Published online Aug 27, 2024. doi: 10.4240/wjgs.v16.i8.2735
Revised: June 3, 2024
Accepted: June 21, 2024
Published online: August 27, 2024
Processing time: 103 Days and 1.5 Hours
Anorectal hemangioma is a rare and frequently misdiagnosed cause of lower gastrointestinal (GI) bleeding. Here, we present a minimally invasive therapy with selective embolization.
A 21-year-old male patient experienced painless rectal bleeding since childhood and was treated for ulcerative colitis. Diagnostic studies later revealed specific characteristics for vascular lesions-anorectal hemangiomas. The severity of rectal bleeding caused symptomatic anemia and possible surgical treatment was asso
Awareness of the clinical and radiological features of GI hemangiomas may help improve diagnostics and avoid inappropriate therapeutic procedures.
Core Tip: Anorectal hemangioma is a rare and frequently misdiagnosed cause of lower gastrointestinal bleeding. Surgical resection of the affected area is acknowledged as a treatment of choice; however, we present a minimally invasive therapeutic approach - selective embolization. This may be performed in a specific group of symptomatic patients for whom the risks and disadvantages (such as ostomy) of the surgical procedure outweigh the possible benefits.
- Citation: Pospisilova B, Frydrych J, Krajina A, Örhalmi J, Kajzrlikova IM, Vitek P. Anorectal hemangioma, a rare cause of lower gastrointestinal bleeding, treated with selective embolization: A case report. World J Gastrointest Surg 2024; 16(8): 2735-2741
- URL: https://www.wjgnet.com/1948-9366/full/v16/i8/2735.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i8.2735
Anorectal hemangioma is a rare cause of lower gastrointestinal (GI) bleeding. GI hemangioma, first described in 1839[1-4], typically manifests as rectal bleeding and is commonly misdiagnosed despite many reported cases[1-3,5]. Here, we present a case of a 21-year-old male patient with painless rectal bleeding since childhood and misdiagnosed with ulcerative colitis. He was treated with minimally invasive selective embolization after a successful anorectal hemangioma diagnosis.
A 21-year-old male patient who experienced painless rectal bleeding since childhood was referred to our gastroenterological center.
He experienced intermittent rectal bleeding since childhood and was treated for ulcerative colitis.
He was treated with azathioprine and mesalazine for ulcerative proctitis since 13 years of age. During the years, he presented with intermittent rectal bleeding despite the medication. Rectal bleeding worsened, and he required blood transfusions due to symptomatic anemia. At 18 years of age, he switched to a gastroenterologist for adults and was referred to a specialized gastroenterological center for appropriate atypical endoscopic finding management.
He experienced no other diseases and had no history of trauma or surgery. He reported no family history of inflammatory bowel diseases or other relevant diseases.
The patient presented with an anemic appearance, with no abnormalities during a digital rectal examination.
Serology (antineutrophil cytoplasmic antibodies and anti-saccharomyces cerevisiae antibody) was negative and blood tests revealed no signs of inflammation.
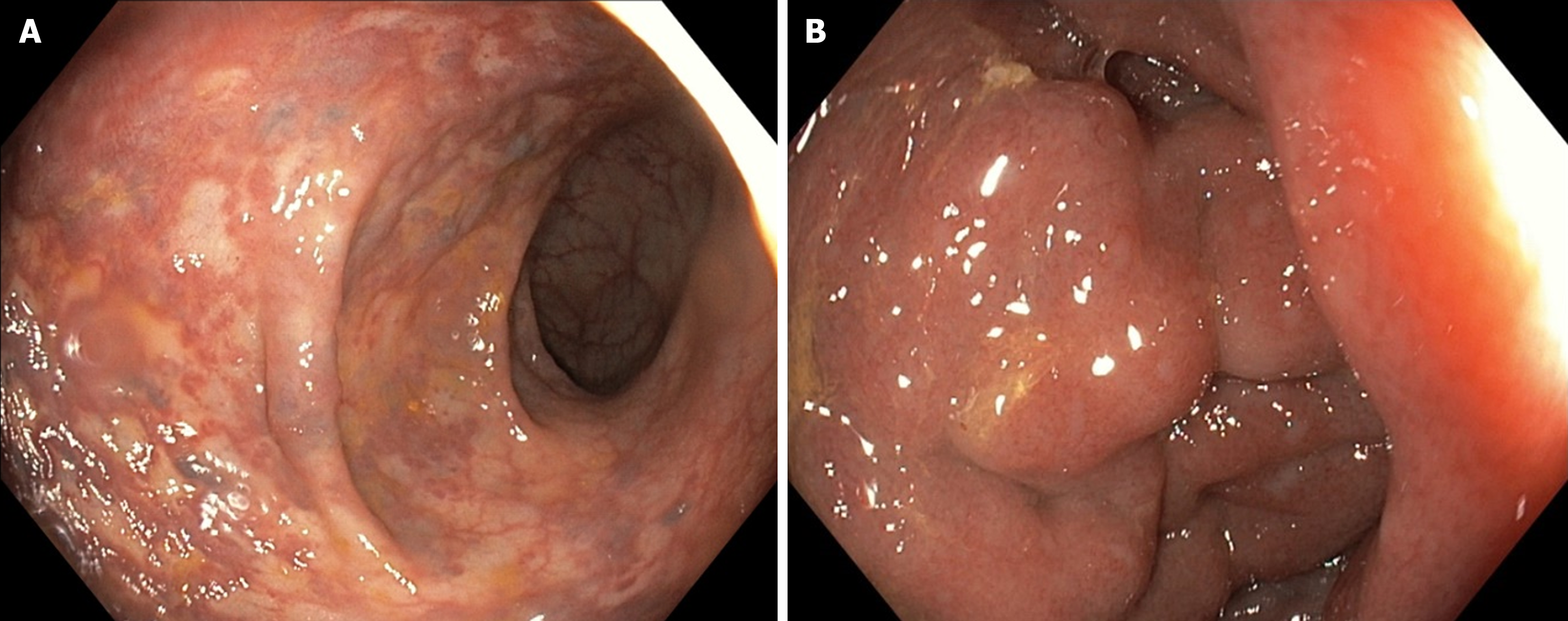
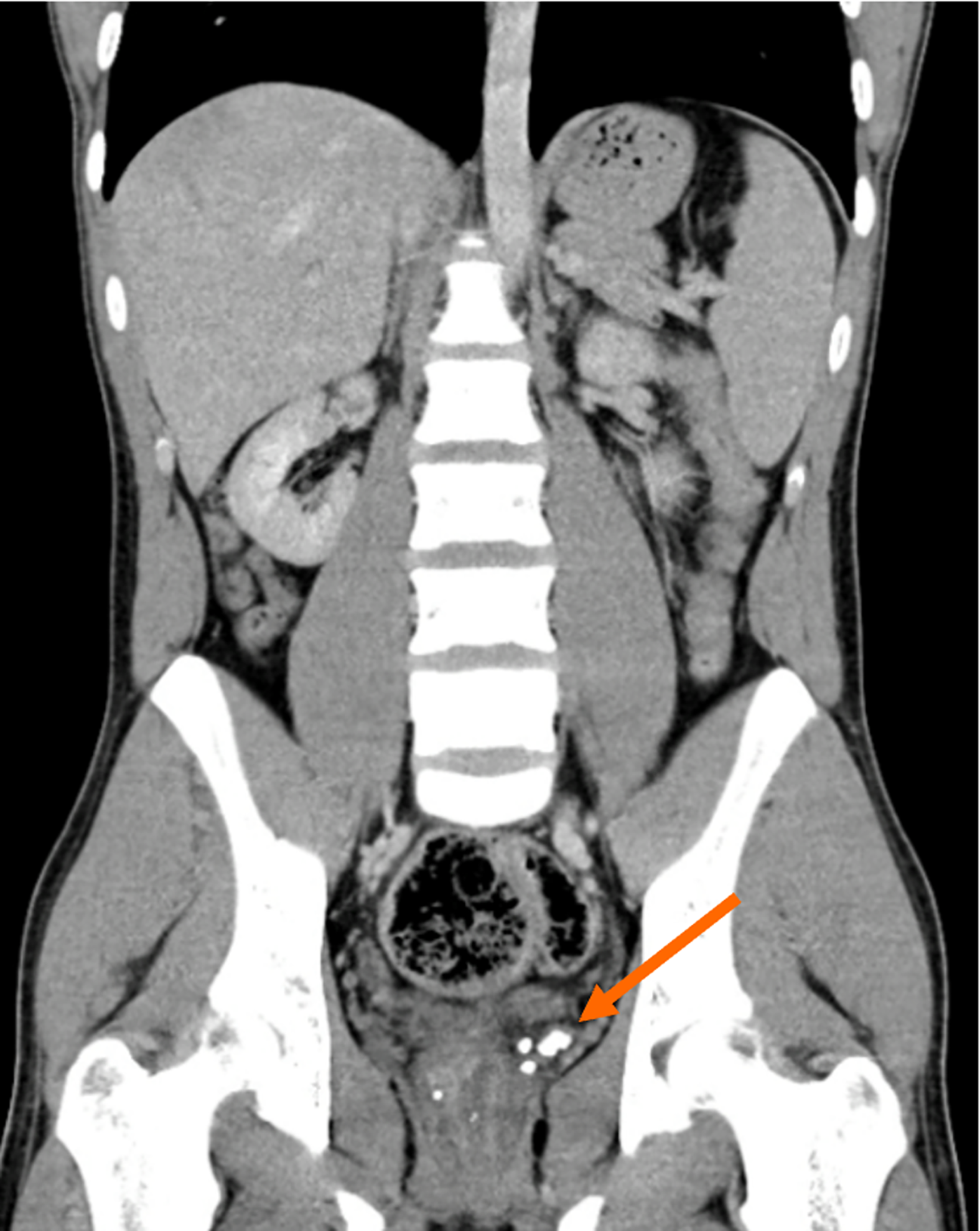
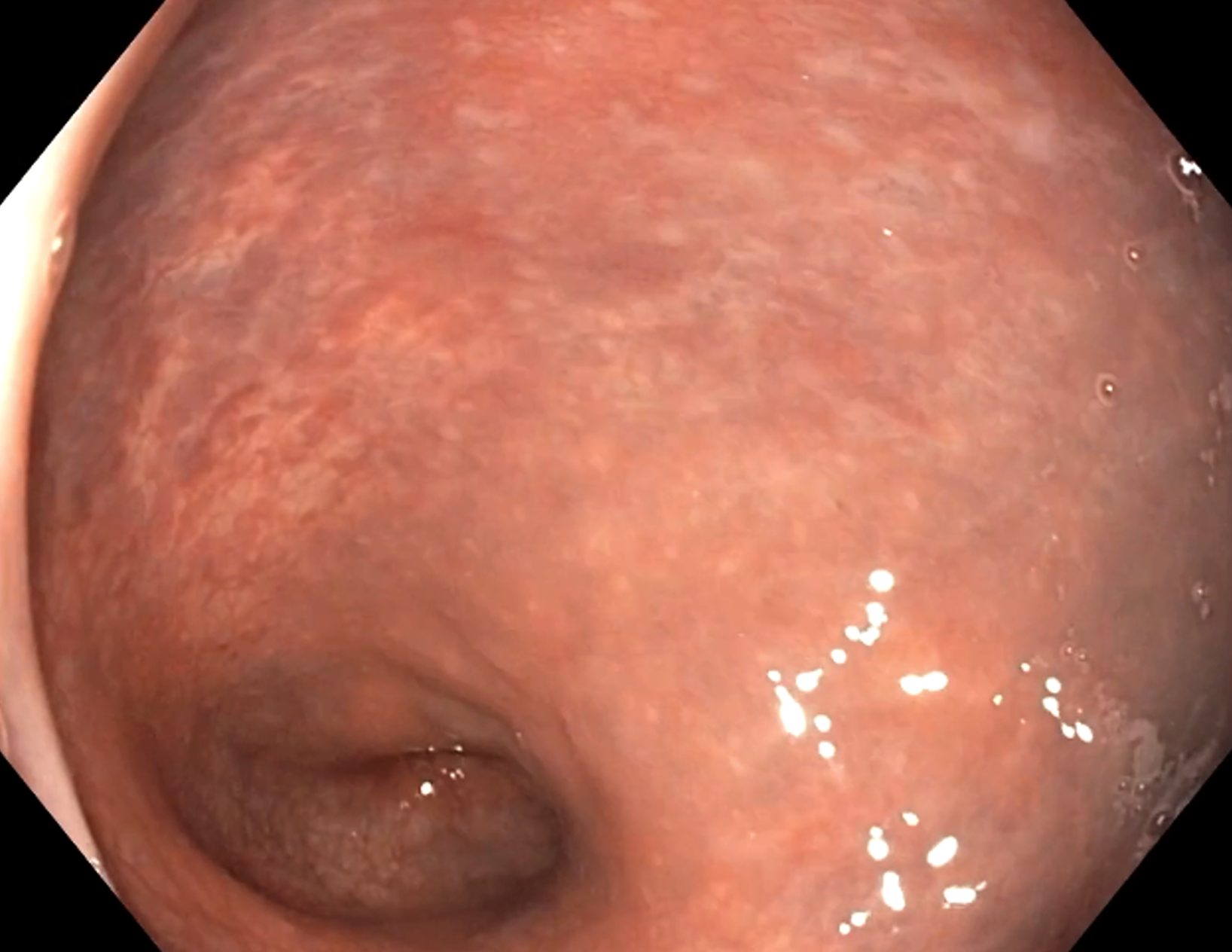
Control colonoscopy revealed significantly dilatated veins starting from the anal verge and continuing to the rectosigmoid junction (Figure 1), histology demonstrated no inflammation, and gastroscopic findings were normal. Pelvic and abdominal computed tomography (CT) scan was performed which ruled out portal and pelvic vein thrombosis as a possible cause of rectal varices. Additionally, a CT scan revealed several phleboliths around the rectum (Figure 2), which appeared as an important diagnostic clue. Pelvic magnetic resonance imaging (MRI) was planned.
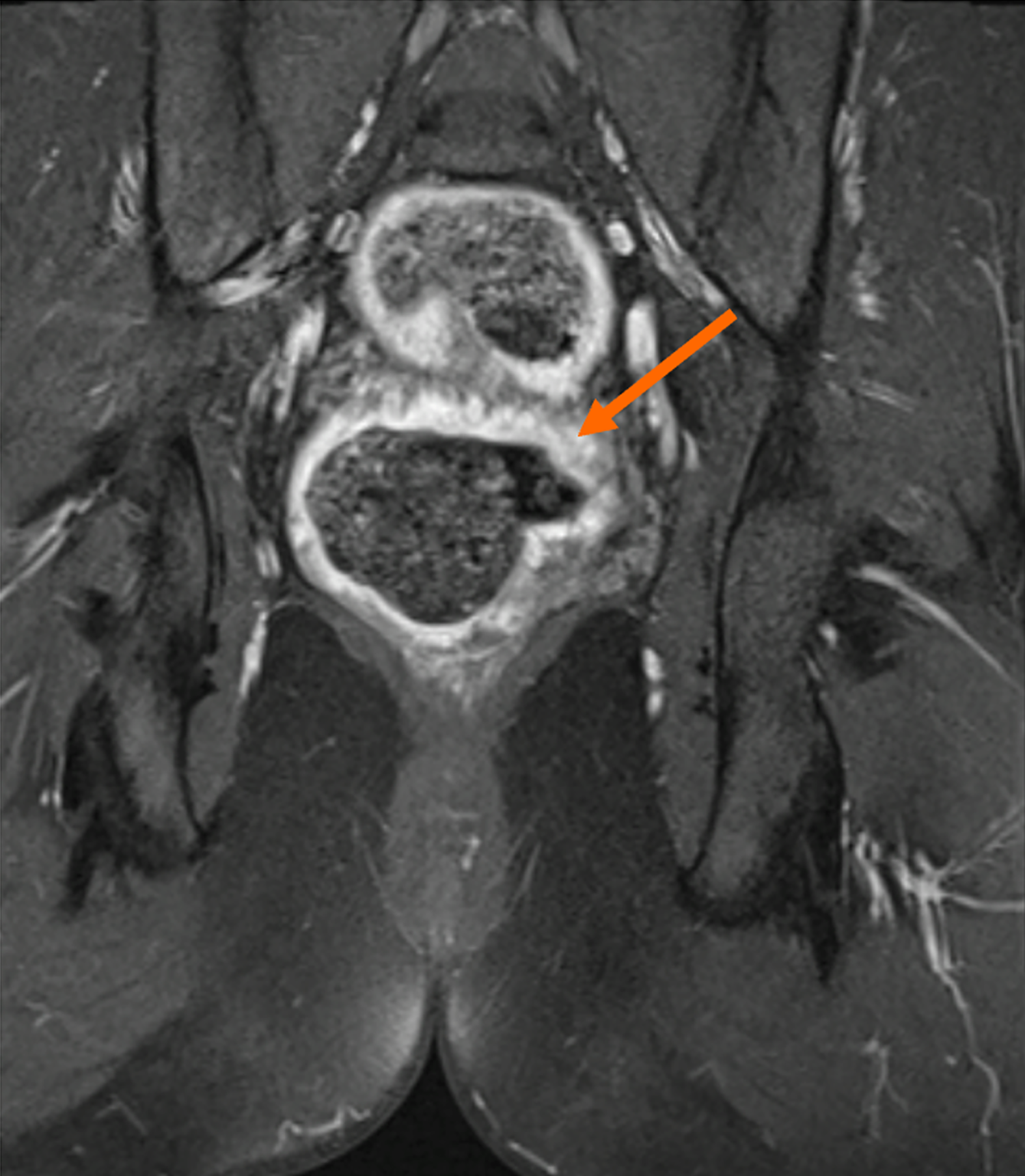
MRI unveiled a rare vascular lesion-anorectal hemangioma (Figure 3).
A coloproctologist was consulted because the patient was still presenting with intermittent rectal bleeding and a repetitive need for blood transfusions due to symptomatic anemias. A possible surgical treatment was assumed to be associated with a high risk of fecal incontinence. We selected a minimally invasive procedure using modalities of interventional radiology, considering the risks and patient’s preferences.
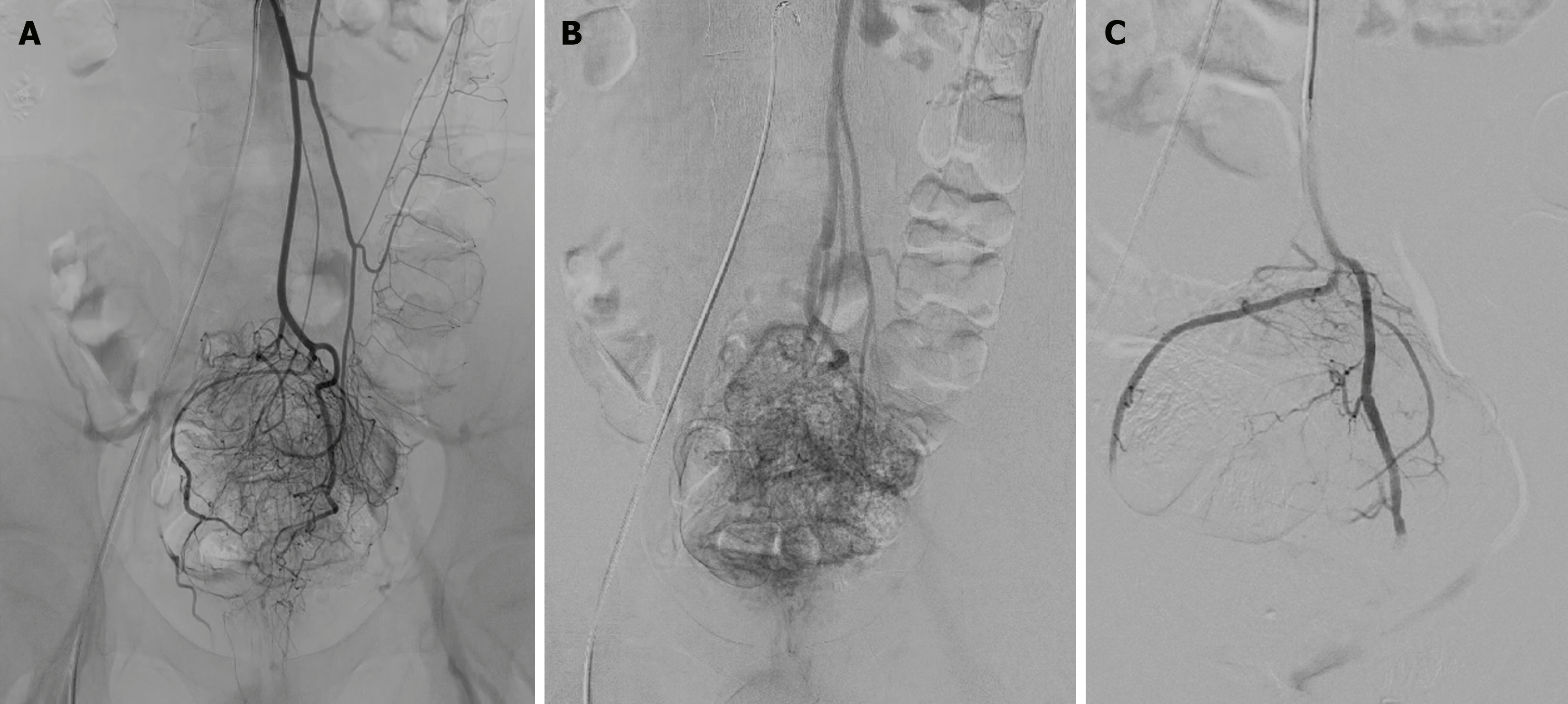
Our patient underwent angiography of the inferior mesenteric artery (Figure 4A and B) as well as partial embolization of rectal branches using polyvinyl alcohol (PVA) microparticles (Figure 4C). Angiography revealed a slightly hypertro
So far, the patient has had to undergo this treatment twice at a 9-month interval. He experienced mild rectal pain after the second embolization. Endoscopy revealed a significant vascular lesion regression as well as a small ischemic ulcer of the rectosigmoid junction, associated with the embolization procedure. The pain disappeared shortly and a follow-up colonoscopy revealed no ulcer (Figure 5). One year follow-up after these procedures indicated that rectal bleeding became less frequent and intensive, but parenteral iron therapy is still required despite verified endoscopic regression.
Anorectal hemangioma was considered a benign vascular tumor; however, these colonic hemangiomas are categorized with venous malformations according to the latest classification (May 2018 by the International Society for the Study of Vascular Anomalies). Unlike hemangiomas, these malformations exhibit normal endothelial cell turnover[2]. The most common type is “cavernous hemangioma” representing 80% of cases, capillary, or mixed occupying the rest[2,3,5]. GI hemangiomas generally occur more predominantly in the small intestine than in the large intestine and most colonic hemangiomas are located in the rectum and sigmoid colons[5,6]. The term hemangioma has been used because of its clinical familiarity and its possible existence in the GI tract. However, far more frequent vascular malformations, such as “cavernous hemangioma” are found[5].
Clinical presentation of anorectal vascular malformation is predominant with enterorrhagia of varying severity in children and young adults and causes secondary sideropenic anemia[3,7]. Approximately 10% of patients with colonic malformation remain asymptomatic[1,2]. Several syndromes, such as Rendu-Osler-Weber, blue rubber bleb nevus, Maffuci, and Klippel-Trenaunay-Weber, with characteristic organ involvement, were observed although GI vascular malformations may be solitary or multiple and may exist as separate entities[2,5,6,8].
Colonoscopy is considered a gold diagnostic standard as it helps evaluate the morphology and size of the lesion. Blue nodular lesions are typical results in diffuse cavernous vascular malformation and represent submucosal veins, which are dilatated and engorged[4,9]. In our patient, these lesions were present but were initially misdiagnosed as inflammatory changes by a pediatric gastroenterologist. Generally, rectal cavernous vascular malformation should not be biopsied due to a high risk of bleeding[1-3,5,7,9].
Both MRI and CT scans are selected for imaging methods. They both may reveal an irregular bowel wall thickening as well as the extent of the lesion and possible adjacent organ involvement. CT scan revealed a crucial diagnostic clue, phleboliths, which are most prevalently found in the pelvis[1,2]. Phleboliths are rounded hyaline-organized thrombi that are visible on imagining when calcified[10]. Phleboliths were also present in our patient. However, MRI is the preferred diagnostic method, especially when considering surgery. It helps evaluate the extent of anal canal invasion as well as sphincter involvement[4,9]. MRI reveals hypointensity on T1-weighted and hyperintensity on T2-weighted imaging[2,4,8].
An affected area surgical resection is generally a treatment of choice. The sphincter-saving procedure is preferred if technically feasible with anterior rectal resection and colo-anal anastomosis. Additionally, extracolonic organs can be affected; therefore, a thorough abdominal cavity exploration must be performed[9]. Endoscopic resection should be preferred to surgery in cases of pedunculated lesions. However, bleeding and perforation are a high risk; thus, having a careful endoscopic approach and adequate bleeding prophylaxis is important[11].
A minimally invasive selective embolization should be considered in a specific group of symptomatic patients for whom the risks of the surgery and disadvantages (such as ostomy) of the surgical procedure outweigh the possible benefits. In our case, PVA microparticles were used for partial embolization only, considering the risk of ischemia and the possibility of causing stenosis. Additionally, we found only one ischemic ulcer in the rectosigmoid junction that healed without subsequent stenosis. In general, these PVA microparticles induce mechanical occlusion, cause thrombus, and induce inflammatory response characterized by vessel wall angionecrosis. PVA is considered a permanent embolic agent as it is not biodegradable[12]. However, vessel recanalization and bleeding recurrence after this procedure are not exceptions[9,12]. Selective embolization of the rectal branches of the inferior mesenteric artery is performed for treating symptomatic hemorrhoids (Vidal). In patients with less severe symptoms, an even more conservative approach, ferrum substitution, may be considered, which is eventually combined with blood transfusions if required.
In conclusion, anorectal vascular malformation, with only a small number of case reports, is a rare cause of rectal bleeding, and misdiagnosis is frequent because of a lack of awareness. More uncommon causes must be considered, such as GI hemangiomas and vascular malformations, in cases of atypical clinical, imaging, or endoscopic findings in patients with rectal bleeding.
With this case report, we aimed to present a treatment using a minimally invasive method, selective embolization. Our patient still experiences rectal bleeding episodes and requires ferrum substitution, but we consider this treatment successful as it had a major impact on improving the quality of his life, and the patient no longer required blood transfusions during our one-year follow-up.
| 1. | Shen JD, Chen CW, Chen TA, Yueh T. Colonic hemangioma, a diagnostic challenge in young adults with lower gastrointestinal tract bleeding. Formosan J Surg. 2016;49:238-241. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Ganesananthan S, Barlow J, Durai D, Hawthorne AB. Multiple venous malformations in the left colon and rectum: a long-standing case managed conservatively and an update of current literature. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Neto WBDS, Neto GT, Cunha CMQD, Brasil AC, Feitosa JNP. Anorectal hemangioma – differential diagnosis of anal bleeding. J Coloproctol. 2017;37:44-46. [DOI] [Full Text] |
| 4. | Zeng Z, Wu X, Chen J, Luo S, Hou Y, Kang L. Safety and Feasibility of Transanal Endoscopic Surgery for Diffuse Cavernous Hemangioma of the Rectum. Gastroenterol Res Pract. 2019;2019:1732340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Yoo S. GI-Associated Hemangiomas and Vascular Malformations. Clin Colon Rectal Surg. 2011;24:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Levy AD, Abbott RM, Rohrmann CA Jr, Frazier AA, Kende A. Gastrointestinal hemangiomas: imaging findings with pathologic correlation in pediatric and adult patients. AJR Am J Roentgenol. 2001;177:1073-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Cotzias E, Rehman SF, Arsalani Zadeh R, Smith D. Conservative management of diffuse cavernous haemangioma of the sigmoid and rectum. Ann R Coll Surg Engl. 2020;102:e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Al-Tkrit A, Aneeb M, Mekaiel A, Alawawdeh F, Mehta A. Cavernous Hemangioma: A Rare Cause of Massive Lower Gastrointestinal Bleeding. Cureus. 2020;12:e10075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Hermosa AR, Zorrilla-Ortuzar J, Valle-Hernández ED. Diffuse cavernous hemangioma of the rectum. Cir Cir. 2021;89:818-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, Burrows P, Frieden IJ, Garzon MC, Lopez-Gutierrez JC, Lord DJ, Mitchel S, Powell J, Prendiville J, Vikkula M; ISSVA Board and Scientific Committee. Vascular Anomalies Classification: Recommendations From the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136:e203-e214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 827] [Cited by in RCA: 807] [Article Influence: 80.7] [Reference Citation Analysis (0)] |
| 11. | Mascarenhas M, Morais R, Teixeira R, Macedo G. A case report of an unexpected colonic polyp: cavernous hemangioma. Ann Coloproctol. 2023;39:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Sheth RA, Sabir S, Krishnamurthy S, Avery RK, Zhang YS, Khademhosseini A, Oklu R. Endovascular Embolization by Transcatheter Delivery of Particles: Past, Present, and Future. J Funct Biomater. 2017;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |