Published online Aug 27, 2024. doi: 10.4240/wjgs.v16.i8.2719
Revised: July 17, 2024
Accepted: July 23, 2024
Published online: August 27, 2024
Processing time: 142 Days and 8 Hours
Anterior cutaneous nerve entrapment syndrome (ACNES) is a condition mani
A 66-year-old woman manifested ACNES after a robot-assisted distal gastrec
In this case, the trocar port was inserted between the rectus and transverse abdominis muscles. The intercostal nerves might have been entrapped on both sides of the rectus and transversus abdominis muscles. Hence, rectus sheath and transverse abdominis plane blocks were required to achieve complete pain relief. To the best of our knowledge, this is the first report on use of a combination of rectus sheath and transverse abdominis plane blocks for pain relief in ACNES.
Core Tip: Anterior cutaneous nerve entrapment syndrome (ACNES) is defined as chronic abdominal wall pain caused by entrapment of cutaneous branches of lower thoracoabdominal intercostal nerves. In the present report, ACNES after a robot-assisted distal gastrectomy was successfully treated with a combination of ultrasound-guided rectus sheath and transverse abdominis plane blocks. Peripheral nerve block should be selected based on the extent and degree of adhesions causing ACNES.
- Citation: Saito Y, Takeuchi H, Tokumine J, Sawada R, Watanabe K, Yorozu T. Ultrasound-guided peripheral nerve blocks for anterior cutaneous nerve entrapment syndrome after robot-assisted gastrectomy: A case report. World J Gastrointest Surg 2024; 16(8): 2719-2723
- URL: https://www.wjgnet.com/1948-9366/full/v16/i8/2719.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i8.2719
Anterior cutaneous nerve entrapment syndrome (ACNES) is an idiopathic, pathologic state primarily involving pain caused by strangulation of the anterior cutaneous branch of the lower intercostal nerves[1]. ACNES pain can be sharp, dull, or burning in character and is localized along the course of abdominal nerves[1,2]. The diagnosis of ACNES is primarily based on physical examination[1]. Carnett’s sign, where the examiner’s finger is placed at the site of maximum tenderness in the abdominal wall, and the patient is instructed to raise their head and torso with arms crossed over the chest, is the most useful diagnostic test. If pain increases with this movement, it indicates that the pain source is in the abdominal wall suggesting a diagnosis of ACNES[1,3].
ACNES treatment includes drug therapy, nerve blocks, and surgical neurotomy[1,3]. Herein, we report a case of ACNES after robot-assisted distal gastrectomy with successful application of rectus sheath and transversus abdominis plane blocks. A written informed consent for publication was obtained from the patient.
A 66-year-old woman underwent endoscopic submucosal dissection for a neuroendocrine tumor in the stomach, which was causing hypergastrinemia, type A gastritis, and megaloblastic anemia. Pathological examination of the tumor indicated the need for additional resection. Two months later, the patient had a robot-assisted distal gastrectomy. On the second postoperative day, she developed "pulling and throbbing" pain at the right abdominal port insertion site following body movement.
The pain was severe (numerical pain rating scale 8/10) but transient with sudden onset. Tramadol hydrochloride and acetaminophen were administered orally for pain control. However, the pain did not improve after discharge from the hospital (numerical pain rating scale 10/10) and became more frequent, interfering with daily life. Eventually, the patient could not perform daily activities and was urgently hospitalized 3 weeks after discharge.
The patient’s medical history included bronchial asthma, coronavirus disease 2019 pneumonia, and thyroid tumor.
No special remarks.
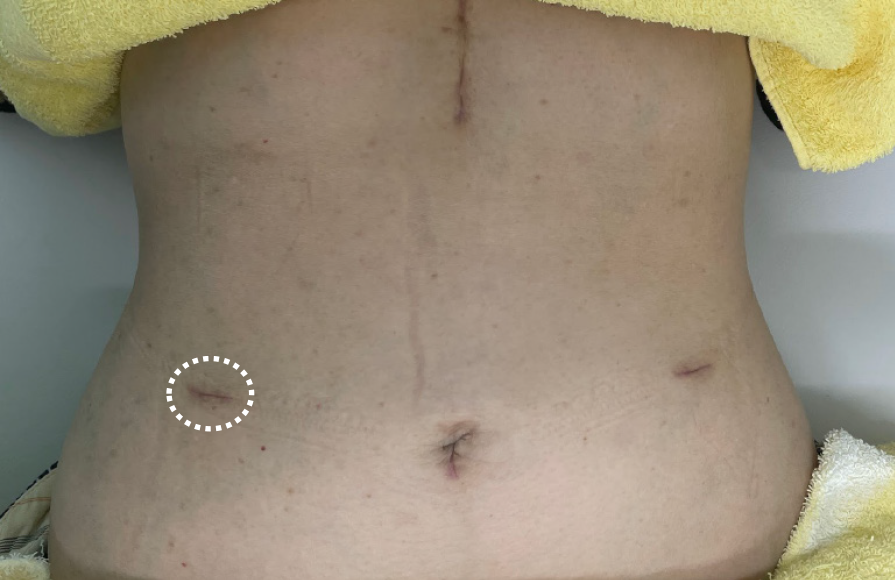
On physical examination, pain was elicited after compression of the right surgical wound (Figure 1) and elevation of the head (positive Carnett’s sign).
Nonspecific.
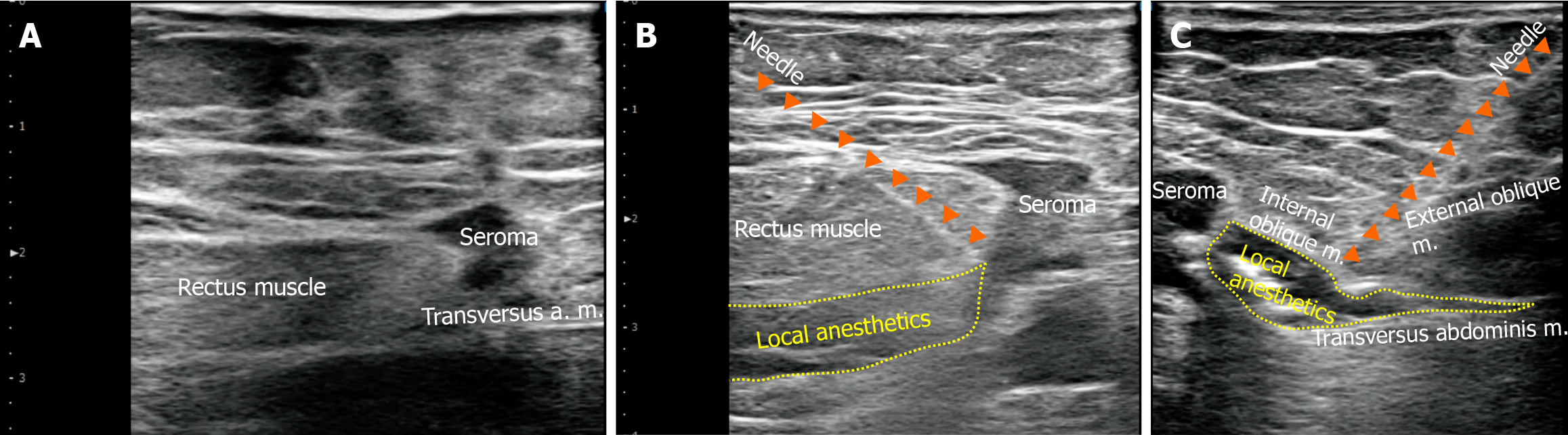
Ultrasonography revealed a scar with a seroma between the rectus abdominis and internal oblique and transversus abdominis muscles. This coincided with the entry site of a 12-mm trocar port used during surgery (Figure 2A).
ACNES was diagnosed in this patient.
A rectus sheath block using 40 mL of 0.25% levobupivacaine and 6.6 mg of dexamethasone was performed targeting the scar site under ultrasound guidance (Figure 2B). After the rectal sheath block, no pain was noted until bedtime that day. However, during defecation the following day, the patient felt severe pain radiating laterally from the previous site of pain. Therefore, a transverse abdominis plane block was performed using 40 mL of 0.25% levobupivacaine and 6.6 mg of dexamethasone under ultrasound guidance (Figure 2C).
There was no pain following these injections, and the patient was discharged from the hospital. The patient has ex
Follow-up computed tomography at 3 months after the treatment showed that the seroma had disappeared.
Traditionally, ACNES was considered an idiopathic pain syndrome. Therefore, the definition of ACNES generally does not include surgical causes of pain[1]. However, surgery-related ACNES has been frequently reported[3], and a definition of ACNES that does not exclude surgery-related pathology should be considered[4,5].
The anatomic landmarks for intercostal nerves T8–T12 are the internal oblique and transversus abdominis muscles[1-3]. The intercostal nerve enters the rectus abdominis sheath with a sharp curve to its path, which is considered the likely site of injury[1-3]. In this case, the trocar port was inserted between the rectus and transverse abdominis muscles. The intercostal nerves may be entrapped on both sides of the rectus and transversus abdominis muscles. Hence, both rectus sheath and transverse abdominal plane blocks were needed to achieve complete pain relief.
Injections of small volumes (≤ 10 mL and usually 2–5 mL) of local anesthetics have been used to treat ACNES[1,3], and many cases of ACNES have been effectively treated with this regimen[1,3]. Peripheral nerve blocks have been recently reported to be useful in cases of surgically related ACNES with rectus sheath or transverse abdominis plane blocks being used[5-7]. In our previous case report, an ultrasound-guided rectus sheath block with 20 mL of local anesthetic facilitated hydrodissection between the rectus abdominis muscle and the posterior wall sheath, where an adhesion-like object was present[5]. In the current case, we used 40 mL of local anesthetic for ultrasound-guided peripheral nerve block enabling hydrodissection and subsequent pain relief. However, Batistaki et al[6] and Sahoo et al[7] used a smaller volume of local anesthetics (≤ 10 mL) for repeated nerve blocks to attain pain relief[5,6]. Recently, the efficacy of ultrasound-guided hydrodissection for treating peripheral nerve entrapment has been demonstrated[8,9]. We believe that this technique can also be successfully applied in the treatment of surgery-related ACNES.
In this case, the trocar site was closed using a fascial close instrument (Endo Close™, COVIDIEN JAPAN INC. Japan), which enabled the tying of both muscle layers and facias to prevent trocar-site hernia. Shin et al[10] hypothesized that nerve entrapment during laparoscopic surgery was not caused by direct port-related trauma but by the fascial suture. This hypothesis was established following experience with many cases in which pain disappeared when the sutures were removed. In the present case, however, the pain was relieved after hydrodissection with a nerve block. Therefore, it is unclear whether the ACNES in this case were due to adhesions developing during the wound healing process or en
Treatment of ACNES includes systemic medication, trigger point injections with local anesthetics, ultrasound-guided nerve blocks, chemical neurolysis, neurotomy of anterior cutaneous nerve, intraperitoneal onlay mesh reinforcement, radiofrequency ablation, and botulinum toxin injection[1]. If a nerve block had been ineffective in this case, invasive treatment modalities, such as chemical neurolysis with 5% phenol solution or surgical anterior neurotomy, might have been considered[1]. In particular, anterior neurotomy has been reported to be effective in many clinical studies[1]. In
The performed diagnostics in this ACNES case showed that intercostal nerves might be entrapped on both sides of rectus and transversus abdominis muscles. To the best of our knowledge, this is the first report on the combination of rectus sheath and transverse abdominis plane blocks necessary for pain relief in ACNES. Cases of laparoscopic surgery are increasing every year[11]. During these interventions, the location of the trocar port incision should be carefully determined to avoid the possible risk of ACNES.
| 1. | Chrona E, Kostopanagiotou G, Damigos D, Batistaki C. Anterior cutaneous nerve entrapment syndrome: management challenges. J Pain Res. 2017;10:145-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Scheltinga MR, Roumen RM. Anterior cutaneous nerve entrapment syndrome (ACNES). Hernia. 2018;22:507-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Boelens OB, Scheltinga MR, Houterman S, Roumen RM. Management of anterior cutaneous nerve entrapment syndrome in a cohort of 139 patients. Ann Surg. 2011;254:1054-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | van Assen T, Brouns JA, Scheltinga MR, Roumen RM. Incidence of abdominal pain due to the anterior cutaneous nerve entrapment syndrome in an emergency department. Scand J Trauma Resusc Emerg Med. 2015;23:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Sawada R, Watanabe K, Tokumine J, Lefor AK, Ando T, Yorozu T. Ultrasound-guided rectus sheath block for anterior cutaneous nerve entrapment syndrome after laparoscopic surgery: A case report. World J Clin Cases. 2022;10:2357-2362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Reference Citation Analysis (0)] |
| 6. | Batistaki C, Saranteas T, Adoni A, Kostopanagiotou G. Ultrasound-guided anterior abdominal cutaneous nerve block for the management of bilateral abdominal cutaneous nerve entrapment syndrome (ACNES). Pain Physician. 2013;16:E799-E801. [PubMed] |
| 7. | Sahoo RK, Nair AS. Ultrasound Guided Transversus Abdominis Plane Block for Anterior Cutaneous Nerve Entrapment Syndrome. Korean J Pain. 2015;28:284-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Lam KHS, Hung CY, Chiang YP, Onishi K, Su DCJ, Clark TB, Reeves KD. Ultrasound-Guided Nerve Hydrodissection for Pain Management: Rationale, Methods, Current Literature, and Theoretical Mechanisms. J Pain Res. 2020;13:1957-1968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 9. | Buntragulpoontawee M, Chang KV, Vitoonpong T, Pornjaksawan S, Kitisak K, Saokaew S, Kanchanasurakit S. The Effectiveness and Safety of Commonly Used Injectates for Ultrasound-Guided Hydrodissection Treatment of Peripheral Nerve Entrapment Syndromes: A Systematic Review. Front Pharmacol. 2020;11:621150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Shin JH, Howard FM. Abdominal wall nerve injury during laparoscopic gynecologic surgery: incidence, risk factors, and treatment outcomes. J Minim Invasive Gynecol. 2012;19:448-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Joris JL, Georges MJ, Medjahed K, Ledoux D, Damilot G, Ramquet CC, Coimbra CI, Kohnen LP, Brichant JF. Prevalence, characteristics and risk factors of chronic postsurgical pain after laparoscopic colorectal surgery: Retrospective analysis. Eur J Anaesthesiol. 2015;32:712-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |