Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.100244
Revised: November 11, 2024
Accepted: December 18, 2024
Published online: February 27, 2025
Processing time: 164 Days and 5.6 Hours
Gastric cancer is the fifth most common cancer and the fourth leading cause of death worldwide. Most cases of newly diagnosed gastric cancer involve not only locally advanced tumor growth and regional lymph node metastases but also distant metastases. We report a rare case finding of a mass in the right inguinal area which is derived from gastric cancer.
A 68-year-old male initially diagnosed with an inguinal hernia presented with a 2 cm mass in the right inguinal area. Gastrointestinal symptoms led to the discovery of a stomach tumor. Biopsy confirmed gastrointestinal adenocarcinoma. The diagnosis was advanced gastric cancer with peritoneal dissemination, and the inguinal mass was due to direct infiltration. Due to gastrointestinal bleeding, the patient underwent palliative gastrectomy and lymph node dissection. Postoperatively, the patient received hyperthermic intraperitoneal chemotherapy and localized radiation therapy.
This case indicates that a systematic evaluation should be conducted during the initial consultation to explore the potential connection between unrecognized distant masses and the primary tumor.
Core Tip: This case highlights the importance of thorough evaluation in patients presenting with unusual masses, such as an inguinal mass, to identify potential distant metastases from primary gastric cancer. Early diagnosis and multidisciplinary treatment, including palliative surgery, hyperthermic intraperitoneal chemotherapy, and radiation, can improve patient management in advanced gastric cancer.
- Citation: Hao JQ, Hu SY, Zhuang ZX, Zhang YJ, Zhang JW, He FJ, Zhuang W, Wang MJ. Distant metastasis in the right inguinal area from gastric cancer: A case report. World J Gastrointest Surg 2025; 17(2): 100244
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/100244.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.100244
Gastric cancer (GC) is the fifth most common cancer and the fourth leading cause of death worldwide[1]. Most cases of newly diagnosed gastric cancer involve not only locally advanced tumor growth and regional lymph node metastases but also distant metastases. The most common distant metastases of gastric cancer include the liver, peritoneum, lung, and bone[2]. Approximately 27% of gastric cancer patients have synchronous peritoneal metastases (PM) at initial diagnosis[3]. Peritoneal implantation metastases commonly occur in the omentum, pelvis, mesentery, diaphragm, and the small intestine and its mesentery, due to the structural and vascular characteristics of these areas that facilitate the deposition and proliferation of cancer cells.
We present a case of a patient who sought medical attention due to the discovery of a mass in the right inguinal area. Further gastroscopy and biopsy confirmed gastric cancer with concurrent gastric retention. During hospitalization, the right inguinal mass underwent a puncture biopsy. Subsequently, the patient experienced upper gastrointestinal bleeding, and conservative medical treatment and endoscopic assessment were ineffective, leading to emergency surgical intervention. Postoperatively, the biopsy of the puncture revealed that the inguinal mass originated from metastatic gastrointestinal adenocarcinoma.
A 68-year-old male patient presented with a solid mass in the right inguinal area and dull pain in the right scrotum, persisting for the past two months.
The patient had previously been diagnosed with an inguinal hernia at a local hospital. During treatment there, he experienced symptoms including nausea, vomiting, and loss of appetite, leading to a weight loss of approximately 15 kg. He was subsequently referred to our hospital for further evaluation and management.
The patient had a free previous medical history.
The patient had no significant personal or family medical history.
Upon admission, the patient's vital signs were stable. Physical examination revealed a hard, fixed mass measuring approximately 2.5 cm × 2.0 cm × 1.5 cm in the right inguinal region, with ill-defined borders and significant tenderness upon palpation. No signs of skin ulceration or itching were observed.
Elevated serum tumor markers were noted, with carcinoembryonic antigen levels at 18.70 ng/mL and carbohydrate antigen 19-9 levels at 578.5 U/mL.
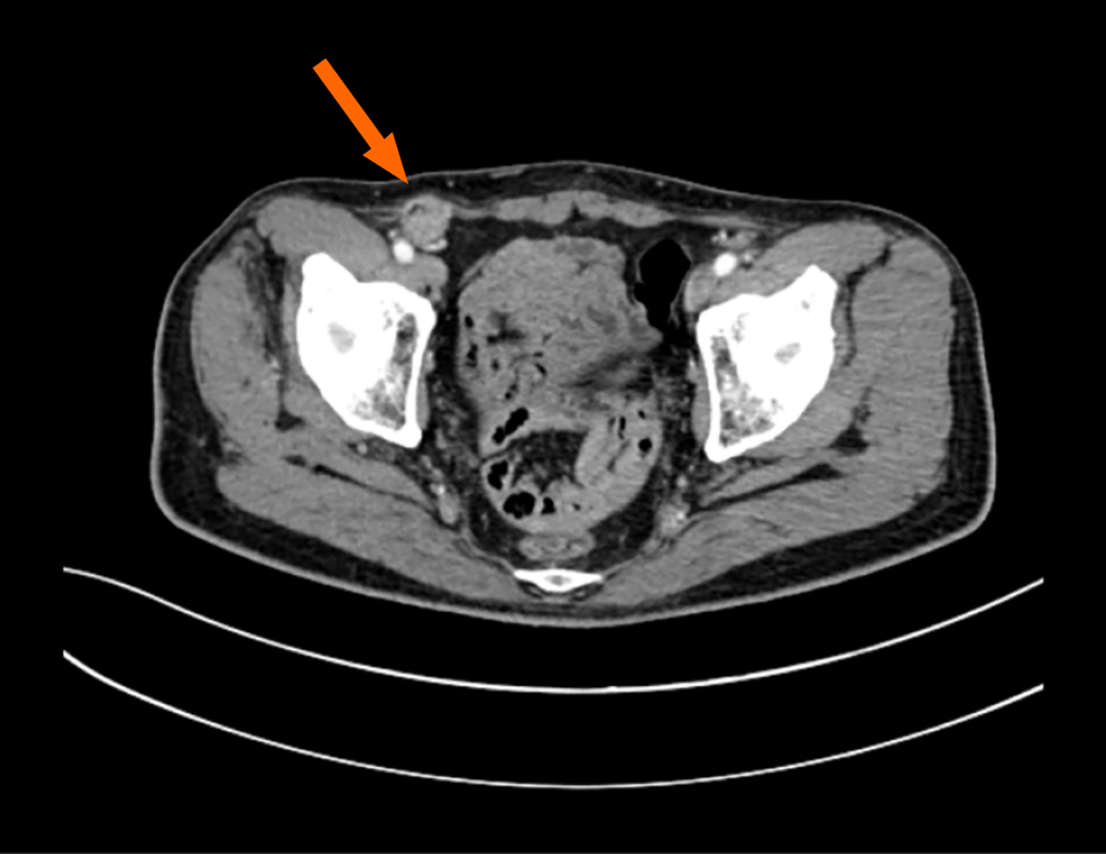
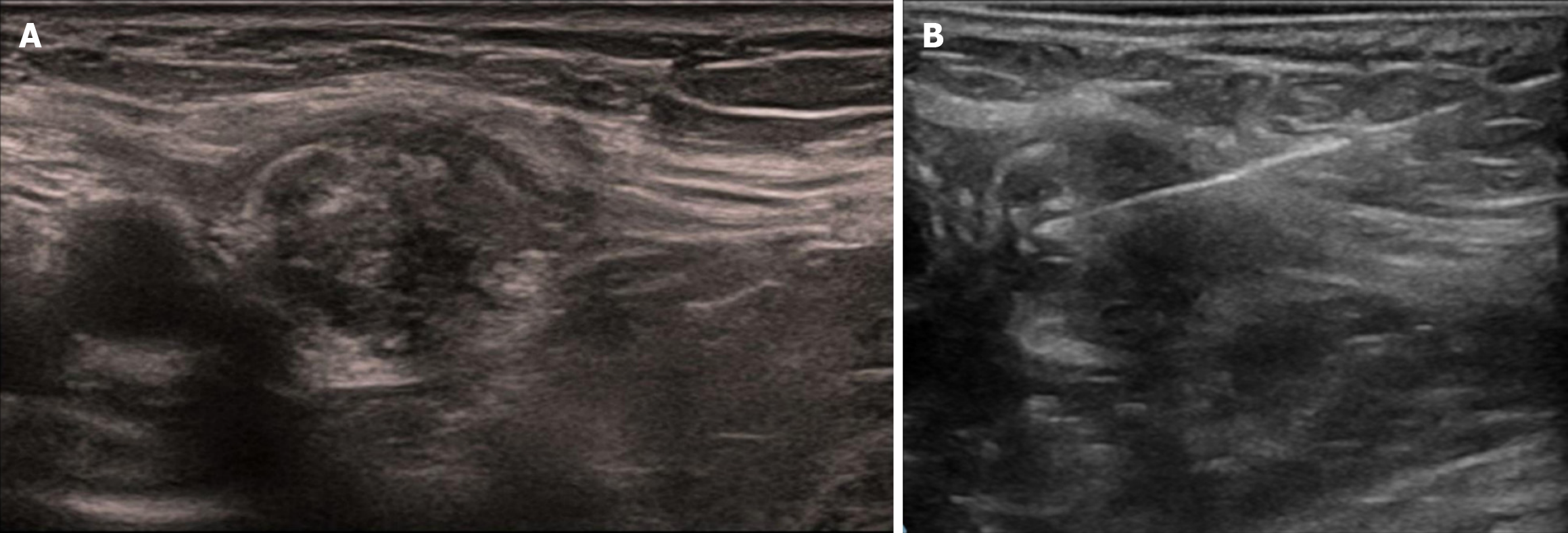
Upper gastrointestinal endoscopy indicated gastric retention and a large ulcerative lesion in the antrum. Computed tomography (CT) imaging showed a thickening of the lesser curvature of the gastric antrum wall. Additionally, a soft tissue shadow was detected in the right inguinal area (Figure 1). Color doppler ultrasound of the right inguinal mass showed a heterogeneous echo pattern measuring approximately 22 mm × 13 mm × 26 mm, with ill-defined borders and irregular shape, and blood flow signals were detected within the mass (Figure 2A). A fine needle aspiration biopsy was performed under the guidance of color Doppler ultrasound (Figure 2B).
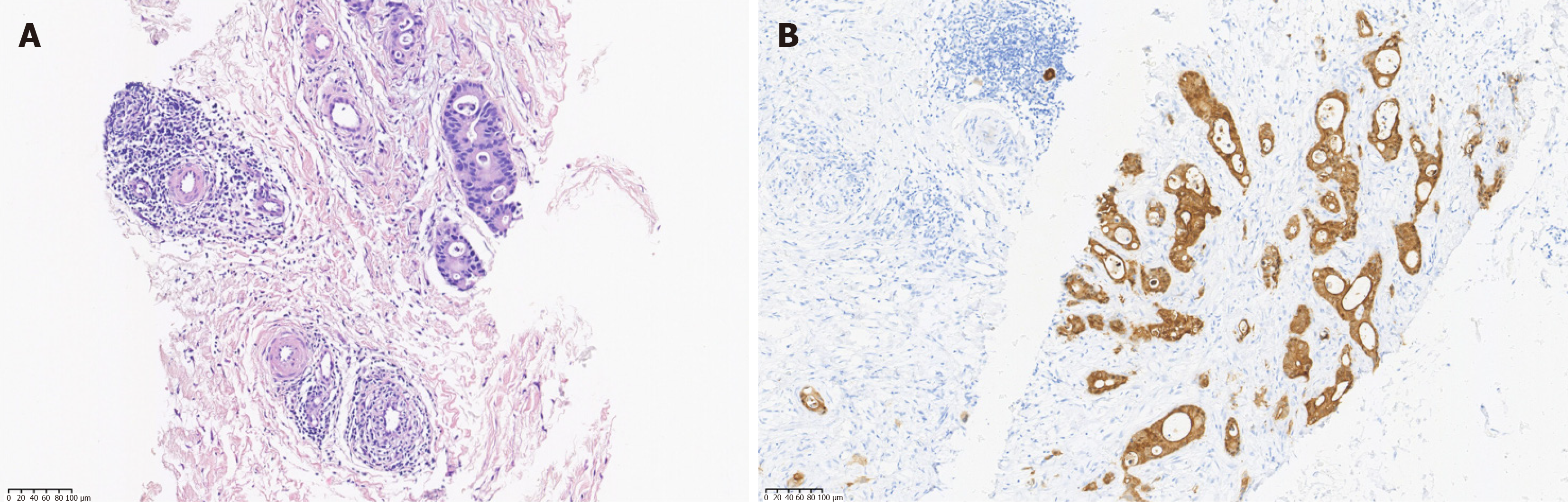
Biopsy specimens revealed moderately to poorly differentiated adenocarcinoma (G2-G3). Immunohistochemical analysis showed the mass was CK7-positive, CK20-negative, CDX-positive, Villin-positive, PSA-negative, TTF-1-negative, and HER2 (0), confirming metastasis of digestive tract adenocarcinoma (Figure 3). The patient was finally diagnosed with gastric cancer with right inguinal metastasis. Pathological stage: PT4aN3aM1.
During hospitalization, the patient's right inguinal mass underwent a puncture biopsy. However, before the biopsy pathology results were available, the patient suddenly developed upper gastrointestinal bleeding. As conservative medical treatment and endoscopic assessment were ineffective, emergency surgical intervention was urgently carried out. The surgery revealed implantation nodules on the peritoneum and PM staged as P1c, located in zones 2, 5, and 6, with a peritoneal cancer index of 3. Additionally, a locally resectable gastric tumor was identified. The patient subsequently underwent palliative total gastrectomy and D2 lymph node dissection. The excised specimen showed a Borrmann type III advanced gastric tumor, measuring 4.7 cm × 4.5 cm × 1.5 cm, located on the lesser curvature of the gastric antrum. The tumor was ulcerated, and bleeding was observed. Pathological examination indicated that there were no residual cancer cells at the proximal and distal margins. Pathological analysis of the primary gastric carcinoma, classified according to the Japanese Classification of Gastric Carcinoma, revealed moderately to poorly differentiated adenocarcinoma. Thirteen of the nineteen resected regional lymph nodes were positive, specifically in the No. 1, 3, 4, 5, 6 (sub-pyloric), 9, and 12 regions. Lymphatic vessel, vascular, and nerve invasion were noted. Postoperatively, the patient received hyperthermic intraperitoneal chemotherapy along with enteral and parenteral nutrition support, and the postoperative course was uneventful. One week post-surgery, the biopsy of the puncture revealed that the inguinal mass originated from metastatic gastrointestinal adenocarcinoma. One month after surgery, the patient continued to receive radiation therapy in the right inguinal area.
After undergoing palliative gastrectomy, the patient experienced moderate improvement in gastrointestinal symptoms. However, after discharge, the patient was lost to follow-up. Through subsequent telephone communication, we learned that he survived for 10 months post-surgery.
Gastric cancer mainly metastasizes to the lymph nodes, liver, and peritoneum[2]. PM is a very poor prognostic factor in patients with advanced gastric cancer[4]. To our knowledge, a few cases have reported gastric cancer metastasis to the umbilicus[5], port site[6], and lower chest[7]. Additionally, metastases to the left armpit[8], scalp[9], and face[10] have been reported, which are far from the stomach. In our case, a patient with a solid mass in the right inguinal area pre
The possible origins of the right lump in the inguinal area are hematogenous metastasis, lymphogenous metastasis from inguinal lymph nodes, and direct infiltration from peritoneal dissemination. The inguinal mass visible on ultrasound and CT scan images appears to be located in the inguinal canal. Since this patient had peritoneal dissemination and no other metastatic lesions suspected of hematogenous or lymphogenous metastasis, direct infiltration from peritoneal dissemination was most likely. We infer that due to implantation in the inguinal hernia sac, a mass formed within the inguinal canal over time. The prognosis of advanced gastric cancer is known to be poor, with the median survival of patients with unresectable advanced gastric cancer being 10-18 months[11]. Early diagnosis of unusual metastasis and implementation of standard treatment before the onset of new clinical symptoms or general deterioration can improve the prognosis and quality of life. We experienced a rare case of distant metastasis in the right inguinal area originating from primary gastric cancer. Clinicians should always keep in mind that distant metastasis is a possible diagnosis when a new mass appears or with discomfort, which may be a signal of patients with preexisting internal organ malignancies. Attention should be paid to the systematic review during the consultation to explore possible connections.
We report a sporadic case of distant metastasis of gastric cancer to the right inguinal region. For patients with gastrointestinal symptoms, local masses should be given high attention. Patients with distant metastasis often have a poor prognosis. Various imaging techniques and fine-needle aspiration biopsy aid in detecting subcutaneous metastatic lesions, and radiotherapy is a possible treatment option.
| 1. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 8170] [Article Influence: 8170.0] [Reference Citation Analysis (2)] |
| 2. | Li GZ, Doherty GM, Wang J. Surgical Management of Gastric Cancer: A Review. JAMA Surg. 2022;157:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 145] [Article Influence: 48.3] [Reference Citation Analysis (0)] |
| 3. | Koemans WJ, Lurvink RJ, Grootscholten C, Verhoeven RHA, de Hingh IH, van Sandick JW. Synchronous peritoneal metastases of gastric cancer origin: incidence, treatment and survival of a nationwide Dutch cohort. Gastric Cancer. 2021;24:800-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Coccolini F, Cotte E, Glehen O, Lotti M, Poiasina E, Catena F, Yonemura Y, Ansaloni L. Intraperitoneal chemotherapy in advanced gastric cancer. Meta-analysis of randomized trials. Eur J Surg Oncol. 2014;40:12-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 179] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 5. | Rais G, Bourhafour M, Nafidi FZ, Rais F. A Huge Sister Mary Joseph's Nodule From Signet Ring Cell Gastric Carcinoma Showing Good Response to FOLFOX-Based Chemotherapy Regimen. J Med Cases. 2022;13:115-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Fukui Y, Kubo N, Sakurai K, Tamamori Y, Maeda K, Ohira M. Metachronous port site, muscular and subcutaneous metastases from a gastric adenocarcinoma: a case report and review of articles. Surg Case Rep. 2021;7:124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Namikawa T, Munekage E, Munekage M, Maeda H, Yatabe T, Kitagawa H, Kobayashi M, Hanazaki K. Subcutaneous metastasis arising from gastric cancer: A case report. Mol Clin Oncol. 2017;6:515-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | He FJ, Zhang P, Wang MJ, Chen Y, Zhuang W. Left armpit subcutaneous metastasis of gastric cancer: A case report. World J Clin Cases. 2019;7:4137-4143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Ryu HR, Lee DW, Choi HJ, Kim JH, Ahn H. Scalp metastasis of advanced gastric cancer. Arch Craniofac Surg. 2021;22:157-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kirchberger MC. Unusual presentation of a cutaneous metastasis in the face arising from gastric cancer: a case report. SAGE Open Med Case Rep. 2018;6:2050313X18795080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Leiting JL, Grotz TE. Advancements and challenges in treating advanced gastric cancer in the West. World J Gastrointest Oncol. 2019;11:652-664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (1)] |