Published online Sep 27, 2024. doi: 10.4240/wjgs.v16.i9.2870
Revised: June 29, 2024
Accepted: July 31, 2024
Published online: September 27, 2024
Processing time: 122 Days and 11.7 Hours
Transjugular intrahepatic portosystemic shunt (TIPS) is a pivotal intervention for managing esophagogastric variceal bleeding in patients with chronic hepatic schistosomiasis.
To evaluate the efficacy of digital subtraction angiography image overlay tech
We conducted a retrospective analysis of patients who underwent TIPS at our hospital, comparing outcomes between an ultrasound-guided group and a DIT-guided group. Our analysis focused on the duration of the portosystemic shunt puncture, the number of punctures needed, the total surgical time, and various clinical indicators related to the surgery.
The study included 52 patients with esophagogastric varices due to chronic hepatic schistosomiasis. Results demonstrated that the DIT-guided group expe
The use of DIT for guiding TIPS procedures highlights its potential to enhance procedural efficiency and reduce surgical times in the treatment of esophagogastric variceal bleeding in patients with chronic hepatic schistosomiasis.
Core Tip: A comparison of procedural metrics between digital subtraction angiography image overlay technology (DIT)-guided and ultrasound-guided transjugular intrahepatic portosystemic shunt (TIPS). Demonstration of significant reductions in puncture time and surgical duration in the DIT-guided group. Improved clinical indicators post-procedure, including reductions in aspartate aminotransferase, B-type natriuretic peptide, and portal vein pressure in both groups, with additional benefits in total bilirubin and alanine aminotransferase levels in the DIT-guided group. Our research addresses a critical need for efficient and safer TIPS procedures in patients with complex hepatic anatomy due to chronic schistosomiasis, which underscores the potential of DIT as a superior guidance technology, providing a foundation for further advancements in interventional radiology techniques.
- Citation: Li XY, Li Y, Li WQ, Ju S, Dong ZH, Luo JJ. Enhancing transjugular intrahepatic portosystemic shunt procedure efficiency with digital subtraction angiography image overlay technology in esophagogastric variceal bleeding. World J Gastrointest Surg 2024; 16(9): 2870-2877
- URL: https://www.wjgnet.com/1948-9366/full/v16/i9/2870.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i9.2870
Chronic hepatic schistosomiasis is a major global health issue affecting > 240 million individuals worldwide, causing significant morbidity and mortality due to complications including portal hypertension and esophagogastric variceal bleeding (EGVB), which represent life-threatening emergencies. The granulomatous response induced by schistosome eggs is primarily responsible for liver fibrosis in patients with chronic schistosomiasis, subsequently leading to such complications[1,2].
Traditional management of EGVB due to portal hypertension involves a combination of pharmacological therapy and endoscopic techniques aimed at reducing portal vein pressure and controlling haemorrhage. However, these methods are often only temporarily effective and do not address persistent portal hypertension[3].
The transjugular intrahepatic portosystemic shunt (TIPS) is a well-established surgical intervention that establishes a shunt between the portal and hepatic veins to effectively reduce portal vein pressure[3]. Clinical guidelines recommend TIPS as an effective treatment for pulmonary hypertension and EGVB. The success of this procedure relies heavily on a precise portal vein puncture, which is a critical step in TIPS[4]. Accurate localisation of the portal vein before surgery and selection of an appropriate puncture angle can decrease the number of attempts required for puncture, thereby enhancing the success rate of TIPS[5].
There are three commonly used methods for guiding portal vein punctures: Traditional guided procedures; real-time ultrasound-guided procedures; and image fusion technology-guided procedures[5]. Traditionally guided and ultrasound-guided procedures involve percutaneous transhepatic puncture of the portal vein, in which a guide catheter is used to access the portal vein directly under angiographic visualisation. However, these methods increase the complexity of surgery and the risk for extrahepatic puncture, which may result in a higher incidence of complications[6].
Patients with chronic liver schistosomiasis often present with severe liver deformities, making them particularly challenging cases for TIPS due to the altered anatomy. Studies have shown that 90% of patients with chronic hepatic schistosomiasis exhibit severe liver lobe imbalance, characterised by significantly decreased volume in the right lobe and increased volume in the left and caudate lobes[7]. These anatomical alterations significantly increase the potential risk for percutaneous transhepatic puncture of the portal vein, including hepatic artery injury, biliary fistula formation, and non-target organ damage, which may lead to surgical failure and intraperitoneal bleeding[8].
Hepatic artery labelling assisted by digital subtraction angiography (DSA) image overlay technology (DIT-guided TIPS) is a novel procedure. By using the relatively fixed anatomical positions of the hepatic artery and portal vein, a catheter can be inserted into the hepatic artery to guide puncture of the portal vein. DSA overlay technology is an image fusion technology that simultaneously depicts the hepatic artery and its accompanying portal vein. Therefore, DIT is anticipated to be an option for TIPS in patients with chronic hepatic schistosomiasis. The present study reviewed data from 41 cases of DIT-guided TIPS, including treatment experience, safety, efficiency, and prognosis in patients with EGVB and chronic hepatic schistosomiasis.
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Jinshan Hospital, Fudan University (Shanghai, China; No. JIEC 2023-S52). Informed consent was obtained from each participant to ensure adherence to ethical standards and relevant guidelines and regulations.
Data from 52 patients diagnosed with chronic hepatic schistosomiasis, who underwent TIPS between October 2019 and August 2023, we retrospectively analysed. The inclusion criteria were a confirmed history of schistosomiasis, computed tomography (CT) or ultrasound diagnosis of chronic hepatic schistosomiasis, or EGVB caused by portal hypertension. Exclusion criteria were heart failure or cardiac insufficiency, acute liver failure or liver malignancy, systemic infection or inflammation, renal insufficiency, severe pulmonary hypertension, and allergy to contrast agents. Patients were divided into two groups according to TIPS method: Real-time ultrasound-guided (n = 11); and DIT-guided (n = 41).
Pre-and postoperative clinical laboratory parameters (measured within one week after the procedure) included aspartate aminotransferase (AST), alanine aminotransferase (ALT), blood ammonia, B-type natriuretic peptide (BNP), partial prothrombin time, prothrombin time, total bilirubin (TB), creatinine, albumin, and international normalised ratio. The presence of ascites was assessed using ultrasonography or CT. All patients were followed-up for up to 12 months postoperatively to monitor the occurrence of complications such as rebleeding, hepatic encephalopathy, intra-abdominal haemorrhage, and stent dysfunction. Surgical duration (from the start of anaesthesia to completion of the surgical procedure), puncture time (from the first skin puncture to successful portal vein cannulation), and number of puncture attempts were recorded for each patient.
The procedure was performed using an ultrasound system (EPIQ Elite, Philips, Amsterdam, Netherlands). In the ultrasound-guided group, ultrasonography was used to locate the portal vein before the procedure. During the procedure, a 21-gauge puncture needle was used for percutaneous transhepatic puncture of the portal vein under ultrasound guidance. A sheath tube and pigtail catheter were then inserted for portal vein angiography to clarify the pattern of portal vein blood flow and the extent of the oesophageal and gastric varices. Portal vein pressure was measured before and after embolisation of the varices using spring coils and tissue glue.
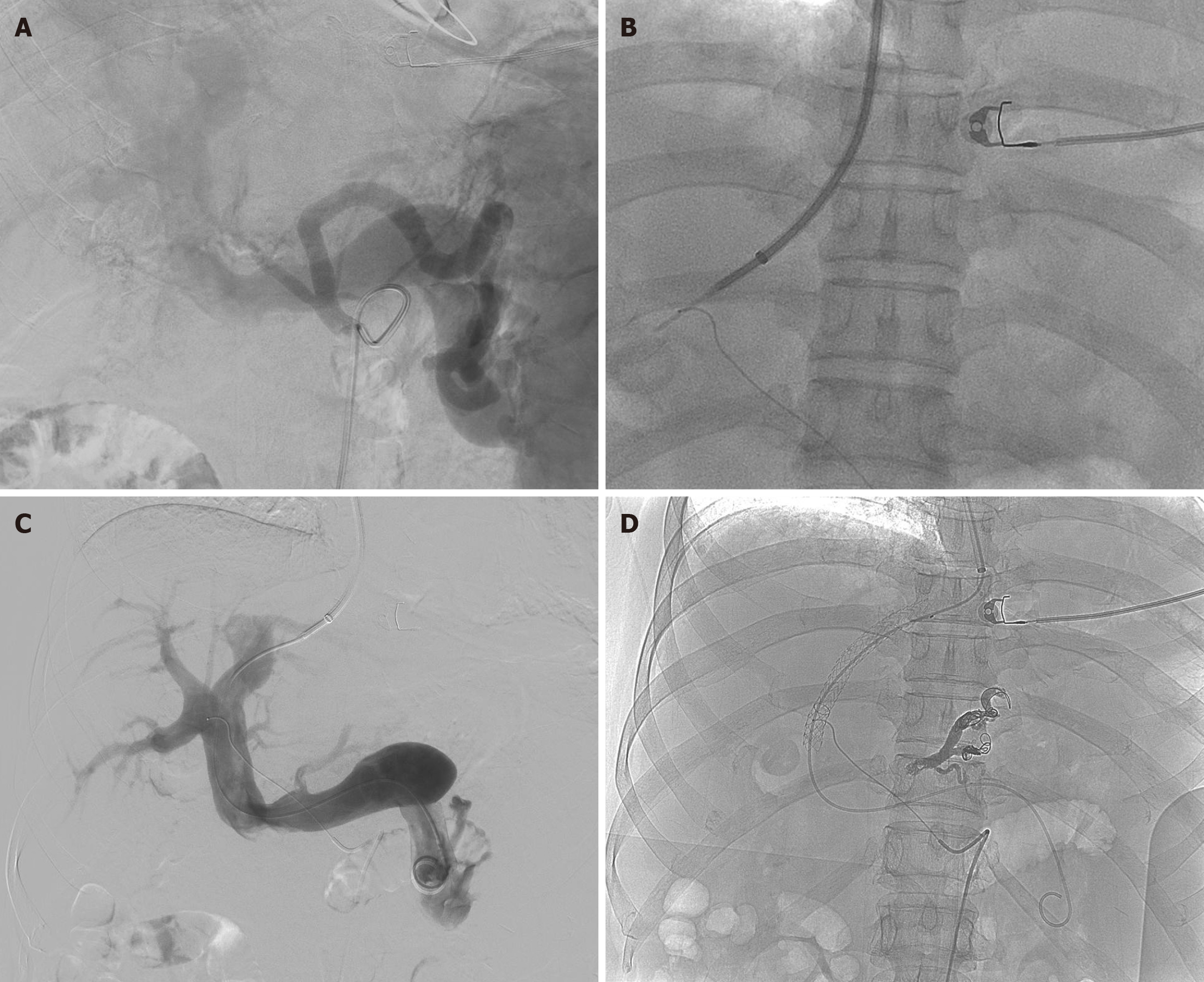
The procedure was performed using DSA (Allura-Xper-FD20, Philips, Amsterdam, Netherlands). For patients in the DIT-guided group, the procedure began with femoral artery puncture. A microcatheter was introduced into the hepatic artery as a guide. DIT was used to simultaneously display the hepatic artery and its accompanying portal vein. The right internal jugular vein was then punctured and a RUPS-100 puncture system (Cook, Bloomington, IL, United States) was introduced to access the portal vein, aiming behind the label placed in the hepatic artery. Following successful puncture, the catheter was advanced into the portal vein to assess blood flow and variceal severity. Portal vein pressure was measured, and the varices were embolised using spring coils and tissue glue. The portosystemic shunt was expanded using an 8 mm diameter balloon, and a covered stent (GORE Viatorr, Gore Medical, Newark, DE, United States) of the same diameter was placed.
Statistical analyses were performed using R version 4.3.0 (R Foundation for Statistical Computing, Vienna, Austria, http://www.Rproject.org). Differences in puncture times, surgical duration, and changes in clinical laboratory indicators before and after surgery were compared between groups. Categorical data are expressed as number and percentage, and were analysed using the Pearson χ2 test. Continuous variables are expressed as mean ± SD and were analysed using the Student’s t-test or Mann–Whitney U test, depending on data distribution (i.e., normal vs non-normal). Differences with P ≤ 0.05 were considered to be statistically significant.
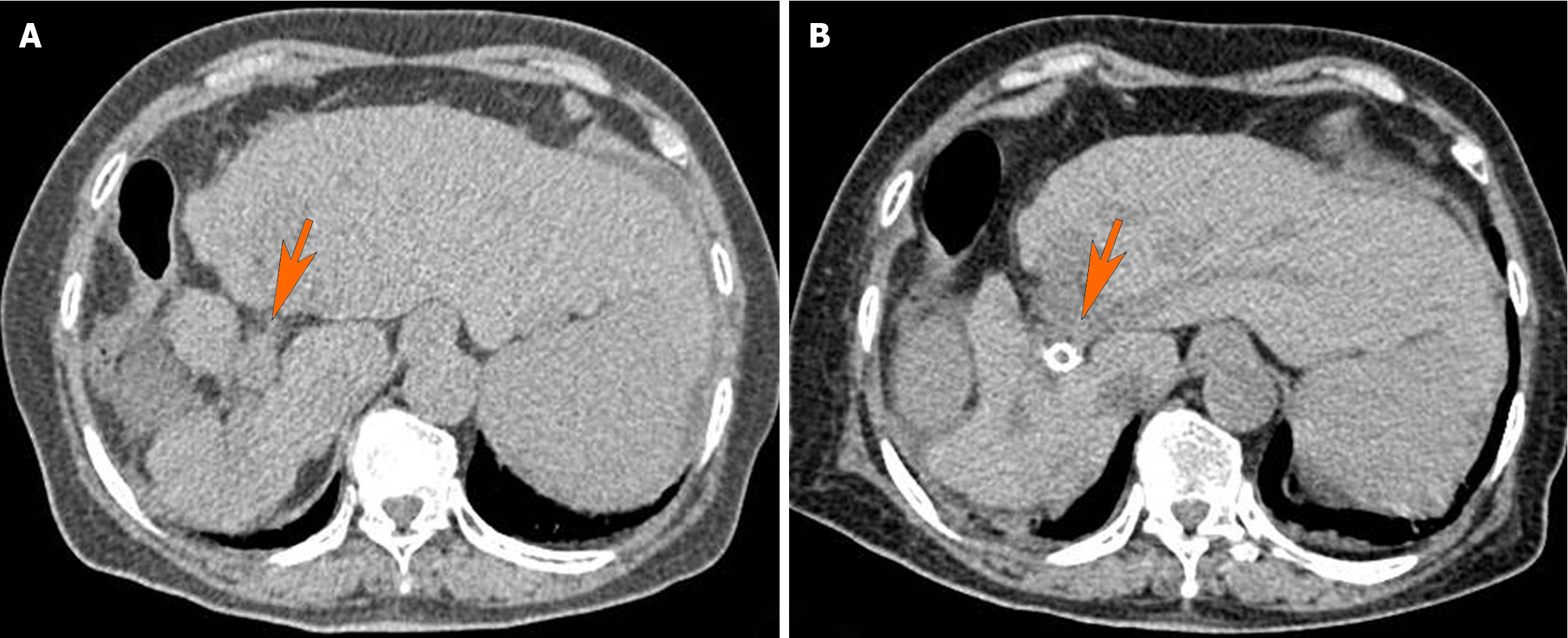
The clinical characteristics of the patients are summarised in Table 1. Preoperative and postoperative liver CT scans, highlighting changes after the TIPS procedure are presented in Figure 1. The study population comprised 52 patients diagnosed with EGVB due to chronic hepatic schistosomiasis. Age distribution among the patients ranged from 32 to 84 years, with a mean (± SD) of 66 ± 11 years, reflecting a diverse cohort in terms of age. In the ultrasound-guided group, there was one male [9.0% (48 years of age)] and 10 females [91.0% (age, 49 to 81 years)], with a mean age of 71 ± 10 years. This demographic profile highlights the predominance of older females. Conversely, the DIT-guided group comprised 19 males (46.3%) and 22 females (53.7%), with ages ranging from 32 to 84 years for males (mean age, 62 ± 15 years) and 46 to 80 years for females (mean age, 70 ± 8 years).
| Ultrasound (n = 11) | DIT (n = 41) | |||||
| Before | After | P value | Before | After | P value | |
| Sex | 0.057 | |||||
| Female | 10 (90.9) | NA | NA | 22 (53.7) | NA | |
| Male | 1 (9.1) | NA | NA | 19 (46.3) | NA | |
| Age (year) | 69 ± 11.7 | NA | NA | 66 ± 12.3 | NA | 0.457 |
| Surgical time (hour) | 2.9 ± 0.8 | NA | NA | 2.2 ± 0.7 | NA | 0.022 |
| Puncture time (minute) | 53 ± 13.7 | NA | NA | 27 ± 14.0 | NA | < 0.001 |
| Puncture times | 1.7 ± 0.7 | NA | NA | 1.2 ± 0.4 | NA | 0.074 |
| ALT (U/L) | 76.1 ± 60.1 | 37.9 ± 21.4 | 0.084 | 135 ± 288 | 28.1 ± 24.5 | 0.023 |
| AST (U/L) | 126 ± 79.3 | 56.0 ± 37.0 | 0.025 | 233 ± 495 | 51.5 ± 36.5 | 0.025 |
| Albumin (g/L) | 31.2 ± 5.0 | 28.5 ± 4.5 | 0.211 | 29.7 ± 5.4 | 29.3 ± 6.0 | 0.803 |
| Ammonia (mol/L) | 56.4 ± 43.0 | 44.3 ± 31.1 | 0.481 | 60.4 ± 52.0 | 64.4 ± 45.0 | 0.713 |
| BNP (pg/L) | 254 ± 217 | 67.1 ± 26.4 | 0.024 | 243 ± 226 | 83.9 ± 77.8 | < 0.001 |
| Creatinine (µmol/L) | 59.5 ± 17.3 | 57.1 ± 15.6 | 0.73 | 69.4 ± 19.3 | 62.3 ± 16.1 | 0.074 |
| Prothrombin time (second) | 16.7 ± 1.9 | 15.7 ± 2.3 | 0.313 | 17.8 ± 3.9 | 17.2 ± 4.3 | 0.576 |
| PPT (second) | 30.4 ± 5.2 | 29.3 ± 3.6 | 0.607 | 31.7 ± 6.6 | 31.1 ± 9.5 | 0.757 |
| PVP (mmHg) | 35.0 ± 7.6 | 19.6 ± 3.3 | < 0.001 | 28.2 ± 7.0 | 19.7 ± 3.2 | < 0.001 |
| INR | 1.5 ± 0.1 | 1.4 ± 0.1 | 0.096 | 1.5 ± 0.1 | 1.5 ± 0.3 | 0.353 |
| TB (μmol/L) | 35.1 ± 17.5 | 23.0 ± 7.93 | 0.069 | 40.0 ± 20.3 | 27.4 ± 12.0 | 0.001 |
| Platelet | 90.6 ± 107 | 115 ± 96.5 | 0.58 | 96.9 ± 70.9 | 101 ± 72.4 | 0.813 |
| Ascites | 1 | 0.356 | ||||
| None | 7 (63.6) | 7 (63.6) | 29 (70.7) | 31 (75.6) | ||
| Mild | 3 (27.3) | 3 (27.3) | 10 (24.4) | 10 (24.4) | ||
| Moderate/severe | 1 (9.1) | 1 (9.1) | 2 (4.9) | 0 (0) | ||
| CTP | 4.9 ± 1.6 | 4.8 ± 1.1 | 0.883 | 4.9 ± 0.8 | 4.8 ± 1.2 | 0.675 |
| MELD | 10.9 ± 1.3 | 9.9 ± 1.8 | 0.154 | 10.6 ± 1.4 | 10.5 ± 2.3 | 0.731 |
Significant improvements were observed in several clinical indicators following these procedures. In the ultrasound-guided group, there were significant reductions in AST and BNP levels, and portal vein pressure preoperatively to postoperatively. The DIT-guided group exhibited even more pronounced reductions, including TB, ALT, AST, and BNP levels, and portal vein pressure decreasing preoperatively to postoperatively.
Comparison of the ultrasound- vs DIT-guided TIPS procedures highlighted significant procedural advantages for the DIT-guided protocol. Notably, the puncture time was reduced, from an average of 53 ± 13.7 minutes in the ultrasound-guided group to 27 ± 14.0 minutes in the DIT-guided group, corresponding to a highly significant reduction (P < 0.001). Similarly, the overall surgical duration decreased from 2.9 ± 0.8 hours to 2.2 ± 0.7 hours (P = 0.022), indicating a more efficient procedure with DIT-guidance. The number of punctures required also tended to be lower in the DIT-guided group, with an average of 1.2 ± 0.4 punctures vs 1.7 ± 0.7 in the ultrasound-guided group, although this difference narrowly failed to reach statistical significance (P = 0.074). The steps involved in the TIPS procedure using DIT tech
During follow-up, both groups exhibited good procedural tolerance and safety. Hepatic encephalopathy was observed in two patients each in the ultrasound-guided and DIT-guided groups. No significant complications, such as intra-abdominal haemorrhage or stent dysfunction, were reported, confirming the clinical safety and feasibility of both ultrasound- and DIT-guided TIPS procedures in this patient population.
This study highlighted the significant enhancements in procedural efficiency and outcomes using DIT-guided TIPS in patients with chronic hepatic schistosomiasis and complications of EGVB. The DIT-guided method notably reduced both puncture and surgical durations compared with the traditional ultrasound-guided approach, which is a critical impro
Schistosomiasis, a neglected tropical disease, affects > 240 million individuals globally, with an additional 779 million at risk for infection. The granulomatous response induced by schistosome eggs is a major cause of hepatic fibrosis in patients with chronic schistosomiasis, leading to portal hypertension and EGVB, which are major causes of morbidity and mortality in these patients[9].
While traditional treatments for EGVB, including pharmacological therapy and endoscopic interventions, have made significant progress, they often fail to prevent recurrent bleeding and do not adequately address underlying portal hypertension. The mortality rate within six weeks after post-bleeding remains unacceptably high (20%) when treated with medication and endoscopy alone[10]. TIPS offers a minimally invasive alternative that rapidly decreases portal vein pressure and effectively controls bleeding, significantly lowering the risk for rebleeding and associated mortality[11].
One of the key challenges in TIPS is accurate puncture of the portal vein, which has historically relied on techniques that may increase the duration of surgery and the risk for complications. The introduction of real-time ultrasound-guided TIPS and DIT-guided TIPS has progressively reduced these risks by improving accuracy and reducing the number of attempts required for successful portal vein access. Our findings revealed that the use of DIT reduced the number of puncture attempts and surgical duration, which is not only pivotal in reducing patient stress and risk, but also in decreasing intraoperative complications such as blood loss and infection[6,12].
Moreover, our results indicate that fewer puncture attempts are required with the DIT-guided method, contributing to fewer postoperative complications such as intra-abdominal haemorrhage, thus improving overall procedural safety. The use of hepatic artery labelling to guide percutaneous transhepatic portal vein puncture has been reported to have a high technical success rate, which our study corroborates, demonstrating a 100% success rate in DIT-guided portal vein punctures compared with 94.4% reported by Gipson et al[13]. These enhancements in procedural metrics suggest that DIT-guided TIPS may represent a new standard for such interventions.
The key aspects of DIT-guided TIPS are as follows. First, the accuracy of indirect portal vein angiography can be significantly affected by abdominal motion artefacts, which is why patients are required to hold their breath. Given that many patients with acute bleeding are in critical condition and may struggle to cooperate, all TIPS surgeries at our centre were performed with the patient under general anaesthesia. This practice ensures controlled suspension of breathing, enhanced imaging accuracy, and procedural safety. Second, after labelling the hepatic artery, it is crucial to perform anteroposterior and lateral angiography. This dual approach helps to accurately display the position of the hepatic artery alongside its adjacent portal vein from a three-dimensional perspective, thus facilitating a more precise approach for portal vein puncture. Third, portal vein puncture carries an inherent risk for accidental penetration of the hepatic artery or biliary tract. To mitigate these risks, routine hepatic angiography is performed post-procedure to check for potential complications such as fistulas between the hepatic artery and portal vein. Fourth, selecting the opening of the right branch of the portal vein for the puncture significantly enhances the procedural success rate. This approach takes advantage of the anatomical positioning and offers a more straightforward pathway for catheterisation. Fifth, due to the potential for significant bleeding from portal vein punctures, special caution is advised, particularly in patients with coagulation disorders. Precautionary measures and readiness for immediate intervention are essential to manage adverse events during the procedure.
Consistent with the literature, liver function indicators generally improve post-TIPS, as confirmed by our study. This improvement was attributed to the alleviation of portal hypertension, which facilitated the recovery of liver function[14]. Both groups in our study exhibited significant improvement(s) in liver function tests and a reduction in portal vein pressure post-procedure, confirming the efficacy of TIPS in managing portal hypertension and its complications[15,16].
In conclusion, results of our study not only support the use of DIT to enhance the precision and safety of TIPS proce
| 1. | Song L, Wu X, Ren J, Gao Z, Xu Y, Xie H, Li D, Gong Z, Hu F, Liu H, Chen Y, Wu Z, Ning A. Assessment of the effect of treatment and assistance program on advanced patients with schistosomiasis japonica in China from 2009 to 2014. Parasitol Res. 2016;115:4267-4273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | European Association for the Study of the Liver. Corrigendum to "EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis" [J Hepatol 69 (2018) 406-460]. J Hepatol. 2018;69:1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 3. | Rajesh S, George T, Philips CA, Ahamed R, Kumbar S, Mohan N, Mohanan M, Augustine P. Transjugular intrahepatic portosystemic shunt in cirrhosis: An exhaustive critical update. World J Gastroenterol. 2020;26:5561-5596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 86] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 4. | Orpen-Palmer J, Stanley AJ. Update on the management of upper gastrointestinal bleeding. BMJ Med. 2022;1:e000202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | Lebrec D, Giuily N, Hadengue A, Vilgrain V, Moreau R, Poynard T, Gadano A, Lassen C, Benhamou JP, Erlinger S. Transjugular intrahepatic portosystemic shunts: comparison with paracentesis in patients with cirrhosis and refractory ascites: a randomized trial. French Group of Clinicians and a Group of Biologists. J Hepatol. 1996;25:135-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 288] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 6. | Haochen W, Yinghua Z, Jian W. Intrahepatic arterial localizer guided transjugular intrahepatic portosystemic shunt placement: Feasibility, efficacy, and technical success assessed by a case series-a STROBE- compliant article. Medicine (Baltimore). 2019;98:e16868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Monzawa S, Uchiyama G, Ohtomo K, Araki T. Schistosomiasis japonica of the liver: contrast-enhanced CT findings in 113 patients. AJR Am J Roentgenol. 1993;161:323-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Gaba RC, Khiatani VL, Knuttinen MG, Omene BO, Carrillo TC, Bui JT, Owens CA. Comprehensive review of TIPS technical complications and how to avoid them. AJR Am J Roentgenol. 2011;196:675-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Niu X, Hu T, Hong Y, Li X, Shen Y. The Role of Praziquantel in the Prevention and Treatment of Fibrosis Associated with Schistosomiasis: A Review. J Trop Med. 2022;2022:1413711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 10. | Jairath V, Barkun AN. Improving outcomes from acute upper gastrointestinal bleeding. Gut. 2012;61:1246-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Vizzutti F, Schepis F, Arena U, Fanelli F, Gitto S, Aspite S, Turco L, Dragoni G, Laffi G, Marra F. Transjugular intrahepatic portosystemic shunt (TIPS): current indications and strategies to improve the outcomes. Intern Emerg Med. 2020;15:37-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 12. | Dastmalchian S, Aryafar H, Tavri S. Intravascular Ultrasound Guidance for TIPS Procedures: A Review. AJR Am J Roentgenol. 2022;219:634-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Gipson MG, Smith MT, Durham JD, Brown A, Johnson T, Ray CE Jr, Gupta RK, Kondo KL, Rochon PJ, Ryu RK. Intravascular US-Guided Portal Vein Access: Improved Procedural Metrics during TIPS Creation. J Vasc Interv Radiol. 2016;27:1140-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Yamagami T, Tanaka O, Yoshimatsu R, Miura H, Suzuki T, Hirota T, Nishimura T. Hepatic artery-targeting guidewire technique during transjugular intrahepatic portosystemic shunt. Br J Radiol. 2011;84:315-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Warner DL, Owens CA, Hibbeln JF, Ray CE Jr. Indirect localization of the portal vein during a transjugular intrahepatic portosystemic shunt procedure: placement of a radiopaque marker in the hepatic artery. J Vasc Interv Radiol. 1995;6:87-9; discussion 89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | He J, Li J, Fang C, Qiao Y, Feng D. The Relationship and Changes of Liver Blood Supply, Portal Pressure Gradient, and Liver Volume following TIPS in Cirrhosis. Can J Gastroenterol Hepatol. 2022;2022:7476477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |