Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.96493
Revised: October 17, 2024
Accepted: November 29, 2024
Published online: February 27, 2025
Processing time: 258 Days and 19.1 Hours
Ischemic bowel disease (IBD) is a critical condition caused by reduced blood flow to the intestines, leading to tissue damage and potentially severe complications. Early recognition and timely management are essential for improving patient outcomes and reducing morbidity and mortality associated with IBD.
To evaluate the knowledge, attitude and practice (KAP) of healthcare professionals regarding IBD.
This cross-sectional study was conducted among healthcare professionals in China from November 2023 to December 2023 using a self-designed question
A total of 315 valid questionnaires were analyzed, with 215 participants (68.25%) being female. The mean KAP scores were 17.55 ± 5.35 (range: 0-24), 27.65 ± 2.77 (range: 8-40), and 18.88 ± 4.23 (range: 6-30), respectively. Multivariate linear regre
Healthcare professionals demonstrated adequate knowledge but moderate attitude and inactive practice regarding IBD. Addressing the gaps in attitude and practice through targeted training programs and interventions is essential for improving patient care and outcomes.
Core Tip: Ischemic bowel disease (IBD) poses a significant clinical challenge due to its potential for severe complications. This study highlights the knowledge, attitude and practice of healthcare professionals regarding IBD. Although knowledge levels were adequate, attitudes were moderate, and practices were inactive. Targeted training programs and interventions are essential to enhance patient care and outcomes in the management of IBD.
- Citation: Ying M, Li YJ, Chen Y, Fu MY, Zhang G. Healthcare professionals' knowledge, attitude and practice towards ischemic bowel disease. World J Gastrointest Surg 2025; 17(2): 96493
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/96493.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.96493
Ischemic bowel disease (IBD), a heterogeneous group of disorders caused by insufficient oxygenated blood supply to the bowel walls, is associated with significant morbidity and mortality, as reported in previous studies[1-3]. This condition includes acute and chronic mesenteric ischemia (CMI) as well as colon ischemia, arising primarily from pathophy
The knowledge, attitude and practice (KAP) survey is a structured tool designed to assess cognitive levels, attitudes, and behaviors toward specific medical topics, including IBD[8-10]. Evaluating healthcare professionals' KAP levels provides insights into their understanding of the disease, attitudes toward patients, and clinical coping strategies. This method is essential for identifying gaps among healthcare professionals, enabling the development of targeted strategies to improve diagnosis and treatment.
Additionally, the complexity and multidisciplinary treatment requirements of IBD underscore the importance of understanding healthcare professionals' KAP levels. Identifying gaps in interdisciplinary collaboration is vital for improving patient outcomes. While existing research primarily addresses the basic science of the disease, further investigation is needed into the role of healthcare professionals in diagnosing and managing it and their overall understanding of the condition. Therefore, this study aimed to evaluate the KAP of healthcare professionals regarding IBD.
This cross-sectional study was conducted between November 2023 and December 2023 at the Second Affiliated Hospital of Shandong First Medical University.
Inclusion criteria: (1) Healthcare professionals working in the departments of general surgery, cardiology, gastroenterology, emergency medicine, and those on rotation in gastroenterology; and (2) Individuals who provided informed consent to participate in the study.
Exclusion criteria: (1) Medical students; (2) Resident physicians; and (3) Healthcare professionals lacking the requisite qualifications.
The study received ethical approval from the Ethics Committee of Shandong First Medical University Second Affiliated Hospital (Ethics Approval Number: 2023-096), and informed consent was obtained from all participants via the first page of the questionnaire.
The questionnaire was adapted from a previous study[11] and revised accordingly. A preliminary pilot study with 27 participants yielded a Cronbach's α coefficient of 0.894 for the overall questionnaire. Specifically, the knowledge section achieved a coefficient of 0.888, the attitude section scored 0.824, and the practice section scored 0.773. The final questionnaire, written in Chinese, includes four main components: (1) Demographic information (including age, gender, years of professional experience, education level, professional title, position, hospital grade, department, participation in IBD training, and the number of patients admitted in the past month); (2) Knowledge dimension; (3) Attitude dimension; and (4) Practice dimension. Within the knowledge dimension, participants respond to 13 questions. Responses are scored as 2 points for "very familiar", 1 point for "somewhat familiar", and 0 points for "not familiar at all". Question 4 is excluded from scoring and used solely for descriptive analysis. The total knowledge score ranges from 0 to 24 points. The attitude dimension comprises 6 questions rated on a five-point Likert scale, ranging from "strongly agree" (5 points) to "strongly disagree" (1 point). The total attitude score ranges from 8 to 40 points. In the practice dimension, participants respond to 8 questions, with responses varying from very positive behavior (5 points) to very negative behavior (1 point) for questions 1-6. Questions 7 and 8 are reserved for descriptive analysis. The total practice score ranges from 6 to 30 points. A score exceeding 70% of the maximum possible score in each section indicates adequate knowledge, a positive attitude, and proactive practice[12].
This study employed a convenience sampling method. Questionnaires were distributed electronically to participants via WeChat and QQ groups for healthcare professionals. The distribution process utilized Questionnaire Star (https://www.wjx.cn), allowing participants to access and complete the survey by scanning a QR code using WeChat or following a provided link. To ensure data quality and comprehensive responses, each IP address was limited to one submission, and all questionnaire items were mandatory. Participants were assured of anonymity throughout the survey process.
To maintain data integrity, a research team of three trained doctors acted as research assistants to promote and distribute the questionnaire. They reviewed all submissions to ensure completeness, internal consistency, and logical coherence. The team received training to fully understand the research objectives and survey process, improving the accuracy and reliability of the collected data. Questionnaires with logical errors, incomplete answers, or uniform responses across all items were deemed invalid.
The minimum required sample size was calculated as 10 times the number of predictors to ensure robust statistical analysis[13]. With 27 independent variables in the questionnaire, the recommended minimum sample size was 270. Accounting for a 10% non-response rate, the final required sample size was determined to be 300.
Statistical analysis was performed using Stata 14.0 (Stata Corporation, College Station, TX, United States). Continuous variables were reported as mean ± SD, and between-group comparisons were conducted using t-tests or analysis of variance (ANOVA). Categorical variables were presented as n (%). Pearson correlation analysis was used to evaluate correlations between KAP scores. Univariate variables with P < 0.05 were included in multivariate linear regression analysis. Structural equation modeling (SEM) was used to test the hypotheses that knowledge influences attitude, attitude influences practice, and knowledge influences practice. Two-sided P < 0.05 was considered statistically significant.
Initially, a total of 316 questionnaires were collected. The following samples were excluded: 2 cases where the response time was < 60 seconds and 9 cases where it was < 90 seconds; 5 cases where participants declined to answer; 4 cases where all responses in the knowledge dimension were marked as "c. Not familiar" (excluding K4); and 32 cases where trap questions were answered incorrectly. This resulted in 315 valid questionnaires, with an effective response rate of 99.68%. The mean KAP scores were 17.55 ± 5.35 (range: 0-24) for knowledge, 27.65 ± 2.77 (range: 8-40) for attitude, and 18.88 ± 4.23 (range: 6-30) for practice. Of the respondents, 215 (68.25%) were female, 260 (82.54%) were aged 26-45 years, 164 (52.06%) had a bachelor's degree or below, 175 (55.56%) had more than 10 years of work experience, 187 (59.37%) worked in gastroenterology, 154 (48.89%) had attended training on IBD, and 283 (89.84%) had treated or cared for 0-5 patients with IBD in the past month. Healthcare professionals with different levels of education, professional titles, positions, hospital grades, departments, participation in training, and the number of patients admitted in the past month showed significant differences in knowledge (all P < 0.05). Differences in attitude were observed based on education, professional title, position, and department (all P < 0.05). Practice differences were associated with department, training participation, and the number of patients admitted in the past month (all P < 0.05; Table 1).
| n = 315 | n (%) | Knowledge | Attitude | Practice | |||
| mean ± SD | P value | mean ± SD | P value | mean ± SD | P value | ||
| Total score | 17.55 ± 5.35 | 27.65 ± 2.77 | 18.88 ± 4.23 | ||||
| Age (years) | 0.078 | 0.182 | 0.681 | ||||
| Under 25 | 15 (4.76) | 14.26 ± 5.37 | 26.06 ± 3.97 | 19.8 ± 3.42 | |||
| 26-35 | 126 (40) | 17.99 ± 5.03 | 27.88 ± 2.84 | 18.77 ± 3.85 | |||
| 36-45 | 134 (42.54) | 17.53 ± 5.57 | 27.67 ± 2.50 | 18.76 ± 4.73 | |||
| Over 45 | 40 (12.7) | 17.42 ± 5.32 | 27.4 ± 2.70 | 19.27 ± 3.85 | |||
| Gender | 0.921 | 0.307 | 0.352 | ||||
| Male | 100 (31.75) | 17.68 ± 5.02 | 28.02 ± 2.41 | 19.32 ± 4.20 | |||
| Female | 215 (68.25) | 17.48 ± 5.50 | 27.47 ± 2.90 | 18.67 ± 4.23 | |||
| Education | 0.001 | < 0.001 | 0.057 | ||||
| Bachelor’s degree and below | 164 (52.06) | 16.49 ± 5.80 | 26.97 ± 3.09 | 18.39 ± 4.84 | |||
| Master’s degree and above | 151 (47.94) | 18.69 ± 4.57 | 28.37 ± 2.13 | 19.41 ± 3.37 | |||
| Years of professional experience, years | 0.313 | 0.423 | 0.914 | ||||
| 1 to 3 | 46 (14.6) | 16.80 ± 4.93 | 27.5 ± 3.18 | 18.97 ± 4.20 | |||
| 4 to 6 | 40 (12.7) | 18.55 ± 5.24 | 28 ± 3.30 | 19.45 ± 4.01 | |||
| 7 to 10 | 54 (17.14) | 17.55 ± 5.31 | 27.77 ± 2.47 | 19.18 ± 3.13 | |||
| > 10 | 175 (55.56) | 17.51 ± 5.50 | 27.56 ± 2.61 | 18.63 ± 4.57 | |||
| Professional title | < 0.001 | 0.045 | 0.214 | ||||
| Junior and below | 96 (30.48) | 15.91 ± 5.17 | 26.96 ± 3.15 | 18.25 ± 4.48 | |||
| Intermediate | 143 (45.4) | 17.75 ± 5.33 | 27.81 ± 2.68 | 19.04 ± 4.00 | |||
| Vice/senior | 76 (24.13) | 19.22 ± 5.08 | 28.18 ± 2.20 | 19.38 ± 4.26 | |||
| Position | 0.002 | < 0.001 | 0.107 | ||||
| Doctor | 230 (73.02) | 17.96 ± 5.03 | 27.97 ± 2.42 | 18.96 ± 3.85 | |||
| Department (vice) director | 31 (9.84) | 18.64 ± 5.71 | 28.54 ± 2.12 | 19.90 ± 5.60 | |||
| Nurse/nursing supervisor | 54 (17.14) | 15.14 ± 5.87 | 25.74 ± 3.56 | 17.92 ± 4.71 | |||
| Hospital grade | 0.001 | 0.277 | 0.655 | ||||
| Tertiary hospital | 217 (68.89) | 18.17 ± 4.93 | 27.70 ± 2.74 | 18.89 ± 3.69 | |||
| Secondary hospital | 58 (18.41) | 17.43 ± 5.77 | 27.94 ± 2.54 | 19.22 ± 4.38 | |||
| Primary hospital/other | 40 (12.70) | 14.35 ± 5.85 | 26.92 ± 3.14 | 18.32 ± 6.29 | |||
| Department | < 0.001 | 0.045 | 0.006 | ||||
| Emergency/intensive care unit/general surgery | 29 (9.21) | 17.17 ± 4.50 | 28.58 ± 2.14 | 18.58 ± 3.77 | |||
| Gastroenterology | 187 (59.37) | 19.06 ± 4.96 | 27.83 ± 2.61 | 19.47 ± 3.79 | |||
| Cardiology | 27 (8.57) | 16.03 ± 4.63 | 27.18 ± 2.74 | 18.55 ± 3.43 | |||
| Other | 72 (22.86) | 14.31 ± 5.34 | 26.95 ± 3.22 | 17.58 ± 5.35 | |||
| Participation in training on ischemic bowel disease | < 0.001 | 0.214 | < 0.001 | ||||
| Yes | 154 (48.89) | 19.76 ± 4.44 | 27.85 ± 2.68 | 19.88 ± 3.75 | |||
| No | 161 (51.11) | 15.42 ± 5.29 | 27.45 ± 2.83 | 17.92 ± 4.43 | |||
| Number of patients admitted in the past month | < 0.001 | 0.856 | < 0.001 | ||||
| 0-5 cases | 283 (89.84) | 17.10 ± 5.33 | 27.62 ± 2.80 | 18.64 ± 4.30 | |||
| > 5 cases | 32 (10.16) | 21.43 ± 3.70 | 27.81 ± 2.48 | 20.96 ± 2.71 | |||
In the knowledge dimension, the question with the highest percentage of participants selecting "Very familiar" was "Colonoscopy is the primary diagnostic method for ischemic colitis" (K2), with 62.54%. Conversely, the question most commonly marked as "Somewhat familiar" was "Medications such as cocaine, danazol, digoxin, estrogen, phenylpropanolamine, diuretics, and nonsteroidal anti-inflammatory drugs can contribute to the occurrence of IBD in the elderly" (K9), with 56.83%. Regarding the most valuable diagnostic method for ischemic colitis, 51.11% considered endoscopy, while 47.62% considered ultrasound (B-mode; K4; Supplementary Table 1).
Responses in the attitude dimension revealed that 66.98% strongly agreed that early diagnosis of IBD is important for patient prognosis (A1). Similarly, 67.3% strongly agreed that timely and accurate clinical diagnosis is critical for patient outcomes (A3), and 69.21% strongly agreed that healthcare professionals should receive more training and education on IBD (A4; Supplementary Table 2).
Regarding related practices, 35.24% and 32.7% of participants reported sometimes experiencing missed diagnoses (P1) and delayed diagnoses (P2) of IBD, respectively. Positively, 46.03% stated that they always pay close attention to patients with suspected IBD and aim to make a diagnosis as soon as possible (P4). For factors contributing to the early diagnosis of IBD without infarction (P7), 86.03% identified the presence of cardiovascular risk factors, while 70.48% mentioned abdominal pain with tenderness. Similarly, the same two factors were reported as the most useful for making a correct diagnosis of IBD (P8), with 69.21% and 64.44%, respectively (Supplementary Table 3).
In the correlation analysis, significant positive correlations were observed between knowledge and attitude (r = 0.433, P < 0.001), knowledge and practice (r = 0.377, P < 0.001), and attitude and practice (r = 0.250, P < 0.001).
Multivariate linear regression analysis showed that the following factors were independently associated with knowledge: Age 26–35 years (β = 2.80, 95%CI: 0.31-5.30, P = 0.028), vice or senior professional title (β = 2.66, 95%CI: 0.91-4.41, P = 0.003), being a nurse or nursing supervisor (β = -3.78, 95%CI: -5.45 to -2.11, P < 0.001), participation in IBD training (β = 3.45, 95%CI: 2.39-4.51, P < 0.001), and managing more than five IBD cases in the past month (β = 3.25, 95%CI: 1.58-4.92, P < 0.001; Supplementary Table 4). Knowledge (β = 0.20, 95%CI: 0.15-0.26, P < 0.001) and being a nurse or nursing supervisor (β = -1.30, 95%CI: -2.16 to -0.4, P = 0.003) were independently associated with attitude (Supplementary Table 5). Additionally, knowledge (β = 0.20, 95%CI: 0.10-0.30, P < 0.001) and attitude (β = 0.24, 95%CI: 0.06-0.42, P = 0.007) were independently associated with practice (Supplementary Table 6).
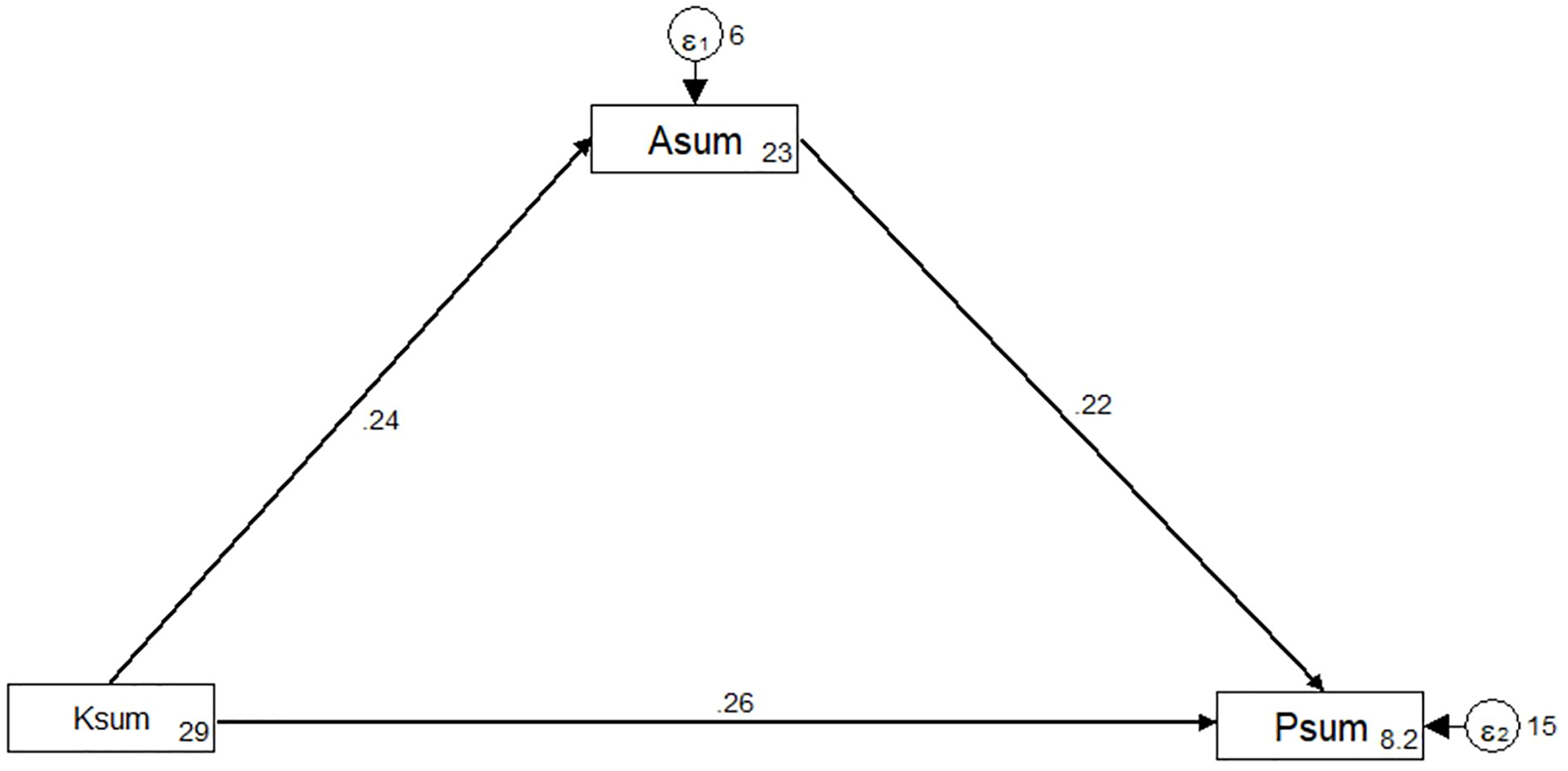
The fit indices of the SEM model were within the desired range, indicating good model fit (Supplementary Table 7). The analysis showed direct effects of knowledge on attitude (β = 0.24, P < 0.001) and practice (β = 0.26, P < 0.001), as well as attitude on practice (β = 0.22, P = 0.012; Table 2 and Figure 1).
Healthcare professionals demonstrated sufficient knowledge but suboptimal attitude and inactive practice regarding IBD. SEM revealed direct effects of knowledge on attitude and practice, as well as of attitude on practice. A key finding of this study is the clear gap between healthcare professionals' knowledge and their attitude and practice toward IBD. While participants exhibited adequate knowledge, their attitude and practice remained suboptimal. This highlights the need to address not only knowledge but also attitude and practice in training programs, as knowledge alone may not necessarily lead to effective clinical practice. These findings align with previous studies that emphasized the importance of comprehensive training programs to bridge the gap between knowledge and practice in healthcare settings[14,15].
The study also identified demographic and professional factors associated with participants' KAP. Individuals with higher education levels, such as a master's degree or above, demonstrated superior knowledge and attitude toward IBD. Participants with vice or senior professional titles had higher knowledge scores, indicating that experience and seniority positively influence healthcare professionals' knowledge. However, nurses and nursing supervisors exhibited lower knowledge scores and were associated with negative attitudes. Participation in training on IBD and exposure to a greater number of IBD cases in the past month were both positively correlated with higher knowledge, emphasizing the importance of continuous education and clinical experience in improving knowledge levels. These findings are consistent with prior studies highlighting the positive impact of training and clinical exposure on healthcare professionals' knowledge and practice[16,17].
SEM further supported these associations, showing that knowledge positively influenced both attitude and practice, while attitude positively impacted practice. These results are in line with the theory of planned behavior, which suggests that attitude and perceived behavioral control significantly influence behavioral intentions and actions[18,19].
Most participants demonstrated substantial knowledge of key aspects of IBD, including its classification into three types: (1) AMI; (2) CMI; and (3) Ischemic colitis, with particular emphasis on the severity and high mortality associated with AMI[1]. However, certain areas of knowledge require further attention. For example, familiarity with specific diagnostic methods was limited, as evidenced by the under-recognition of magnetic resonance imaging and mesenteric artery computed tomography angiography as valuable diagnostic tools for IBD. This gap indicates a need for enhanced training and education programs that cover diverse diagnostic modalities to ensure early and accurate diagnosis. Additionally, the underutilization of contrast-enhanced ultrasound and diagnostic laparoscopy/abdominal surgery highlights the potential for improving awareness and use of these techniques in clinical practice. To address these gaps, recommendations should focus on comprehensive diagnostic training programs to enhance healthcare professionals' knowledge in these areas. Continuous medical education courses should also be organized to keep professionals updated on the latest advancements in the diagnosis and management of IBD[20,21].
The assessment of healthcare professionals' attitudes toward IBD management provided valuable insights into their perspectives on the importance of early diagnosis and the need for collaborative approaches. Most participants strongly agreed that early diagnosis is critical for the prognosis of IBD patients, emphasizing their recognition of the impact of timely intervention. Their belief in the importance of interdisciplinary teamwork for accurate diagnosis and management reflects a positive attitude toward collaboration among healthcare professionals in this context. However, while attitudes were generally positive, a subset of participants expressed neutrality or disagreement regarding certain aspects. For example, some participants showed neutral or negative attitudes toward the necessity of additional training and education on IBD, which could affect their preparedness to manage the condition effectively. To address this, recommendations should focus on ongoing education and training initiatives to strengthen positive attitudes and foster a culture of continuous learning among healthcare professionals[22,23]. Additionally, efforts should target identifying and addressing specific concerns or barriers contributing to neutral or negative attitudes, ensuring alignment among professionals in their commitment to providing optimal care for IBD patients[3,24].
The evaluation of healthcare professionals' practices related to the diagnosis and management of IBD revealed areas of strength and opportunities for improvement. While some participants frequently engaged in practices that support early diagnosis and prompt treatment—such as closely monitoring patients with suspected IBD and performing differential diagnoses for elderly patients with relevant risk factors—others reported instances of underdiagnosis and delayed diagnosis. The survey highlighted key factors considered most useful for diagnosing IBD. Cardiovascular risk factors and abdominal pain with tenderness were widely recognized as critical diagnostic indicators by healthcare professionals. However, certain diagnostic tools, such as elevated serum lactate levels and acidosis, were less frequently selected[25,26]. This suggests a need to enhance awareness and use of specific diagnostic markers that can improve the accuracy and timeliness of diagnoses. Recommendations should emphasize integrating these diagnostic markers into clinical practice guidelines and continuous education programs to ensure healthcare professionals understand their importance in the diagnostic process[27-29].
Several limitations of this study should be acknowledged. First, the cross-sectional design limits the ability to establish causality. Second, the self-reported nature of the data, including responses to KAP questions, introduces the potential for response bias.
In conclusion, healthcare professionals possess sufficient knowledge but demonstrate suboptimal attitudes and inactive practices regarding IBD. To improve clinical care, it is essential to enhance healthcare professionals' attitudes and practices through targeted training and intervention programs.
| 1. | Ahmed M. Ischemic bowel disease in 2021. World J Gastroenterol. 2021;27:4746-4762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (4)] |
| 2. | Clair DG, Beach JM. Mesenteric Ischemia. N Engl J Med. 2016;374:959-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 329] [Article Influence: 36.6] [Reference Citation Analysis (1)] |
| 3. | Liao JN, Chan YH, Kuo L, Tsai CT, Lim SS, Chao TF. Risk of Ischemic Bowel Disease in Patients With Atrial Fibrillation Receiving Warfarin or Non-vitamin K Antagonist Oral Anticoagulants. Front Cardiovasc Med. 2022;9:874460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Cotter TG, Bledsoe AC, Sweetser S. Colon Ischemia: An Update for Clinicians. Mayo Clin Proc. 2016;91:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Prakash VS, Marin M, Faries PL. Acute and Chronic Ischemic Disorders of the Small Bowel. Curr Gastroenterol Rep. 2019;21:27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Yadav S, Dave M, Edakkanambeth Varayil J, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sweetser SR, Melton LJ 3rd, Sandborn WJ, Loftus EV Jr. A population-based study of incidence, risk factors, clinical spectrum, and outcomes of ischemic colitis. Clin Gastroenterol Hepatol. 2015;13:731-8.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (2)] |
| 7. | Iacobellis F, Narese D, Berritto D, Brillantino A, Di Serafino M, Guerrini S, Grassi R, Scaglione M, Mazzei MA, Romano L. Large Bowel Ischemia/Infarction: How to Recognize It and Make Differential Diagnosis? A Review. Diagnostics (Basel). 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Aerts C, Revilla M, Duval L, Paaijmans K, Chandrabose J, Cox H, Sicuri E. Understanding the role of disease knowledge and risk perception in shaping preventive behavior for selected vector-borne diseases in Guyana. PLoS Negl Trop Dis. 2020;14:e0008149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 9. | Liao L, Feng H, Jiao J, Zhao Y, Ning H. Nursing assistants' knowledge, attitudes and training needs regarding urinary incontinence in nursing homes: a mixed-methods study. BMC Geriatr. 2023;23:39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Mumena WA. Maternal Knowledge, Attitude and Practices toward Free Sugar and the Associations with Free Sugar Intake in Children. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Hess B, Cahenzli M, Forbes A, Burgos R, Coccolini F, Corcos O, Holst M, Irtun Ø, Klek S, Pironi L, Rasmussen HH, Serlie MJ, Thibault R, Gabe S, Reintam Blaser A; ESPEN Special Interest Group on Acute Intestinal Failure ESPEN (European Society for Clinical Nutrition and Metabolism). Management of acute mesenteric ischaemia: Results of a worldwide survey. Clin Nutr ESPEN. 2023;54:194-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Lee F, Suryohusodo AA. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: A cross-sectional study. Front Public Health. 2022;10:957630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 84] [Reference Citation Analysis (0)] |
| 13. | Li H, Zheng L, Le H, Zhuo L, Wu Q, Ma G, Tao H. The Mediating Role of Internalized Stigma and Shame on the Relationship between COVID-19 Related Discrimination and Mental Health Outcomes among Back-to-School Students in Wuhan. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Dhaliwal G, Mirza W, Vincent Coralde JM, Dhillon J, Patel T. Imposter Zoster: An Atypical Case of Varicella-Zoster Virus Infection. Cureus. 2023;15:e42104. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Hillel D, Schwimmer M, Barshack I, Mayer C. [Idiopathic myointimal hyperplasia of the mesenteric veins: a case report]. Harefuah. 2023;162:681-683. [PubMed] |
| 16. | Le Gall G, Kirchgesner J, Bejaoui M, Landman C, Nion-Larmurier I, Bourrier A, Sokol H, Seksik P, Beaugerie L. Clinical activity is an independent risk factor of ischemic heart and cerebrovascular arterial disease in patients with inflammatory bowel disease. PLoS One. 2018;13:e0201991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Orihashi K. Multimodality Diagnosis of Mesenteric Ischemia. J Vis Exp. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Chen H, Wu Q, Fang H, Liang B, Fang L. Intestinal necrosis cannot be neglected in a patient with hepatic portal vein gas combined with appendicitis: a rare case report and literature review. BMC Surg. 2019;19:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Tervonen T, Vora P, Seo J, Krucien N, Marsh K, De Caterina R, Wissinger U, Soriano Gabarró M. Patient Preferences of Low-Dose Aspirin for Cardiovascular Disease and Colorectal Cancer Prevention in Italy: A Latent Class Analysis. Patient. 2021;14:661-672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Okano S, Yao T, Nomura O, Nagahara A, Hagiwara T, Sugimoto K, Takahashi M, Sakamoto K. Enterocolic Lymphocytic Phlebitis Treated Preoperatively with Biologics and Immunosuppressive Agents. Case Rep Pathol. 2022;2022:5120607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Yu SJ, Heo JH, Choi EJ, Kim JH, Lee HS, Kim SY, Lim JH. Role of multidetector computed tomography in patients with acute infectious colitis. World J Clin Cases. 2022;10:3686-3697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (2)] |
| 22. | Bawa D, Khalifa YM, Khan S, Norah W, Noman N. Surgical outcomes and prognostic factors associated with emergency left colonic surgery. Ann Saudi Med. 2023;43:97-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 23. | Fisher A, Halalau A. A Case Report and Literature Review of Clostridium difficile Negative Antibiotic Associated Hemorrhagic Colitis Caused by Klebsiella oxytoca. Case Rep Gastrointest Med. 2018;2018:7264613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Sunakawa T, Ito N, Moriyasu R, Seki N, Takeuchi D, Sasahara K. Smooth muscle degeneration of the mesenteric and branching veins causing ischemic enteritis: a case report. Surg Case Rep. 2022;8:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Ambe PC, Kang K, Papadakis M, Zirngibl H. Can the Preoperative Serum Lactate Level Predict the Extent of Bowel Ischemia in Patients Presenting to the Emergency Department with Acute Mesenteric Ischemia? Biomed Res Int. 2017;2017:8038796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Mothes H, Wickel J, Sponholz C, Lehmann T, Kaluza M, Zanow J, Doenst T. Monitoring of the Progression of the Perioperative Serum Lactate Concentration Improves the Accuracy of the Prediction of Acute Mesenteric Ischemia Development After Cardiovascular Surgery. J Cardiothorac Vasc Anesth. 2021;35:1792-1799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Li H, Sun D, Sun D, Xiao Z, Zhuang J, Yuan C. The Diagnostic Value of Coagulation Indicators and Inflammatory Markers in Distinguishing Between Strangulated and Simple Intestinal Obstruction. Surg Laparosc Endosc Percutan Tech. 2021;31:750-755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Rizwan R, Feuerstadt P. Bad blood: ischemic conditions of the large bowel. Curr Opin Gastroenterol. 2022;38:72-79. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Sinha D, Kale S, Kundaragi NG, Sharma S. Mesenteric ischemia: a radiologic perspective. Abdom Radiol (NY). 2022;47:1514-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |