Published online Jan 27, 2025. doi: 10.4240/wjgs.v17.i1.99155
Revised: October 18, 2024
Accepted: November 12, 2024
Published online: January 27, 2025
Processing time: 106 Days and 5.1 Hours
Routinely separating the ligamentum teres uteri (LTU) intraoperatively remains an unresolved issue for female children undergoing surgery for indirect inguinal hernia (IIH).
To identify the effect of LTU preservation in laparoscopic high hernia sac ligation (LHSL) in children with IIH.
The participants were 100 female children with unilateral IIH admitted from April 2022 to January 2024 to the Pediatric Surgery Department of Zhangzhou Muni
This study comparatively analyzed the operation time, hospitalization time, blood loss, postoperative recurrence rate, and complications (repeated pain in the in
The above results indicate that LTU preservation during LHSL exerts certain therapeutic benefits for children with IIH. LTU preservation does not increase hospitalization time, blood loss, postoperative recurrence rate, and complications, which is safe and feasible, compared with conventional LTU ligation. LHSL with LTU preservation should be performed if conditions permit, which is worth popularizing.
Core Tip: The ligamentum teres uteri (LTU) is one of the main ligaments of the uterus and plays a crucial role in maintaining the anteverted uterine position. However, currently, the surgical method of ligating the LTU together with the hernia sac is mostly adopted intraoperatively for female patients with indirect inguinal hernia, which may cause LTU ligation-associated complications in some female children. This study revealed that LTU preservation intraoperatively does not increase hospital stay, blood loss, postoperative recurrence rate, or complications, which is safe and feasible, compared with conventional LTU ligation. Laparoscopic high hernial sac ligation with LTU preservation should be performed when conditions permit, which is worthy of popularization.
- Citation: Lin XQ, Li HF, Lin YZ, Chen WY. Effect of ligamentum teres uteri preservation in laparoscopic high hernia sac ligation in children with indirect inguinal hernia. World J Gastrointest Surg 2025; 17(1): 99155
- URL: https://www.wjgnet.com/1948-9366/full/v17/i1/99155.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i1.99155
Indirect inguinal hernia (IIH) is a prevalent condition in pediatric surgery, with high hernial sac ligation being the mainstay of treatment[1]. Laparoscopic high hernial sac ligation (LHSL) exhibits certain clinical advantages over conventional open inguinal hernial repair and high hernial sac ligation, including cosmetic incision, short operation time (OT), easy contralateral concealed hernia detection intraoperatively, rapid postoperative recovery, and low recurrence rate[2]. Clinically, female patients with IIH have different anatomical structures from male patients. The ligament that passes through the inguinal canal is the ligamentum teres uteri (LTU; not the spermatic cord), which is tightly adhered to the peritoneum, making deperitonealization difficult to achieve during surgery[3,4]. At present, the LTU is usually ligated together with the hernial sac, which may cause LTU ligation-associated complications in some female children[5]. More and more scholars argue that the LTU should be separated and protected intraoperatively with the role and function of the LTU being discovered. However, research is currently limited, and relevant clinical guidelines remain unavailable on whether to preserve and protect the LTU both domestically and internationally[6,7]. Therefore, routinely separating the LTU intraoperatively remains an unresolved issue for female children undergoing surgery for IIH[8]. This study aims to address this problem and further expounds on the significance and necessity of LTU preservation by confirming the safety and short-term efficacy of intraoperative LTU preservation in treating IIH in children to provide practical evidence for future diagnosis and treatment norms.
The LTU, which is one of the major uterine ligaments, plays an important role in maintaining uterine anteversion[9]. LTU damage will affect its tone, which may cause the loss of forward tension and backward inclination of the uterus, thereby increasing the risk of uterine prolapse in adulthood[10,11]. Additionally, a certain angle is formed between the uterine cavity and the external uterine orifice in the retroversion and retroflection position. The pregnancy product cannot be discharged in time and will remain in the uterine cavity when the uterus is rhythmically contracted due to medical abortion, causing prolonged bleeding and uterine orifice non-closure, thereby easily causing ascending infection or adhesion and obstruction due to blood reflux into the fallopian tubes to form salpingitis[12,13], which is the main causes of female infertility[14]. Additionally, LTU injury causes partial lymphatic reflux obstruction in the labia majora and the operation area, causing edema of the labia majora and swelling of the operation area in the short-term, in addition to the above-mentioned long-term complications[15]. Therefore, a growing number of scholars prefer to separate the LTU intraoperatively, and strive to reduce LTU damage while preserving its function[16]. However, intraoperative LTU separation may increase the difficulty of the surgeon, prolong the OT, and subsequently exacerbate the perioperative stress response of the child[17].
Therefore, this study aims to further validate and analyze the effects of preserving or ligating the LTU on clinical indicators, such as OT, hospitalization time, blood loss, postoperative recurrence rate, and complication rate, of female children undergoing LHSL for IIH.
This study collected 100 cases of female children with unilateral IIH treated at Zhangzhou Affiliated Hospital of Fujian Medical University from April 2022 to January 2024. Of them, 45 cases in the control group underwent intraoperative LTU ligation, and 55 cases in the experimental group underwent LTU preservation intraoperatively. LHSL of unilateral IIH was performed in both groups.
Inclusion criteria were: (1) Female children under 14 years old; (2) Meeting the diagnostic criteria for unilateral IIH[18]; and (3) Elective operation, with no systemic disease or incarceration of hernia contents.
Exclusion criteria were: (1) Over 14 years old; (2) Bilateral IIH; (3) Previous history of inguinal hernia surgery; or (4) Surgical intolerance caused by other diseases.
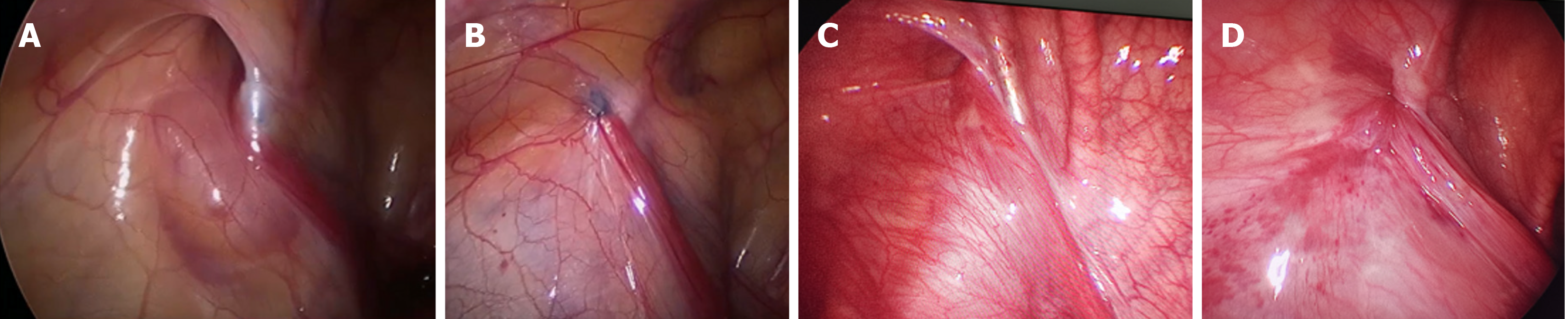
Both groups received endotracheal intubation and intravenous-inhalation anesthesia. The patient was placed in the supine position, with the head low and the feet high. A 3 mm curved incision was then created at the upper edge of the navel as the observation hole A, and a pneumoperitoneum was established with a pressure of 8-12 mmHg (1 mmHg = 0.133 kPa). The closure of bilateral inner ring orifices was found after entering the abdomen. The skin was incised approximately 1 mm at the inner ring orifice surface, and a hernia crochet needle with a silk thread was inserted into the outer peritoneum from the incision [Surgaid Medical (Xiamen) Co., Ltd., Model and specification: ZcA-1.6 × 100]. The inner ring was first half circled from the inside and then poked out under the direct vision of laparoscopy, after which the thread was drawn from the outer half circle around the inner ring. The LTU was stripped from the peritoneum with the hernia needle and passed through the gap between them in the experimental group. Only the hernia sac was ligated at a high position. The peritoneum is lifted by injecting water between the peritoneum and the LTU to increase the space between the two, and the peritoneum is flattened with the help of 3 mm separating forceps to facilitate the separation of the two for patients with difficulty in separating the LTU from the peritoneum. The LTU was not detached in the control group, and the hernia needle passed behind the LTU and was ligated together with the hernia sac (Figure 1).
Surgical indicators: The OT, hospitalization time, and blood loss of the two groups were counted.
Recurrence rate: The recurrence rate of hernia during the six-month follow-up period in the two groups was counted.
Safety: The incidence of complications, such as incision infection, postoperative bleeding, and labia majora edema, in the two groups was analyzed.
The data were processed and statistically analyzed with Statistical Package for the Social Sciences (version 20.0). Quantitative data were presented as the mean ± SD, and independent sample t-tests were conducted to compare means between groups. Counting data were represented by the number of cases (percentage), and χ2 tests were conducted to determine differences. A minimum significance threshold of P values of < 0.05 was utilized.
The control and experimental groups were not markedly different in baseline data, including age, disease course, hernia side, premature infants, and family disease history (P > 0.05; Table 1).
| Indicators | Control group (n = 45) | Experimental group (n = 55) | χ2/t | P value |
| Age (years old) | 5.27 ± 2.24 | 5.56 ± 2.45 | 0.612 | 0.542 |
| Course of disease (months) | 22.38 ± 6.59 | 22.64 ± 5.92 | 0.208 | 0.836 |
| Hernia side | 20/25 | 23/32 | 0.070 | 0.792 |
| Premature baby (yes/no) | 4/41 | 6/49 | 0.112 | 0.738 |
| Family medical history (yes/no) | 6/39 | 12/43 | 1.207 | 0.272 |
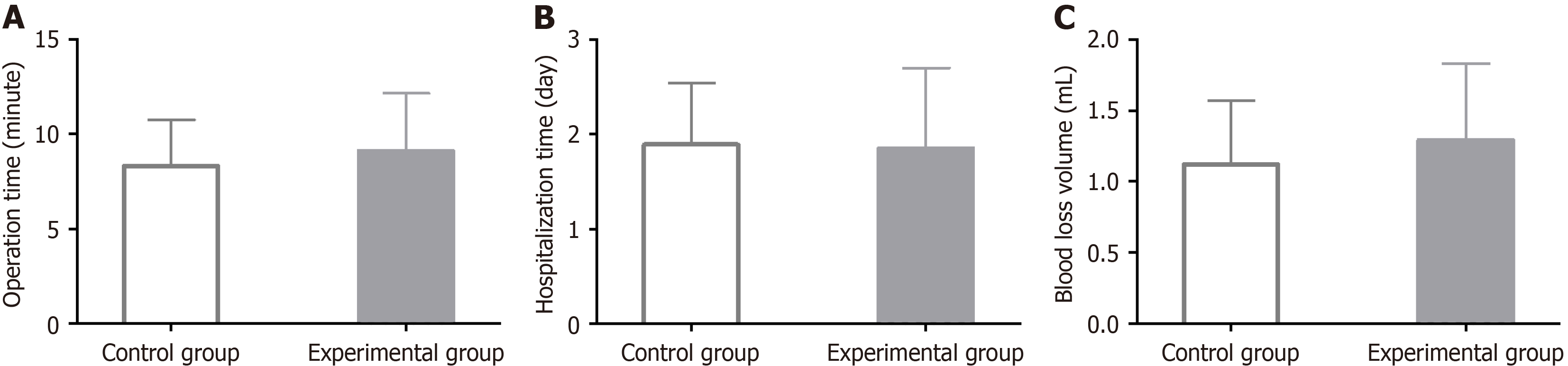
Analysis of surgical indicators, such as OT, hospitalization time, and blood loss volume, revealed no significant inter-group differences in the above surgical indicators between the control and experimental groups (P > 0.05; Figure 2 and Table 2).
| Indicators | Control group (n = 45) | Experimental group (n = 55) | t | P value |
| Operation time | 8.31 ± 2.43 | 9.11 ± 3.03 | 1.433 | 0.155 |
| Hospitalization time | 1.89 ± 0.65 | 1.85 ± 0.85 | 0.260 | 0.796 |
| Blood loss | 1.12 ± 0.45 | 1.29 ± 0.54 | 1.686 | 0.095 |
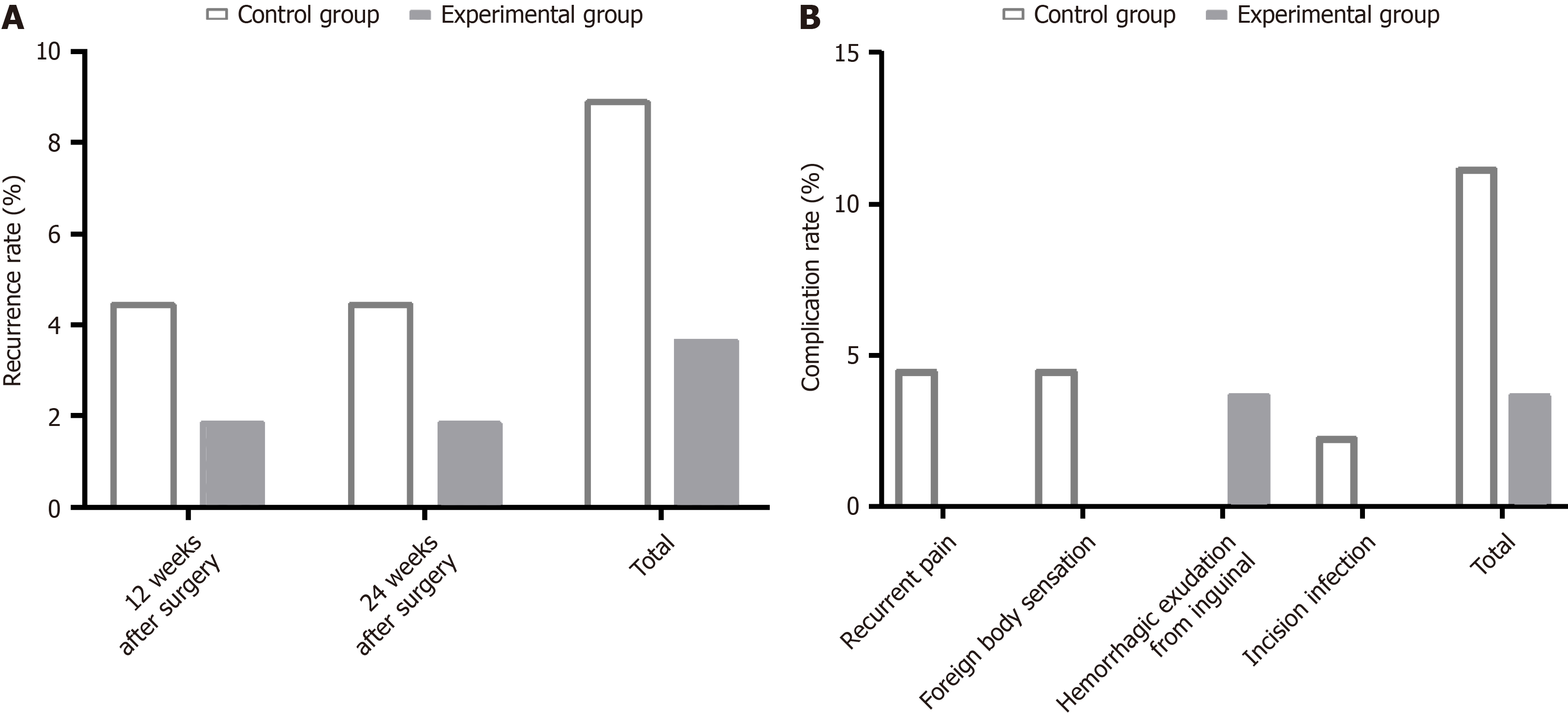
Both groups were successfully followed up for 6 months. The follow-up results indicated no significant difference in the recurrence rate between the two groups at 12 weeks and 24 weeks postoperatively (P > 0.05), nor was there any notable inter-group difference in the total recurrence rate (P > 0.05; Figure 3A and Table 3).
| Indicators | Control group (n = 45) | Experimental group (n = 55) | χ2 | P value |
| 12 weeks after surgery | 2 (4.44) | 1 (1.82) | 0.587 | 0.444 |
| 24 weeks after surgery | 2 (4.44) | 1 (1.82) | 0.587 | 0.444 |
| Total | 4 (8.89) | 2 (3.64) | 1.211 | 0.271 |
The statistics indicated that the two groups were not statistically different in the incidence of complications, including recurrent pain in the inguinal region, foreign body sensation in the inguinal region, bloody exudation at the inguinal incision, and incision infection (P > 0.05; Figure 3B and Table 4).
| Indicators | Control group (n = 45) | Experimental group (n = 55) | χ2 | P value |
| Recurrent pain in the inguinal region | 2 (4.44) | 0 (0.00) | - | - |
| Foreign body sensation in the inguinal region | 2 (4.44) | 0 (0.00) | - | - |
| Bloody exudation at the inguinal incision | 0 (0.00) | 2 (3.64) | - | - |
| Incision infection | 1 (2.22) | 0 (0.00) | - | - |
| Total | 5 (11.11) | 2 (3.64) | 2.124 | 0.145 |
Inguinal hernias in children are primarily related to a non-closure of the vaginal process of the peritoneum after birth, which causes outward protrusion of abdominal contents, mainly manifested as IIH[19,20]. The disease frequently requires surgical intervention and a high requirement for minimally invasive surgical treatment occurs due to the immature development of the child’s organs[21]. The LTU, which is composed of smooth muscle and connective tissue, plays a crucial role in maintaining the normal uterine position[22,23]. The LTU is ligated along with blood vessels, retroperitoneal loose connective tissue, and the hernia sac if not preserved during the LHSL procedure[24,25]. This causes necrosis and tissue absorption outside the hernia sac, thereby loosening the ligature, increasing the risk of IIH recurrence, and to some extent, inducing LTU cysts[26]. The results of this study revealed that the experimental group preserved the LTU, but no significant difference was found in the OT, hospitalization time, and blood loss compared with the control group (P > 0.05), indicating that LTU preservation exhibits certain surgical efficacy and feasibility in LHSL for female children with IIH. The experimental group was not markedly different from the control group in recurrence rates at 12 weeks and 24 weeks postoperatively (P > 0.05), with an equivalent total recurrence rate (P > 0.05), which to some extent helps to reduce the recurrence risk at 12 weeks and 24 weeks postoperatively, and is beneficial to reduce the total recurrence risk (decreased from 8.89% to 3.64%), indicating that LTU retention has a certain preventive effect on reducing the risk of postoperative recurrence. In terms of complications, two cases of bloody exudation at the inguinal incision were reported in the experimental group, whereas not only repeated pain and foreign body sensation in the inguinal region (2 cases each) but also incision infection (1 case) were found in the control group. No statistical inter-group difference was observed in the complication rate (P > 0.05), indicating that LTU preservation is clinically safe. Conversely, LTU preservation involves several precautions in LHSL in female children with IIH. First, the peritoneum of female children is different from that of adults, frequently with good elasticity and tough texture, and surrounds the LTU in an ω-shape, requiring the operator to peel off as gently and accurately as possible to prevent hematoma caused by repeated puncture and injury to blood vessels. Second, the peritoneum should be flattened and kept at a certain tension during the stripping process to prevent incomplete ligation caused by the missed peritoneum on the surface of the LTU. Third, performing the entire knotting process under the supervision of laparoscopy is best to prevent inaccurate ligation. The silk thread is cut after confirming a successful ligation, and the abdominal wall is pulled to bury the knot under the skin to reduce rejection reactions.
Altogether, LTU preservation retains the original physiological function of the LTU without increasing the OT and surgical trauma of children, which is more congruent with the concept of minimally invasive surgery and provides female children with better treatment benefits. The innovation of this study is to confirm the feasibility and necessity of LTU preservation in LHSL for female children with IIH. However, several limitations in this study warrant further investigation and improvement. First, the follow-up time is too short (only 6 months). Thus, longer follow-up to supplement long-term outcomes and reproductive function data in adulthood would help to better understand the potential long-term benefits of LTU preservation during LHSL. Second, a quantitative evaluation of intraoperative stress response, pain, and other indicators is not available. Subsequent statistical analysis should be conducted to compare the clinical effects of the two surgical procedures more comprehensively. Finally, an in-depth analysis of the factors influencing the recurrence of female children with IIH after LHSL was not conducted. Further analysis supplemented with these data will help to further optimize LHSL management. In the future, we will improve this research project based on the above perspectives.
In conclusion, it is not only feasible but also clinically safe for female children with IIH to preserve the LTU during LHSL; thus, LHSL with LTU preservation should be performed when conditions permit. Despite one more operation step, it will not significantly increase the OT, hospitalization time, and bleeding volume, nor will it elevate the risk of recurrence and complications. Our research results provide a deeper experience summary for the safety and short-term efficacy of LTU preservation in LHSL for IIH in female children and offer medical evidence for future diagnosis and treatment norms.
| 1. | Marte A, Caldamone AA, Aguiar LM. The history of the pediatric inguinal hernia repair. J Pediatr Urol. 2021;17:485-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Li J, Bao P, Shao X, Cheng T. The Management of Indirect Inguinal Hernia Sac in Laparoscopic Inguinal Hernia Repair: A Systemic Review of Literature. Surg Laparosc Endosc Percutan Tech. 2021;31:645-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Saguintaah M, Eulliot J, Bertrand M, Prodhomme O, Béchard N, Bolivar-Perrin J, Taleb Arrada I, Simon AH, Baud C, Millet I. Canal of Nuck Abnormalities in Pediatric Female Patients. Radiographics. 2022;42:541-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Wu WT, Chang KV, Lin CP, Yeh CC, Özçakar L. Ultrasound imaging for inguinal hernia: a pictorial review. Ultrasonography. 2022;41:610-623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 5. | Hori T, Yasukawa D. Fascinating history of groin hernias: Comprehensive recognition of anatomy, classic considerations for herniorrhaphy, and current controversies in hernioplasty. World J Methodol. 2021;11:160-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (9)] |
| 6. | Xu M, Huo C, Huang C, Liu Y, Ling X, Xu G, Lin Z, Lu H. Round ligament suspension and vaginal purse-string suture: Newly optimized techniques to prevent tumor spillage in laparoscopic radical trachelectomy for cervical cancer. J Obstet Gynaecol Res. 2022;48:1867-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Meng S, Li Z, Chen L, Yang X, Su P, Wang Y, Yi P. Laparoscopic radical hysterectomy for cervical cancer by pulling the round ligament without a uterine manipulator. Eur J Obstet Gynecol Reprod Biol. 2021;264:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Plumb AA, Rajeswaran G, Abbasi MA, Masci L, Warren O, Wilson J. Contemporary imaging of inguinal hernia and pain. Br J Radiol. 2022;95:20220163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 9. | Chen J, Zhang J, Wang F. A finite element analysis of different postures and intra-abdominal pressures for the uterine ligaments in maintaining the normal position of uterus. Sci Rep. 2023;13:5082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Chen J, Zhang J, Yu C. A 3D finite element model of uterus support to evaluate mechanisms underlying uterine prolapse formation. Comput Methods Biomech Biomed Engin. 2023;26:1930-1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Kakinuma T, Kaneko A, Kakinuma K, Imai K, Takeshima N, Ohwada M. New native tissue repair for pelvic organ prolapse: Medium-term outcomes of laparoscopic vaginal stump-round ligament fixation. World J Clin Cases. 2023;11:3457-3463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | La X, Wang W, Zhang M, Liang L. Definition and Multiple Factors of Recurrent Spontaneous Abortion. Adv Exp Med Biol. 2021;1300:231-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 13. | Zhang Y, Wang Q, Gao CY, Tian HJ, He WJ, Zhang X, Xiong X. Evaluation of the safety and effectiveness of tubal inflammatory drugs in patients with incomplete tubal obstruction after four-dimensional hysterosalpingo-contrast-sonography examination. BMC Pregnancy Childbirth. 2022;22:395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Zhang F, Feng Q, Yang L, Liu X, Su L, Wang C, Yao H, Sun D, Feng Y. Analysis of the etiologies of female infertility in Yunnan minority areas. BMC Womens Health. 2021;21:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Kalafat E, Acar D, Aytac R. Swollen labia majora: An unusual presentation of occult inguinal hernia secondary to ovarian hyperstimulation syndrome. Taiwan J Obstet Gynecol. 2016;55:446-447. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Silveira CAB, de Figueiredo SMP, Rasador ACD, Fernandez MG, Martin RRH, Dias YJM, Lu R. Round ligament management during minimally invasive groin hernia repair in women: a systematic review and meta-analysis. Surg Endosc. 2024;38:1731-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 17. | Zhao B, Dong T, Chen Y, Yang M, Luo Q. Laparoscopic abdominal cerclage during pregnancy: a simplified approach. Am J Obstet Gynecol. 2022;227:333-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Zakaria OM. Patent Contralateral Processus Vaginalis in Infants and Children: Is Herniotomy Justified? Oman Med J. 2018;33:481-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Ohkura T, Kumori K, Kawamura T, Manako J, Ishibashi S, Funabashi N, Tajima Y. Association of pediatric inguinal hernia contents with patient age and sex. Pediatr Int. 2022;64:e15193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Michler V, Elrod J, Wingtes K, Trah J, Reinshagen K, Boettcher M. Should the processus vaginalis sac be opened or closed in pediatric herniotomy? A two-center cohort study. Pediatr Surg Int. 2022;38:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Morini F, Dreuning KMA, Janssen Lok MJH, Wester T, Derikx JPM, Friedmacher F, Miyake H, Zhu H, Pio L, Lacher M, Sgró S, Zani A, Eaton S, van Heurn LWE, Pierro A. Surgical Management of Pediatric Inguinal Hernia: A Systematic Review and Guideline from the European Pediatric Surgeons' Association Evidence and Guideline Committee. Eur J Pediatr Surg. 2022;32:219-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 22. | Tympa A, Grigoriadis C, Terzakis E, Goudeli C, Melemeni A. Leiomyoma of the uterine round ligament: A case report. Exp Ther Med. 2021;22:1285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Xholli A, Londero AP, Scovazzi U, Cagnacci A. Elasticity of the Cervix in Relation to Uterus Position. J Clin Med. 2024;13:2572. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Xu LS, Li Q, Wang Y, Wang JW, Wang S, Wu CW, Cao TT, Xia YB, Huang XX, Xu L. Current status and progress of laparoscopic inguinal hernia repair: A review. Medicine (Baltimore). 2023;102:e34554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 25. | Zhong W, Zhang L, Zhong JQ, He XP, Liu HQ, Zhu WQ, Fang CF. Comparison of outcomes between preservation or division of the uterine round ligament in laparoscopic groin hernia repair in females: a meta-analysis and trial sequential analysis. Hernia. 2024;28:343-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Fan G, Yao G. Analysis of the efficacy of laparoscopic high hernia sac ligation in adolescent indirect hernia. BMC Surg. 2023;23:160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |