Published online Jan 27, 2025. doi: 10.4240/wjgs.v17.i1.100544
Revised: November 12, 2024
Accepted: November 29, 2024
Published online: January 27, 2025
Processing time: 79 Days and 5 Hours
Intrahepatic and extrahepatic bile duct stones (BDSs) have a high rate of residual stones, a high risk of recurrence, and a high rate of reoperation. It is very im
To analyze the efficacy, postoperative rehabilitation, and quality of life (QoL) of patients with intra- and extrahepatic BDSs treated with endoscopic retrograde cholangiopancreatography (ERCP) + endoscopic papillary balloon dilation (EPBD) + laparoscopic hepatectomy (LH).
This study selected 114 cases of intra- and extrahepatic BDSs from April 2021 to April 2024, consisting of 55 cases in the control group receiving laparoscopic common bile duct exploration and LH and 59 cases in the observation group treated with ERCP + EPBD + LH. Efficacy, surgical indicators [operation time (OT) and intraoperative blood loss (IBL)], postoperative rehabilitation (time for body temperature to return to normal, time for pain relief, and time for drainage to reduce jaundice), hospital stay, medical expenses, and QoL [Gastrointestinal Quality of Life Index (GIQLI)] were comparatively analyzed. Further, Logistic regression analysis was conducted to analyze factors influencing the QoL of patients with intra- and extrahepatic BDSs.
The data demonstrated a higher overall effective rate in the observation group compared to the control group (P = 0.011), together with notably reduced OT, less IBL, shorter body temperature recovery time, pain relief time, time for drainage to reduce jaundice, and hospital stay (all P < 0.05). The postoperative GIQLI of the observation group was more significantly increased compared to the control group (P < 0.05). The two groups demonstrated no marked difference in medical expenses (P > 0.05).
The above indicates that ERCP + EPBD + LH is effective in treating patients with intra- and extrahepatic BDSs, which is conducive to postoperative rehabilitation and QoL improvement, with promising prospects for clinical promotion.
Core Tip: Failure to receive timely and effective surgical intervention may cause massive invasion of the biliary tract by infectious substances in patients with both intra- and extrahepatic bile duct stones (BDSs), subsequently inducing obstructive suppurative cholangitis and liver abscesses, thereby posing a severe threat to life and health. This study analyzed the efficacy, surgical parameters, postoperative rehabilitation, hospital stay, medical expenses, and quality of life (QoL) of patients with intra- and extrahepatic BDSs treated with endoscopic retrograde cholangiopancreatography (ERCP) + endoscopic papillary balloon dilation (EPBD) + laparoscopic hepatectomy (LH). The ERCP + EPBD + LH approach has been confirmed to exhibit a remarkable therapeutic effect in patients with intra- and extrahepatic BDSs, facilitating postoperative recovery and improving the QoL, thereby meriting clinical application and popularization.
- Citation: Chen ZL, Fu H. Endoscopic retrograde cholangiopancreatography, endoscopic papillary balloon dilation, and laparoscopic hepatectomy for intra- and extrahepatic bile duct stones. World J Gastrointest Surg 2025; 17(1): 100544
- URL: https://www.wjgnet.com/1948-9366/full/v17/i1/100544.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i1.100544
Bile duct stones (BDSs) are a kind of calculous disease occurring in the hepatobiliary system with a complicated etiology, which is closely associated with factors, including cholestasis, bile duct infection, stenosis or obstruction, and the presence of foreign bodies in the bile duct[1,2]. Statistics reported that patients with the disease exhibit a risk of approximately 15% of developing gallbladder stones, which is not only unfavorable for improving the condition, but also increases treatment burden and difficulty[3]. Based on the different stone locations, BDSs are classified into either intrahepatic or extrahepatic[4]. Intra- and extrahepatic BDSs are characterized by clustering and sporadicity, which are prone to causing hepatobiliary stricture, bile duct obstruction, and recurrent cholangitis in the body, thereby inducing clinical discomforts, including fever and abdominal pain[5]. Additionally, intra- and extrahepatic BDSs are associated with a high stone residual rate, an increased risk of recurrence, and a relatively high reoperation rate[6]. Untimely and ineffective surgical intervention for such patients may cause infectious substances to wantonly invade the biliary tract of the body, inducing obstructive suppurative cholangitis and liver abscess in the body, which is severely life-threatening[7,8].
Traditional or conservative therapeutic approaches, such as anti-inflammatory agents and liver protection, are used for treating intrahepatic concurrent with extrahepatic BDSs. However, their efficacy is restricted, and the therapeutic outcomes of surgical treatment are suboptimal, accompanied by a certain risk of postoperative complications[9,10]. Consequently, the treatment for patients with intrahepatic combined with extrahepatic BDSs still requires continuous investigation for further optimization. In this study, we aimed to compare the clinical effects of laparoscopic common bile duct exploration (LCBDE) + laparoscopic hepatectomy (LH) with endoscopic retrograde cholangiopancreatography (ERCP) + endoscopic papillary balloon dilation (EPBD) + LH in patients with intra- and extrahepatic BDSs. LCBDE + LH exhibited a certain effect on stone removal, but it may cause substantial trauma and considerable intraoperative blood loss (IBL) in the body, thereby potentially escalating the risk of postoperative complications[11]. ERCP + EPBD + LH represents an efficacious and clinically secure surgical treatment modality for managing complex BDSs, boasting clinical advantages, such as rapid recovery and a low risk of postoperative complications[12,13].
