Published online Jan 27, 2025. doi: 10.4240/wjgs.v17.i1.99464
Revised: October 27, 2024
Accepted: November 18, 2024
Published online: January 27, 2025
Processing time: 93 Days and 6.3 Hours
A total of 100 patients diagnosed with mixed hemorrhoids from October 2022 to September 2023 in our hospital were randomly divided into groups by dice rol
To analyze the clinical effect and prognosis of mixed hemorrhoids treated with polidocanol injection combined with automatic elastic thread ligation operation (RPH).
A total of 100 patients with mixed hemorrhoids who visited our hospital from October 2022 to September 2023 were selected and randomly divided into the control group (n = 50) and the treatment group (n = 50) by rolling the dice. The procedure for prolapse and hemorrhoids (PPH) was adopted in the control group, while polidocanol foam injection + RPH was adopted in the treatment group. The therapeutic effects, operation time, wound healing time, hospital stay, pain si
Compared with the control group, the total effective rate of treatment group was higher, and the difference was significant (P < 0.05). The operation time/wound healing time/hospital stay in the treatment group were shorter than those in the control group (P < 0.05). The pain scores at 24 hours after operation/first defecation pain score of the treatment group was significantly lower than those in the control group (P < 0.05). After surgery, the QOL scores of the two groups decreased, with the treatment group having higher scores than that of the control group (P < 0.05). Compared with the control group, the incidence of postoperative complications in the treatment group was lower, and the difference was significant (P < 0.05); However, there was no significant difference in the incidence of postoperative bleeding between the two groups (P > 0.05); There was no significant difference in the incidence of anal stenosis 3 months after operation and the recurrence rate 1 year after operation between the two groups (P > 0.05).
For patients with mixed hemorrhoids, the therapeutic effect achieved by using polidocanol injection combined with RPH was better. The wounds of the patients healed faster, the postoperative pain was milder, QOL improved, and the incidence of complications was lower, and the short-term and long-term prognosis was good.
Core Tip: Effective surgical and pharmaceutical treatment is particularly important for patients with mixed hemorrhoids, which can achieve better therapeutic effects and good long-term prognosis of patients.
- Citation: Huang YM, Ouyang D. Clinical observation on prognosis of mixed hemorrhoids treated with polidocanol injection combined with automatic elastic thread ligation operation. World J Gastrointest Surg 2025; 17(1): 99464
- URL: https://www.wjgnet.com/1948-9366/full/v17/i1/99464.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i1.99464
Mixed hemorrhoid is a common anorectal disease in clinic, referring to the simultaneous existence of internal and external hemorrhoids in the same direction of the anus, with the prevalence rate as high as 51.56% in China[1,2]. In recent years, changes in dietary habits have led to a rising prevalence of mixed hemorrhoids. Patients with mixed hemorrhoids often have symptoms such as hematochezia, bulge, and fluid oozing. In severe cases, they can cause inflammation and thrombosis, causing great pain and reducing the quality of life of patients. Aibuedefe et al[3] of St Kyle's Hospital in the United Kingdom proposed the mixed hemorrhoid external dissection and internal ligation in 1937. The operation is simple, low in device requirements, and accurate. It is a traditional surgical method widely used in clinical practice. However, patients will suffer obvious pain after operation, and the wound healing takes a long time, resulting in high risk of complications. Therefore, it is necessary to seek a safer and more effective minimally invasive surgical plan in time. The procedure for prolapse and hemorrhoids (PPH) is a minimally invasive surgery that can lift the prolapsed hemorrhoidal nucleus, block blood supply and stop bleeding. Besides, it has the advantages of small pain and small trauma. However, due to the difficult operation and high incidence of postoperative complications, PPH has gradually been replaced by other operations[4]. The application of polidocanol injection in mixed hemorrhoids has not been reported in China, but there are some foreign literature reports that polidocanol injection has a positive hemostatic effect on mixed hemorrhoids, but has a weak effect in lifting the anal pad[5]. Automatic elastic thread ligation operation (RPH) is developed based on the traditional ligation of internal hemorrhoids. It can perform multi-site ligation and effectively lift and lower the anal pad. In addition, it has the advantages of simple operation, mild pain for patients, rapid wound healing and good prognosis. However, it has the risk of bleeding after the operation[6]. Therefore, it is proposed that if the combined application of polidocanol injection and RPH to mixed hemorrhoids can achieve good surgical efficacy and hemostatic effect. In order to further explore the clinical prognosis observation of the treatment of mixed hemorrhoids with polidocanol injection combined with RPH, 100 patients with mixed hemorrhoids who were admitted to our hospital from October 2022 to September 2023 were selected for the following analysis.
Diagnostic criteria: Mixed hemorrhoid was diagnosed with reference to Clinical Practice Guidelines for the Treatment of Hemorrhoid Disease[7].
Inclusion criteria: (1) Diagnosis has been confirmed; (2) During the treatment, no drugs or methods that may affect the treatment effect are used; (3) Patients have good compliance and can be matched with regular follow-up; and (4) The patient knows the situation and signs the consent form.
Exclusion criteria: (1) Patients with non-hemorrhoidal constipation and diarrhea; (2) Combined with acute inflammation in the anal region, such as perianal abscess and anal fistula; (3) Chronic inflammatory anorectal disease, such as Crohn’s disease; (4) Ulcerative colitis and other diseases; (5) Allergic to polidocanol or its components; (6) Hematopoietic and coagulation system diseases; (7) Severe cardiovascular and cerebrovascular diseases, and anorectal malignant tumor diseases; or (8) Patients with poor compliance and no regular follow-up.
Time: From October 2022 to September 2023.
Source: A total of 100 patients with mixed hemorrhoids who visited our hospital were randomly divided into two groups (control group and treatment group) with 50 cases by dice rolling. Patients in the control group: 19 males and 31 females; with the lower age limit of 24 years old and the upper limit of 87 years old, with the average age of (51.42 ± 13.89) years old; the course of disease of 1-7 years, with the average age of (4.00 ± 1.12) years; patients were classified into grade III (32 cases) and grade IV (18 cases); with the body mass index of at the lowest 18 kg/m2 and the highest 24 kg/m2, with the average age of (21.00 ± 1.23) kg/m2. Patients in the treatment group: 24 males and 26 females; with the lower age limit of 27 years old and the upper age limit of 83 years old, with the average age of (54.62 ± 12.85) years old; and the course of disease of 2-6 years, with the average age of (4.00 ± 1.10) years; patients were classified into the grade III (33 cases) and grade IV (17 cases); with the body mass index of at the lowest 17 kg/m2 and 25 kg/m2 at the highest, with the average age of (21.00 ± 1.26) kg/m2. The clinical data of the two groups were comparable (P > 0.05).
Control group: PPH was adopted: Local anesthesia, after the onset of anesthesia, the patients were kept in the lithotomy position. The patients were routinely sterilized and draped. The anoscope was used to assist in observing the lesions of the patients and appropriate anal dilatation was performed. The anal dilator was inserted into the anus and sutured and fixed at the periphery of the anus. The inner core was taken out and the hemorrhoidal nucleus was also contained, so that the patient's dentate line was exposed. The semi-endoscopic insertion was performed, and the double purse-string suture was performed on the rectal mucosa at the positions of 3-3.5 cm and 4-4.5 cm above the toothed wire, the stapler was expanded to the maximum extent and inserted, the purse-string wire was sequentially tightened and ligated, the ligature wire was pulled out from the side hole of the stapler, and the thread end of the ligature wire was moderately pulled, and the knob at the tail end of the stapler was rotated to slowly tighten the circular cutting head of the head of the stapler. In female patients, digital examination of the vagina is performed to ensure that there is no tension in order to prevent rectovaginal fistula. The safety device was opened, and the stapler was fired for 30 seconds, and then it was taken out to check whether there was active bleeding at the anastomosis of the patient. If there was active bleeding, three absorbable sutures were used for ligation and hemostasis, and the anal dilator was removed. The condition of external hemorrhoid was carefully examined. If necessary, the external hemorrhoid was removed. After the operation, Vaseline gauze was placed for dressing.
Treatment group: Polidocanol injection + RPH was adopted: Local anesthesia, after the anesthesia was effective, the lithotomy position was taken for routine disinfection and towel laying. The fixing clip of the push tube was removed, and the anoscope was inserted. The inner core was pulled out to fully expose the dentate line and hemorrhoidal nucleus. The anal canal and mucosa are disinfected, the anoscope is fixed by the left hand of an operator, the handle is held by the right hand, the ligating port is aligned with the mucosa tissue/hemorrhoidal tissue at the upper part of the hemorrhoidal nucleus, negative pressure suction is performed, when the pointer of the negative pressure meter slowly rises to between -0.08 and -0.1 MPa and keeps still, the driving wheel is rotated by 360° to the blue point to return to the original position, the push wire tube is rotated to the number 1, the first push wire tube is released, the assistant helps to rob, The operator took the push wire tube in his left hand and the push wire tube in his right hand, tightly pinched the tail part of the elastic wire, and forcibly opposed the traction. The loop at the front end of the elastic wire was tightened to the target tissue and tied tightly, and the negative pressure was turned on, the switch and the tied tissue were released. The push wire tube was held in his left hand, and he drew back with a little force to expose the front end of the elastic wire. The long shear was held in his right hand, and it was cut at the knot with a length of about 4-5 mm. The wound surface was carefully examined to ensure no bleeding. In the same method, internal hemorrhoids and hemorrhoidal mucosa at other sites are treated, 2-3 mL of 1% polidocanol injection is taken, polidocanol and air are prepared by using a three-way pipe and foam in a ratio of 1:4, and are repeatedly pushed and injected, and then 10 mL of air foam is prepared; hemorrhoids needing to be injected are exposed through an anoscope, and 2-3 mL of foam liquid is injected into hemorrhoidal tissues, until the volume of the hemorrhoids became larger and the color turned white. After the injection is completed, the hemorrhoid tissues are treated by using the foam liquid, cotton balls were used for compression for a moment to stop bleeding. After the hemorrhoidal nuclei of the patients were completely treated, the anoscope was withdrawn, and the condition of external hemorrhoids of the anus was carefully examined. If necessary, the external hemorrhoids were excised. After the surgery, Vaseline gauze was placed and bound.
(1) Treatment effects. Cure: The patient's symptoms (hemorrhoid prolapse, bleeding, pain, etc.) completely disappeared, hemorrhoids completely atrophy, wound healing; Improved: The patient's symptoms (hemorrhoid prolapse, bleeding, pain, etc.) were significantly reduced, most of the hemorrhoids atrophy, and the surgical wound healing was delayed; Non-healing: The symptoms (hemorrhoid prolapse, bleeding, pain, etc.) of the patient were not significantly relieved, and the wound surface was not healed[8]. Total effective rate = (cured + improved) cases/total cases × 100%;
(2) The operation time, wound healing time and hospital stay of the two groups were compared. The operation time, the time from postoperative to wound healing, and the total hospitalization time from admission to discharge of patients in the two groups were counted and recorded;
(3) The pain situations of the two groups were compared. At 24 hours after surgery and from the time of surgery to the first defecation, the visual analogue scale (VAS) was used to assess the pain severity of the patients, and a 10 cm long straight line was drawn, with 0 at the leftmost end indicating no pain, and 10 at the rightmost end indicating severe pain. The higher the score was, the more obvious the pain would be[9];
(4) The patients' quality of life (QOL) was compared before and after surgery between the two groups, and their social activities and daily living abilities were evaluated using the QOL-35 scale, with 0-4 points for each item. The higher the score, the worse the patients' QOL;
(5) The incidence of complications was compared between the two groups. After the surgery, the occurrence of postoperative bleeding, edema, and infection in the two groups was assessed, and the incidence of complications was calculated as the sum of the three;
And (6) The prognosis of patients in the two groups were compared. Three months after surgery, anal stenosis was calculated between the two groups. The criteria were as follows: When the patients were examined again, anal stenosis was defined as the resistance sensation of the forefinger passing through the anus. One year after surgery, the recurrence cases of the two groups were counted, and the criteria were as follows: Prolapse of hemorrhoidal tissue, pain, bleeding, and other symptoms.
Statistical software SPSS22.0 was used for data processing. The enumeration data were presented in the form of [n (%)]. The data were compared with the χ2 test, and the measurement data were presented in the form of (mean ± SD), and analyzed using Shapiro-Wilk normality. For the difference comparison, t test was used, and P < 0.05 represented the difference was significant.
The total effective rate in the treatment group was higher than that in the control group, with statistical significance (χ2 = 7.111, P = 0.007; Table 1). In the treatment group, the total effective rate was 98.00% (49/50 cases), and only one case was not resolved. In the control group, the total effective rate was 82.00% (41/50 cases), and 9 cases were not resolved.
| Group | Number of cases | Cured | Improved | Non-healing | Total effective rate |
| Control group | 50 | 23 (46.00) | 18 (36.00) | 9 (18.00) | 41 (82.00) |
| Treatment group | 50 | 29 (58.00) | 20 (40.00) | 1 (2.00) | 49 (98.00) |
| χ2 value | 7.111 | ||||
| P value | 0.007 |
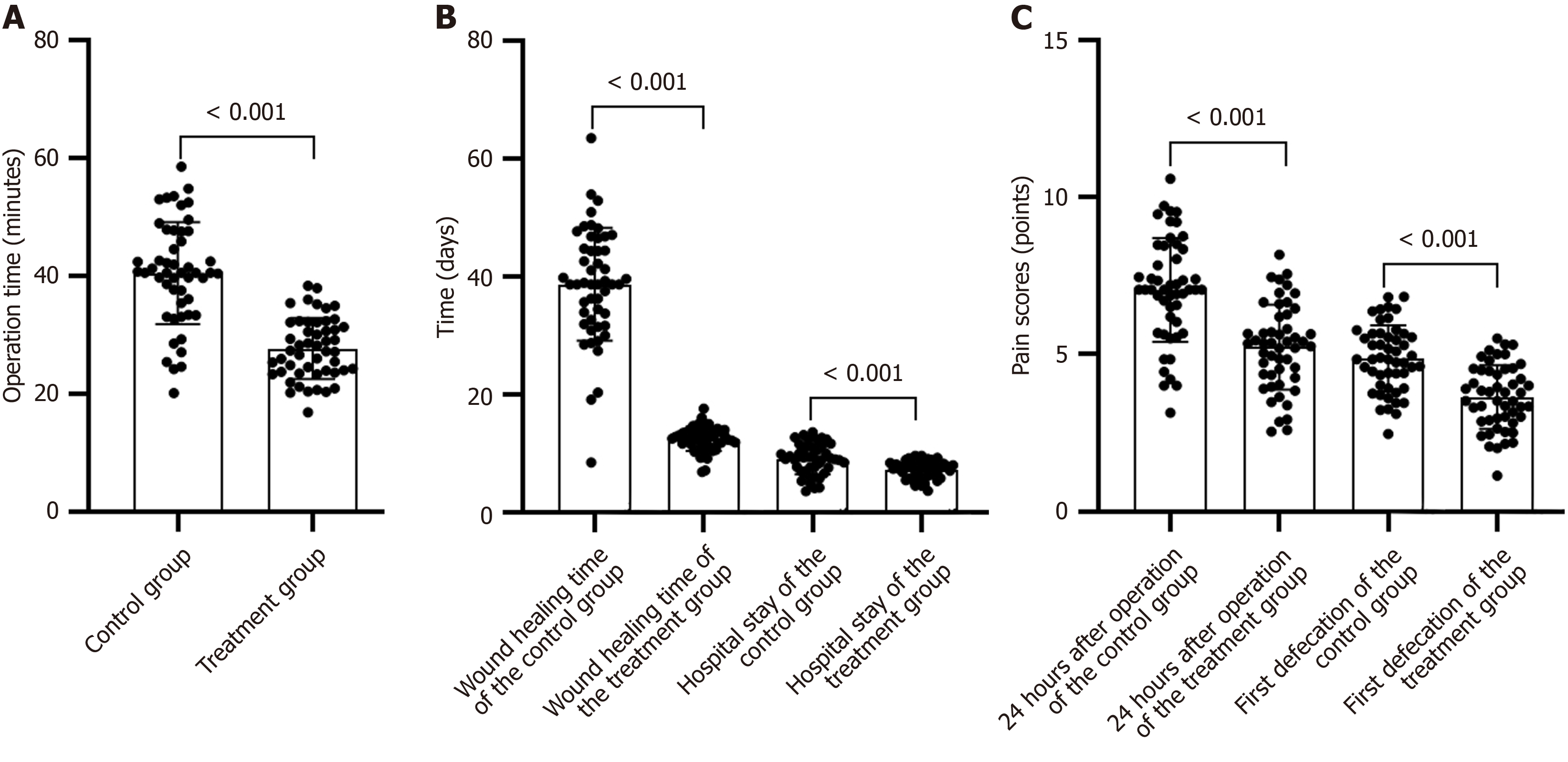
The surgery duration, wound healing time, and hospital stay in the treatment group were shorter than those in the control group, and the difference was statistically significant (P < 0.05; Table 2, Figure 1A and B).
| Group | Number of cases | Operation time (minutes) | Wound healing time (day) | Hospital stay (day) |
| Control group | 50 | 55.90 ± 12.84 | 16.72 ± 3.04 | 9.72 ± 3.04 |
| Treatment group | 50 | 31.70 ± 11.63 | 14.06 ± 2.71 | 6.26 ± 1.95 |
| t value | 9.878 | 4.619 | 6.774 | |
| P value | < 0.001 | < 0.001 | < 0.001 |
The pain scores at 24 hours after surgery or first defecation in the treatment group were significantly shorter than those in the control group (P < 0.05; Table 3 and Figure 1C).
| Group | Number of cases | 24 hours after surgery (points) | First defecation pain score (points) |
| Control group | 50 | 3.94 ± 1.33 | 5.86 ± 1.36 |
| Treatment group | 50 | 1.96 ± 1.40 | 3.56 ± 1.80 |
| t value | 7.250 | 7.209 | |
| P value | < 0.001 | < 0.001 |
Before surgery, there was no statistically significant difference in QOL scores between the two groups (P > 0.05). After surgery, the QOL scores of the two groups decreased, with the treatment group scored being significantly higher than those of the control group (P < 0.05; Table 4).
| Group | Number of cases | Before surgery, mean ± SD, points | After surgery, mean ± SD, points | t value | P value |
| Control group | 50 | 73.61 ± 9.25 | 54.26 ± 8.17 | 11.087 | < 0.001 |
| Treatment group | 50 | 72.98 ± 9.34 | 41.38 ± 8.06 | 18.112 | < 0.001 |
| t value | - | 0.339 | 7.936 | - | - |
| P value | - | 0.735 | < 0.001 | - | - |
The incidence of postoperative complications in the treatment group was lower than that in the control group, with statistical significance (χ2 = 0.060, P = 0.013; Table 5). Complications occurred in two cases (4.00%, 2/50) in the treatment group. In the control group, 10 patients experienced complications (20.00%, 10/50). However, there was no significant difference in the incidence of postoperative bleeding between the two groups (P > 0.05; Table 5).
| Group | Number of cases | Postoperative hemorrhage | Edema | Infect | Complication incidence |
| Control group | 50 | 5 (10.00) | 3 (6.00) | 2 (4.00) | 10 (20.00) |
| Treatment group | 50 | 1 (2.00) | 1 (2.00) | 0 (0.00) | 2 (4.00) |
| χ2 value | 0.060 | ||||
| P value | 0.013 |
There was no significant difference in the incidence of anal stenosis 3 months after operation and the recurrence rate 1 year after operation between the two groups (P > 0.05; Table 6).
| Group | Number of cases | Anal stenosis rate 3 months after surgery | Recurrence rate in 1 year after operation |
| Control group | 50 | 2 (4.00) | 3 (6.00) |
| Treatment group | 50 | 0 | 1 (2.00) |
| χ2 value | 0.510 | 0.260 | |
| P value | 0.475 | 0.610 |
Hemorrhoid is a common benign disease in anorectal department. According to statistics, the prevalence rate of hemorrhoids in China accounts for 80.60% of anorectal diseases. Pathologically, hemorrhoids is a chronic disease caused by the tortuous and expanding of blood vessels and anal veins at the lower end of rectum due to abdominal duct/other space-occupying lesions, including internal hemorrhoid, external hemorrhoid and mixed hemorrhoid[10]. PPH is a common operation for the treatment of this disease, with the advantages of minimal invasion, good effect, and mild pain. However, according to the research by Romaguera et al[11], the incidence of secondary hemorrhage after PPH for mixed hemorrhoids was 3.10%, which affected the prognosis of patients. Sturiale et al[12] foreign scholars have found that PPH surgery is relatively difficult. If it is not properly operated, serious complications such as bleeding, anastomotic stenosis and postoperative recurrence can easily occur. At present, the treatment of mixed hemorrhoids is still challenging, and there are many different evidence-based treatment options available. There is evidence that the use of new surgical techniques is expected to reduce pain, but there has been controversy about this conclusion[13,14].
Some scholars have found that RPH had obvious therapeutic effects on patients with mixed hemorrhoids in the observation group, with short operation time and low incidence of postoperative complications in patients[15]. However, clinical findings showed that in some patients treated with RPH in the past, the mucosal erosion was serious, and some eroded mucosa could not be completely inserted between the ligation points, resulting in incomplete hemostasis after surgery. Polidocanol injection can be used as a vascular embolization hardener. Gallo et al[16] verified that polidocanol injection was safe, painless and effective, and it could treat hemorrhoidal hemorrhage repeatedly and at low cost. This study found that after treatment, the total effective rate of the treatment group was 98%, which was higher than 82% of the control group (P < 0.05). Analysis of the reason: RPH mainly used the automatic elastic thread hemorrhoid ligation anastomat with negative pressure suction effect to aim the negative pressure gun head at the hemorrhoidal tissue to be ligated and the mucosal tissue on hemorrhoids. After the negative pressure suction, the elastic thread was tightened, which can effectively promote the ischemia, atrophy, necrosis and shedding of hemorrhoidal tissue[17]. In combination with that polidocanol injection, foam is for by mixing with air, and the foam bubble can maximize the contact surface area in vivo, enable the drug to locally spread in hemorrhoid tissues for a long time and have a better hemostatic effect, and better curative effect can be achieve by the combination of the two[18].
It was also found that the operation time, wound healing time and hospital stay in the treatment group were shorter than those in the control group (P < 0.05). The reason was that the RPH operation was simple in operation and short in operation time. The hemostatic treatment with polidocanol injection had a definite hemostatic effect, which could promote the earlier healing of the wound, avoid postoperative complications, improve the prognosis, and promote the patient to be discharged from hospital earlier[19]. The data in Table 3 showed that the VAS scores of the treatment group at 24 hours after operation and first defecation pain score were lower (P < 0.05). We considered that the combined treatment could also improve the postoperative pain. RPH is a minimally invasive surgery, which causes less trauma to patients and milder pain. The operation has good continuity, which can reduce the blood supply of hemorrhoids and gradually shrink the hemorrhoidal nuclei, thereby relieving the symptoms and pain. The hemostatic effect of polidocanol injection is good. The wounds of patients can heal earlier after operation and the degree of postoperative pain can be reduced. The results of this study showed that the QOL scores of the two groups decreased after surgery, with the treatment group score being higher than that of the control group (P < 0.05), indicating that the QOL of the patients in the treatment group was higher after surgery. This may be owing to the higher total effective rate of the patients in the treatment group, lower VAS score at 24 hours after the surgery, and lower incidence of postoperative complications.
The report shows that the recurrence rate of mixed hemorrhoids after operation is 0%-56.50%, and the recurrence rate of most reports is 20%. The recurrence of mixed hemorrhoids after operation is mostly related to the incomplete cure of the disease, anal stenosis and bad living habits[20]. The results of this study showed that the incidence of complications in the treatment group was lower (P < 0.05), However, there was no significant difference in the incidence of anal stenosis 3 months after operation and the recurrence rate 1 year after operation between the two groups, suggesting that the treatment of polidocanol injection + RPH was safer and had a better prognosis. In the RPH treatment, the contraction of elastic thread can continuously cut off the hemorrhoidal nucleus, reduce the bleeding during the operation and the risk of bleeding during the off-line period. Besides, the suture and ligation method in this operation is more firm, and the anal pad can be lifted up. Under the strong contraction of the elastic thread, the internal hemorrhoidal nucleus contracts indefinitely, and the wound surface is smaller after the hemorrhoidal nucleus falls off, which enables the disease to recover earlier, and further reduces the risk of postoperative complications[21,22]. Similar to sanguinol, polidocanol injection shows obvious hemostatic effect and can ensure the safety of operation. The combined treatment of the two is more thorough, and the long-term prognosis of the patients is better, thus reducing the recurrence rate of the disease[23]. However, the results of this study are on the contrary, which may be related to the small sample size of this study.
For patients with mixed hemorrhoids, the treatment effect with polidocanol injection combined with RPH is better. The operation time, wound healing time and hospital stay are shorter, and the postoperative pain is milder, the postoperative quality of life is higher. It can reduce the incidence of surgical complications. The short-term and long-term prognosis is good. However, this study still has some limitations, because the number of selected cases is small and the study time is relatively short. Further study is needed on the explored treatment plan.
| 1. | Hollingshead JR, Phillips RK. Haemorrhoids: modern diagnosis and treatment. Postgrad Med J. 2016;92:4-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Picciariello A, Tsarkov PV, Papagni V, Efetov S, Markaryan DR, Tulina I, Altomare DF. Classifications and Clinical Assessment of Haemorrhoids: The Proctologist's Corner. Rev Recent Clin Trials. 2021;16:10-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Aibuedefe B, Kling SM, Philp MM, Ross HM, Poggio JL. An update on surgical treatment of hemorrhoidal disease: a systematic review and meta-analysis. Int J Colorectal Dis. 2021;36:2041-2049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | He F, Zhang X, Lu D, Wang Z. Clinical efficacy of ultrasound doppler-guided hemorrhoidal artery ligation combined with procedure for prolapse and hemorrhoids in treatment of severe hemorrhoids. Medicine (Baltimore). 2023;102:e36189. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Fernandes V, Fonseca J. Polidocanol Foam Injected at High Doses with Intravenous Needle: The (Almost) Perfect Treatment of Symptomatic Internal Hemorrhoids. GE Port J Gastroenterol. 2019;26:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 6. | He YH, Tang ZJ, Xu XT, Huang DQ, Zhang LS, Tang QZ, Fan ZM, Zou XJ, Zou GJ, Zhang CY, Hu F, Xie B, Li YH, Tong Y, Liu HC, Li K, Luo YL, Liu F, Situ GW, Liu ZL. A Randomized Multicenter Clinical Trial of RPH With the Simplified Milligan-Morgan Hemorrhoidectomy in the Treatment of Mixed Hemorrhoids. Surg Innov. 2017;24:574-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Abramowitz L, Godeberge P, Staumont G, Soudan D; Société Nationale Françoise de Colo-Proctologie (SNFCP). [Clinical practice guidelines for the treatment of hemorrhoid disease]. Gastroenterol Clin Biol. 2001;25:674-702. [PubMed] |
| 8. | Anorectal Branch of Chinese Medical Doctor Association; Colorectal Surgery Group, Surgical Society of Chinese Medical Association. [Chinese expert consensus on the treatment of hemorrhoids by injection(2023 edition)]. Zhonghua Wei Chang Wai Ke Za Zhi. 2023;26:1103-1111. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Liu J, Wang M, Zheng X. Analysis of the effect of evidence-based nursing intervention model in patients with mixed hemorrhoids after PPH. Minerva Surg. 2024;79:100-102. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Romaguera VP, Sancho-Muriel J, Alvarez-Sarrdo E, Millan M, Garcia-Granero A, Frasson M. Postoperative Complications in Hemorrhoidal Disease and Special Conditions. Rev Recent Clin Trials. 2021;16:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Sturiale A, Fabiani B, Menconi C, Cafaro D, Fusco F, Bellio G, Schiano di Visconte M, Naldini G. Long-term results after stapled hemorrhoidopexy: a survey study with mean follow-up of 12 years. Tech Coloproctol. 2018;22:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Yuan XG, Wu J, Yin HM, Ma CM, Cheng SJ. Comparison of the efficacy and safety of different surgical procedures for patients with hemorrhoids: a network meta-analysis. Tech Coloproctol. 2023;27:799-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Yu K, Li H, Xue P, Xie Z, Tang M, He H, Wu J. Modified ultrasound scalpel haemorrhoidectomy versus conventional haemorrhoidectomy for mixed haemorrhoids: a study protocol for a single-blind randomised controlled trial. Trials. 2023;24:140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Xie G, Su QL, Luo MQ, Wu XW, Luo JE. [Clinical effect of automatic elastic wire ligation for hemorrhoids combined with submucosal injection in the treatment of mild to moderate mixed hemorrhoids]. Linchuang Yu Bingli Zazhi. 2018;38:2129-2133. [DOI] [Full Text] |
| 16. | Gallo G, Picciariello A, Pietroletti R, Novelli E, Sturiale A, Tutino R, Laforgia R, Moggia E, Pozzo M, Roveroni M, Bianco V, Realis Luc A, Giuliani A, Diaco E, Naldini G, Trompetto M, Perinotti R, D'Andrea V, Lobascio P. Sclerotherapy with 3% polidocanol foam to treat second-degree haemorrhoidal disease: Three-year follow-up of a multicentre, single arm, IDEAL phase 2b trial. Colorectal Dis. 2023;25:386-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 17. | Yu Q, Zhi C, Jia L, Li H. Efficacy of Ruiyun procedure for hemorrhoids combined simplified Milligan-Morgan hemorrhoidectomy with dentate line-sparing in treating grade III/IV hemorrhoids: a retrospective study. BMC Surg. 2021;21:251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Moser KH, Mosch C, Walgenbach M, Bussen DG, Kirsch J, Joos AK, Gliem P, Sauerland S. Efficacy and safety of sclerotherapy with polidocanol foam in comparison with fluid sclerosant in the treatment of first-grade haemorrhoidal disease: a randomised, controlled, single-blind, multicentre trial. Int J Colorectal Dis. 2013;28:1439-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 19. | Fang ZJ, Wang LX, Jin F. [Efficacy of polidocanol foam sclerotherapy in treatment of patients with advanced hemorrhoids]. Shijie Huaren Xiaohua Zazhi. 2024;32:361-367. [DOI] [Full Text] |
| 20. | Lohsiriwat V, Sheikh P, Bandolon R, Ren DL, Roslani AC, Schaible K, Freitag A, Martin M, Yaltirik P, Godeberge P. Recurrence Rates and Pharmacological Treatment for Hemorrhoidal Disease: A Systematic Review. Adv Ther. 2023;40:117-132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Dekker L, Han-Geurts IJM, Rørvik HD, van Dieren S, Bemelman WA. Rubber band ligation versus haemorrhoidectomy for the treatment of grade II-III haemorrhoids: a systematic review and meta-analysis of randomised controlled trials. Tech Coloproctol. 2021;25:663-674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Lisi G, Campanelli M, Grande S, Milito G, Grande M. Sclerotherapy with 3% polidocanol foam for third- and fourth-degree hemorrhoids as "bridge treatment" during the COVID-19 pandemic in Italy. Int J Colorectal Dis. 2021;36:1321-1322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 23. | Makanjuola A, Balogun OS, Osinowo AO, Adesanya AA, da Rocha JT. Comparison of rubber band ligation with 3% polidocanol injection sclerotherapy for the treatment of internal haemorrhoids at a Nigerian tertiary hospital. Niger Postgrad Med J. 2020;27:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |