Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.99423
Revised: November 29, 2024
Accepted: December 23, 2024
Published online: February 27, 2025
Processing time: 173 Days and 3.9 Hours
Laparoscopic cholecystectomy (LC) and laparoscopic common bile duct exploration (LCBDE) are widely used in gallbladder and biliary tract diseases. During these procedures, vessels or tissues are commonly ligated using clips. However, postoperative migration of clips to the common bile duct (CBD) or T-tube sinus tract is an overlooked complication of laparoscopic biliary surgery. Previously, most reported cases of postoperative clip migration involved metal clips, with only a few cases involving Hem-o-lok clips and review of the literature.
This report describes two cases in which Hem-o-lok clips migrated into the CBD and the T-tube sinus tract following laparoscopic surgery. Case 1 is a 68-year-old female admitted due to abdominal discomfort, and two Hem-o-lok clips were found to have migrated into the CBD 17 months after LC and LCBDE with T-tube drainage, and were removed using a stone extraction balloon. The patient was discharged smoothly after recovery. Case 2 is a 74-year-old male who underwent LC and LCBDE with T-tube drainage and laparoscopic biliary tract basket stone extraction. Nine weeks postoperatively, following T-tube removal, a Hem-o-lok clip was found in the sinus tract, and was extracted from the T-tube sinus tract. The patient recovered smoothly postoperatively. This study also reviews the literature from 2013 to July 2024 on using Hem-o-lok clips in LC and/or LCBDE treatment of gallbladder and biliary diseases and the postoperative migration of these clips into the CBD, T-tube sinus tract, or duodenum.
In patients with a history of LC and/or LCBDE, clip migration should be considered as a differential diagnosis.
Core Tip: Postoperative migration of clips is an overlooked complication of laparoscopic biliary surgery. This report describes two cases in which Hem-o-lok clips migrated into the common bile duct (CBD) and T-tube sinus tract after laparoscopic cholecystectomy (LC) and laparoscopic CBD (LCBDE) exploration operation. One clip was removed using a stone extraction balloon, while the other was expelled spontaneously without treatment. Furthermore, literature regarding clip migration following laparoscopic biliary surgery was reviewed. In patients with a history of LC and LCBDE presenting with biliary colic, cholangitis, or abdominal discomfort, clip migration should be considered a differential diagnosis.
- Citation: Huang YZ, Lin YY, Xie JP, Deng G, Tang D. Clip-stone and T clip-sinus post laparoscopic biliary surgery: Two case reports and review of the literature. World J Gastrointest Surg 2025; 17(2): 99423
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/99423.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.99423
Gallbladder and biliary tract diseases have a high incidence rate domestically and internationally. Currently, laparoscopic cholecystectomy (LC) and laparoscopic common bile duct exploration (LCBDE) are widely used in the surgical treatment of gallbladder and CBD stones[1,2]. Post-laparoscopic BD surgery, ligation clip migration is a rare but definite complication, with metallic clip migration being more common, while Hem-o-lok clip migration is less frequent[3-5]. According to a study report, among all complications after LC and LCBDE, 11.8% of patients experienced clip migration, with a 1.8% incidence of non-metallic clip migration[4]. In 1978, Walker et al[6] reported the first clip migration into the CBD after cholecystectomy, forming a gallstone with the clip as the core. Subsequently, similar cases have also been reported[7-15]. Moreover, studies have reported rare instances of clip migration into the CBD, T-tube tract, or duodenal bulb following LC and/or LCBDE[8,16].
Therefore, this article reports two cases of Hem-o-lok clip migration into the CBD or T-tube tract after LC and LCBDE in our department, and reviews the relevant literature from 2013 to July 2024, summarizing the diagnosis, mechanism, treatment, and prevention of Hem-o-lok clip migration into the biliary tract.
Case 1: A 68-year-old female patient was admitted on September 22, 2022, complaining of recurrent abdominal distension for over 8 years, worsening over the past 3 months.
Case 2: A 74-year-old male patient was admitted on January 18, 2023, for T-tube removal 9 weeks after biliary drainage.
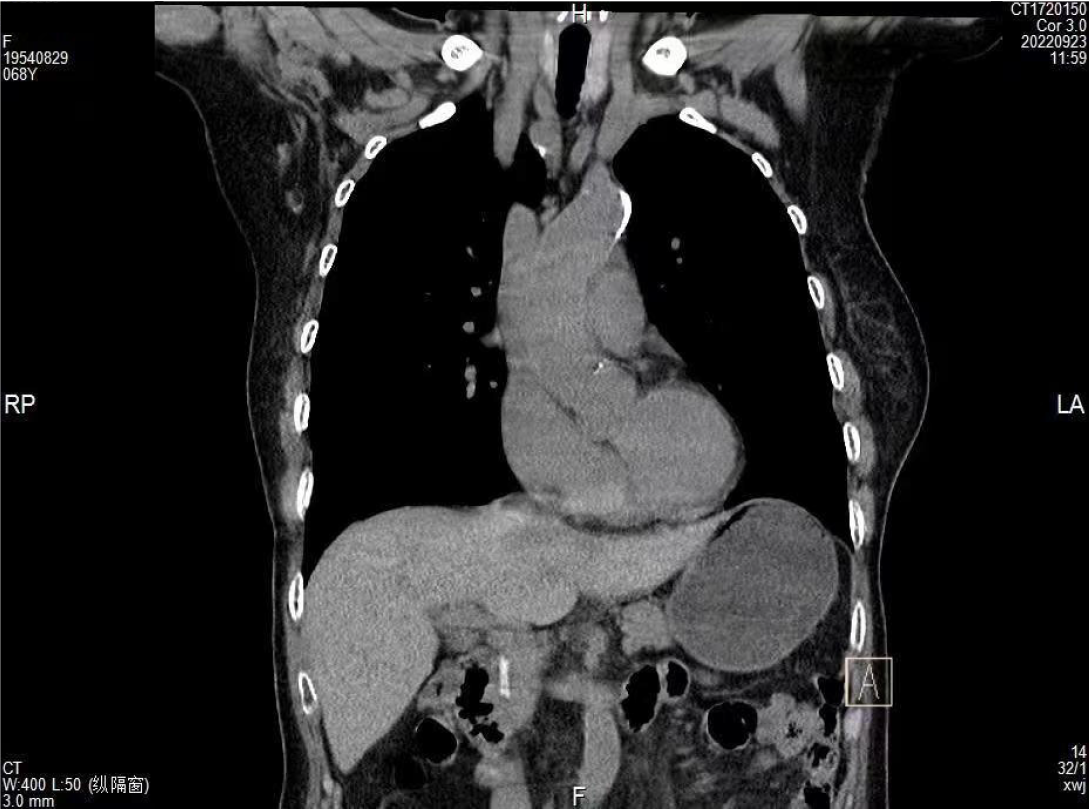
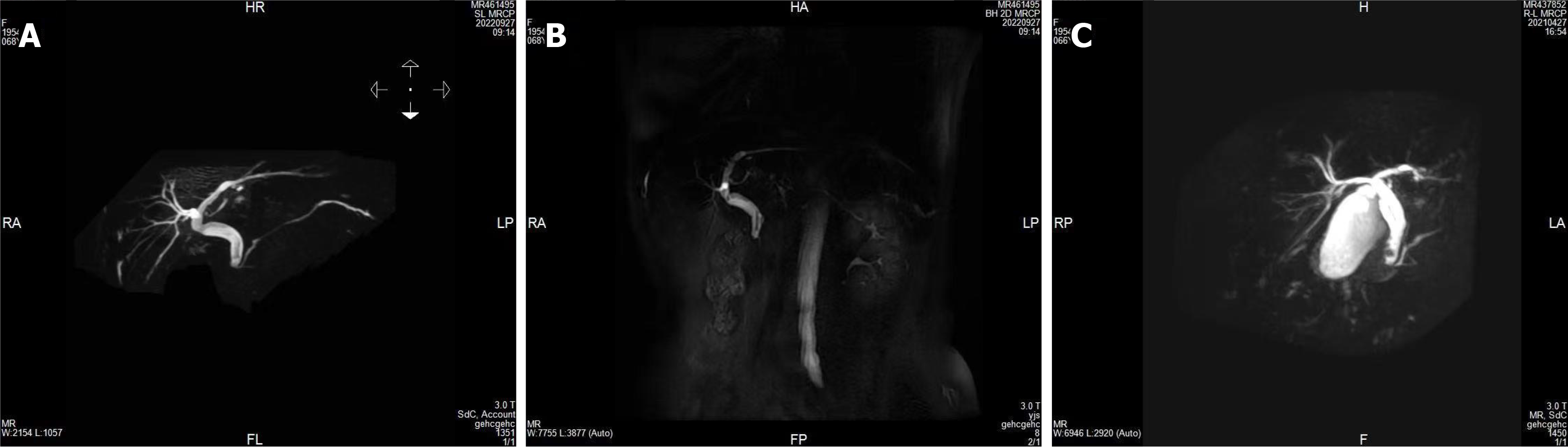
Case 1: Eight years prior, the patient experienced unexplained abdominal distension and poor appetite. More than 1 year ago (April 23, 2021), her symptoms worsened, accompanied by upper abdominal distension and pain. Upper abdominal magnetic resonance imaging (MRI) revealed multiple stones in the CBD and gallbladder, as well as chronic cholecystitis. Contraindications were excluded and the patient underwent LCBDE with stone extraction, T-tube drainage, and LC under general anesthesia, resulting in significant symptom relief post-surgery. Three months ago (July 11, 2022), the patient experienced a recurrence of the aforementioned symptoms. An abdominal ultrasound suggested possible sludge-like stones or biliary sludge in the CBD. Ten days ago (September 13, 2022), she sought medical attention again, and an endoscopy indicated chronic non-atrophic gastritis with erosive bleeding and mild bile reflux. The diagnoses considered were BD stones, post-cholecystectomy status, and chronic non-atrophic gastritis with bile reflux. Upon admission, a computed tomography (CT) scan showed a high-density shadow in the CBD (Figure 1), and magnetic resonance cholangiopancreatography (MRCP) suggested a filling defect in the BD (Figure 2).
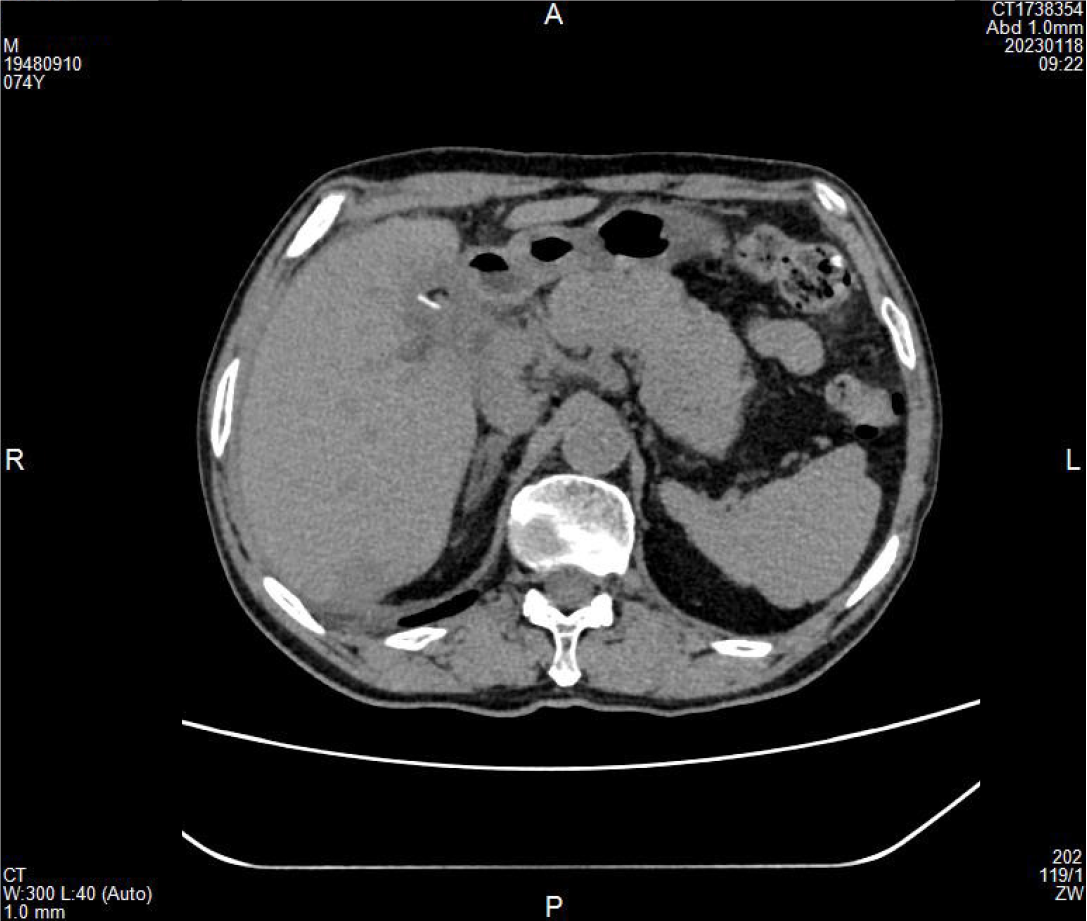
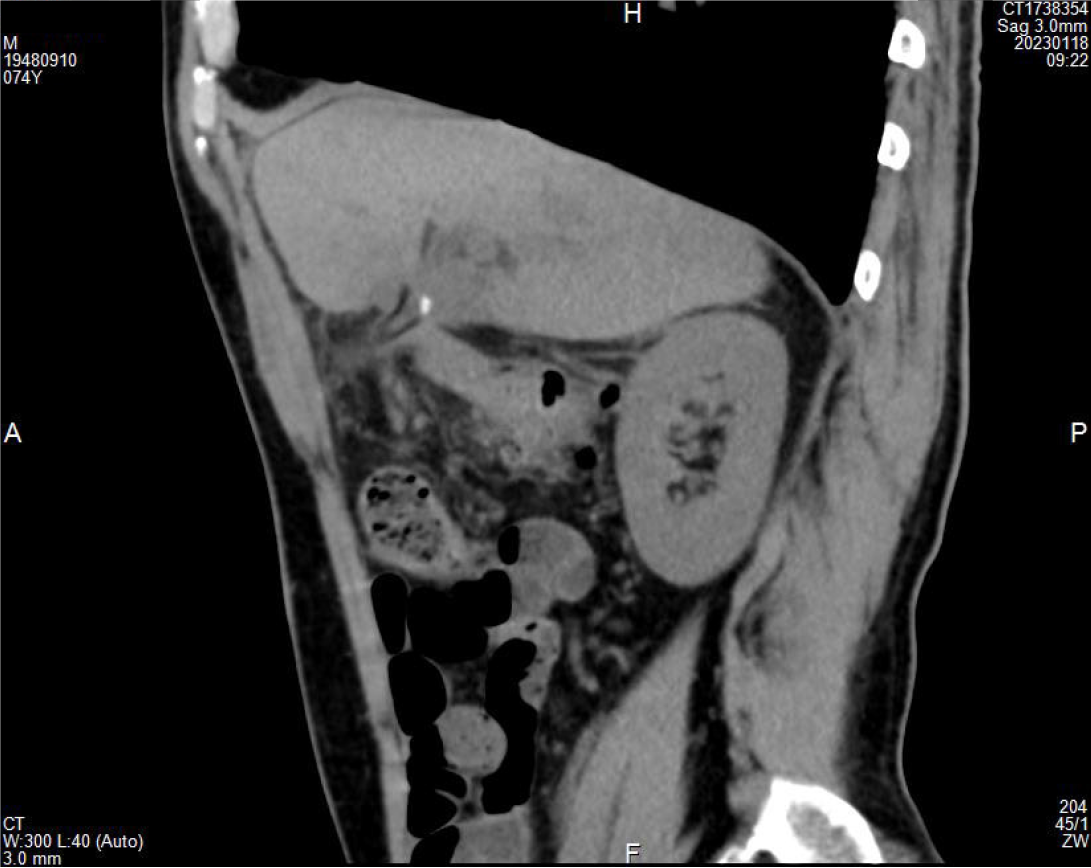
Case 2: Nine weeks prior (October 30, 2022), the patient was admitted to our hospital due to intermittent right upper abdominal pain and yellow urine for 1 day. An abdominal CT scan revealed multiple stones in the gallbladder and CBD, mild dilation of intrahepatic and extrahepatic BDs, an enlarged gallbladder, and multiple high-density spots in the right lobe of the liver, suggesting possible intrahepatic BD stones. After excluding surgical contraindications, the patient underwent endoscopic sphincterotomy (EST), endoscopic retrograde cholangiopancreatography (ERCP), and endoscopic nasobiliary drainage (ENBD) under local anesthesia (October 31, 2022). After 8 days, the patient underwent LCBDE with T-tube drainage, laparoscopic biliary tract basket stone extraction, and LC (November 8, 2022). He recovered well and was discharged. During this admission, a CT scan showed high-density shadows (Figures 3 and 4).
Case 1: The patient had no history of chronic diseases such as high blood pressure (BP), diabetes, and heart disease, and no history of infectious diseases such as hepatitis and tuberculosis.
Case 2: The patient had no history of chronic diseases such as high BP, diabetes, and heart disease, and had no history of infectious diseases such as hepatitis and tuberculosis. But the patient has a history of bronchial asthma and is treated regularly.
Case 1: There is no similar patient in the family, and his siblings are in good health. Grandparents, parents, brothers, and sisters have no history of hereditary disease.
Case 2: There is no similar patient in the family, and his siblings are in good health. Grandparents, parents, brothers, and sisters have no history of hereditary disease.
Case 1: Temperature 36.5 °C, P 84 times/min, BP 116/73 mmHg, and respiratory rate (RR) 18 times/min. The patient was conscious and energetic, with obvious stomachache. Anorexia was evident, with weight loss of 5 kg. The skin and sclera were not jaundiced. Superficial lymph nodes throughout the body were not palpable. There was no edema in both lower limbs. Specialist physical examination showed that the abdominal wall was soft, with no tenderness, no rebound tenderness, and no palpable mass, and the liver and spleen were not palpable under the ribs. Murphy's sign (-), shifting dullness (-). Bowel sounds were normal at 2 times/min.
Case 2: Temperature 36.5 °C, P 72 times/min, BP 131/73 mmHg, RR 18 times/min, and oxygen saturation 98%. The skin and sclera were not jaundiced. The neck was soft and superficial lymph nodes throughout the body were not palpable. Specialist physical examination showed a flat abdomen, no varicose veins in the abdominal wall, and no gastrointestinal pattern or peristaltic waves. The abdominal wall was soft, there was no tenderness in the whole abdomen, no rebound tenderness or muscle tension, Murphy's sign (-), the T-tube was in place, the fixation line was loose, the drainage was smooth, no mass was touched in the abdomen, and the liver and spleen were not touched under the ribs. The boundaries of liver dullness are percussion pain (-) and moving dullness (-) in the normal kidney area. Bowel sounds were normal at 4-6 times/min, and there was no circumference, percussion pain in the liver area (-), or vascular murmur. There was no edema in both lower limbs.
Case 1: July 8, 2022: Liver enzyme combination + liver function combination + electrolyte three items: Total bilirubin (TBIL) 28.99 μmol/L, direct bilirubin 10.10 μmol/L, indirect bilirubin 18.89 μmol/L.
Case 2: October 30, 2022 emergency liver enzymes + emergency liver function: TBIL 92.83 μmol/L, alanine aminotransferase 392 U/L, aspartate aminotransferase 532.86 U/L; October 30, 2022 emergency blood routine: White blood cells 10.41 × 109/L, neutrophil percentage 92.8%.
(1) BD stones; (2) Post cholecystectomy status; and (3) Chronic non-atrophic gastritis with bile reflux.
(1) CBD stones with acute suppurative cholangitis; (2) Bronchial asthma; and (3) Abnormal liver function.
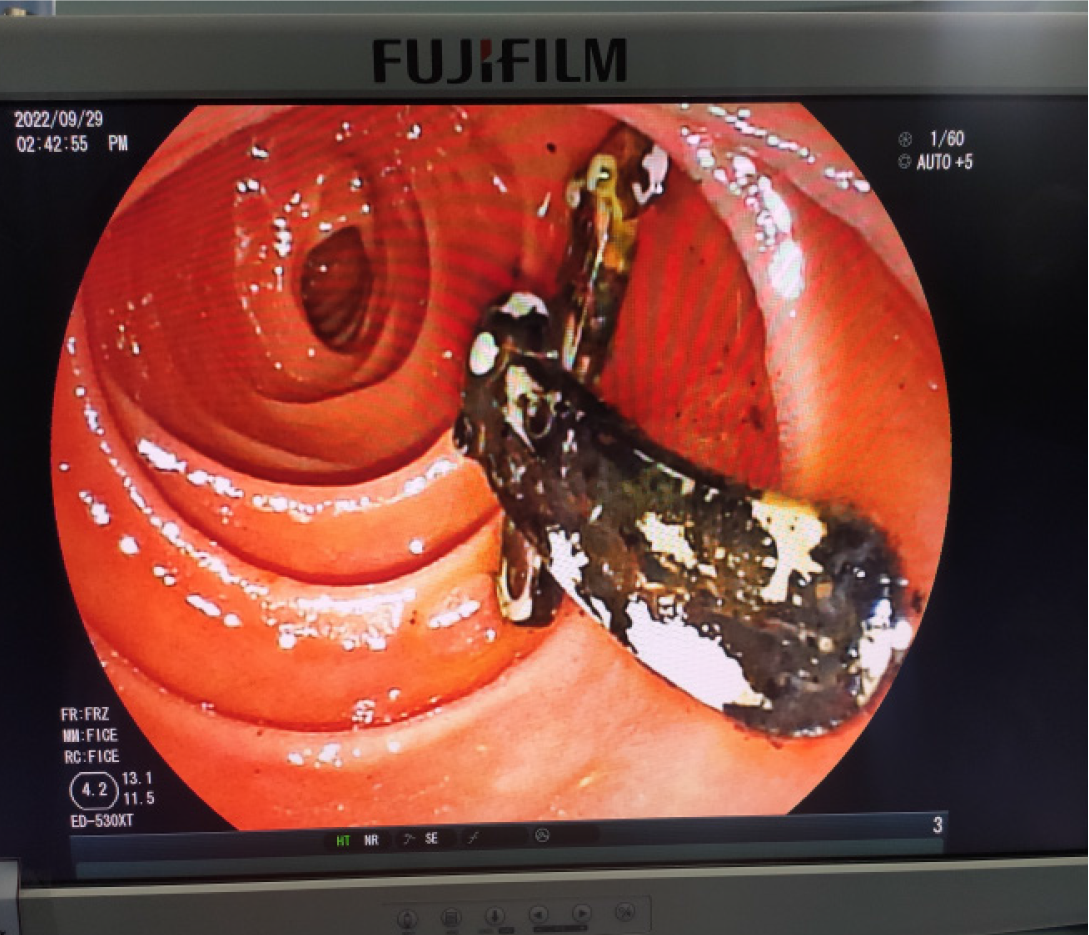
The patient underwent EST, ERCP, ENBD, and endoscopic balloon dilation. During surgery, two large Hem-o-lok clips were found (Figure 5), which were covered with black-brown stones (Figure 6). The stones were removed using a stone extraction balloon, and a nasobiliary drainage tube was placed post-surgery.
After completing relevant auxiliary examinations, the patient further received BD stone extraction via the fistula tract (January 18, 2023). A 3 mm choledochoscope was introduced through the original T-tube tract, revealing a brown stone inside the T-tube, which was removed along with the original T-tube. Stones and a small Hem-o-lok clip were found in the lumen. The ectopic Hem-o-lok clip was extracted from the T-tube sinus tract, and a 16 Fr T-tube was placed in the original sinus tract and fixed to the abdominal wall.
Ultimately, the patient was discharged smoothly after recovery.
The patient returned to the ward without any discomfort during the procedure and recovered smoothly.
With the widespread adoption of minimally invasive methods and the rapid development of laparoscopic surgery, LC and LCBDE have emerged as pivotal treatment strategies for patients with gallbladder and biliary tract diseases. Compared to open surgery, laparoscopic procedures offer numerous advantages, including smaller incisions, less trauma, faster postoperative recovery, shorter hospital stays, and fewer complications[17-19]. Moreover, ligation clips can effectively seal the cystic duct and blood vessels, improving surgical efficiency. Therefore, ligation clips have been increasingly used in biliary tract surgery. Initially, metallic titanium clips were adopted, but these clips were found to loosen, detach, migrate, and cause significant pathological changes in the surrounding tissues. In 1999, non-absorbable polymer Hem-o-lok clips were developed and introduced into laparoscopic surgery, demonstrating good sealing and biocompatibility. Hem-o-lok clips feature integrated anti-slip teeth, arched prongs, and flexible hinges, providing flexibility and secure ligation while minimizing interference with postoperative CT and MRI examinations[20]. Hence, Hem-o-lok clips are widely used in laparoscopic biliary surgery[21]. Despite the large number of laparoscopic gallbladder and biliary surgeries performed globally each year, reports of postoperative clip migration are rare, with only occasional cases mentioned.
The PubMed, Web of Science, MEDLINE, and Scopus databases were searched from 2013 to July 2024 using the keywords “clip migration and laparoscopic cholecystectomy or clip migration and LCBDE.” After screening, 17 articles were identified, describing 30 cases of Hem-o-lok clip migration following LC and/or LCBDE[7-16,22-27] (Table 1). Among previous laparoscopic surgeries, 14 cases involved both LC and LCBDE (47%), while 16 cases involved LC or LCBDE alone (53%). The patient ages ranged from 31 to 88 years. The time of migration ranged from 6 weeks to 4 years post-LC and/or LCBDE. Among these, 8 patients remained asymptomatic and were diagnosed as an incidental finding during surgical cholangioscopy or ERCP. The most common manifestations of clip migration were symptoms of acute cholecystitis and CBD obstruction, such as abdominal pain, fever, and chills. Some patients presented with jaundice, which was differentiated from non-iatrogenic CBD stones, or anemia, which required investigation for duodenal ulcers. In the 24 cases, the clips were wedged in the CBD. In three cases, the clips became part of the T-tube tract; in another three cases, the clips migrated into the duodenum. Most migrated Hem-o-lok clips were treated with surgical cholangioscopy or ERCP stone extraction, while clip migration into the duodenum was managed by endoscopic removal or observation.
| Ref. | Case number | Age | Initial operations | Time to clip migration after initial surgery | Migration site | Clinical manifestation | Imaging approach | Treatment for the migrated clips |
| Liu et al[16], 2024 | 1 | 72 | LC | 2 years | Duodenum | Abdominal pain | EGD, CT | EGD, biopsy forceps |
| Zhu et al[22], 2024 | 1 | 72 | LC | 2 years, 2 months | CBD | Upper abdominal pain, fever | MRCP, CT, ERCP | ERCP, stone basket |
| Wu et al[7], 2024 | 4 | 62-88 | LC + LCBDE | 17 months-24 months | CBD | Varying degrees of epigastric pain (2/4), epigastric pain with chills and fever (2/4) | MRI, MRCP, CT | LCBDE (1/4); LCBD, adhesions removed (3/4) |
| Slim et al[23], 2023 | 1 | 88 | LC | 6 months | CBD | Asymptomatism | ERCP | ERCP, balloon catheter |
| Liu et al[8], 2022 | 1 | 59 | LC + LCBDE | 2 months | CBD | Fever, acute right upper abdominal pain. | CT, ERCP | ERCP, stone basket |
| Tan et al[9], 2021 | 1 | 72 | LC + LCBDE | 4 years | CBD, the hepatic bile duct | Abdominal pain | MRCP, ultrasound | LCBDE, T-tube drainage |
| Kihara et al[10], 2021 | 1 | 80 | LC | 3 years | CBD | Asymptomatism (Inflammatory pseudotumor) | CT, MRCP | Laparoscopic bile duct resection and reconstruction, removed by ERCP |
| Jiang et al[11], 2021 | 1 | 67 | LCBDE | 12 months | CBD | Acute right upper abdominal pain | CT | LCBDE, primary closure |
| Desai et al[12], 2021 | 1 | 74 | LC | 1.5 years | CBD | Abdominal pain, nausea, vomiting | Endoscopic ultrasound, CECT, ERCP | ERCP |
| Roh et al[13], 2019 | 1 | 65 | LC | 13 months | CBD | Upper abdominal pain, fever | CT, ERCP | ERCP, balloon catheter |
| Kou et al[14], 2019 | 1 | 84 | LC+LCBDE | 3 years | CBD | Upper abdominal pain, chills, hyperpyrexia | ERCP, ENBD, LCBDE | LCBDE, T-tube biliary drainage |
| Pang et al[15], 2019 | 6 | 31-83 | LCBDE (5/6); LC (1/6) | 2 months-1.5 years | CBD (3/6), T-tube sinus (3/6) | Asymptomatism (3/6); Right upper abdominal pain (3/6) | CT (1/6); Choledochoscopy (3/6); Abdominal ultrasound (1/6); T-tube cholangiography, digital subtraction angiography of the biliary tract (1/6) | Choledochoscope, reticular basket (3/6); Exploratory laparotomy, bile duct exploration, and J tube drainage (1/6); Roux-en-Y (1/6); PTBD and stent implantation (1/6) |
| Rou et al[24], 2018 | 1 | 53 | LC | 10 months | CBD | Abdominal pain | CT | ERCP, stone basket |
| Zheng et al[4], 2018 | 6 | NA | LC + LCBDE T-tube drainage (4/6); LC + LCBDE primary closure (2/6) | 6 weeks-50 months | Duodenum (1/6), CBD (5/6) | Abdominal discomfort (1/6); Jaundice (2/6); Asymptomatism (3/6) | EGD (1/6); Laparotomy operation (1/6); Choledochoscope (1/6); Choledochoscope check through T-tube sinus (3/6) | Not processed (1/6); Laparotomy operation, stone retrieving basket (1/6); LCBDE, stone basket (4/6) |
| Qu et al[25], 2017 | 1 | 54 | LC + LCBDE, primary closure | 12 months | CBD | Intermittent upper abdominal pain | MRCP, ERCP | ENBD tube was inserted after ESBD |
| Ribeiro et al[26], 2016 | 1 | 75 | LC | 2 years | CBD | Abdominal pain | Abdominal ultrasound, ERCP | ERCP, balloon sweep |
| Seyyedmajidi et al[27], 2013 | 1 | 41 | LC | 8 months | Duodenum | Severe abdominal pain | Upper gastrointestinal endoscopic | Upper gastrointestinal endoscopy, olympus grasping forceps |
The exact mechanism underlying Hem-o-lok clip migration after laparoscopic biliary surgery remains incompletely understood. Based on previous literature, several possible mechanisms can be hypothesized. First, incomplete closure of the cystic duct may lead to the formation of a bile tumor, causing clip migration[7,8,25]. Second, surrounding structures may exert pressure on the clip[14,15,22]. Third, inflammation and necrosis of the tissue around the clip may result in fistula formation, leading to erosion of the BD wall, causing the clip to enter the CBD or even the duodenum. Additionally, the clip itself may also trigger an immune rejection reaction and infection, resulting in migration[11,12,14,16,22,27]. Fourth, improper surgical techniques, including excessive or incorrectly placed clips, may damage the BD and surrounding structures, accelerating migration[13]. Fifth, certain anatomical factors might affect the stability of the clip[10,15,28]. Finally, increased abdominal pressure or exacerbation of pre-existing pathological conditions in the patient may affect the stability of the clip, leading to migration[13]. In this study, 1 patient had an ectopic clip in the T-tube sinus tract, which may be due to the clip being placed too close to the T-tube sinus. In another patient, the migrated clip was found in the CBD, possibly due to increased fragility of the BD wall caused by local inflammation around the clip. Moreover, the clip itself is a foreign object and may elicit a rejection reaction.
Hem-o-lok clip migration in the BD typically does not cause noticeable symptoms in the early stages. Abdominal discomfort may only occur when clamping the T-tube before its removal. Furthermore, the long-term presence of a Hem-o-lok clip in the BD can alter BD motility, potentially becoming a site for gallstone formation and possibly causing cholangitis. Clip migration to the duodenum may cause duodenal ulcer and perforation, presenting clinical manifestations similar to other conditions, such as CBD stones, cholangitis, or duodenal ulcers[29]. Preoperative imaging studies such as CT and MRI often cannot clearly distinguish between Hem-o-lok clips and stones, requiring surgical cholangioscopy or ERCP. Patients with clip migration to the duodenal bulb may manifest atypical clinical symptoms. Hence, for patients undergoing LC or LCBDE who present with recurrent abdominal pain, clinicians should be aware of the possibility of Hem-o-lok clip displacement and consider scheduling CT scans and gastroscopy[16]. Notably, all types of surgical clips carry a risk of migration. Due to the lack of specific clinical symptoms and imaging features, clip migration is often confused with CBD stones or duodenal ulcers, potentially misleading physicians and causing delays in diagnosis and treatment.
With the rapid development of endoscopic technology, ERCP and cholangioscopy have emerged as the preferred methods for managing clip migration, offering advantages such as speed, cost-effectiveness, minimal invasiveness, and fewer complications[11,14,15,26]. According to the article, preoperative ERCP combined with LC is associated with a higher rate of CBD stone clearance and a lower rate of postoperative bile leakage compared to LCBDE + LC, while LCBDE + LC may be associated with shorter hospital stays[7,30]. In this study, 1 of the 2 patients had the migrated clip identified and removed through the sinus tract via cholangioscopy, as the T-tube had not yet been removed. The other patient presented with significant symptoms 17 months post-surgery, and had the clip removed via ERCP without the need for a CBD incision, resulting in less trauma and faster recovery. According to previous research, Hem-o-lok clips migrated into the CBD should be removed regardless of symptoms[7,8,22,23]. For clips migrated into the duodenum, symptomatic cases should be managed endoscopically or surgically, while asymptomatic cases may consider conservative treatment[16]. Therefore, treatment plans should be individualized based on the patient's condition to optimize safety, while minimizing trauma and medical resources.
Although reports of Hem-o-lok clip migration into the biliary tract are relatively rare, the increasing use of Hem-o-lok clips in laparoscopic biliary surgery has led to a gradual rise in such cases, which warrants our attention. Surgeons should be vigilant in employing proper techniques, selecting clips appropriately, or exploring alternative methods. In patients with a history of LC or LCBDE who present with biliary colic, cholangitis, or abdominal discomfort, clip migration into the biliary tract or other body parts should be considered a differential diagnosis. Further research will provide a deeper understanding of this postoperative complication, promoting the development of more suitable solutions.
Although Migration of the Hem-o-lok clip to the CBD, T-tube sinus tract or duodenum are relatively rare, the increasing use of Hem-o-lok clips in laparoscopic biliary surgery has led to a gradual rise in such cases, which warrants our attention. Surgeons should be vigilant in employing proper techniques, choosing and using clips appropriately, or exploring alternative methods. In patients with a history of LC and/or LCBDE who present with biliary colic, cholangitis, or abdominal discomfort, clip migration into the biliary tract or duodenum should be considered a differential diagnosis. It is believed that we will gain a deeper understanding of this postoperative complication over time and discover more suitable solutions.
| 1. | European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65:146-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 346] [Article Influence: 38.4] [Reference Citation Analysis (2)] |
| 2. | Lan WF, Li JH, Wang QB, Zhan XP, Yang WL, Wang LT, Tang KZ. Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography combined with laparoscopic cholecystectomy for patients with gallbladder and common bile duct stones a meta-analysis of randomized controlled trials. Eur Rev Med Pharmacol Sci. 2023;27:4656-4669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 3. | Chong VH, Chong CF. Biliary complications secondary to post-cholecystectomy clip migration: a review of 69 cases. J Gastrointest Surg. 2010;14:688-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Zheng Y, Wang Y, Bai X, Liu D, Li F. Letter to the editor on "The cystic duct and artery were clipped using a clip applier". Nonmetal clip migration after laparoscopic cholecystectomy. Asian J Surg. 2018;41:585-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Singh R, Arumugam P, Mathur K, Deo A. Post-cholecystectomy Clip Migration: A Case Report. Cureus. 2024;16:e58580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Walker WE, Avant GR, Reynolds VH. Cholangitis with a silver lining. Arch Surg. 1979;114:214-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Wu X, Yan H, Zhao S, Zhang X, Zhu K. Clip migration complicated by choledocholithiasis after laparoscopic biliary surgery: a report of four cases. J Int Med Res. 2023;51:3000605231190766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Liu DR, Wu JH, Shi JT, Zhu HB, Li C. Hem-o-lok clip migration to the common bile duct after laparoscopic common bile duct exploration: A case report. World J Clin Cases. 2022;10:6548-6554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 9. | Tan Z, Wan R, Qian H, Xie P. Migration of Hem-o-lok clip into the common hepatic duct after laparoscopic bile duct exploration: A case report. Clin Case Rep. 2021;9:e04834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Kihara Y, Takeda Y, Ohmura Y, Katsura Y, Shinke G, Ikeshima R, Katsuyama S, Kawai K, Hiraki M, Sugimura K, Masuzawa T, Takeno A, Hata T, Murata K. Migration of non-absorbable polymer clips in hepato-biliary-pancreatic surgery: a report of four cases. Surg Case Rep. 2021;7:183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Jiang C, Liu X, Li S, Wu G, Wang G, Wang M. Laparoscopic treatment of a recurrent biliary stone forming around a Hem-o-lok clip in a patient with previous gastrectomies: Case report. Medicine (Baltimore). 2021;100:e27213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Desai PN, Patel CN, Kabrawala MV, Nandwani SK, Mehta RM, Kalra P, Prajapati R, Patel N, Parekh KK. Foreign bodies in common bile duct in post cholecystectomy status—case series of 8 cases—A single center experience in western India. Int J Gastrointest Interv. 2021;10:84-88. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Roh YJ, Kim JW, Jeon TJ, Park JY. Common bile duct stone development due to a Hem-o-lok clip migration: a rare complication of laparoscopic cholecystectomy. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Kou K, Liu X, Hu Y, Luo F, Sun D, Wang G, Li Y, Chen Y, Lv G. Hem-o-lok clip found in the common bile duct 3 years after laparoscopic cholecystectomy and surgical exploration. J Int Med Res. 2019;47:1052-1058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Pang L, Yuan J, Zhang Y, Wang Y, Kong J. Clip-stone and T clip-sinus: A clinical analysis of six cases on migration of clips and literature review from 1997 to 2017. J Minim Access Surg. 2019;15:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Liu HY, Yin AH, Wei Z. Hem-o-lok clip migration to duodenal bulb post-cholecystectomy: A case report. World J Gastrointest Surg. 2024;16:1461-1466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81:1362-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 181] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Shamiyeh A, Wayand W. Current status of laparoscopic therapy of cholecystolithiasis and common bile duct stones. Dig Dis. 2005;23:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Grubnik VV, Tkachenko AI, Ilyashenko VV, Vorotyntseva KO. Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg Endosc. 2012;26:2165-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 20. | Meng MV. Reported failures of the polymer self-locking (Hem-o-lok) clip: review of data from the Food and Drug Administration. J Endourol. 2006;20:1054-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Madhavan S, Pandey A, Masood S, Kumar S, Chauhan S, Kumar D, Jha S. Polymeric locking clips [Hem-o-lok] versus Metallic clips in elective Laparoscopic Cholecystectomy: A Retrospective study of 1496 patients. Pol Przegl Chir. 2021;93:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Zhu Z, Wang J, Li C, Wei G, Wang Y. A case of Hem-o-lok clip migrating to common bile duct after laparoscopic cholecystectomy. Asian J Surg. 2024;47:4117-4118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 23. | Slim R, Safar C, Osseis M. A Double Clip Slip. Clin Gastroenterol Hepatol. 2023;21:A20. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Rou WS, Joo JS, Kang SH, Moon HS, Kim SH, Sung JK, Lee BS, Lee ES. [Abdominal Pain Due to Hem-o-lok Clip Migration after Laparoscopic Cholecystectomy]. Korean J Gastroenterol. 2018;72:313-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Qu JW, Wang GY, Yuan ZQ, Li KW. Hem-o-lok Clips Migration: An Easily Neglected Complication after Laparoscopic Biliary Surgery. Case Rep Surg. 2017;2017:7279129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Ribeiro I, Pinho R, Proença L, Carvalho J. A strange finding in the common bile duct. Gastroenterol Hepatol. 2016;39:531-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Seyyedmajidi M, Hosseini SA, Hajiebrahimi S, Vafaeimanesh J. Hem-o-Lok Clip in the First Part of Duodenum after Laparoscopic Cholecystectomy. Case Rep Gastrointest Med. 2013;2013:251634. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Xia Y, Gao XF, Shi CY, Jiang YH, Yi X. Migration of hem-o-lock clips and stitches into the duodenum after laparoscopic hepatectomy and cholecystectomy: A case report. Medicine (Baltimore). 2019;98:e18153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Barabino M, Luigiano C, Piccolo G, Pellicano R, Polizzi M, Giovenzana M, Santambrogio R, Pisani Ceretti A, Andreatta E, Palamara MA, Giacobbe G, Consolo P, Opocher E. Hem-o-Lok clip migration into the duodenum after laparoscopic digestive surgery: a systematic review. Minerva Chir. 2019;74:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Lyu Y, Cheng Y, Li T, Cheng B, Jin X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc. 2019;33:3275-3286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 92] [Article Influence: 13.1] [Reference Citation Analysis (0)] |