At present, related studies on the analysis of the efficacy, postoperative rehabilitation, and quality of life (QoL) of patients with intra- and extrahepatic BDSs treated by LCBDE + LH and ERCP + EPBD + LH are relatively few; this study will help fill the gap in this respect.
This retrospective study selected 114 patients with intra- and extrahepatic BDSs from April 2021 to April 2024, consisting of 55 cases in the control group receiving LCBDE + LH and 59 cases in the observation group receiving ERCP + EPBD + LH.
Inclusion criteria were meeting the diagnostic criteria for intra- and extrahepatic BDSs[14]; the presence of both intra- and extrahepatic BDSs; receiving treatment for the first time; no surgical contraindications; age of ≥ 18 years; intact case data.
Exclusion criteria were the presence of other hepatobiliary diseases, such as intra- and extrahepatic bile duct stenosis and suppurative cholangitis; a history of upper abdominal surgery; patients during pregnancy or lactation; malignancies; serious cardiovascular or respiratory diseases; previous bile duct-jejunum anastomosis and hepatic cross-section choledochoscopy procedures; mental illness or cognitive impairment.
The observation group received ERCP + EPBD + LH. The patient was required to fast for 8 hours preoperatively and was intramuscularly injected with diazepam of 10 mg 30 minutes pre-procedure. Additionally, the patient was continuously anesthetized with propofol via an intravenous pump. The patient was then placed in the left lateral decubitus position, and ERCP was conducted to determine the specific location, volume, size, and number of the lesions and stones in the bile duct system. The imaging characteristics of the common bile duct and the duodenal papilla area were understood after investigating the common bile duct and the major papilla through the zebra guidewire and entering the interior of the duodenal cavity, and the location of the stone was further confirmed. Subsequently, a balloon dilator with an 8-mm diameter was introduced, ensuring that the middle of the balloon was located within the narrow area of the papilla. The pressure was gradually elevated, and the sphincter of the duodenal papilla was dilated under direct vision. The maximum pressure level was 8 atm, which was maintained for approximately 3 minutes. It was expanded for 2 minutes after an interval of 0.5 minute to fully dilate the duodenal papillary sphincter. The balloon was expanded to 6-20 mm according to stone conditions, and the stones were then removed with a stone extractor. LH was performed 1-2 days after the complete common BDS removal.
The control group received LBDE + LH. The patient was placed in a supine position with separated legs. The surgeon stood between the patient's legs, and the assistants stood on both sides of the patient. The five-port method was utilized for the operation. The ligamentum teres hepatis and falciform ligament were sequentially disconnected with an ultrasonic scalpel or coagulating and dissecting electrode to expose the hepatic vein. The left coronary ligament and left triangular ligament were then severed, and the hepatogastric ligament was cut close to the liver surface to complete left hepatic perihepatic ligament dissociation. The left branch of the hepatic artery was then separated, the blood vessel was clamped and disconnected with a vascular clip, and the left branch of the portal vein was separated near the ligamentum teres hepatis fissure, followed by ligation and blocking with silk thread or clamping and vascular clip disconnection. The left hepatic duct was determined and exposed without sufficient anatomical dissociation. An ischemic demarcation line could be seen on the liver surface after left hepatic pedicle vessel ligation or disconnection. The pre-incision line was marked with an electric scalpel and the liver capsule was incised along the ischemic demarcation line on the liver surface or slightly to the left. Subsequently, the liver parenchyma was cut from the lower edge of the liver with an ultrasonic scalpel, and the liver parenchyma was severed along the pre-incision line until the first hepatic port. The liver tissue around the hepatic portal was continuously separated, thereby fully exposing the left hepatic pedicle, including the left hepatic duct. The liver parenchyma was continuously disconnected along the running of the middle hepatic vein, paying attention to the identification and protection of the middle hepatic vein trunk. Each branch of the middle hepatic vein was carefully separated. Among them, the branches with a > 3 mm diameter could be clamped and disconnected with vascular clips. The remaining liver tissue along with the left hepatic vein was closed and severed with a stapler when the liver parenchyma was severed to the root of the left hepatic vein. Preoperative biliary drainage (percutaneous transhepatic biliary drainage or endoscopic nasobiliary drainage) and intraoperative T-tube drainage were performed as required.
Efficacy: The criteria for clinical therapeutic effect determination include the following: Cured indicates that the gallstone symptoms, such as abdominal pain, have completely or basically disappeared, the postoperative examination reveals no stone lesion residue, and disease recurrence is absent within half a year postoperatively; effective denotes a significant reduction in gallstone symptoms, including abdominal pain, a slight stone lesion residue in the postoperative examination, and no disease recurrence within half a year postoperatively; ineffective represents no alleviation of gallstone symptoms, such as abdominal pain, a large stone lesion residue in the postoperative examination, and disease recurrence within half a year postoperatively. The total effective rate is the percentage of the sum of the number of cured cases and number of effective patients in the total number of cases.
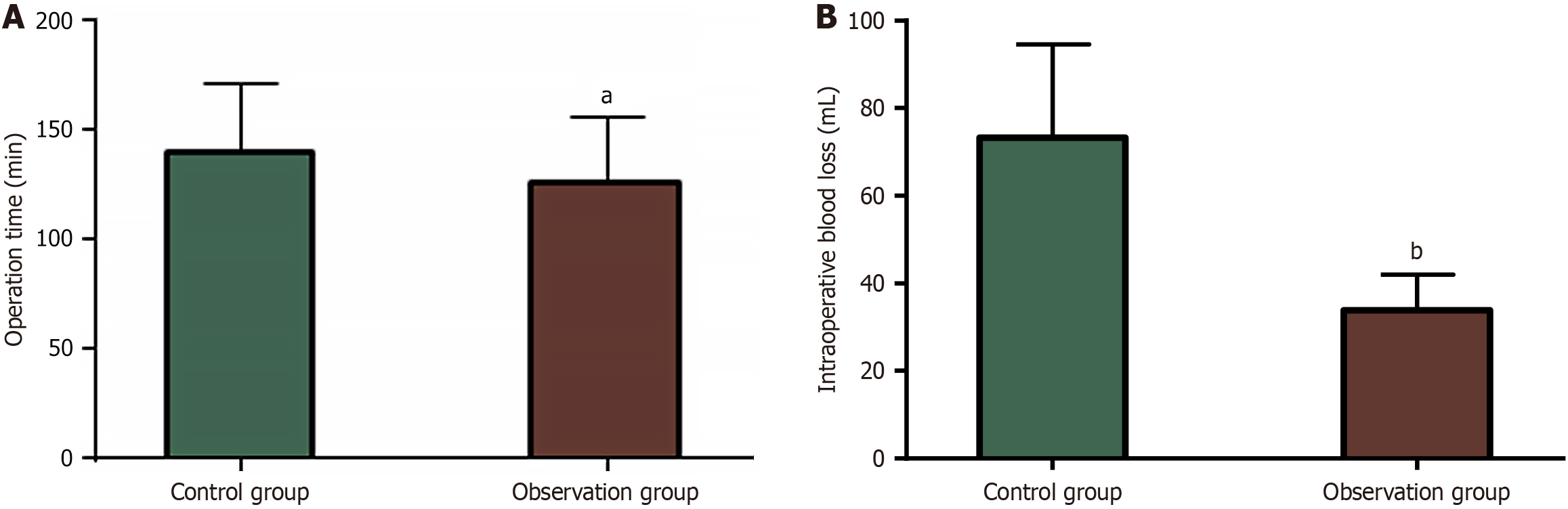
Surgical indicators: The operation time (OT) and IBL of the two groups were documented and compared.
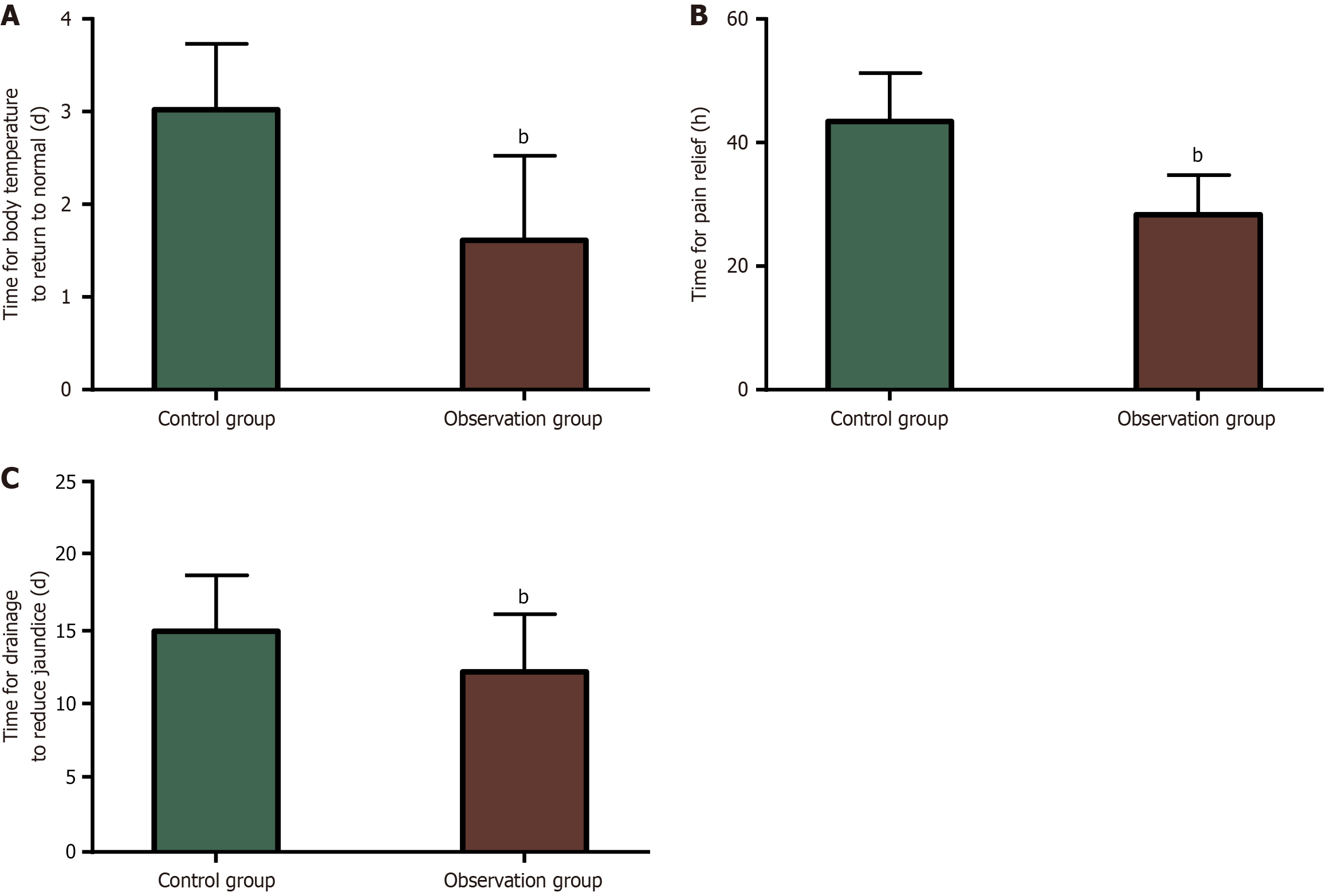
Postoperative rehabilitation: The time for postoperative body temperature to return to normal, the time for pain relief, and the time for drainage to reduce jaundice were assessed and recorded.
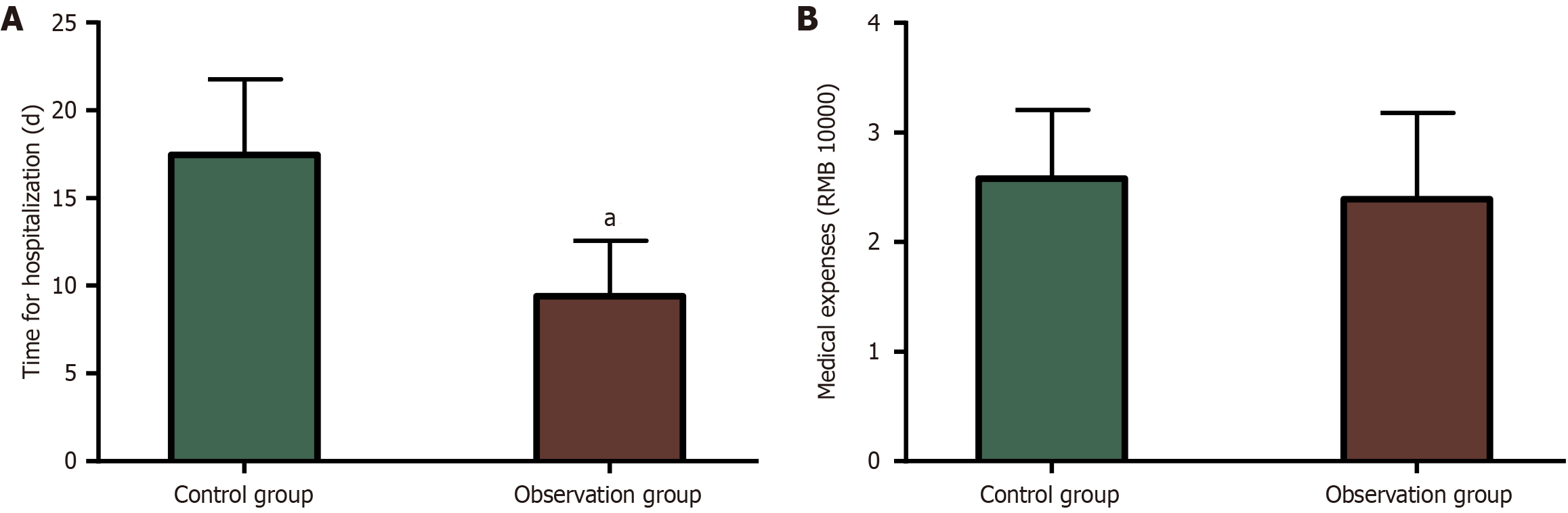
Hospital stays and medical expenses: The length of hospital stay and medical expenses of the two groups were evaluated and recorded.
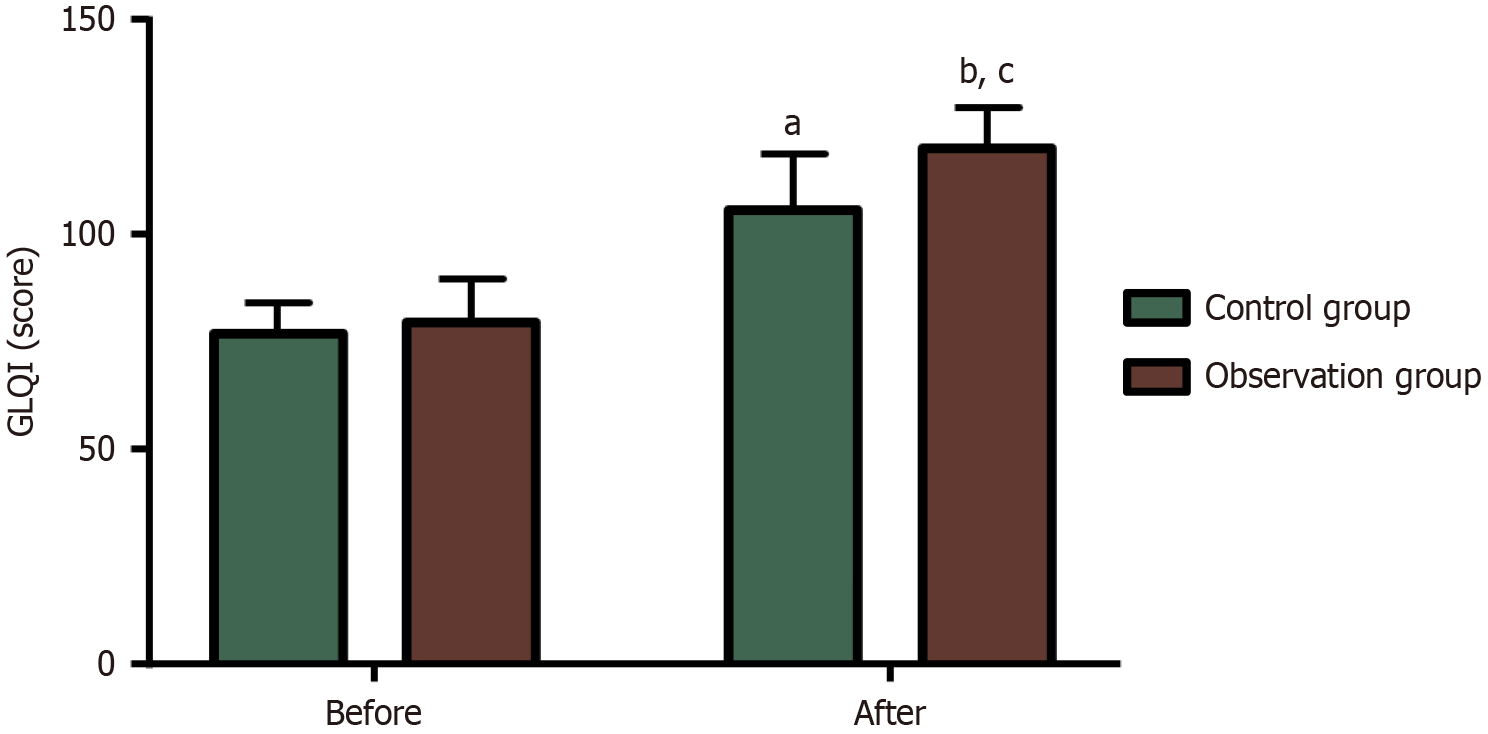
QoL: Patients were scored with the Gastrointestinal Quality of Life Index (GIQLI) for their QoL[15], with a total score of 0-144. The higher the score, the better the QoL.
Statistical Package for the Social Sciences version 20.0 software package was used for statistical analysis. The counting data were presented as n (%). The measurement data were expressed as the mean ± SEM. Among them, the χ2 test was conducted to compare count data. The independent sample t-test was conducted for between-group comparisons and the paired t-test for within-group comparisons before and after treatment for measurement data. A P value of < 0.05 was the statistical threshold.
The control and observation groups demonstrated no statistical differences in gender, age, body weight, disease course, and time from onset to operation (P > 0.05; Table 1).
| Data | Control group (n = 55) | Observation group (n = 59) | χ2/t | P value |
| Sex, n (%) | 0.477 | 0.490 | ||
| Male | 31 (56.36) | 37 (62.71) | ||
| Female | 24 (43.64) | 22 (37.29) | ||
| Age (year) | 64.36 ± 7.08 | 65.46 ± 6.65 | 0.855 | 0.394 |
| Body mass (kg) | 55.91 ± 7.01 | 58.07 ± 8.84 | 1.439 | 0.153 |
| Disease course (year) | 2.82 ± 0.88 | 2.93 ± 1.03 | 0.611 | 0.543 |
| Time from onset to operation (day) | 3.04 ± 0.86 | 3.14 ± 0.99 | 0.574 | 0.567 |
The total effective rate of treatment in the control group was 70.91%, which is significantly lower than 89.83% in the observation group (P < 0.05; Table 2).
| Curative effect | Control group (n = 55) | Observation group (n = 59) | χ2 | P value |
| Cured | 16 (29.09) | 23 (38.98) | ||
| Effective | 23 (41.82) | 30 (50.85) | ||
| Ineffective | 16 (29.09) | 6 (10.17) | ||
| Total effective rate | 39 (70.91) | 53 (89.83) | 6.544 | 0.011 |
The observation group exhibited significantly lower OT (124.53 ± 31.11 minutes vs 137.85 ± 32.59 minutes) and IBL (34.58 ± 8.57 mL vs 73.64 ± 21.20 mL) than the control group (P < 0.05; Figure 1).
The observation group demonstrated statistically better postoperative rehabilitation indicators, such as shorter time for body temperature to return to normal (1.61 ± 0.91 days vs 3.02 ± 0.71 days), less time for pain relief (28.39 ± 6.35 hours vs 43.47 ± 7.81 hours), and reduced time for drainage to reduce jaundice (11.95 ± 4.50 days vs 14.60 ± 4.50 days) than the control group (P < 0.05; Figure 2).
A markedly shorter hospital stay was identified in the observation group vs the control group ((9.41 ± 3.17 days vs 17.47 ± 4.32 days; P < 0.05). Besides, the medical expenses were lower in the observation group (24369.22 ± 6918.09 RMB vs 26006.93 ± 5934.45 RMB), but the difference was not statistically different compared to the control group (P > 0.05; Figure 3).
The QoL levels of the two groups were assessed with the GIQLI. The data demonstrated no significant inter-group difference in the GIQLI score before treatment (79.44 ± 10.22 score vs 77.02 ± 7.02 score; P > 0.05). The GIQLI scores of both groups increased significantly after treatment (P < 0.05), with even higher scores in the observation group (120.12 ± 9.46 score vs 105.78 ± 12.82 score; P < 0.05; Figure 4).
We utilized GIQLI score improvement of 50% as the dependent variable and gender, age, body weight, disease course, time from onset to operation, and treatment method as independent variables to analyze the factors affecting the QoL of patients with intra- and extrahepatic BDSs through Logistic regression analysis. The data indicated that gender, age, body weight, disease course, and time from onset to operation were not risk factors (P > 0.05), but the treatment method was a protective factor affecting the QoL of patients with intra- and extrahepatic BDSs (P < 0.05; Tables 3 and 4).
| Variable | Assignment |
| X1, gender | Female = 0, male = 1 |
| X2, age (year) | < 65 = 0, ≥ 65 = 1 |
| X3, body mass (kg) | < 55 = 0, ≥ 55 = 1 |
| X4, disease course (year) | < 3 = 0, ≥ 3 = 1 |
| X5, time from onset to operation (day) | < 3 = 0, ≥ 3 = 1 |
| X6, treatment method | ERCP + EPBD + LH = 0, LCBDE plus hepatectomy = 1 |
| Variable | β | SE | Wald | P value | Exp (β) | 95%CI |
| Sex | -0.601 | 0.450 | 1.785 | 0.182 | 0.548 | 0.227-1.324 |
| Age (year) | -0.643 | 0.425 | 2.288 | 0.130 | 0.526 | 0.229-1.209 |
| Body mass (kg) | -0.327 | 0.428 | 0.585 | 0.444 | 0.721 | 0.311-1.668 |
| Disease course (year) | -0.055 | 0.447 | 0.015 | 0.902 | 0.946 | 0.394-2.271 |
| Time from disease onset to operation (day) | 0.768 | 0.485 | 2.509 | 0.113 | 2.155 | 0.833-5.572 |
| Therapeutic method | -1.227 | 0.427 | 8.244 | 0.004 | 0.293 | 0.127-0.677 |
This study initially included 114 patients with intra- and extrahepatic BDSs. The control group received LCBDE and hepatectomy, whereas the observation group was treated with ERCP + EPBD + LH. The application efficacy of the two treatments in intra- and extrahepatic BDSs was comparatively analyzed. The observation group demonstrated a statistically higher total effective rate than the control group (89.83% vs 70.91%), indicating that ERCP + EPBD + LH for intra- and extrahepatic BDSs significantly improved overall efficacy. Liu et al[16] revealed that RCP + EPBD + LH is not only suitable for patients with liver stones but also demonstrates certain therapeutic effects for patients with severe comorbidities or unsuccessful endoscopic surgeries. The high therapeutic efficacy of ERCP + EPBD + LH for intra- and extrahepatic BDSs may benefit from the use of double endoscopes to fulfill the requirements of minimally invasive surgical approaches through the natural body cavity, which not only demonstrates a definite therapeutic effect but also provides certain operational convenience[17,18]. Fujisawa et al[19] presently reported that EPBD is beneficial in reducing the risk of ERCP-associated early complications, such as bleeding, biliary tract infection, and perforation, and that adequate intraoperative dilation helps prevent pancreatitis occurrence. The observation group demonstrated significantly lower OT and IBL than the control group, indicating that ERCP + EPBD + LH contributes to significantly shorter OT and lower IBL, with superior surgical outcomes to LCBDE + LH. This may be because ERCP intervention enables clear and visual operation and provides surgeons with relatively comprehensive angiographic images of the biliary tract, which helps shorten the OT[20]. Besides, the function of the Oddi sphincter is partially preserved with EPBD, thereby reducing the risk of blood loss and perforation[21]. A network meta-analysis revealed that EPBD is associated with a lower risk of bleeding than endoscopic sphincterotomy (EST) and EST combined with balloon dilation[22]. The postoperative rehabilitation indicators, such as the time for body temperature to return to normal, the time for pain relief, and the time for drainage to reduce jaundice, were notably shorter in the observation group than in the control group, indicating that undergoing ERCP + EPBD + LH treatment significantly promoted postoperative rehabilitation in patients with intra- and extrahepatic BDSs. Liu et al[23] reported that ERCP + EPBD + LH for patients with intra- and extrahepatic BDSs exhibit advantages, such as less postoperative bleeding, a shorter hospital stay, and a lower additional analgesia rate postoperatively compared to open surgery, which is similar to our results. The observation group demonstrated an advantage in terms of hospital stay compared to the control group, and the medical expenses were relatively lower, indicating that ERCP + EPBD + LH treatment for intra- and extrahepatic BDSs shortened the hospital stay and exhibited a certain cost advantage. Wang et al[24] revealed that ERCP + EPBD + LH treatment for intra- and extrahepatic BDSs not only shortens the hospital stay, OT, and recovery time of gastrointestinal function but also helps reduce IBL and the risk of postoperative complications, supporting our research results. Furthermore, the observation group demonstrated a significantly higher post-treatment GIQLI score than that of pre-treatment and the control group, indicating that ERCP + EPBD + LH intervention in patients with intra- and extrahepatic BDSs significantly improved the QoL level.
The Logistic regression analysis revealed that gender, age, body weight, disease course, and time from onset to operation were not risk factors influencing the QoL of patients with intra- and extrahepatic BDSs, but the treatment method was a protective factor. This further indicates that ERCP + EPBD + LH treatment is beneficial for a significant improvement in the QoL of patients with intra- and extrahepatic BDSs. Lu et al[25] reported that EPBD is a protective factor for cholangitis, stone recurrence, and cholecystitis in patients with BDS, indicating to some extent that EPBD improved patient prognosis by reducing the risk of cholangitis, stone recurrence, and cholecystitis, thereby contributing to QoL enhancement to some extent. This study has several limitations that need to be gradually resolved in subsequent research. First, this study included a relatively small sample size, which to some extent may affect the universality of the research results. Future research is warranted to consider expanding the sample size and conducting multi-center studies to solve the problems that may be caused by the insufficient sample size, thereby improving the extrapolation and reliability of the research results. Second, this study did not conduct molecular-level research regarding the treatment mechanism associated with the surgical procedure. Supplementing this analysis will help to further deepen the understanding of the association between the disease and the treatment, reveal the internal mechanism of the treatment effect at the microscopic level, and provide a more in-depth theoretical basis for clinical treatment. Finally, this study did not include a long-term follow-up analysis. This relationship should be considered in subsequent research. The potential clinical advantages of this therapy for the long-term prognosis of patients can be further analyzed through long-term follow-ups of patients, to more comprehensively assess the treatment effect and long-term safety. In the future, we will gradually improve this study from the above three directions to enhance the research quality and clinical guiding value.
In conclusion, ERCP + EPBD + LH for patients with intra- and extrahepatic BDSs significantly improved efficacy, promoted postoperative rehabilitation, and enhanced QoL, with better surgical effects, lower medical cost, and clinical advantages over LCBDE + LH. Our results provide better options for patients with intra- and extrahepatic BDSs and offer more reliable information for clinical management.
| 1. | Koksal AS, Eminler AT, Parlak E. Fully Covered Metal Stents Safely Facilitate Extraction of Difficult Bile Duct Stones. Surg Laparosc Endosc Percutan Tech. 2023;33:152-161. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Xia H, Zhang H, Xin X, Liang B, Yang T, Liu Y, Wang J, Meng X. Surgical Management of Recurrence of Primary Intrahepatic Bile Duct Stones. Can J Gastroenterol Hepatol. 2023;2023:5158580. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 3. | Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006;20:1075-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 311] [Article Influence: 16.4] [Reference Citation Analysis (1)] |
| 4. | Zhuo H, Chen Z, Lin R, Yang S, Zhuang H, He C, Liu X. Percutaneous Transhepatic Choledochoscopic Lithotomy (PTCSL) is Effective for the Treatment of Intrahepatic and Extrahepatic Choledocholithiasis. Surg Laparosc Endosc Percutan Tech. 2020;31:326-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Yu H, Uyeda JW. Imaging of Acute Hepatobiliary Dysfunction. Radiol Clin North Am. 2020;58:45-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Wen N, Wang Y, Cai Y, Nie G, Yang S, Wang S, Xiong X, Li B, Lu J, Cheng N. Risk factors for recurrent common bile duct stones: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2023;17:937-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Yin Z, Shen B. Comparative study of the effect of U100 laser and pneumatic ballistic combined with percutaneous transhepatic cholangioscopic lithotomy in the treatment of intra-and extrahepatic bile duct stones and its effect on liver function. Pak J Med Sci. 2022;38:1686-1690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Jin P, Jing W, Zhan W, Han C, Si M, Yang J, Li Y, Gu Y, Ma Y, Guo T. Efficacy and safety of laparoscopic holmium laser lithotripsy in the treatment of complicated biliary calculus: A PRISMA-compliant systematic reviews and meta-analysis. Medicine (Baltimore). 2019;98:e14286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Gutt C, Schläfer S, Lammert F. The Treatment of Gallstone Disease. Dtsch Arztebl Int. 2020;117:148-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 10. | Wright M, Chan J, Rudolph R, Haghighi KS. Percutaneous SpyGlass cholangioscopy for treatment of intrahepatic bile duct calculi. ANZ J Surg. 2022;92:1924-1926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Ng HJ, Nassar AHM. Reinterventions following laparoscopic cholecystectomy and bile duct exploration. A review of prospective data from 5740 patients. Surg Endosc. 2022;36:2809-2817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Yang J, Zhang F, Du X, Wang A, Lv S, Fang Z. Laparoscopic hepatectomy combined with endoscopic papillary balloon dilation for complex bile duct stones. ANZ J Surg. 2018;88:E522-E525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Ishii S, Isayama H, Ushio M, Takahashi S, Yamagata W, Takasaki Y, Suzuki A, Ochiai K, Tomishima K, Kanazawa R, Saito H, Fujisawa T, Shiina S. Best Procedure for the Management of Common Bile Duct Stones via the Papilla: Literature Review and Analysis of Procedural Efficacy and Safety. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Jacob JS, Lee ME, Chew EY, Thrift AP, Sealock RJ. Evaluating the Revised American Society for Gastrointestinal Endoscopy Guidelines for Common Bile Duct Stone Diagnosis. Clin Endosc. 2021;54:269-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Fuchs KH, Musial F, Retzbach L, Hann A, Meining A. Quality of life in benign colorectal disease-a review of the assessment with the Gastrointestinal Quality of Life Index (GIQLI). Int J Colorectal Dis. 2023;38:172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 16. | Liu B, Cao PK, Wang YZ, Wang WJ, Tian SL, Hertzanu Y, Li YL. Modified percutaneous transhepatic papillary balloon dilation for patients with refractory hepatolithiasis. World J Gastroenterol. 2020;26:3929-3937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 17. | Almario CV, May FP, Shaheen NJ, Murthy R, Gupta K, Jamil LH, Lo SK, Spiegel BM. Cost Utility of Competing Strategies to Prevent Endoscopic Transmission of Carbapenem-Resistant Enterobacteriaceae. Am J Gastroenterol. 2015;110:1666-1674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Jiang X, Yang G, Wang K, Bi W, Shang D, Zhang G. Clinical Efficacy Analysis of the Combination of the Laparoscope and Preoperative or Intraoperative Duodenoscope in the Treatment of Cholecystolithiasis with Choledocholithiasis: A Retrospective Study. J Laparoendosc Adv Surg Tech A. 2019;29:1539-1543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Fujisawa T, Kagawa K, Hisatomi K, Kubota K, Nakajima A, Matsuhashi N. Is endoscopic papillary balloon dilatation really a risk factor for post-ERCP pancreatitis? World J Gastroenterol. 2016;22:5909-5916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Shen JB, Chen PC, Su JG, Feng QC, Shi PD. Clinical application of ERCP concurrent laparoscopic cholecystectomy in the treatment of cholecystolithiasis complicated with extrahepatic bile duct stones. Heliyon. 2024;10:e31022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Ding J, Li F, Zhu HY, Zhang XW. Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: An anatomic view. World J Gastrointest Endosc. 2015;7:274-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Park CH, Jung JH, Nam E, Kim EH, Kim MG, Kim JH, Park SW. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc. 2018;87:43-57.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 23. | Liu YY, Li TY, Wu SD, Fan Y. The safety and feasibility of laparoscopic approach for the management of intrahepatic and extrahepatic bile duct stones in patients with prior biliary tract surgical interventions. Sci Rep. 2022;12:14487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Wang W, Xia H, Dai B. Comparison of the clinical effects of dual-modality endoscopy and traditional laparotomy for the treatment of intra- and extrahepatic bile duct stones. World J Gastrointest Surg. 2024;16:759-767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 25. | Lu Y, Wu JC, Liu L, Bie LK, Gong B. Short-term and long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Eur J Gastroenterol Hepatol. 2014;26:1367-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |