Published online Jan 27, 2025. doi: 10.4240/wjgs.v17.i1.97975
Revised: October 27, 2024
Accepted: November 22, 2024
Published online: January 27, 2025
Processing time: 195 Days and 22 Hours
Petersen’s hernia occurring through the epiploic foramen of the greater omentum, is an uncommon type of internal hernia. When it presents with complications such as chylous ascites, which is the lymphatic fluid accumulation in the abdomi
A 62-year-old male patient developed Petersen’s hernia following laparoscopic total gastrectomy (LTG) for gastric cancer, after Roux-en-Y anastomosis. Intestinal torsion and obstruction were experienced by the patient, along with a small amount of chylous ascites. Imaging studies and clinical assessment confirmed the diagnosis. Emergency surgery was performed promptly for the patient in the operating room. The twisted small intestine was reduced and the defect in Petersen’s space was repaired. The procedure was successful in the correction of the intestinal torsion and approximation of the hernia without the need for bowel resection. The patient’s condition significantly improved following the surgery. The ascites evolved from a milky white appearance to a pale yellow, with a substantial decrease in the triglyceride levels in the ascitic fluid, implying a favorable recovery trajectory. The patient was monitored closely and received appropriate care postoperatively, including nutritional support and fluid mana
This report illustrates the significance of recognizing Petersen’s hernia as a potential complication following gastrectomy for gastric cancer. It highlights the fundamental role of early surgical intervention in the effective management of such complications. The favorable outcome in this patient illustrates that prompt and appropriate surgical management can deter the necessity for more extensive procedures such as bowel resection.
Core Tip: This report emphasizes the rare but critical occurrence of Petersen’s hernia complicated by chylous ascites following laparoscopic total gastrectomy and Roux-en-Y anastomosis. The report accentuates the importance of early diagnosis and prompt surgical intervention in managing this condition, significantly improving the outcomes in patients. The significance of recognizing non-specific clinical symptoms and utilization of imaging studies, particularly computed tomography scans, for accurate diagnosis, is underscored. Furthermore, the case and literature review emphasizes the need for heightened clinical vigilance and the development of effective preventive strategies to alleviate this potentially fatal postoperative complication risk.
- Citation: Hu SF, Hao YY, Liu XY, Liu HB. Petersen's hernia with chylous ascites following laparoscopic total gastrectomy and Roux-en-Y anastomosis: A case report and review of literature. World J Gastrointest Surg 2025; 17(1): 97975
- URL: https://www.wjgnet.com/1948-9366/full/v17/i1/97975.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i1.97975
Gastric cancer is a predominant neoplasm, with early diagnosis being critical for the enhancement of the treatment outcomes[1]. A minimally invasive surgical approach, laparoscopic total gastrectomy (LTG), offers quicker recovery postoperatively and superior cosmetic results than traditional open surgeries[2,3]. However, laparoscopic surgery is associated with certain complications, such as internal hernias[4]. A rare and serious internal hernia, Petersen’s hernia, typically occurs during reconstruction surgeries of the digestive tract, particularly in iatrogenic spaces formed between elevated intestinal loops and the transverse colon with the posterior peritoneum[4]. The rate of incidence is relatively low post-gastric cancer surgery; however, can lead to adverse prognoses in male patients because of the acute onset and rapid progression[5]. A 1.61% incidence rate of Petersen’s hernia is indicated from the research data of 2021 following gastric cancer surgery[6]. An actual incidence rate of 0.7% was noted by a 2023 systematic review and meta-analysis in patients undergoing bariatric and upper gastrointestinal surgeries[7]. LTG comprises not only the removal of the stomach and lymph nodes but also Roux-en-Y anastomosis performance to prevent reflux postoperatively[8,9]. Although this reduces recovery and hospital stay times, the risk of complications like Petersen’s hernia may be increased.
Chylous ascites is an infrequently diagnosed disease, characterized by chyle-rich fluid accumulation in the peritoneal cavity, and its exact incidence remains unclear[10]. Approximately one case per 20000 hospitalized patients was indicated by the data from 1984 in the United States, with mortality rates as high as 40%-70%[11]. However, the mortality rate has significantly decreased, with the diversification of treatment modalities and advancements in medical care.
The diagnosis of Petersen’s hernia presents challenges owing to its non-specific clinical symptoms, which may include abdominal pain, nausea, and vomiting[12]. Severe consequences may arise owing to delayed diagnosis and treatment. The simultaneous occurrence of Petersen’s hernia and chylous ascites is exceptionally rare and barely documented in the literature, suggesting underlying complex pathological mechanisms requiring thorough diagnostic and therapeutic approaches by physicians. Through case reporting and literature review, this paper highlights the importance of diagnosing and managing Petersen’s hernia and chylous ascites post-gastric cancer surgery and the critical role of early diagnosis and timely intervention in improving the patient’s prognosis.
Acute abdominal pain, bloating, and nausea persisted for 2 hours.
A 62-year-old male patient reported a history of laparoscopic-assisted total gastrectomy performed for early-stage gastric cancer at the age of 55 years, followed by Roux-en-Y anastomosis. Similar symptoms were experienced by him on three occasions over the past year, diagnosed as incomplete intestinal obstruction and resolved without any surgical inter
Early-stage gastric cancer (stage IB, T2N0M0) with no residual disease at the surgical margins. There was an uneventful postoperative recovery.
The physical examination revealed mild abdominal distension with the upper abdomen tenderness. No rebound ten
The white blood cell and neutrophil counts were elevated (11.6 × 109/L and 10.18 × 109/L, respectively). Other laboratory parameters were within normal limits.
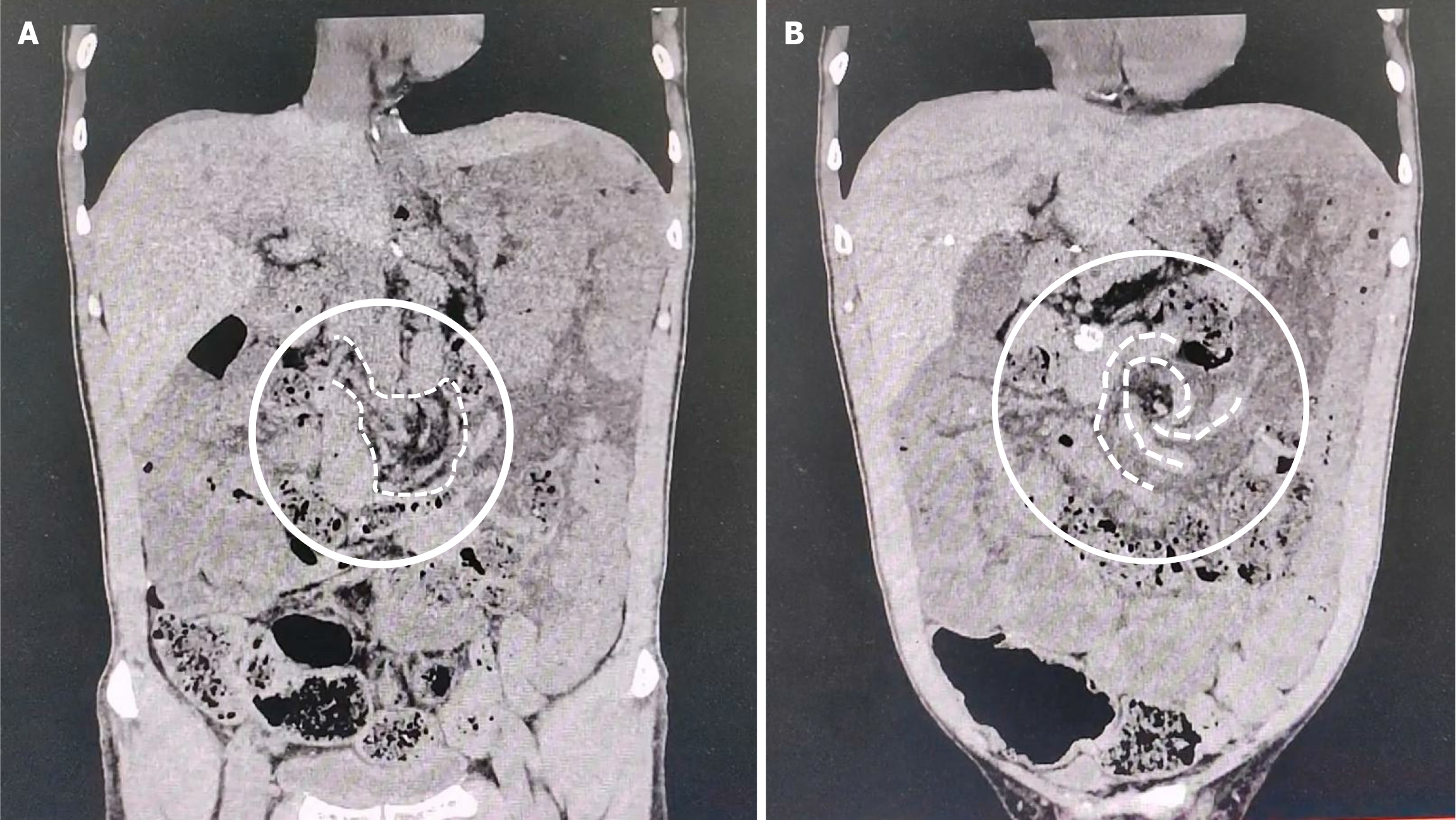
Emergency abdominal computed tomography (CT) scan showed a “spiral” or “whirl” sign, which is characteristic of small bowel torsion. There was the presence of contents, gas, and fluid within the bowel lumen, and fluid in the abdo
Petersen’s hernia, chylous ascites, intestinal obstruction, volvulus, and ascites following endoscopic total gastrectomy and Roux-en-Y anastomosis were noted as the final diagnosis.
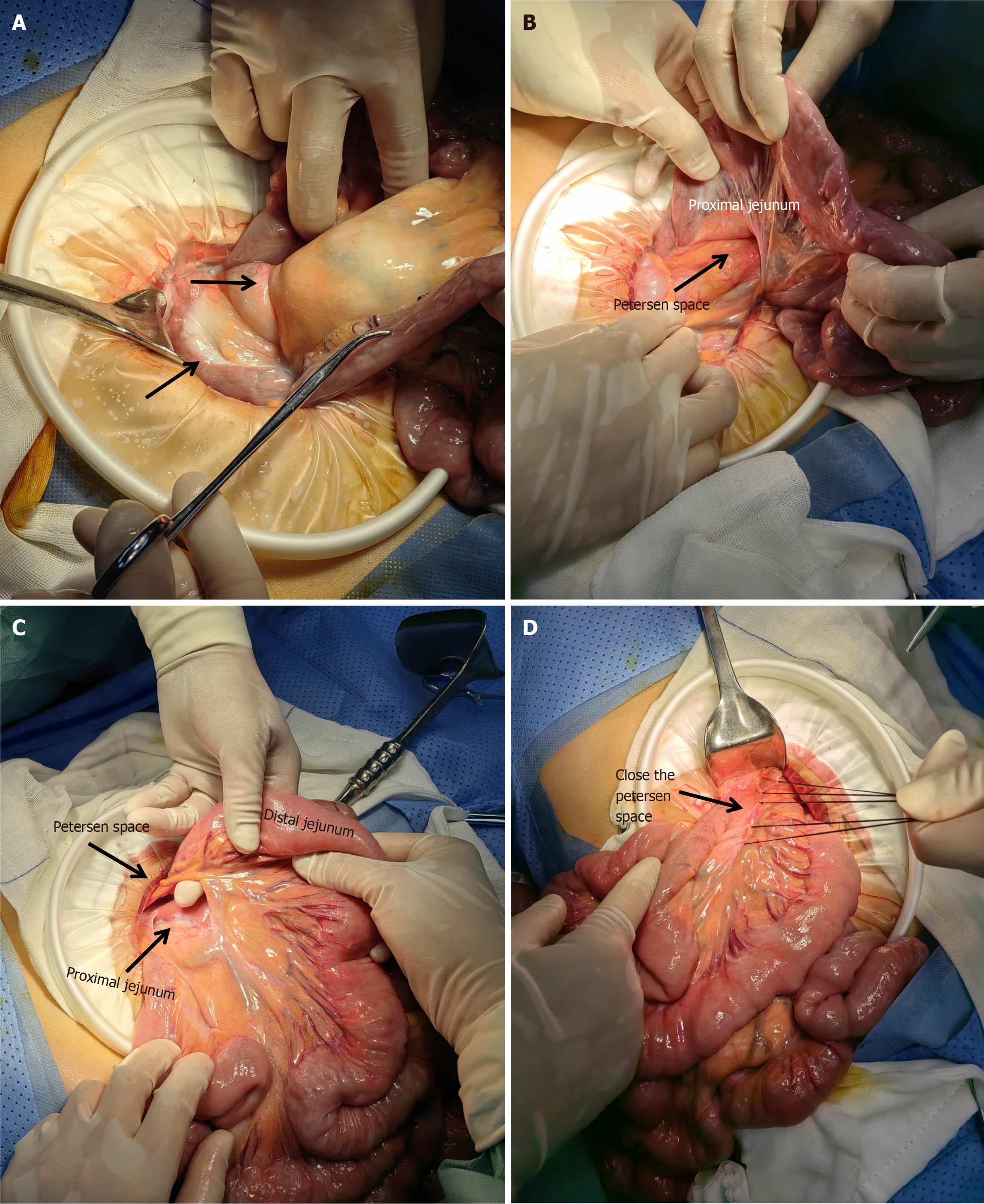
Approximately 50 mL of milky white fluid was detected in the abdomen, with the small intestine herniating through the Petersen defect that was formed after esophagogastric anastomosis. This led to torsion and obstruction that was accom
During the surgery, there was a reduction in the intestinal herniation, and the Petersen defect was intermittently sutured. Since the intestinal segments demonstrated no signs of ischemic necrosis, bowel resection was not performed. The abdominal cavity was thoroughly rinsed, with the placement of a peritoneal drain. The triglyceride (TG) levels in the ascitic fluid were initially high at 310 mg/dL, which subsequently reduced to 16 mg/dL.
The patient had an uneventful postoperative recovery. The color of the ascites and TG levels normalized. There was no requirement for a low-fat diet and the patient was discharged on the fourth postoperative day.
Petersen’s hernia, a specific type of internal hernia, is highly correlated with abdominal surgery, leading to severe clinical consequences[11,12]. For instance, procedures such as Roux-en-Y gastric bypass surgery, radical gastrectomy, gastrec
There are significant variations in the incidence rates of Petersen’s hernia across different surgical types. The rate of incidence of symptomatic Petersen’s hernia is approximately 4.44%, following bariatric surgery, particularly laparoscopic gastrectomy with Roux-en-Y gastric bypass, with most cases diagnosed within 21.3 months postoperatively[20]. In contrast, the incidence rate in patients who undergo post-radical gastrectomy is relatively lower, at approximately 1.61%[11]. Notably, the incidence rate of Petersen’s hernia following LTG is extremely low, that is, less than 0.1%[21]. Although Petersen’s hernia is a rare but potentially fatal complication, these statistical data reveal that its probability of occurrence following gastrointestinal surgery cannot be overlooked.
By altering the abdominal anatomy and increasing abdominal pressure, these surgeries may facilitate the formation of visceral hernias. Although gastrectomy is a major surgical procedure, it does not induce Petersen’s hernia directly. Alternatively, it may be more closely associated with the postoperative restructuring of anatomy[16]. Consequently, total gastrectomy does not have a direct causal relationship with Petersen’s hernia but may be more directly associated with subsequent reconstructive surgeries. Roux-en-Y reconstruction surgery alters the postoperative abdominal anatomy and rearranges the position of visceral organs[22]. Additionally, the application of laparoscopic techniques may assist in reduction of the postoperative intra-abdominal adhesions[12]. Moreover, the changes in postoperative abdominal pressure[13] may also be a contributing factor. The combined effects may lead to the abnormal accumulation of intestinal contents and organ torsion, potentially resulting in internal hernia formation.
The clinical manifestations of Petersen's hernia may include severe abdominal pain and distension, typically caused by mechanical obstruction due to a portion of the small intestine being trapped in the Petersen defect[23]. Vomiting and diarrhea may indicate intestinal dysfunction[24]. When Petersen's hernia progresses to a closed-loop obstruction, symptoms may become more severe, including torsion or ischemia[14]. Imaging studies, particularly CT scans, play a crucial role in the diagnosis and management of Petersen's hernia. CT imaging can reveal features such as rotation of the mesenteric vessels, small bowel dilation, and torsion[24,16]. Abnormal positioning of the small bowel, displacement of the Treitz angle, and the mushroom-like shape of the mesentery are key indicators for the diagnosis of Petersen's hernia following gastric cancer resection[25]. Magnetic resonance imaging is also a useful diagnostic tool in certain situations, such as during pregnancy[18].
Chylous ascites is a rare condition that is characterized by a milky white fluid accumulation in the abdominal cavity, which is rich in TGs, because of the damage to the lymphatic system[26]. This condition may be due to various factors, including surgery, tumors, or infections. It more likely occurs after gastric bypass surgery, where damage to or blockage of the lymphatic vessels can lead to the development of chylous ascites. In addition, chylous ascites may also be asso
This report details a 62-year-old man who experienced three episodes of intestinal obstruction over 6 years following LTG and Roux-en-Y reconstruction. All these episodes were conservatively resolved. Recently, the patient was admitted urgently owing to acute abdominal pain and distension. The development of Petersen’s hernia, in this case, was likely progressive, based on the medical history. Neglecting early symptoms and a lack of timely imaging assessment led to the current emergency. An abdominal CT scan revealed spiral congestion of the mesentery and vessels, small bowel dilation, and peritoneal effusion, indicating small bowel torsion, consistent with the CT characteristics of Petersen’s hernia post-gastric cancer resection. The surgical intervention successfully evaded intestinal necrosis and bowel resection. This case focuses on the importance of early diagnosis and prompt treatment. The patient’s TG level in the ascites was abnormally elevated to 310 mg/dL, confirming chylous ascites, with a TG level above 200 mg/dL being a key diagnostic criterion.
A comprehensive literature review retrieved data from 16 patients with Petersen’s hernia from eight articles. The patient cohort, aged between 53 to 75 years, predominantly comprised men (15 cases) with one woman, with an average age of 63.7 years. The ratio of open surgery to laparoscopic surgery was 11:5, in the initial total gastrectomy. The eso
| Age | Gender | Type of surgery | R-Y approach | Postoperative time (month) | CT findings | Ref. |
| 56 | M | OS, R-Y | Anterior colon | 48 | "Spiral" or "whirl" sign | [32] |
| 72 | M | OS, R-Y | Anterior colon | 6 | "Spiral" or "whirl" sign | [33] |
| 52 | M | OS, R-Y | Anterior colon | 11 | "Spiral" or "whirl" sign | |
| 73 | M | LS, R-Y | Anterior colon | 24 | "Spiral" or "whirl" sign | |
| 54 | M | LS, R-Y | Anterior colon | 26 | "Spiral" or "whirl" sign | |
| 62 | M | OS, R-Y | Anterior colon | 60 | "Spiral" or "whirl" sign | [34] |
| 54 | M | OS, R-Y | Anterior colon | 6 | "Spiral" or "whirl" sign | |
| 69 | M | OS, R-Y | Posterior colon | 24 | "Spiral" or "whirl" sign | [35] |
| 70 | M | OS, R-Y | Anterior colon | - | "Spiral" or "whirl" sign | [36] |
| 50 | M | OS, R-Y | Anterior colon | 18 | "Spiral" or "whirl" sign | |
| 71 | M | LS, R-Y | Anterior colon | 11 | "Spiral" or "whirl" sign | [37] |
| 75 | W | LS, R-Y | Anterior colon | 128 | "Spiral" or "whirl" sign | |
| 66 | M | LS, R-Y | Anterior colon | 0.5 | "Spiral" or "whirl" sign | [38] |
| 71 | M | OS, R-Y | Anterior colon | 24 | "Spiral" or "whirl" sign | [39] |
| 73 | M | OS, R-Y | Anterior colon | 7 | "Spiral" or "whirl" sign | |
| 62 | M | LS, R-Y | Anterior colon | 84 | "Spiral" or "whirl" sign |
| Chylous ascites | Surgical approach | Intestinal management of internal hernia | Close Peterson's defect | From onset to operation time (hour) | Prognosis | Ref. |
| N | OS | IR | Y | 4 | Recovery | [32] |
| N | OS | IR | Y | 30 | Death | [33] |
| N | OS | IR | Y | 150 | Recovery | |
| N | OS | IR | Y | 48 | Recovery | |
| N | OS | IR | Y | 48 | Recovery | |
| N | OS | IR | Y | 31 | Recovery | |
| N | OS | IR | Y | 24 | Recovery | [34] |
| N | OS | IR | Y | 120 | Recovery | |
| Y | LS | IR | Y | 48 | Recovery | [35] |
| N | OS | IR | Y | 24 | Recovery | [36] |
| N | OS | IR | Y | 24 | Recovery | |
| N | LS | IR | Y | - | Recovery | [37] |
| N | LS | IR | Y | - | Recovery | |
| N | OS | IR, IPR | Y | 24 | Recovery | [38] |
| N | OS | IR, IRA | Y | 70 | Death | [39] |
| N | OS | IR, IRA | Y | 22 | Recovery | |
| Y | OS | IR | Y | 4 | Recovery |
Petersen’s hernia is primarily managed through prevention, with specific suturing techniques being paramount. The Mefix method, barbed sutures, and double-row suturing techniques are examples of preventive measures that are more critical than post-event repairs[37,38]. The multicenter trial conducted by Korean scholars showed that the Mefix method is a rapid and straightforward technique for approximating Peterson’s defect, without an increase in postoperative complications when compared to conventional methods[39]. Postoperative regular monitoring[14] is essential for patients with high risk. Furthermore, controlling body mass index can mitigate the impact of obesity on abdominal pressure, thereby reducing the risk of the formation of hernia[11]. Enhancing the sensitivity to symptoms and early diagnostic capabilities for conditions like small bowel torsion or other severe complications caused by Petersen’s hernia is critical for timely surgical intervention to prevent further tissue damage and potentially fatal consequences. Postoperatively, patients should be monitored closely for early detection of the recurrence of hernia or other complications.
Petersen’s hernia is a rare but critical complication, especially after a laparoscopic total gastrectomy. This report empha
| 1. | Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 9898] [Article Influence: 4949.0] [Reference Citation Analysis (2)] |
| 2. | Chen K, Pan Y, Zhai ST, Yu WH, Pan JH, Zhu YP, Chen QL, Wang XF. Totally laparoscopic versus open total gastrectomy for gastric cancer: A case-matched study about short-term outcomes. Medicine (Baltimore). 2017;96:e8061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Wu Q, Wang Y, Peng Q, Bai M, Shang Z, Li L, Tian F, Jing C. Safety and effectiveness of totally laparoscopic total gastrectomy vs laparoscopic-assisted total gastrectomy: a meta-analysis. Int J Surg. 2024;110:1245-1265. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Zhang M, Fan Y, Li J, Yong L. Petersen's hernia after gastric cancer surgery: Unravelling clinical characteristics and optimal management approaches. J Minim Access Surg. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Liu S, Lu XF, Miao J, Tao L, Xia XF, Song P, Wang M, Guan WX. [Clinical characteristics and management of Petersen hernia after gastrectomy in patients with gastric cancer]. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23:1182-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Liu S, Hu Q, Song P, Tao L, Ai S, Miao J, Wang F, Kang X, Shen X, Sun F, Xia X, Wang M, Lu X, Guan W. Risk Factor and Surgical Outcome of Petersen's Hernia After Gastrectomy in Gastric Cancer. Front Oncol. 2021;11:765509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Apostolou KG, Lazaridis II, Kanavidis P, Triantafyllou M, Gkiala A, Alexandrou A, Ntourakis D, Delko T, Schizas D. Incidence and risk factors of symptomatic Petersen's hernias in bariatric and upper gastrointestinal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg. 2023;408:49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 8. | Paluszkiewicz R, Kalinowski P, Wróblewski T, Bartoszewicz Z, Białobrzeska-Paluszkiewicz J, Ziarkiewicz-Wróblewska B, Remiszewski P, Grodzicki M, Krawczyk M. Prospective randomized clinical trial of laparoscopic sleeve gastrectomy versus open Roux-en-Y gastric bypass for the management of patients with morbid obesity. Wideochir Inne Tech Maloinwazyjne. 2012;7:225-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Sun KK, Wu YY. Current status of internal hernia after gastrectomy for gastric cancer. Langenbecks Arch Surg. 2022;407:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Gritsiuta AI, Bracken A, Lara-Gutierrez J, Gilleland WN. Sit-ups and emergency abdominal surgery: a rare case of intestinal volvulus and resultant chylous ascites incited by abdominal exercises. J Surg Case Rep. 2022;2022:rjac155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Sinicropi T, Mazzeo C, Sofia C, Biondo SA, Cucinotta E, Fleres F. Acute Chyloperitoneum with Small Bowel Volvulus: Case Series and Systematic Review of the Literature. J Clin Med. 2024;13:2816. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | El Nogoomi I, Nouh AK, Jaber AA, Toubah AM, Alkaram SS. Petersen's Hernia After Roux-en-Y Gastric Bypass: A Case Report. Cureus. 2023;15:e50757. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Caixeiro L, Varanda J, Morais J, Ferreira A, Rios L. Petersen Hernia After Abdominoplasty: A Provocative Factor or a Coincidence? Cureus. 2023;15:e45014. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Perim CA, Guedes MAE, Carvalho MFCE, Lopes PGF, Simões RL. A simple method for the diagnosis of Petersen’s hernia compromising the biliopancreatic limb. Arq Bras Cir Dig. 2019;32:e1429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Rigney B, Flanagan M, McCullough P, Neary P, Cooke F. Internal hernia through Petersen's defect 13 years post gastrectomy with Roux-en-Y - A Video Vignette. Colorectal Dis. 2022;24:345. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Goh YL, Haworth A, Wilson J, Magee CJ. Life-threatening Petersen's hernia following open Beger's procedure. J Surg Case Rep. 2016;2016:rjw036. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Mahawar KK. Petersen's Hernia may be Commoner After OAGB/MGB Than Previously Reported. Obes Surg. 2018;28:257-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Goldenshluger M, Goitein D, Segal G, Apter S, Mor E, Klang E. Petersen Hernia in Pregnancy: A Report of Two Cases and Their Radiologic Findings. Isr Med Assoc J. 2018;20:588-589. [PubMed] |
| 19. | Kim H, Chung YE, Hyung WJ, Lim JS. Petersen's Hernia after Subtotal Gastrectomy with Billroth II Gastrojejunostomy for Gastric Cancer: A Specific CT Finding. J Korean Soc Radiol. 2018;79:88. [DOI] [Full Text] |
| 20. | Stenberg E, Ottosson J, Magnuson A, Szabo E, Wallén S, Näslund E, Thorell A, Näslund I. Long-term Safety and Efficacy of Closure of Mesenteric Defects in Laparoscopic Gastric Bypass Surgery: A Randomized Clinical Trial. JAMA Surg. 2023;158:709-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 21. | Ng ZQ, Low W, Subramanian P, Stein J. Dual incarcerated internal hernias after laparoscopic total gastrectomy with Roux-en-Y reconstruction for gastric cancer. BMJ Case Rep. 2017;2017:bcr2017219290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 22. | Day M, Duke D. Petersen's Hernia Complicating Pregnancy after Laparoscopic Roux-en-Y Gastric Bypass. The American Surgeon™. 2019;85:403-404. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Santos DC, Viveiros O, Gameiro H, Pereira J. Petersen's hernia after gastric bypass for morbid obesity: a diagnostic challenge. Adv Obes Weight Manag Control. 2019;9:173-174. [DOI] [Full Text] |
| 24. | Abraham V, Dsouza R, Suraj S. Petersen's space hernia - An expanding diagnosis after bariatric surgery: A case report and review of literature. Curr Med Issues. 2020;18:59. [DOI] [Full Text] |
| 25. | Navarro-Sánchez A, López-Fernández J, Hernández-Hernández JR. Left lobe of liver in a Morgagni's hernia. ANZ J Surg. 2019;89:257-258. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Leibovitch I, Mor Y, Golomb J, Ramon J. The diagnosis and management of postoperative chylous ascites. J Urol. 2002;167:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 174] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 28. | Morosin T, De Robles MS. Chylous ascites as a marker for intestinal viability in a small bowel obstruction: a case report. J Surg Case Rep. 2021;2021:rjab411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 29. | Athanasiadis DI, Carr RA, Painter R, Selzer D, Lee NK, Banerjee A, Stefanidis D, Choi JN. Chylous ascites in the setting of internal hernia: a reassuring sign. Surg Endosc. 2022;36:2570-2573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | Hayama T, Shioya T, Hankyo M, Shimizu T, Shibuya H, Komine O, Watanabe Y, Nanbu K, Yamada T. Primary Volvulus of the Small Intestine Exhibiting Chylous Ascites: A Case Report. J Nippon Med Sch. 2017;84:83-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Imam A, Khalayleh H, Rahat M, Mavor E, Pines G, Sapojnikov S. Chylous Ascites Following Bariatric Surgery Report of Two Cases. J Metab Bariatr Surg. 2019;8:22. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Peng J, Tian JZ, Li GY, Ji EM, Xu JG. A [Case of Petersen's Hernia After Gastrectomy for Gastric Cancer]. Anhui Yixue. 2020;41:1244-1245. [DOI] [Full Text] |
| 33. | Liu WZ. [Clinical Characteristics Analysis of Petersen Hernia After Gastrectomy for Gastric Cancer]. Henan Yixue Yanjiu. 2021;30:3698-3702. [DOI] [Full Text] |
| 34. | Koyama R, Maeda Y, Minagawa N, Shinohara T, Hamada T. Chylous Ascites Accompanying Internal Hernia after Total Gastrectomy with Roux-en-Y Reconstruction. Case Rep Gastroenterol. 2019;13:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Baba A, Yamazoe S, Dogru M, Okuyama Y, Mogami T, Kobashi Y, Nozawa Y, Aoyagi Y, Fujisaki H, Ogura M, Matsui J. Petersen hernia after open gastrectomy with Roux-en-Y reconstruction: a report of two cases and literature review. Springerplus. 2015;4:753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 36. | Ojima T, Nakamori M, Nakamura M, Katsuda M, Hayata K, Kato T, Tsuji T, Yamaue H. Internal Hernia After Laparoscopic Total Gastrectomy for Gastric Cancer. Surg Laparosc Endosc Percutan Tech. 2017;27:470-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 37. | Hara K, Hayashi T, Nakazono M, Nagasawa S, Shimoda Y, Kumazu Y, Yamada T, Yamamoto N, Shiozawa M, Morinaga S, Yoshikawa T, Rino Y, Masuda M, Ogata T, Oshima T. An easy and reliable method to close Petersen's defect using barbed suture to prevent internal hernia from developing after gastrectomy with Roux-en-Y reconstruction. Asian J Endosc Surg. 2020;13:238-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Min JS, Jeong SH, Park JH, Kim TH, Hong SC, Jung EJ, Ju YT, Jeong CY, Lee JK, Park M, Lee YJ. Prevention of Petersen's hernia using jejunal mesentery fixing (Mefix). Minim Invasive Ther Allied Technol. 2022;31:580-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 39. | Park JK, Kim DH, Jeon TY, Jeong SH, Kim TH, Min JS, Kim RB, Lee YJ, Park JH, Son YG, Yoon KY, Seo KW, Kim KH, Kim Y, Chae HD, Hwang SH, Lee SH, Chung JH, Kim HI, Park DJ, Kim KH, Seo SH, Oh SJ, Lee WY, In Choi C. Comparison between the mesenteric fixation method (MEFIX) and conventional methods at preventing the occurrence of Petersen's hernia: a study protocol for a multicenter randomized controlled trial. Trials. 2024;25:7. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |