Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.103266
Revised: December 8, 2024
Accepted: December 20, 2024
Published online: February 27, 2025
Processing time: 70 Days and 1.6 Hours
Gastric cancer is the most common malignancy of the digestive system and surgical resection is the primary treatment. Advances in surgical technology have reduced the risk of complications after radical gastrectomy; however, post-sur
To determine the predictive value of CRP, PCT, and TBil levels for pancreatic fistula after gastric cancer surgery.
In total, 158 patients who underwent radical gastrectomy for gastric cancer at our hospital between January 2019 and January 2023 were included. The patients were assigned to a pancreatic fistula group or a non-pancreatic fistula group. Multiva
On day 1 post-surgery, the CRP, PCT, and TBil levels were significantly higher in the pancreatic fistula group than in the non-pancreatic fistula group (P < 0.05). A higher fistula grade was associated with higher levels of the indices. Univariate analysis revealed significant differences in the presence of diabetes, hyperlipidemia, pancreatic injury, splenectomy, and the biomarker levels (P < 0.05). Logistic multivariate analysis identified diabetes, hyperlipidemia, pancreatic injury, CRP level, and PCT level as independent risk factors. ROC curves yielded predictive values for CRP, PCT, and TBil levels, with the PCT level having the highest area under the curve (AUC) of 0.80 [95% confidence interval (CI): 0.72-0.90]. Combined indicators improved the predictive value, with an AUC of 0.86 (95%CI: 0.78-0.93).
Elevated CRP, PCT, and TBil levels predict risk of pancreatic fistula post-gastrectomy for gastric cancer.
Core Tip: This study found that the serum C-reactive protein (CRP), procalcitonin (PCT), and total bilirubin (TBil) levels on day 1 post-surgery had a significant predictive value for pancreatic fistula post-radical gastrectomy; therefore, elevated serum CRP, PCT, and TBil levels in the early post-operative period could be used to indicate the presence of pancreatic fistula.
- Citation: Yuan JL, Wen X, Xiong P, Pei L. Predictive value of C-reactive protein, procalcitonin, and total bilirubin levels for pancreatic fistula after gastrectomy for gastric cancer. World J Gastrointest Surg 2025; 17(2): 103266
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/103266.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.103266
Gastric cancer is a malignant tumor with the highest incidence rate in the digestive system. Surgical resection is the primary treatment for gastric cancer. With continuous improvements in surgical technology, the risk of complications post-radical gastrectomy has decreased. However, the risk of post-surgical pancreatic fistula, one of the most serious complications post-surgery, has not been eliminated[1,2]. Pancreatic fistula not only cause complications, such as abdo
This study included 158 patients who underwent radical gastrectomy for gastric cancer at our hospital between January 2019 and January 2023. The cohort comprised 88 males and 70 females, with ages ranging from 36 years to 88 years and a mean ± SD age of 63.66 ± 15.14 years. The post-operative histopathological staging distribution was: 13 patients with stage I, 50 with stage II, 66 with stage III, and 29 with stage IV; 22 underwent proximal gastric cancer resection, 93 underwent distal gastric cancer radical resection, and 43 underwent radical total gastrectomy. Post-operative histo
Inclusion criteria: (1) Diagnosed with gastric cancer based on clinical symptoms, imaging findings, and histopathological examination; and (2) Underwent radical gastrectomy.
Exclusion criteria: (1) Severe liver, heart, or kidney disease; (2) Cognitive impairment; (3) Poor compliance; and (4) Missing clinical data. The study was approved by the Ethics Committee of Western Theater Command Air Force Hospital (Chengdu, Sichuan Province, China). Informed consent was obtained from all patients.
The diagnosis of post-surgical pancreatic fistula was based on the relevant standards established by the International Study Group of Pancreatic Fistula[7]: Three days or more post-surgery, the amylase level in the drainage fluid of the percutaneous drainage tube was three times higher than the normal serum level (135 U/L). For patients who did not have a drainage tube inserted during surgery or those who had the tube removed within three days post-surgery, the presence of elevated body temperature (> 38 °C), elevated white blood cell count, peritonitis, and B-mode ultrasound findings of peri-pancreatic effusion were used to confirm the diagnosis. Post-surgical pancreatic fistulas were divided into three grades: (1) Grade A, postoperative drainage for three weeks, no infection, no special treatment required, and delayed extubation was sufficient; (2) Grade B, drainage for more than three weeks or infection, requiring adjustment of strategies, which may include dietary control, nutrition, antibiotics, and drainage tube adjustment; and (3) Grade C, surgical or interventional treatment required, and serious events may occur, requiring aggressive intervention, such as fasting, nutritional support, antibiotics, somatostatin, and possibly computed tomography/ultrasound-guided drainage, which may prolong hospitalization.
PCT, CRP, and TBil were used to predict post-operative abdominal infection and anastomotic fistula. Within 24 hours of surgery, peripheral venous blood was collected from patients who underwent radical gastrectomy for gastric cancer. Serum was separated at 3000 rpm, and the serum PCT, CRP and TBil levels were measured using chemiluminescence[8], immunoturbidimetry[9], and the vanadate oxidation method, respectively[10]. The reagent kits were purchased from Shanghai Jining Biotechnology Co., Ltd. and operated strictly in accordance with their relevant standards.
Based on clinical experience and relevant studies[11-13], factors that may affect the development of pancreatic fistulas after radical gastrectomy for gastric cancer were included. They included pre-operative complications (diabetes, hypertension, and hyperlipidemia), serum nutritional indicators (hemoglobin and albumin), surgical factors (including operation time, intra-operative blood loss, intra-operative pancreatic injury, retro-pancreatic lymph node dissection, and combined splenectomy), repeat abdominal surgery, histopathological factors (including tumor size, histopathological type, and histopathological stage), post-operative related factors (including the day 1 post-surgery serum amylase level in the drainage fluid and the day 1 post-surgery serum CRP, PCT and TBil levels). Univariate and multivariate logistic regression analyses were performed to identify the independent risk factors affecting the development of pancreatic fistulas following radical gastrectomy for gastric cancer. Among them, a hemoglobin level ≥ 110 g/L was considered to be normal, and an albumin level ≥ 35 g/L was considered to be normal.
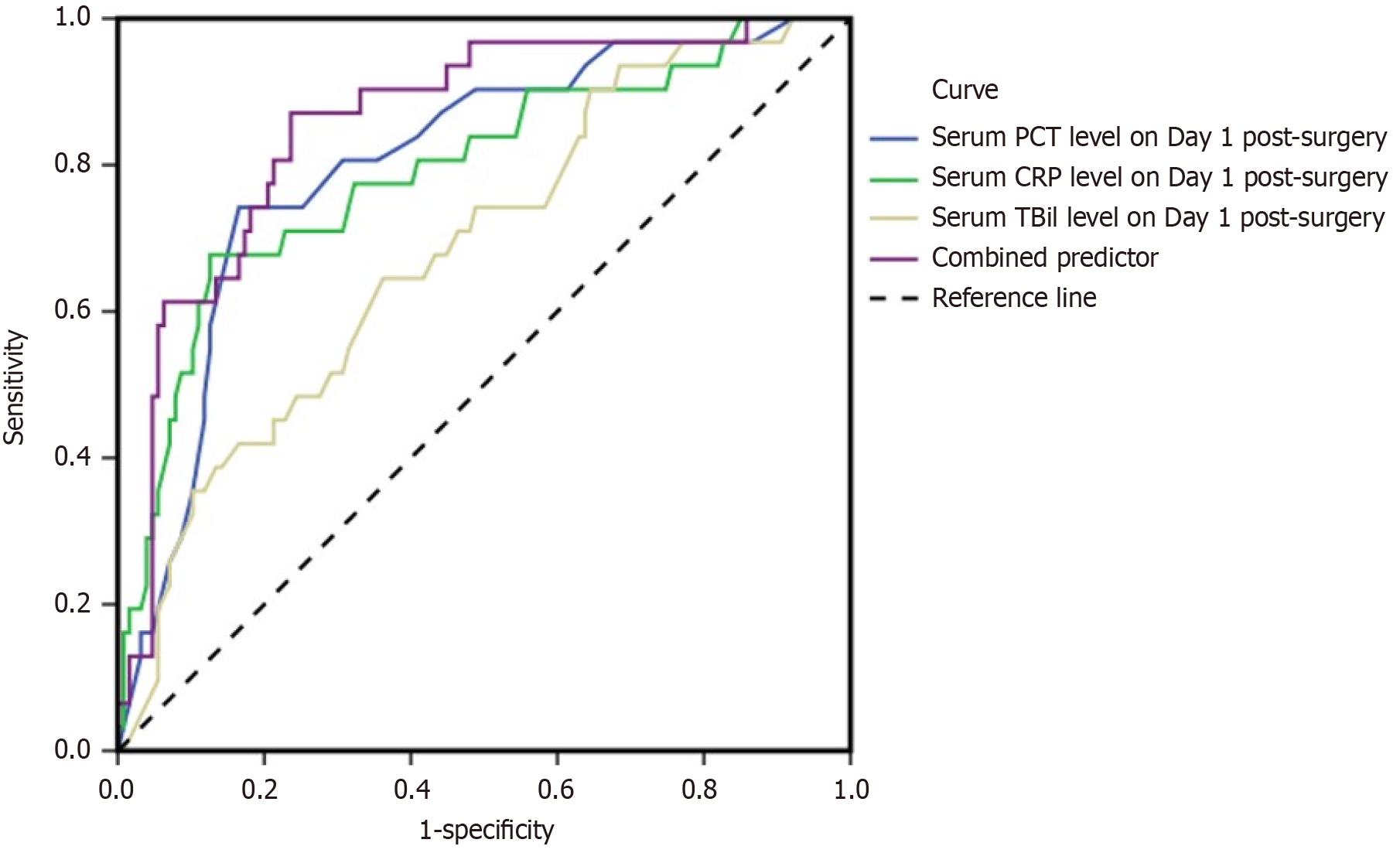
Receiver operating characteristic (ROC) curves were used to determine the predictive value of serum CRP, PCT, and TBil levels, as individual indices or combined, on day 1 post-surgery for the development of pancreatic fistula post-radical gastrectomy for gastric cancer.
The data were analyzed using statistical product and service solutions 19.0 statistical software. Measurement data are presented as mean ± SD and t-tests were used for comparisons of two groups or a one-way analysis of variance for multiple groups, with a subsequent least significant difference-t test for pairwise comparisons, if obvious differences were identified. Comparisons between the two groups were performed using the χ2 test or continuity correction test. Variables that were statistically significant in the univariate analysis were further analyzed using multivariate logistic regression, and binary logistic regression was used to calculate the predictive value of the combined indices for post-surgical pan
Comparisons of the serum CRP, PCT, and TBil levels between the two groups on day 1 post-surgery are summarized in Table 1. On day 1 post-surgery, the serum CRP, PCT, and TBil levels were significantly higher in the pancreatic fistula group compared to those in the non-pancreatic fistula group (P < 0.05).
| Groups | n | PCT (μg/mL) | CRP (mg/L) | TBil (μmol/L) |
| Non-pancreatic fistula group | 127 | 0.71 ± 0.11 | 106.69 ± 20.46 | 17.69 ± 4.13 |
| Pancreatic fistula group | 31 | 0.99 ± 0.33 | 173.14 ± 32.45 | 20.83 ± 4.18 |
| t value | 8.020 | 14.266 | 3.786 | |
| P value | 0.000 | 0.000 | 0.000 |
Comparison of the serum CRP, PCT, and TBil levels on day 1 post-surgery in patients with different grades of pancreatic fistulas are summarized in Table 2. A higher grade of pancreatic fistula was associated with higher serum CRP, PCT, and TBil levels on day 1 post-surgery with significant differences between the two groups (P < 0.05).
The univariate analysis of factors affecting the development of pancreatic fistula after radical gastrectomy for gastric cancer is summarized in Table 3.
| Factors | Groups | Pancreatic fistula group (n = 31) | Non-pancreatic fistula group (n = 127) | t/χ2 value | P value |
| Age (years) | ≥ 60 | 20 | 71 | 0.756 | 0.384 |
| < 60 | 11 | 56 | |||
| Sex | Male | 18 | 70 | 0.088 | 0.767 |
| Female | 13 | 57 | |||
| Diabetes | Yes | 16 | 30 | 9.460 | 0.002 |
| No | 15 | 97 | |||
| Hypertension | Yes | 6 | 21 | 0.140 | 0.708 |
| No | 25 | 106 | |||
| Hyperlipidemia | Yes | 13 | 16 | 14.311 | 0.000 |
| No | 18 | 111 | |||
| Hemoglobin (g/L) | Normal | 29 | 117 | 0.012 | 0.912 |
| Descend | 2 | 10 | |||
| Albumin (g/L) | Normal | 29 | 121 | 0.004 | 0.949 |
| Descend | 2 | 6 | |||
| History of abdominal surgery | Yes | 3 | 7 | 0.196 | 0.658 |
| No | 28 | 120 | |||
| Operative time (hour) | ≤ 3 | 19 | 84 | 0.258 | 0.611 |
| > 3 | 12 | 43 | |||
| Intraoperative pancreatic injury | Yes | 14 | 16 | 17.177 | 0.000 |
| No | 17 | 111 | |||
| Combined splenectomy | Yes | 4 | 2 | 4.785 | 0.029 |
| No | 27 | 125 | |||
| Combined splenectomy and partial pancreatectomy | Yes | 2 | 2 | 0.832 | 0.362 |
| No | 29 | 125 | |||
| Retro-pancreatic lymph node dissection | Yes | 19 | 60 | 1.967 | 0.161 |
| No | 12 | 67 | |||
| Scope of gastric resection | Proximal stomach | 4 | 18 | 0.080 | 0.961 |
| Distal stomach | 18 | 75 | |||
| Whole stomach | 9 | 34 | |||
| Post-operative pathological staging | I-II | 12 | 51 | 0.022 | 0.883 |
| III-IV | 19 | 76 | |||
| Serum PCT level on day 1 post-surgery (g/mL) | 0.99 ± 0.33 | 0.71 ± 0.11 | 8.020 | 0.000 | |
| Serum CRP level on day 1 post-surgery (mg/L) | 173.14 ± 32.45 | 106.69 ± 20.46 | 14.266 | 0.000 | |
| Serum TBil level on day 1 post-surgery (μmol/L) | 20.83 ± 4.18 | 17.69 ± 4.13 | 3.786 | 0.000 |
The results of the univariate analysis show differences in the presence of diabetes, hyperlipidemia, postoperative pancreatic injury, and combined splenectomy, and the serum CRP, PCT, and TBil levels on day 1 post-surgery between the two groups (P < 0.05).
The multivariate analysis of the factors affecting the development of pancreatic fistula after radical gastrectomy for gastric cancer is summarized in Table 4.
| Factors | β | SE | Wald χ2 value | OR | P value | 95%CI |
| Diabetes | 1.336 | 0.453 | 8.698 | 3.804 | 0.003 | 1.565-9.243 |
| Hyperlipidemia | 1.016 | 0.337 | 9.089 | 2.762 | 0.003 | 1.427-5.347 |
| Intraoperative pancreatic injury | 1.559 | 0.336 | 18.144 | 21.528 | 0.000 | 2.461-9.185 |
| Serum PCT level on day 1 post-surgery | 0.841 | 0.216 | 15.159 | 2.319 | 0.000 | 1.518-3.541 |
| Serum CRP level on day 1 post-surgery | 0.461 | 0.049 | 88.514 | 1.586 | 0.000 | 1.440-1.745 |
The logistic multivariate analysis shows that the presence of diabetes, hyperlipidemia, and pancreatic injury during surgery, and the serum CRP and PCT levels on day 1 post-surgery were independent risk factors for pancreatic fistula after radical gastrectomy.
The predictive values of the serum CRP, PCT, and TBil levels for post-surgical pancreatic fistula on day 1 post-surgery are summarized in Table 5 and Figure 1.
| Indicators | Critical value | AUC | 95%CI | P value | Sensitivity | Specificity |
| Serum PCT level on day 1 post-surgery | 0.84 | 0.803 | 0.718-0.889 | 0.000 | 74.2 | 83.5 |
| Serum CRP level on day 1 post-surgery | 133.83 | 0.792 | 0.697-0.887 | 0.000 | 67.7 | 87.3 |
| Serum TBil level on day 1 post-surgery | 20.16 | 0.683 | 0.581-0.785 | 0.002 | 64.5 | 63.8 |
| Combination of the three indices | 0.857 | 0.784-0.929 | 0.000 | 87.1 | 76.4 |
ROC curve analysis showed that the serum PCT, CRP, and TBil levels on day 1 post-surgery predict post-operative pancreatic fistula. The area under the curve (AUC) of the PCT, CRP, TBil levels, and their combination for predicting post-operative pancreatic fistula were 0.80, 0.79, 0.68, and 0.86, respectively. The 95% confidence intervals were (0.72-0.89), (0.70-0.89), (0.58-0.79) and (0.78-0.93), respectively. The sensitivities and specificities for PCT, CRP, TBil, and the three combined indices were 74.2%, 67.7%, 64.5%, 87.1%, respectively, and 83.5%, 87.3%, 63.8%, 76.4%, respectively. The AUC and sensitivities of the three combined indices were higher than those of each individual index.
Pancreatic fistula refers to the phenomenon of rupture of the pancreatic duct and the outflow of pancreatic juice through non-physiological pathways. This is a common complication of radical gastrectomy for gastric cancer. It has been reported that the incidence of pancreatic fistula development post-radical gastrectomy for gastric cancer is between 10% and 20%[14]. Once a pancreatic fistula occurs, it increases the incidence of hemorrhage, infection, and treatment costs and may also cause death if not diagnosed and treated in a timely manner[15,16]. The symptoms and imaging manifestations of post-surgical pancreatic fistula and abdominal infection are similar and easily misdiagnosed. In addition, the diagnosis of pancreatic fistula is mainly based on the amylase level in the drainage fluid of the percutaneous drainage tube. However, this diagnosis is not applicable to patients who do not have a drainage tube placed during surgery. The combination of elevated body temperature (> 38 °C), abnormal white blood cell count, peritonitis, and ultrasound examination data can delay the diagnosis of pancreatic fistula, thus impeding timely intervention.
Serum CRP is a sensitive inflammatory marker that participates in various pathophysiological processes. It is a relatively stable and common acute-phase response protein used in clinical practice[17]. The PCT level is a common indicator of bacterial and fungal infections[18]. Studies have reported that an elevated serum PCT level on day 2 and day 5 post-pancreaticoduodenectomy have better positive and negative predictive values for diagnosing post-surgical pancreatic fistula, and in combination with the CRP level has a better predictive value for post-surgical pancreatic fistula[19,20]. The present study has demonstrated that patients who underwent radical gastrectomy for gastric cancer and developed pancreatic fistula post-surgery had significantly higher serum CRP and PCT levels on day 1 post-surgery than those who did not develop pancreatic fistula. In addition, a higher grade pancreatic fistula is associated with higher serum CRP and PCT levels on day 1 post-surgery. This suggests that the serum CRP and PCT levels on day one post-surgery are of great significance in reflecting the risk and severity of pancreatic fistula post-surgery. This is important because pancreatic fistula is a serious post-operative complication that can lead to electrolyte imbalance, infection, hemorrhage, organ failure, and other complications. The leakage of pancreatic juice into the abdominal cavity triggers widespread inflammation, prompting the release of inflammatory factors such as PCT and CRP; PCT is a sensitive indicator of inflammation, which increases during surgery and infection, and further increases when a pancreatic fistula is present due to abdominal inflammation; CRP is an acute reactive protein that rises rapidly during infection and inflammation, and also significantly increases in patients with pancreatic fistula. The higher the grade of pancreatic fistula, the more severe the inflammation in the abdominal cavity, with associated higher PCT and CRP levels. Relevant studies have also found that the PCT and CRP levels in patients with pancreatic fistula are higher than those in patients without pancreatic fistula[21,22].
TBil is a breakdown product of hemoglobin and an antioxidant produced autonomously in humans. An excessively high TBil level indicates abnormal bile metabolism, leading to increased pressure in the biliary system, causing biliary inflammation and further spreading to the pancreas, which is prone to pancreatic fistula[23]. In this study, the serum TBil level in 31 patients who developed pancreatic fistula post-surgery was significantly higher than for those in the non-pancreatic fistula group on day 1 post-surgery. As the pancreatic fistula grade increased, the serum TBil level on day 1 post-surgery was elevated, indicating that the serum TBil level on day 1 post-surgery is valuable for predicting post-surgical pancreatic fistula and the severity of the pancreatic fistula. This may be because a high TBil level may also affect the microcirculation of the pancreas, damage the microvasculature of the pancreas, leading to ischemia and hypoxia of the pancreatic tissue, which in turn can cause pancreatitis or pancreatic fistula. Also, microcirculation disorders may also affect the ability of the pancreas to repair and regenerate, making it more difficult for the pancreas to recover after damage, thereby increasing the risk of pancreatic fistula. Li et al[24] also reported that a high TBil level is a risk factor for pancreatic fistula.
In addition, this study screened 18 factors related to the occurrence of pancreatic fistula post-surgery and conducted a single-factor analysis, which revealed that the presence of diabetes, hyperlipidemia, post-operative pancreatic injury, and combined splenectomy, and the serum CRP, PCT, and TBil levels on day 1 post-surgery differed. Multivariate analysis confirmed that the presence of diabetes, hyperlipidemia, and intraoperative pancreatic injury, and the serum CRP and PCT levels on day 1 post-surgery were independent risk factors for pancreatic fistula after radical gastrectomy. The ROC curve analysis showed that the serum CRP, PCT, and TBil levels, individually, on day 1 post-radical gastrectomy for gastric cancer, had predictive value for post-operative pancreatic fistula, but the combination of the three indices had a higher predictive value.
This study had limitations as it was conducted at a single-center with a small sample size and a limited research design. The serum indices were not measured at multiple time points, such as pre-operatively, intra-operatively, or post-operatively.
In summary, the serum CRP, PCT, and TBil levels on day 1 post-surgery have predictive value for the development of pancreatic fistula following radical gastrectomy for gastric cancer, thus elevated serum levels of these indices in the early post-operative period can serve to predict the risk of pancreatic fistula.
| 1. | Kubo N, Sakurai K, Hasegawa T, Tamamori Y, Iseki Y, Nishii T, Shimizu S, Inue T, Nishiguchi Y, Maeda K. Impact of a robotic system on intra-abdominal infectious complications after minimally invasive gastrectomy in patients with gastric cancer: A propensity score matching analysis regarding visceral obesity. Ann Gastroenterol Surg. 2024;8:221-233. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Ishida R, Komatsu S, Takashima Y, Nishibeppu K, Ohashi T, Kosuga T, Konishi H, Shiozaki A, Kubota T, Fujiwara H, Otsuji E. Pancreatic fistula as a pivotal prognostic factor among postoperative complications in gastric cancer. Am J Cancer Res. 2023;13:6063-6071. [PubMed] |
| 3. | Zhou M, Zhong G, Sun H, Zhu Q, Wang Z. Risk factors for postoperative pancreatic fistula (POPF) in gastric cancer patients: A systematic review and meta-analysis. Eur J Surg Oncol. 2023;49:107092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Reference Citation Analysis (0)] |
| 4. | Vauclair E, Moreno-Lopez N, Orry D, Fournel I, Rat P, Ortega-Deballon P, Facy O. Inflammatory markers for the early detection of post-operative infection: The same threshold for rectal and colic surgery? J Visc Surg. 2021;158:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Song G, Guo H, Jiang C, Shi Y, Liu M. Magnetic Nanoparticles Detection of C-Reactive Protein Combined with Neutrophil to Lymphocyte Ratio to Predict the Occurrence of Anastomotic Fistula after Rectal Cancer Surgery. Cell Mol Biol (Noisy-le-grand). 2022;68:116-122. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Xu SB, Jia CK, Liu L, Zhu HZ. The net parenchymal thickness predicts pancreatic fistula after pancreaticoduodenectomy: a retrospective cohort study of objective data. ANZ J Surg. 2022;92:1097-1104. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Shi S, Xiang JF, Xu J, Yu XJ. [Introduction and analysis of the updated definition and grading system of postoperative pancreatic fistula by the international pancreatic surgery research group in 2016]. Zhongguo Shiyong Waike Zazhi. 2017;37:149-152. [DOI] [Full Text] |
| 8. | Wang ZQ, Rong YW, Chen Y. [The Diagnostic Value of PCT, CRP and WBC Levels in Respiratory Infec-tions in Children]. Xitong Yixue. 2024;9:38-40. [DOI] [Full Text] |
| 9. | Ming T, Hu JJ, Zha F. [The value analysis of combined detection of serum CRP, IL-6, IL-10 in the diagnosis of anastomotic fistula after laparoscopic colorectal cancer surgery]. Zhongguo Shiyong Yiyao. 2023;18:12-16. [DOI] [Full Text] |
| 10. | Zhang Q, Yuan J, Xu XY, Fan JW, Wu FG. [Relationship between serum TBIL,Hcy,hs-CRP,UA and unstable coronary plaque formation in elderly patients with coronary heart disease]. Shiyong Laonian Yixue. 2022;36:77-80. [DOI] [Full Text] |
| 11. | Al-Magedi AAS, Wu R, Tao Q. Comparison of postoperative pancreatic fistula between open and laparoscopic surgery in patients with gastric cancer: A meta-analysis. Ann Med Surg (Lond). 2022;76:103558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 12. | Zhu Y, Wu D, Yang H, Lu Z, Wang Z, Zu G, Li Z, Xu X, Zhang Y, Chen X, Chen W. Analysis of factors influencing pancreatic fistula after minimally invasive pancreaticoduodenectomy and establishment of a new prediction model for clinically relevant pancreatic fistula. Surg Endosc. 2024;38:2622-2631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Hayashi K, Inaki N, Sakimura Y, Yamaguchi T, Obatake Y, Terai S, Kitamura H, Kadoya S, Bando H. Pancreatic thickness as a predictor of postoperative pancreatic fistula after laparoscopic or robotic gastrectomy. Surg Endosc. 2023;37:5358-5367. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Wang YL, Yan Y, Dong SL. [Research progress on pancreatic CT anatomic features and prediction of postoperative pancreatic fistula in patients with gastric cancer]. Zhonghua Jiepou Yu Linchuang Zazhi. 2022;12:877-880. [DOI] [Full Text] |
| 15. | Turner KM, Delman AM, Lim SA, Marasligiller S, Ammann AM, Vaysburg DM, Wallen TE, Ahmad SA, Wilson GC, Patel SH. Contemporary Outcomes of Grade-C Postoperative Pancreatic Fistula in a Nationwide Database. J Surg Res. 2024;296:302-309. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Wu J, Tang Z, Zhao G, Zang L, Li Z, Zang W, Li Z, Qu J, Yan S, Zheng C, Ji G, Zhu L, Zhao Y, Zhang J, Huang H, Hao Y, Fan L, Xu H, Li Y, Yang L, Song W, Zhu J, Zhang W, Li M, Qin X, Liu F. Incidence and risk factors for postoperative pancreatic fistula in 2089 patients treated by radical gastrectomy: A prospective multicenter cohort study in China. Int J Surg. 2022;98:106219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Heard JC, Smith GH, Tolman A, Karumuri JS, Osman HG, Jeyarajah RD. No Drain, No Problem: Serum-Based Marker Prediction of Clinically Relevant Postoperative Pancreatic Fistula. Am Surg. 2024;90:1074-1081. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Kaya F, Alsafdi T. Elevated Procalcitonin Levels can Occur in Bacterial Infections and also in Medullary Thyroid Carcinoma. Eur J Case Rep Intern Med. 2024;11:004679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 19. | Al Hussan M, Qiao S, Abuheit EMI, Abdun MA, Al Mahamid M, Guo H, Zheng F, Nobah AMAM. The Role of C-reactive Protein and Procalcitonin in Predicting the Occurrence of Pancreatic Fistula in Patients who Underwent Laparoscopic Pancreaticoduodenectomy: a Retrospective Study. Zentralbl Chir. 2023;148:508-515. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Coppola A, La Vaccara V, Angeletti S, Spoto S, Farolfi T, Cammarata R, Maltese G, Coppola R, Caputo D. Postoperative procalcitonin is a biomarker for excluding the onset of clinically relevant pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Oncol. 2023;14:1077-1086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Liu HY, Zhou Y, Zhou LL, Liu J, Wang L, Shao Z. [Study on the risk factors of pancreatic fistula after pancreaticoduodenectomy and the value of serum procalcitonin in early prediction]. Xiandai Shengwuyixue Jinzhan. 2019;21:3862-3866. [DOI] [Full Text] |
| 22. | Tian Q, Feng Y, Liu SJ, Liu HM, Liu K, Hu XL. [Analysis of the accuracy of abdominal amylase, C-reactive protein and procalcitonin in predicting the occurrence of clinically relevant pancreatic fistula after gastric cancer surgery]. Guoji Waikexue Zazhi. 2002;49:333-337. [DOI] [Full Text] |
| 23. | Chu W, Ding LL, Jin HL. [Analysis of risk factors related to clinical pancreatic fistula after pancreaticoduodenectomy]. Hainan Yixue. 2019;34:1569-1572. [DOI] [Full Text] |
| 24. | Li HX, Dong AH. [Analysis of risk factors for pancreatic fistula after laparoscopic pancreaticoduodenectomy in elderly patients]. Laonian Yixue Yu Baojian. 2022;28:488-492. [DOI] [Full Text] |