to correct BMI value[18]. At the same time, other parameters such as upper arm circumference also serve as an effective basis for assessing the nutritional status of patients. In the aspect of assessing fat reserve and consumption, triceps skin fold thickness is mainly used to judge, and its change can indirectly reflect the metabolic status of the body to a certain extent[19]. In the study of Chong et al[20], it was found that skeletal muscle fluctuations occurred in liver transplant patients during the perioperative period. Meanwhile, 30% to 70% of liver transplant candidates were found to have decreased muscle mass and function. Studies have found that for liver transplant recipients, lower muscle mass will not only increase the incidence of complications, but also prolong the duration of intensive care unit stay and the need for mechanical ventilation, and may also lead to a decrease in survival[21]. Luo et al[22] introduced the concept of “BMI of abdominal effusion”, which dynamically adjusts the critical value of BMI mainly according to the severity of abdominal effusion. Compared with traditional BMI, it is more reliable in assessing patients’ malnutrition. In addition, in terms of upper body strength, hand grip strength has been recognized as an effective means of identifying patients with potentially high risk of complications and, to a certain extent, can be a unique predictor of assessing the likelihood of developing major complications in malnourished patients with cirrhosis over the next year.
Biochemical indexes: In the liver, a variety of key plasma proteins such as albumin, retinol-binding protein and enzymes involved in creatinine metabolism can be synthesized, and in this process, they are more susceptible to changes in liver health status and inflammatory response[23]. Therefore, serum albumin concentration and 24-hour urinary creatinine output are important indicators for evaluating nutritional status and predicting prognosis of liver transplant recipients to some extent. Albumin is a core indicator of protein reserve and liver function in the body, among which a low serum albumin level is widely regarded as a key factor to increase the risk of postoperative infection and reduce the survival rate[24]. Creatinine, as a byproduct of muscle metabolism, is produced at a relatively constant rate and is regulated by specific enzymes synthesized by the liver, thus further establishing a link with liver function. In addition, the decrease of 24-hour urinary creatinine excretion, which is an effective indicator for evaluating muscle mass, not only predicts a higher risk of death in patients to a certain extent, but also increases the possibility of transplant failure[25]. Therefore, by monitoring the serum albumin concentration and 24-hour urinary creatinine excretion during the perioperative period, the nutrition and health status of liver transplant recipients can be more comprehensively evaluated, which can further provide data support for the development of personalized nutrition intervention plans.
Biological resistance analysis: Bioelectrical impedance analysis (BIA) technology, as a convenient and safe detection method, is mainly used to measure the body’s reactance and resistance, so as to accurately reveal the body’s fat mass, somatic cell mass, phase angle and other key indicators[26]. As a core factor, phase angle is often recommended to be measured on the arm and thigh of patients[27]. Cereda et al[28] showed in related studies that BIA showed significant advantages in evaluating nutritional status and predicting survival in cancer patients. Moreover, Wang et al[29] believed that in the analysis of lung cancer patients, phase angle had higher predictive efficacy than albumin, transferrin and other indicators. At the same time, patients with low preoperative phase angle will not only suffer severe infection after surgery, but also significantly increase the risk of poor prognosis. In addition, phase angle also has the potential of preoperative volume assessment. On the one hand, accurate assessment can reduce blood loss to a certain extent during hepatectomy, and on the other hand, improve surgical safety[30]. Although BIA has a high accuracy in body composition analysis, pathological conditions such as edema and abdominal effusion may interfere with its measurement results, and the detection cost and professional equipment demand of this technology are high[31], so its clinical application is limited to a certain extent.
NRS 2002: NRS 2002 is an evaluation system that comprehensively assesses a patient’s nutritional status by disease status, recent weight loss of 5% or more, reduction in food intake, BMI, and age[32]. Patients with an overall score of 3 or more are considered to be at significant risk of malnutrition and need to undergo a detailed nutrition screening procedure immediately. If the score is less than 3, it is recommended to maintain the frequency of re-evaluation once a week during hospitalization[33]. The NRS 2002 scoring system is mainly used as a preliminary screening tool for nutritional risk, but it is not enough to directly identify malnutrition and its specific degree in patients[34]. In the application, the accuracy and effectiveness of the evaluation system may be further reduced if the patient’s weight is not measured, or if the weight data is affected by fluid retention.
Malnutrition Universal Screening Tool: Based on the Malnutrition Universal Screening Tool (MUST) assessment system, key indicators such as a patient’s BMI, unwanted weight loss, and presence of acute disease, the risk of malnutrition was divided into three levels: Low, medium, and high[35]. Studies have shown that in the nutritional status assessment of patients with colorectal cancer, MUST shows a high degree of consistency with the patient’s subjective overall assessment[36]. However, the applicability of MUST in the medical field of liver transplantation remains to be further explored.
Royal Free Hospital-Nutritional Prioritizing Tool: The Royal Free Hospital-Nutritional Prioritizing Tool (RFH-NPT) is used to assess the nutritional health of patients with cirrhosis in terms of BMI, involuntary weight loss, and daily dietary intake. Patients were further subdivided into three risk levels: Low, medium, and high[37]. In view of the phenomenon of fluid retention in patients with cirrhosis, which significantly improves the complexity of screening for malnutrition to a certain extent, RFH-NPT includes the factor of fluid retention, and compared with NRS 2002, RFH-NPT has a higher sensitivity[38]. Therefore, in 2019 European Society for Parenteral Nutrition selected it as the preferred tool for nutritional screening of patients with liver disease.
Dietary Inflammatory Index: The Dietary Inflammatory Index (DII)[39] is a novel nutritional assessment index that evaluates the potential anti-inflammatory or pro-inflammatory effects of diets by categorizing dietary components into 36 anti-inflammatory and 9 pro-inflammatory components based on the ability of the food and nutrients to affect serum levels of inflammatory markers. Duggan et al[40] showed that diets with high DII scores were associated with an in
Although the specific role of malnutrition on the prognostic mechanism of liver transplantation has not been fully revealed, studies have shown that malnutrition can significantly increase the risk of complications and death of patients, and is a key factor affecting postoperative survival[42]. In addition, the presence of malnutrition and sarcopenia is closely related to the increase of infection and mortality after liver transplantation[43]. Meanwhile, in the study of Prakash et al[44], it was found that for recipients of living donor liver transplantation, the occurrence of malnutrition would increase the duration of postoperative mechanical ventilation and intensive care unit stay. Lee et al[45] also confirmed this view in their study, in which they emphasized that although there are multiple factors that may affect the clinical outcome of liver transplant patients, low vitamin D3 content is an independent risk factor. In addition, the liver after transplantation is unable to obtain sufficient glycogen support and effective glucose uptake, so the nutritional intake of patients not only needs to meet the urgent needs of metabolism, but also needs to provide the necessary energy reserve for the trans
Before liver transplantation, the prevention of sustained loss of nutrition and muscle reserve is the main core goal of nutritional support, and vitamin and mineral deficiencies should be further corrected to minimize the risk of infection and debilitation of patients[47]. Early effective intervention against malnutrition can not only significantly prolong the survival period of patients, improve the quality of life, but also reduce the occurrence of postoperative complications to a certain extent, thus creating favorable conditions for liver transplantation. Nutritional support mainly includes enteral nutrition and parenteral nutrition. According to European Society for Parenteral Nutrition guidelines, enteral nutrition is recommended as the preferred nutritional support means, which is not only more consistent with the natural phy
For patients after liver transplantation, the core of nutritional management is adequate protein and energy supply, so as to avoid excessive protein catabolism caused by surgery to the greatest extent[52]. The high metabolic status often associated with malnutrition was significantly associated with lower survival rates. In recent years, clinical practice has confirmed that adequate nutritional intake in the early stage after liver transplantation is not only conducive to post-transplantation recovery, but also of great value in preventing post-transplantation complications[53]. Some specific nutrients that can play a complementary role in nutritional therapy after transplantation are called immune system modulators in clinic[54].
According to the study of Miyauchi et al[55], seven days before the ischemic injury of liver transplantation mice, after giving an enteral diet rich in antioxidant nutrients, adding vitamins C and E, and supplementing polyphenols, it was found that liver ischemia/reperfusion injury was significantly reduced, and antioxidant and inflammatory parameters could be improved to a certain extent, thus reducing liver cell injury. At the same time, Li et al[56] found in their study that in the early stage of liver transplantation, the recipient mice fed a supplemented tyrosine diet had longer survival time and reduced tissue damage. Moreover, in allograft liver transplantation, Pan et al[57] found that vitamin A could regulate gastrointestinal function after liver transplantation. In the study of Lindqvist et al[58], the nutritional regimen with a higher proportion of enteral nutrition and high-protein oral nutrition supplements in the early stage after liver transplantation would lead to increased protein intake of patients to a certain extent, but there was no significant difference between the two nutritional programs in postoperative severe outcomes. Although the current research on nutritional support for patients after liver transplantation due to biliary atresia, liver cancer, and non-alcoholic hepatitis is gradually in-depth, there is a relative lack of comprehensive nutritional management guidelines. Therefore, the indicators involved in this paper still need a large number of clinical studies to further improve.
In the human gut, there are complex microbial communities, including bacteria, fungi and archaea, which form a close mutually-beneficial symbiotic relationship with the human body. In a healthy state, the number and types of intestinal microbes remain constant, thereby jointly building the harmony of intestinal microecology. If this balance is broken, the imbalance of intestinal flora will be caused, which will not only lead to the disorder of intestinal function, but also affect the metabolism, cardiovascular, nervous and other systems of the human body, and then lead to a series of liver diseases[59].
In recent years, studies have shown that nutrition intervention strategies have been proven to have significant effects on the regulation of human and animal intestinal microbial communities[60]. In this process, specific nutrients can not only act as an active participant in the energy supply or metabolic process, but also play a role in regulating the activity of the immune system, so it is considered as “immune nutrition”. With the in-depth discovery of clinical studies, glutamine, arginine and probiotics are all key substances in immune nutrition[61]. Moreover, studies have revealed that the three components of ecological immune nutrition, probiotics, prebiotics and biostime, can directly act on the intestinal microecosystem[62]. At the same time, the study of Hussain et al[63] confirmed that the increase of dietary nutrients such as protein and fiber was related to the diversity and composition of duodenal microbiome. Meanwhile, recent studies have shown that immune nutrition plays a key role in maintaining intestinal function and health, especially in the aspect of intestinal mucosal barrier[64]. Therefore, the intervention of immune nutrients shows a strong protective and supportive effect at these three levels.
On the other hand, hepatocellular carcinoma, as a systemic inflammatory disease, the inflammatory response triggered by pro-inflammatory factors is important in its pathogenesis. The level of short-chain fatty acids (SCFA), which are metabolites of the intestinal microbiota, is closely related to the level of inflammation in the body, and butyrate (SCFA) can inhibit pro-inflammatory cytokines through inhibition of mediating the activity of histone deacetylase and binding to the G protein-coupled receptor (GPR), GPR41 and GPR43, in order to reduce inflammation[65]. It can be seen that the regulation of intestinal flora SCFA-producing bacteria to become the dominant strain is important in the suppression of body inflammation. Related studies have shown that dietary polyphenol-rich foods such as pomegranate, grapes, and broccoli are able to enrich butyrate-producing bacteria in a targeted manner, while diets high in dietary fiber are able to enrich SCFA-producing bacteria in a targeted manner[66]. Under a reasonable dietary structure, it is recommended to moderately increase the intake of anti-inflammatory dietary components and reduce the intake of pro-inflammatory dietary components, which is important in maintaining intestinal microbial homeostasis as well as suppressing the body’s inflammatory response in tumor patients.
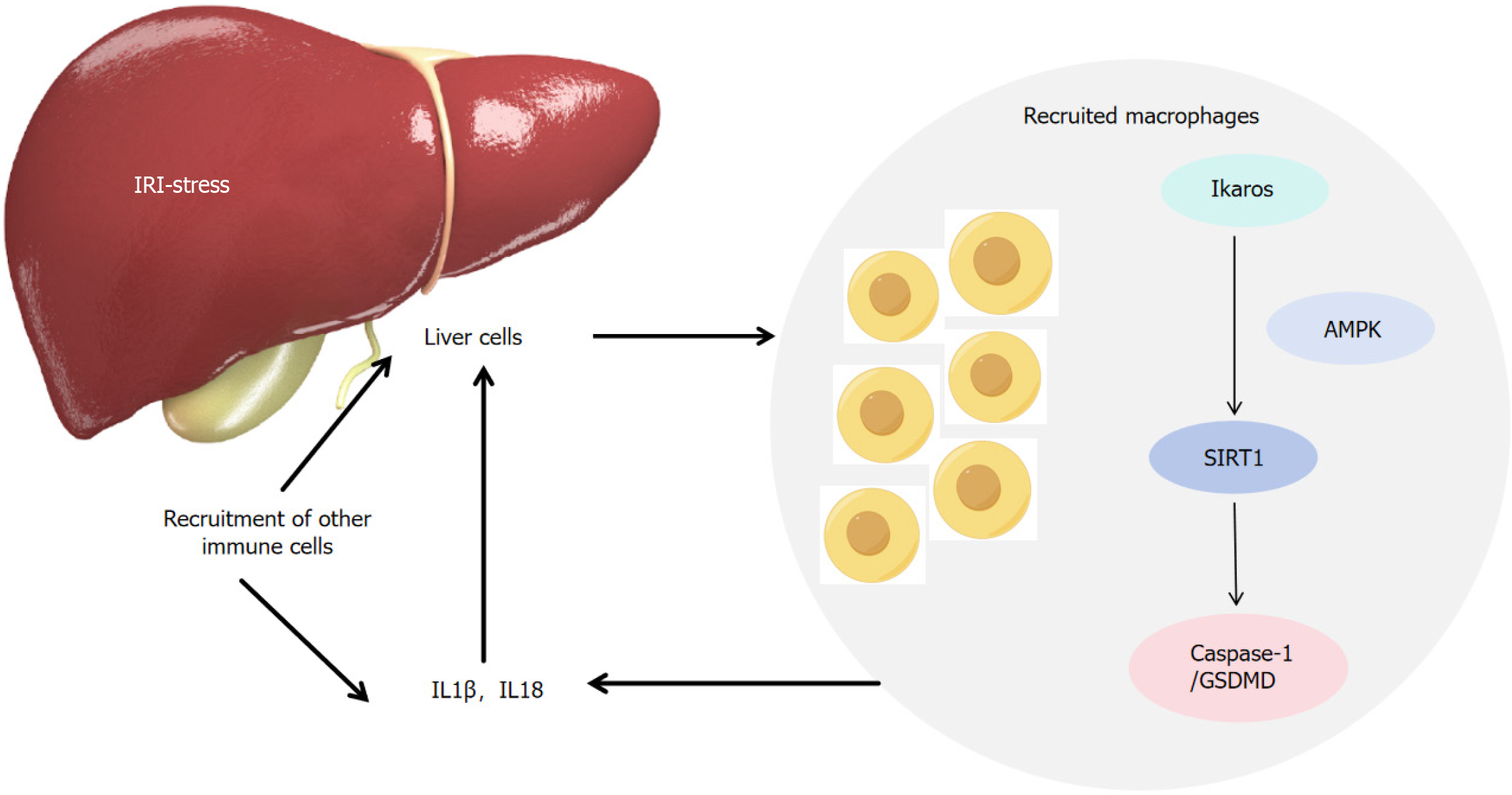
In recent years, some scholars have observed significant changes in the structure and number of intestinal flora in patients with liver cancer, and this relationship between the gut and liver is called the “enterohepatic axis” (Figure 2). Yu and Schwabe[67] pointed out in their study that changes in intestinal flora are of great significance in determining the occurrence and development of hepatocellular carcinoma. Another study also confirmed significant changes in gut microbiota diversity in patients with liver cancer compared to healthy controls, and that porphyromonas and Bacteroides were associated with a reduced risk of liver cancer[68]. These findings reveal that the structural changes of intestinal flora in patients with early liver cancer can be used as a new marker for the diagnosis of early liver cancer to some extent, and its specific analysis is of great significance for the early warning of the disease.
In the progression of liver cancer, the imbalance of intestinal flora interacts with it, and with the deterioration of the disease, the imbalance of intestinal flora will be further aggravated. In an animal experiment exploring the interaction between intestinal microbiota and liver cancer, it was found that intestinal microbiota depletion can impair intestinal tryptophan metabolism, thereby activating aromatics receptor, and thereby accelerate liver tumor genesis, and this process is related to up-regulation of sterol regulatory element-binding protein 2[69]. Feng et al[70] research team revealed that dysregulation of bile acid metabolism is related to the formation of cancer cachexia in mice. The experimental results showed that the intestinal flora of mice with hepatocellular carcinoma cachexia decreased in trichomillaceae and increased in enterobacteriaceae, and the microbial metabolism of bile acids decreased. Targeting bile acid metabolism with taurodeoxycholic acid and other drugs may contribute to the treatment of cancer cachexia. At the same time, studies have further confirmed that intestinal flora disturbance can lead to enterohepatic axis dysfunction by changing the bile acid metabolic pathway, thus promoting the occurrence and development of non-alcoholic fatty liver disease to a certain extent and accelerating its progression to cirrhosis and liver cancer[71].
In addition, the gut microbiota is an important modulator of the anti-tumor immune response in the liver. The body’s innate immune system activates the adaptive immune system by detecting the gut microbiota and its metabolites to exert anti-tumor effects. Previous studies have pointed out that Escherichia coli strain Nissle 1917 has enhanced anti-tumor immune effects and can significantly enhance the inhibitory effects of transforming growth factor receptor blockers on tumor growth and metastasis[72].
For patients with end-stage liver disease, liver transplantation is the primary way to prolong their lives. Although the results are remarkable, complications such as postoperative infection and rejection may endanger the function of the transplanted liver to some extent and seriously affect the postoperative survival of patients. Liver transplantation not only affects the ecological balance of the recipient’s intestinal flora, but also causes significant changes in bacterial distribution and even causes abnormal bacterial migration[73]. At the same time, ischemia-reperfusion injury, immune rejection and antibiotic use during the operation together constitute the key factors for the imbalance of intestinal flora in the early stage after liver transplantation. Among them, ischemia-reperfusion injury is particularly critical, which not only weakens the integrity of intestinal mucosal barrier, promotes abnormal migration of intestinal bacteria, but also reduces intestinal immune function to a certain extent[74]. Bajaj et al[75] found that compared with homogenome, heterogenome showed a higher translocation rate of intestinal bacteria after transplantation, which was accompanied by a significant increase in endotoxin levels and aggravated liver function damage, further emphasizing the central role of immune mismatch in intestinal flora imbalance. Therefore, intestinal microbiography is also considered to be an important biomarker for predicting injury in liver transplantation[76]. At present, the prevention of intestinal flora imbalance and infection caused by bacterial displacement after liver transplantation has been widely studied. In a retrospective study, it was pointed out that the use of antibiotics before liver transplantation could destroy the microvilli of ileal epithelial cells, thus causing changes in the microflora, and thus effectively reducing liver transplant-related infections, thereby reducing liver injury and transplantation dysfunction[77]. At the same time, Jia et al[78] found that ciclosporin A could partially restore intestinal flora after liver transplantation and alleviate liver injury. However, further randomized controlled clinical trials are needed to elucidate the exact mechanism of action of these interventions, their target signaling pathways, and the optimal duration of treatment.
For liver transplantation patients with liver cancer, early postoperative nutritional intervention can effectively improve the prognosis of patients, and can reduce the incidence of postoperative infection and other complications to a certain extent. At the same time, changes in the patient’s gut flora play an important role in this process. However, despite the great potential of early nutritional intervention, it still faces multiple challenges in practical application. The first is the individual differences in nutritional needs. Patients have different nutritional status and metabolic needs before and after surgery. Therefore, targeted nutritional support plans need to be formulated. Secondly, postoperative complications and drug therapy may affect patients’ absorption and utilization of nutrients, and how to effectively maintain nutritional balance under these interfering factors is an important challenge. In addition, the collaboration of the healthcare team and the education of patients and families are also key factors in the successful implementation of nutrition interventions, and the lack of such support may affect the effectiveness of nutrition interventions.
Therefore, future research should aim to further explore strategies for individualized nutritional support and incorporate new nutritional drugs and treatments to optimize postoperative rehabilitation of liver transplant patients with liver cancer. In addition, interdisciplinary teamwork and the application of information technology may improve the efficiency and quality of nutritional support. With the advancement of science and technology and the increasing awareness of the importance of nutrition in disease management, it is expected that nutritional intervention will be more widely used and advanced in the field of liver transplantation for liver cancer in the future. The combination of these efforts will help to maximize the effect of postoperative nutritional interventions in liver transplant patients with liver cancer and improve the survival rate and quality of life of patients.
| 1. | Montano-Loza AJ, Rodríguez-Perálvarez ML, Pageaux GP, Sanchez-Fueyo A, Feng S. Liver transplantation immunology: Immunosuppression, rejection, and immunomodulation. J Hepatol. 2023;78:1199-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 2. | Jamioł-Milc D, Gudan A, Kaźmierczak-Siedlecka K, Hołowko-Ziółek J, Maciejewska-Markiewicz D, Janda-Milczarek K, Stachowska E. Nutritional Support for Liver Diseases. Nutrients. 2023;15:3640. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Koretz RL. Nutritional support in liver disease - an updated systematic review. Curr Opin Gastroenterol. 2023;39:115-124. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Stachowska E, Jakubczyk K, Maciejewska-Markiewicz D. Editorial "Nutrition and Dietary Intake for Liver-Related Diseases". Nutrients. 2021;13:390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Stachowska E, Portincasa P, Jamioł-Milc D, Maciejewska-Markiewicz D, Skonieczna-Żydecka K. The Relationship between Prebiotic Supplementation and Anthropometric and Biochemical Parameters in Patients with NAFLD-A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2020;12:3460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (1)] |
| 6. | Lai CY, Cheng SB, Lee TY, Hsiao YF, Liu HT, Huang YC. Impact of Glutathione and Vitamin B-6 in Cirrhosis Patients: A Randomized Controlled Trial and Follow-Up Study. Nutrients. 2020;12:32635181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | van Dijk AM, Coppens BJP, van Beers MA, Bruins Slot AS, Verstraete CJR, de Bruijne J, Vleggaar FP, van Erpecum KJ. Nutritional status in patients with hepatocellular carcinoma: Potential relevance for clinical outcome. Eur J Intern Med. 2022;104:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Zhang J, Duan H, Zhang J, Qiao H, Jiang J. Symptom clusters and nutritional status in primary liver cancer patients receiving transcatheter arterial chemoembolization. Nutr Hosp. 2024;41:815-823. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Liu T, Liu CA, Zhang QS, Zhang Q, Wang YM, Song MM, Lin SQ, Deng L, Wu SL, Shi HP. Association of the age of onset of metabolic syndrome with the risk of all cancer types. Diabetes Metab Syndr. 2023;17:102896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Xi K, Jingping L, Yaqing L, Xinyuan Y, Hui L, Mei Y, Qingyue C, Dun L. Analysis of the factors influencing moderate to poor performance status in patients with cancer after chemotherapy: a cross-sectional study comparing three models. Sci Rep. 2024;14:3336. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Leraas HJ, Schaps D, Thornton SW, Moya-Mendez M, Donohue V, Hoover A, Olson L, Haines K, Wagner L, Tracy E. Risk of Surgical Intervention in Children with Diagnoses of Cancer and Preoperative Malnutrition: A National Analysis. J Pediatr Surg. 2023;58:1191-1194. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Pimiento JM, Evans DC, Tyler R, Barrocas A, Hernandez B, Araujo-Torres K, Guenter P; ASPEN Value Project Scientific Advisory Council. Value of nutrition support therapy in patients with gastrointestinal malignancies: a narrative review and health economic analysis of impact on clinical outcomes in the United States. J Gastrointest Oncol. 2021;12:864-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Menozzi R, Valoriani F, Ballarin R, Alemanno L, Vinciguerra M, Barbieri R, Cuoghi Costantini R, D'Amico R, Torricelli P, Pecchi A. Impact of Nutritional Status on Postoperative Outcomes in Cancer Patients following Elective Pancreatic Surgery. Nutrients. 2023;15:1958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 14. | Sun Q, Yu H, You T, Zhang D. Individualized nutritional intervention improves the nutritional status of liver cancer patients after transcatheter arterial chemoembolization. Nutr Hosp. 2024;41:649-656. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Huang S, Wang S, Xie Y, He X, Yi X, Zhang J, Deng Z, Yin L. Application of NRS2002 in Preoperative Nutritional Screening for Patients with Liver Cancer. J Oncol. 2021;2021:8943353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Yap KY, Chi H, Ng S, Ng DH, Shelat VG. Effect of perioperative branched chain amino acids supplementation in liver cancer patients undergoing surgical intervention: A systematic review. World J Gastrointest Surg. 2023;15:2596-2618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Hummell AC, Cummings M. Role of the nutrition-focused physical examination in identifying malnutrition and its effectiveness. Nutr Clin Pract. 2022;37:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Holmes CJ, Racette SB. The Utility of Body Composition Assessment in Nutrition and Clinical Practice: An Overview of Current Methodology. Nutrients. 2021;13:2493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 169] [Article Influence: 42.3] [Reference Citation Analysis (0)] |
| 19. | García-Almeida JM, García-García C, Vegas-Aguilar IM, Ballesteros Pomar MD, Cornejo-Pareja IM, Fernández Medina B, de Luis Román DA, Bellido Guerrero D, Bretón Lesmes I, Tinahones Madueño FJ. Nutritional ultrasound®: Conceptualisation, technical considerations and standardisation. Endocrinol Diabetes Nutr (Engl Ed). 2023;70 Suppl 1:74-84. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Chong J, Guorgui J, Coy H, Ito T, Lu M, DiNorcia J, Agopian VG, Farmer DG, Raman SS, Busuttil RW, Kaldas FM. Perioperative Skeletal Muscle Fluctuations in High-Acuity Liver Transplantation. J Surg Res. 2022;270:386-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 21. | Beumer BR, van Vugt JLA, Sapisochin G, Yoon P, Bongini M, Lu D, Xu X, De Simone P, Pintore L, Golse N, Nowosad M, Bennet W, Tsochatzis E, Koutli E, Abbassi F, Claasen MPAW, Merli M, O'Rourke J, Gambato M, Benito A, Majumdar A, Tan EK, Ebadi M, Montano-Loza AJ, Berenguer M, Metselaar HJ, Polak WG, Mazzaferro V, IJzermans JNM; Collaborators. Impact of muscle mass on survival of patients with hepatocellular carcinoma after liver transplantation beyond the Milan criteria. J Cachexia Sarcopenia Muscle. 2022;13:2373-2382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Luo X, Cai B, Jin W. The Prevalence Rate of Adult Sarcopenic Obesity and Correlation of Appendicular Skeletal Muscle Mass Index with Body Mass Index, Percent Body Fat, Waist-Hip Ratio, Basal Metabolic Rate, and Visceral Fat Area. Metab Syndr Relat Disord. 2023;21:48-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 23. | Sullivan KE, Swanhall A, Livingston S. Interpretation of Serum Analytes for Nutritional Evaluation. Vet Clin North Am Exot Anim Pract. 2024;27:135-154. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Zink TM, Kent SE, Choudhary AN, Kavolus JJ. Nutrition in Surgery: An Orthopaedic Perspective. J Bone Joint Surg Am. 2023;105:1897-1906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 25. | Stern R, Chen L, Chan AP, Wozniak LJ, Pearl M. Angiotensin II type 1 receptor antibodies and native kidney function in pediatric liver and intestinal transplant recipients. Pediatr Nephrol. 2023;38:4175-4185. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Branco MG, Mateus C, Capelas ML, Pimenta N, Santos T, Mäkitie A, Ganhão-Arranhado S, Trabulo C, Ravasco P. Bioelectrical Impedance Analysis (BIA) for the Assessment of Body Composition in Oncology: A Scoping Review. Nutrients. 2023;15:4792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 37] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 27. | Da Silva BR, Kirkham AA, Ford KL, Haykowsky MJ, Paterson DI, Joy AA, Pituskin E, Thompson R, Prado CM. Phase angle is associated with muscle health and cardiorespiratory fitness in older breast cancer survivors. Clin Nutr ESPEN. 2023;55:208-211. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Cereda E, Pedrazzoli P, Lobascio F, Masi S, Crotti S, Klersy C, Turri A, Stobäus N, Tank M, Franz K, Cutti S, Giaquinto E, Filippi AR, Norman K, Caccialanza R. The prognostic impact of BIA-derived fat-free mass index in patients with cancer. Clin Nutr. 2021;40:3901-3907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Wang F, Zhen HN, Wang HP, Yu K. Measurement of sarcopenia in lung cancer inpatients and its association with frailty, nutritional risk, and malnutrition. Front Nutr. 2023;10:1143213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 30. | Amano K, Bruera E, Hui D. Diagnostic and prognostic utility of phase angle in patients with cancer. Rev Endocr Metab Disord. 2023;24:479-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 31. | Bellido D, García-García C, Talluri A, Lukaski HC, García-Almeida JM. Future lines of research on phase angle: Strengths and limitations. Rev Endocr Metab Disord. 2023;24:563-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 87] [Reference Citation Analysis (0)] |
| 32. | Hersberger L, Bargetzi L, Bargetzi A, Tribolet P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, Kutz A, Kägi-Braun N, Hoess C, Pavlicek V, Schmid S, Bilz S, Sigrist S, Brändle M, Benz C, Henzen C, Nigg M, Thomann R, Brand C, Rutishauser J, Aujesky D, Rodondi N, Donzé J, Stanga Z, Mueller B, Schuetz P. Nutritional risk screening (NRS 2002) is a strong and modifiable predictor risk score for short-term and long-term clinical outcomes: secondary analysis of a prospective randomised trial. Clin Nutr. 2020;39:2720-2729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 33. | Oh SE, Park JS, Jeung HC. Pre-treatment Nutritional Risk Assessment by NRS-2002 Predicts Prognosis in Patients With Advanced Biliary Tract Cancer: A Single Center Retrospective Study. Clin Nutr Res. 2022;11:183-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 34. | Chen X. A novel nomogram based on the nutritional risk screening 2002 score to predict survival in hepatocellular carcinoma treated with transarterial chemoembolization. Nutr Hosp. 2022;39:835-842. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 35. | Donini LM, Poggiogalle E, Molfino A, Rosano A, Lenzi A, Rossi Fanelli F, Muscaritoli M. Mini-Nutritional Assessment, Malnutrition Universal Screening Tool, and Nutrition Risk Screening Tool for the Nutritional Evaluation of Older Nursing Home Residents. J Am Med Dir Assoc. 2016;17:959.e11-959.e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 36. | Henriksen C, Paur I, Pedersen A, Kværner AS, Ræder H, Henriksen HB, Bøhn SK, Wiedswang G, Blomhoff R. Agreement between GLIM and PG-SGA for diagnosis of malnutrition depends on the screening tool used in GLIM. Clin Nutr. 2022;41:329-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 37. | Yang W, Guo G, Mao L, Hui Y, Wang X, Yu Z, Sun M, Li Y, Fan X, Cui B, Jiang K, Sun C. Comparison of the GLIM criteria with specific screening tool for diagnosing malnutrition in hospitalized patients with cirrhosis: A descriptive cross-sectional study. JPEN J Parenter Enteral Nutr. 2023;47:310-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 38. | Zhang P, Wang Q, Zhu M, Li P, Wang Y. Differences in nutritional risk assessment between NRS2002, RFH-NPT and LDUST in cirrhotic patients. Sci Rep. 2023;13:3306. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 39. | Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17:1689-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 996] [Cited by in RCA: 1826] [Article Influence: 152.2] [Reference Citation Analysis (0)] |
| 40. | Duggan C, Tapsoba JD, Shivappa N, Harris HR, Hébert JR, Wang CY, McTiernan A. Changes in Dietary Inflammatory Index Patterns with Weight Loss in Women: A Randomized Controlled Trial. Cancer Prev Res (Phila). 2021;14:85-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 41. | Cantero I, Abete I, Babio N, Arós F, Corella D, Estruch R, Fitó M, Hebert JR, Martínez-González MÁ, Pintó X, Portillo MP, Ruiz-Canela M, Shivappa N, Wärnberg J, Gómez-Gracia E, Tur JA, Salas-Salvadó J, Zulet MA, Martínez JA. Dietary Inflammatory Index and liver status in subjects with different adiposity levels within the PREDIMED trial. Clin Nutr. 2018;37:1736-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 42. | Hammad A, Kaido T, Uemoto S. Perioperative nutritional therapy in liver transplantation. Surg Today. 2015;45:271-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 43. | Duong N, Sadowski B, Rangnekar AS. The Impact of Frailty, Sarcopenia, and Malnutrition on Liver Transplant Outcomes. Clin Liver Dis (Hoboken). 2021;17:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 44. | Prakash K, Sam AF, K N, Tandon N. Effect of Preoperative Sarcopenia, Malnutrition and Functional status on Postoperative Morbidity Following Liver Transplantation. Prog Transplant. 2022;32:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 45. | Lee HJ, Park M, Lee S, Hong SK. Clinical Effect of Preoperative 25-OH-Vitamin D3 Level in Liver Transplant Recipients. Transplant Proc. 2022;54:2301-2306. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 46. | Chapman B, Goh SK, Parker F, Romero S, Sinclair M, Gow P, Ma R, Angus P, Jones R, Luke J, Muralidharan V, Testro A. Malnutrition and low muscle strength are independent predictors of clinical outcomes and healthcare costs after liver transplant. Clin Nutr ESPEN. 2022;48:210-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 47. | Saïdi SA, Abdelkafi S, Jbahi S, van Pelt J, El-Feki A. Temporal changes in hepatic antioxidant enzyme activities after ischemia and reperfusion in a rat liver ischemia model: effect of dietary fish oil. Hum Exp Toxicol. 2015;34:249-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Zama D, Gori D, Muratore E, Leardini D, Rallo F, Turroni S, Prete A, Brigidi P, Pession A, Masetti R. Enteral versus Parenteral Nutrition as Nutritional Support after Allogeneic Hematopoietic Stem Cell Transplantation: a Systematic Review and Meta-Analysis. Transplant Cell Ther. 2021;27:180.e1-180.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 49. | Victor DW 3rd, Zanetto A, Montano-Loza AJ, Heimbach JK, Towey J, Spiro M, Raptis DA, Burra P; ERAS4OLT. org Working Group. The role of preoperative optimization of the nutritional status on the improvement of short-term outcomes after liver transplantation? A review of the literature and expert panel recommendations. Clin Transplant. 2022;36:e14647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 50. | Ramachandran G, Pottakkat B, Basu S, Mohan P. Effect of probiotics on nutritional status, biochemical parameters, and disease severity in cirrhotic patients referred for liver transplantation-A randomised double blind, placebo-controlled trial. Clin Nutr ESPEN. 2023;57:703-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 51. | Sadanand A, Newland JG, Bednarski JJ. Safety of Probiotics Among High-Risk Pediatric Hematopoietic Stem Cell Transplant Recipients. Infect Dis Ther. 2019;8:301-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 52. | Álvarez-Mercado AI, Bujaldon E, Gracia-Sancho J, Peralta C. The Role of Adipokines in Surgical Procedures Requiring Both Liver Regeneration and Vascular Occlusion. Int J Mol Sci. 2018;19:3395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 53. | Trigui A, Rose CF, Bémeur C. Nutritional Strategies to Manage Malnutrition and Sarcopenia following Liver Transplantation: A Narrative Review. Nutrients. 2023;15:903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 54. | Pereira AZ, Gonçalves SEA, Rodrigues M, Hamerschlak N, Flowers ME. Challenging and Practical Aspects of Nutrition in Chronic Graft-versus-Host Disease. Biol Blood Marrow Transplant. 2020;26:e265-e270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 55. | Miyauchi T, Uchida Y, Kadono K, Hirao H, Kawasoe J, Watanabe T, Ueda S, Jobara K, Kaido T, Okajima H, Terajima H, Uemoto S. Preventive Effect of Antioxidative Nutrient-Rich Enteral Diet Against Liver Ischemia and Reperfusion Injury. JPEN J Parenter Enteral Nutr. 2019;43:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 56. | Li X, Lin Y, Li X, Xu X, Zhao Y, Xu L, Gao Y, Li Y, Tan Y, Qian P, Huang H. Tyrosine supplement ameliorates murine aGVHD by modulation of gut microbiome and metabolome. EBioMedicine. 2020;61:103048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 57. | Pan P, Atkinson SN, Taylor B, Zhu H, Zhou D, Flejsierowicz P, Wang LS, Morse M, Liu C, Gunsolus IL, Chen X. Retinoic Acid Signaling Modulates Recipient Gut Barrier Integrity and Microbiota After Allogeneic Hematopoietic Stem Cell Transplantation in Mice. Front Immunol. 2021;12:749002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 58. | Lindqvist C, Nordstedt P, Vidgren M, Nowak G. Protein intake early after liver transplantation and postoperative outcome: An observational study comparing two nutritional protocols. Nutrition. 2022;98:111635. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 59. | Vasco M, Paolillo R, Schiano C, Sommese L, Cuomo O, Napoli C. Compromised nutritional status in patients with end-stage liver disease: Role of gut microbiota. Hepatobiliary Pancreat Dis Int. 2018;17:290-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 60. | Sarin SK, Pande A, Schnabl B. Microbiome as a therapeutic target in alcohol-related liver disease. J Hepatol. 2019;70:260-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 188] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 61. | Andermann TM, Fouladi F, Tamburini FB, Sahaf B, Tkachenko E, Greene C, Buckley MT, Brooks EF, Hedlin H, Arai S, Mackall CL, Miklos D, Negrin RS, Fodor AA, Rezvani AR, Bhatt AS. A Fructo-Oligosaccharide Prebiotic Is Well Tolerated in Adults Undergoing Allogeneic Hematopoietic Stem Cell Transplantation: A Phase I Dose-Escalation Trial. Transplant Cell Ther. 2021;27:932.e1-932.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 62. | Holmes ZC, Tang H, Liu C, Bush A, Neubert BC, Jiao Y, Covington M, Cardona DM, Kirtley MC, Chen BJ, Chao NJ, David LA, Sung AD. Prebiotic galactooligosaccharides interact with mouse gut microbiota to attenuate acute graft-versus-host disease. Blood. 2022;140:2300-2304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 63. | Hussain SK, Dong TS, Agopian V, Pisegna JR, Durazo FA, Enayati P, Sundaram V, Benhammou JN, Noureddin M, Choi G, Ayoub WS, Lagishetty V, Elashoff D, Goodman MT, Jacobs JP. Dietary Protein, Fiber and Coffee Are Associated with Small Intestine Microbiome Composition and Diversity in Patients with Liver Cirrhosis. Nutrients. 2020;12:1395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 64. | Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021;13:886. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 218] [Article Influence: 54.5] [Reference Citation Analysis (0)] |
| 65. | Tang S, Chen Y, Deng F, Yan X, Zhong R, Meng Q, Liu L, Zhao Y, Zhang S, Chen L, Zhang H. Xylooligosaccharide-mediated gut microbiota enhances gut barrier and modulates gut immunity associated with alterations of biological processes in a pig model. Carbohydr Polym. 2022;294:119776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 66. | Zhao Y, Jiang Q. Roles of the Polyphenol-Gut Microbiota Interaction in Alleviating Colitis and Preventing Colitis-Associated Colorectal Cancer. Adv Nutr. 2021;12:546-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 67. | Yu LX, Schwabe RF. The gut microbiome and liver cancer: mechanisms and clinical translation. Nat Rev Gastroenterol Hepatol. 2017;14:527-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 412] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 68. | Ma J, Li J, Jin C, Yang J, Zheng C, Chen K, Xie Y, Yang Y, Bo Z, Wang J, Su Q, Wang J, Chen G, Wang Y. Association of gut microbiome and primary liver cancer: A two-sample Mendelian randomization and case-control study. Liver Int. 2023;43:221-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 44] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 69. | Chen W, Wen L, Bao Y, Tang Z, Zhao J, Zhang X, Wei T, Zhang J, Ma T, Zhang Q, Zhi X, Li J, Zhang C, Ni L, Li M, Liang T. Gut flora disequilibrium promotes the initiation of liver cancer by modulating tryptophan metabolism and up-regulating SREBP2. Proc Natl Acad Sci U S A. 2022;119:e2203894119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 50] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 70. | Feng L, Zhang W, Shen Q, Miao C, Chen L, Li Y, Gu X, Fan M, Ma Y, Wang H, Liu X, Zhang X. Bile acid metabolism dysregulation associates with cancer cachexia: roles of liver and gut microbiome. J Cachexia Sarcopenia Muscle. 2021;12:1553-1569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 71. | Fang J, Yu CH, Li XJ, Yao JM, Fang ZY, Yoon SH, Yu WY. Gut dysbiosis in nonalcoholic fatty liver disease: pathogenesis, diagnosis, and therapeutic implications. Front Cell Infect Microbiol. 2022;12:997018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 96] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 72. | Shi L, Sheng J, Wang M, Luo H, Zhu J, Zhang B, Liu Z, Yang X. Combination Therapy of TGF-β Blockade and Commensal-derived Probiotics Provides Enhanced Antitumor Immune Response and Tumor Suppression. Theranostics. 2019;9:4115-4129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 73. | Wang W, Xu S, Ren Z, Jiang J, Zheng S. Gut microbiota and allogeneic transplantation. J Transl Med. 2015;13:275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 74. | Álvarez-Mercado AI, Gulfo J, Romero Gómez M, Jiménez-Castro MB, Gracia-Sancho J, Peralta C. Use of Steatotic Grafts in Liver Transplantation: Current Status. Liver Transpl. 2019;25:771-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 75. | Bajaj JS, Kakiyama G, Cox IJ, Nittono H, Takei H, White M, Fagan A, Gavis EA, Heuman DM, Gilles HC, Hylemon P, Taylor-Robinson SD, Legido-Quigley C, Kim M, Xu J, Williams R, Sikaroodi M, Pandak WM, Gillevet PM. Alterations in gut microbial function following liver transplant. Liver Transpl. 2018;24:752-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 76. | Tian X, Yang Z, Luo F, Zheng S. Gut microbial balance and liver transplantation: alteration, management, and prediction. Front Med. 2018;12:123-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 77. | Ito T, Nakamura K, Kageyama S, Korayem IM, Hirao H, Kadono K, Aziz J, Younan S, DiNorcia J 3rd, Agopian VG, Yersiz H, Farmer DG, Busuttil RW, Kupiec-Weglinski JW, Kaldas FM. Impact of Rifaximin Therapy on Ischemia/Reperfusion Injury in Liver Transplantation: A Propensity Score-Matched Analysis. Liver Transpl. 2019;25:1778-1789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 78. | Jia J, Tian X, Jiang J, Ren Z, Lu H, He N, Xie H, Zhou L, Zheng S. Structural shifts in the intestinal microbiota of rats treated with cyclosporine A after orthotropic liver transplantation. Front Med. 2019;13:451-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |