Published online Aug 27, 2024. doi: 10.4240/wjgs.v16.i8.2649
Revised: June 26, 2024
Accepted: July 11, 2024
Published online: August 27, 2024
Processing time: 97 Days and 23.6 Hours
Postoperative pulmonary complications (PPCs) are common in patients who undergo colorectal surgery. Studies have focused on how to accurately diagnose and reduce the incidence of PPCs. Lung ultrasound has been proven to be useful in preoperative monitoring and postoperative care after cardiopulmonary surgery. However, lung ultrasound has not been studied in abdominal surgeries and has not been used with wearable devices to evaluate the influence of postoperative ambulation on the incidence of PPCs.
To investigate the relationship between lung ultrasound scores, PPCs, and postoperative physical activity levels in patients who underwent colorectal surgery.
In this prospective observational study conducted from November 1, 2019 to August 1, 2020, patients who underwent colorectal surgery underwent daily bedside ultrasonography from the day before surgery to postoperative day (POD) 5. Lung ultrasound scores and PPCs were recorded and analyzed to investigate their relationship. Pedometer bracelets measured the daily movement distance for 5 days post-surgery, and the correlation between postoperative activity levels and lung ultrasound scores was examined.
Thirteen cases of PPCs was observed in the cohort of 101 patients. The mean (standard deviation) peak lung ultrasound score was 5.32 (2.52). Patients with a lung ultrasound score of ≥ 6 constituted the high-risk group. High-risk lung ultrasound scores were associated with an increased incidence of PPCs after colorectal surgery (logistic regression coefficient, 1.715; odds ratio, 5.556). Postoperative movement distance was negatively associated with the lung ultrasound scores [Spearman’s rank correlation coefficient (r), -0.356, P < 0.05].
Lung ultrasound effectively evaluates pulmonary condition post-colorectal surgery. Early ambulation and respiratory exercises in the initial two PODs will reduce PPCs and optimize postoperative care in patients undergoing colorectal surgery.
Core Tip: This study investigates the role of lung ultrasound combined with wearable pedometer bracelets in assessing postoperative pulmonary complications (PPCs) in patients who underwent colorectal surgery. Higher lung ultrasound scores (≥ 6) are significantly associated with increased PPC incidence, whereas greater postoperative movement is linked to lower lung ultrasound scores. These findings emphasize the importance of early ambulation and respiratory exercises in reducing PPCs and improving postoperative care in patients undergoing colorectal surgery.
- Citation: Lin C, Wang PP, Wang ZY, Lan GR, Xu KW, Yu CH, Wu B. Innovative integration of lung ultrasound and wearable monitoring for predicting pulmonary complications in colorectal surgery: A prospective study. World J Gastrointest Surg 2024; 16(8): 2649-2661
- URL: https://www.wjgnet.com/1948-9366/full/v16/i8/2649.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i8.2649
Colorectal cancer (CRC) is a common malignant tumor of the gastrointestinal tract. The incidence and mortality rates of CRC have increased in recent years[1]. In China, CRC was among the five leading cancer types in 2020, with an incidence rate of 23.9 per 100000 and a mortality rate of 12 per 100000[2]. Surgery is an important part of the comprehensive treat
PPCs may result from the intra-abdominal pressure of the pneumoperitoneum and the head-down tilt position (Trendelenburg position) during surgery[9]. Atelectasis is one of the most common PPCs, especially after abdominal or thoracoabdominal surgeries[10]. If not managed properly, atelectasis can progress to consolidation, infection, or pleural effusion.
Chest X-ray (CXR) and thoracic computed tomography (CT) scans are widely deployed in the clinical evaluation of pulmonary conditions. Thoracic CT scan is the gold standard for lung imaging. However, intravenous catheters and draining tubes are preserved for only a short period after colorectal surgery, leading to difficulties with patient transport. Considering the exposure to radiation and high expenses, thoracic CT is not recommended for patients who undergo colorectal surgery. The use of CXR is limited by its low sensitivity. The diagnosis and management of PPCs based only on clinical manifestations can be error-prone. Therefore, a fast and convenient evaluation of pulmonary condition is needed to promptly identify the presence and severity of atelectasis in patients who undergo colorectal surgery.
Lung and heart ultrasonography is crucial during cardiopulmonary evaluation in intensive care medicine, enabling real-time optimization of the patient’s respiratory and hemodynamic status[11,12]. By detecting B lines during lung ultrasonography, intensive care unit specialists can evaluate lung consolidation and pleural effusion[13,14]. The diagnostic capability of lung ultrasound is similar to that of CT for many pulmonary diseases, including perioperative lung consolidation, pleural effusion, pulmonary edema, and pneumothorax[15,16]; it is superior to that of CXR[17-19]. Published studies have focused on the use of lung ultrasound in preoperative examination and monitoring after cardiothoracic surgery. However, the use of lung ultrasound in the perioperative period of abdominal surgery has not been reported.
Early postoperative ambulation is an important element of enhanced recovery after surgery and facilitates recovery[20,21]. Less physical activity is associated with an increased risk of perioperative complications in patients with CRC[22]. However, the physical activity of patients is hard to monitor and quantify in clinical settings.
The rapid upgrading of “wearable devices” (portable electronic products), such as smartphones, sports watches, earphones, and bracelets, has conveniently provided clinicians with more accurate physiological data[23,24]. With these data, clinicians can monitor patient’s condition in real-time during hospitalization, promptly adjust treatment strategies according to the information obtained, and effectively reduce the incidence of perioperative complications and medical expenses during hospitalization. Herein, we used sports bracelets to monitor the postoperative physical activity of patients after colorectal surgeries and investigated whether the effect of exercise can be reflected in lung ultrasonography.
This prospective study aims to investigate the relationship between the lung ultrasound score and the occurrence of PPCs and between lung ultrasound scores and postoperative physical activity levels. To our knowledge, this is the first study to investigate the use of lung ultrasound scores to evaluate the incidence of PPCs in patients undergoing colorectal surgery using wearable devices. The results can help to better predict PPCs after colorectal surgeries and guide clinical decision-making.
We included eligible patients who underwent colorectal surgery at our hospital between November 1, 2019 and August 1, 2020. The eligibility criteria were: (1) Age 18-85 years; (2) American Society of Anesthesiologists (ASA) physical status class I-III; (3) Scheduled for a selective operation of the abdomen; (4) Estimated operation time more than 60 minutes; and (5) Willingness to sign the consent form. The exclusion criteria included: (1) Body mass index (BMI) > 30 kg/m2; (2) General anesthesia or mechanical ventilation within 2 weeks before surgery; (3) Severe respiratory insufficiency: Forced expiratory volume in the first second < 30%; (4) History of thoracic surgery (thoracic drainage, thoracotomy, or thoracoscopy); (5) History of bullae; and (6) Recent pneumothorax or subcutaneous emphysema. This study was approved by the Ethics Committee of Peking Union Medical College Hospital (approval number: Zs-2584). All patients provided written informed consent.
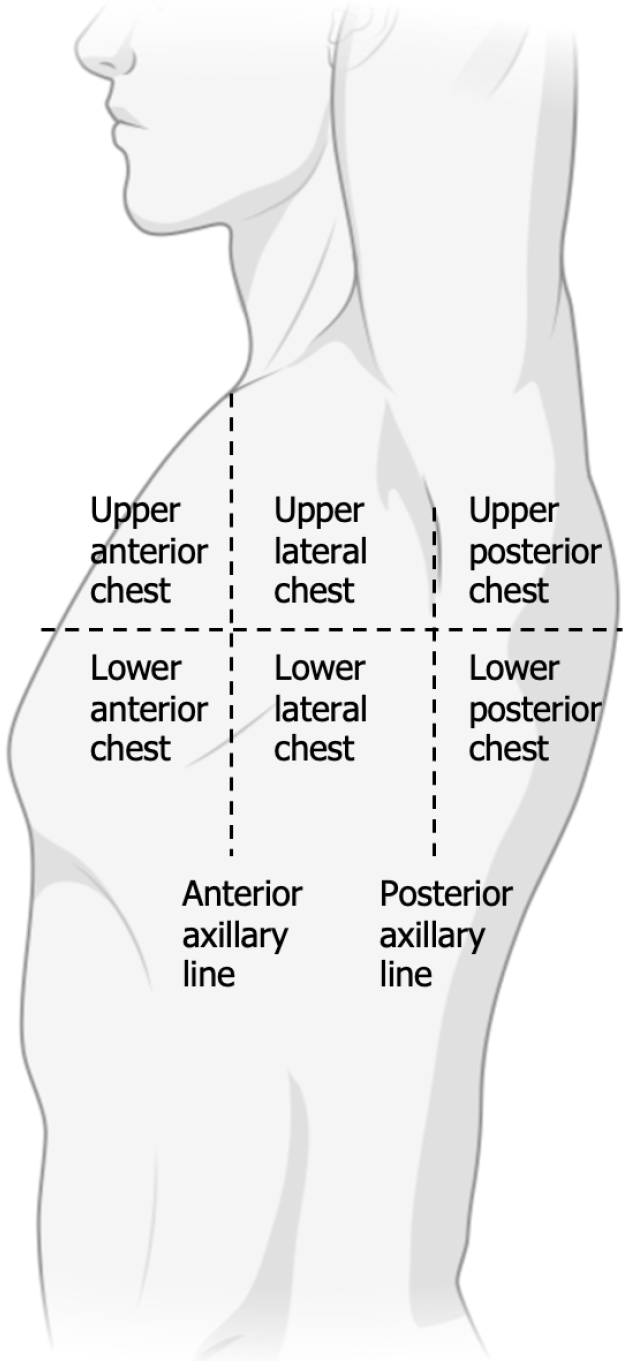
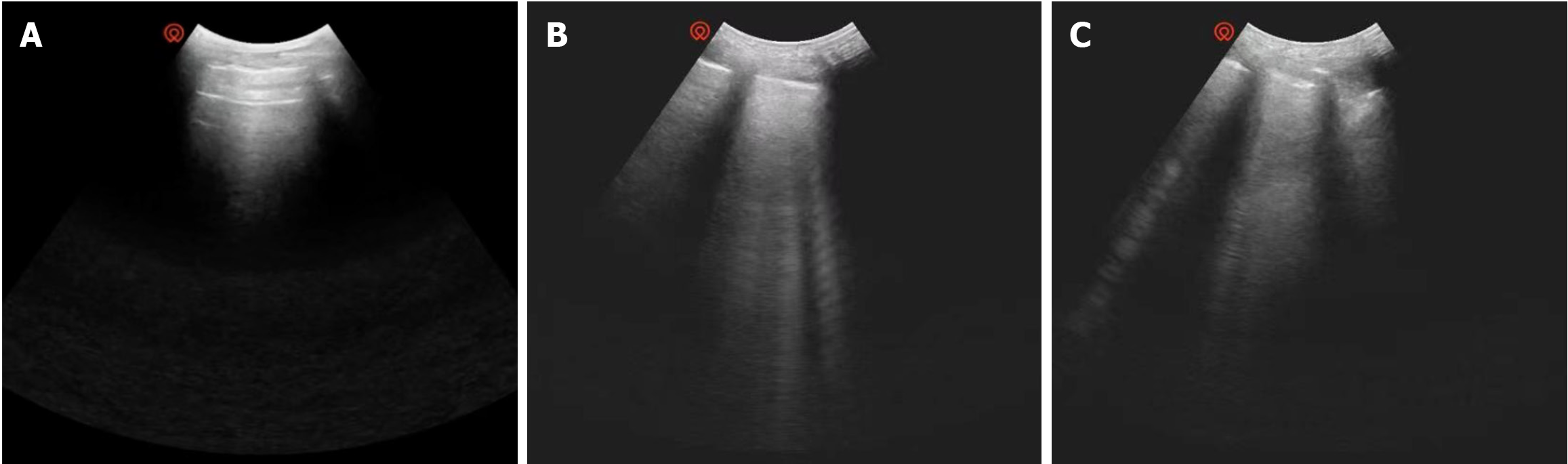
We used the Wisonic Piloter portable ultrasound system for lung ultrasound. Each patient underwent daily bedside ultrasonography the day before surgery and on postoperative days (PODs) 1-5. Ultrasound was performed by an anesthesiologist and a surgeon who had undergone intensive care ultrasound training, both of whom reviewed the data. The time of examination for each patient was approximately 5-10 min. We recorded ultrasound images of the chest at 12 Locations: Upper anterior chest, lower anterior chest, upper lateral chest, lower lateral chest, upper posterior chest, and lower posterior chest on both sides (Figure 1)[25]. The frequency of the probe was 4-15 MHz; the probe was perpendicular to the intercostal space, and the patient was in the supine, semi-recumbent, and lateral recumbent positions. The ultrasound scoring standards were 0 points: 0 to 2 B lines, clear parallel A lines; 1 point: 3 or more B lines, thickened pleural line; 2 points: Multiple overlapped B lines, thickened or irregular pleural line; 3 points: Lung consolidation, subpleural soft tissue signal (Figure 2)[26]. Patients with poor lung ultrasound scores were informed of their score and the risks.
The pedometer bracelet recorded the daily movement distance from POD 1 to 5. The bracelet also presented the patient with other related indicators, such as heart rate, body temperature, and step count. The bracelet was worn on the wrist of the arm without the intravenous infusion catheter. Patients were instructed to wear the bracelet constantly except in special circumstances. After use, the bracelets were disinfected by repeated wiping with 75% alcohol before being given to the next patient.
All patients received routine postoperative care after colorectal surgery. Prophylactic antibiotics were not administered in usual circumstances. We recommended early initiation of ambulation and respiratory function exercises for all patients after surgery. On PODs 1 and 2, we recommended aerosol inhalation twice a day. The postoperative analgesia conditions were consistent. The fluid intake and output volumes were generally balanced.
We recorded patients’ age, BMI, ASA classification, history of abdominal surgery, pulmonary comorbidity, preoperative pulmonary symptoms, smoking history, preoperative respiratory function exercise, time of operation, blood loss, daily movement distance and lung ultrasound scores after surgery, PPCs (Table 1)[27], hospitalization duration, and readmission rate within 30 days.
| Grading of postoperative pulmonary complications | |
| Grade 1 | Cough, dry Microatelectasis: Abnormal lung imaging and temperature > 37.5 ℃ without other documented cause Dyspnea |
| Grade 2 | Cough, productive |
| Bronchospasm | |
| Hypoxemia | |
| Atelectasis | |
| Hypercarbia: Requiring treatment, such as naloxone or increased manual or mechanical ventilation | |
| Grade 3 | Pleural effusion, resulting in thoracentesis |
| Pneumonia, suspected: Radiologic evidence without microbiological evidence | |
| Pneumonia, proved | |
| Pneumothorax | |
| Reintubation postoperatively, period of ventilator dependence does not exceed 48 hours | |
| Grade 4 | Ventilatory failure: Period of ventilator dependence exceeding 48 hours |
IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, United States) was used for statistical analysis. The normality of measured data was firstly examined by Kolmogorov-Smirnov test. Normally distributed continuous variables were reported as mean ± SE[28], compared between two groups using the two-sample t-test, or compared among multiple groups by analysis of variance (ANOVA). Continuous variables with non-normal distribution were reported as the median with interquartile range and were compared using the Mann-Whitney U test. Enumeration data were reported as percentages, and were compared using the χ2 test or Fisher’s exact test. Spearman’s rank correlation was used for correlation analysis. Variables with significance in the univariable analysis were further analyzed using multivariable logistic regression for ordinal categorical variables. P values less than 0.05 were considered significant.
A total of 101 patients were included in the study. Seventy-two were male, 29 were female, and the male-to-female ratio was 2.52:1. The mean age at surgery was 62.3 ± 7.2 years old. The patients’ BMI ranged from 15.92 to 28.74 kg/m2, with a mean of 23.26 ± 0.28 kg/m2. Among the included patients, 25 were classified as ASA I, 66 as ASA II, and 10 as ASA III. Twelve patients had preoperative comorbidities, including chronic obstructive pulmonary disease and bronchiectasis. Forty-eight patients had a smoking history, and 26 had a history of abdominal surgery. Three patients had ulcerative colitis and received total proctocolectomy with ileal pouch-anal anastomosis laparoscopically, seven patients received ostomy closure, and the other 91 patients received surgery for colorectal tumors. PPCs were observed in 13 patients. The mean hospitalization duration was 7.5 ± 2.2 days.
The mean peak lung ultrasound score among the 101 patients was 5.32 ± 2.51. Using a cut-off value of 6, we defined the patients with a score of ≥ 6 as the high-risk group for pulmonary conditions. Univariate logistics regression showed that a high-risk lung ultrasound score was associated with PPCs after colorectal surgery (regression coefficient, 1.715, odds ratio, 5.556, 95% confidence interval: 1.425-21.656, P = 0.013, < 0.05). Data are detailed in Table 2.
| Lung ultrasound score (n = 101) | Lung ultrasound score ≥ 6 | Regression coefficient B | Standard error | P value | OR | Lower CI | Upper CI | |
| Pre-operative | 0.47 (0.83) | 0 (0) | ||||||
| POD1 | 3.54 (2.22) | 18 (17.8) | 0.378 | 0.717 | 0.597 | 1.46 | 0.358 | 5.949 |
| POD2 | 4.64 (2.88) | 36 (35.6) | 1.232 | 0.614 | 0.045 | 3.429 | 1.029 | 11.429 |
| POD3 | 2.75 (1.86) | 6 (5.9) | 0.324 | 1.138 | 0.776 | 1.383 | 0.149 | 12.874 |
| POD4 | 1.87 (1.72) | 5 (5.0) | 2.557 | 0.972 | 0.009 | 12.9 | 1.919 | 86.703 |
| POD5 | 1.15 (1.39) | 1 (1.0) | -19.302 | 40192.97 | 1 | 0 | 0 | - |
| Mean for POD1-5 | 2.79 (1.61) | 2 (2.0) | 1.981 | 1.447 | 0.171 | 7.25 | 0.425 | 123.688 |
| Peak in POD1-5 | 5.32 (2.51) | 43 (42.6) | 1.715 | 0.694 | 0.013 | 5.556 | 1.425 | 21.656 |
The movement distance increased daily within 4 days after surgery. There was a significant difference in the distance for the 4 days (P < 0.05). The difference between movement distances on PODs 4 and 5 was not significant. In most patients, lung ultrasound scores peaked on POD 2 and then gradually decreased. There was a significant difference in the score of each day (P < 0.05). Detailed data are presented in Table 3.
| Movement distance | Lung ultrasound score | |||||||
| n = 101 | Difference from yesterday | 95%CI of mean difference | P value | n = 101 | Difference from yesterday | 95%CI of mean difference | P value | |
| POD1 | 466 (195) | 3.54 (2.22) | ||||||
| POD2 | 743 (310) | 277 (216) | (234, 319) | 0.000 | 4.64 (2.88) | 1.10 (2.54) | (0.60, 1.60) | 0.000 |
| POD3 | 1025 (347) | 281 (221) | (238, 325) | 0.000 | 2.75 (1.86) | -1.89 (1.98) | (-2.28, -1.50) | 0.000 |
| POD4 | 1212 (391) | 187 (208) | (146, 228) | 0.000 | 1.87 (1.72) | -0.88 (1.49) | (-1.18, -0.59) | 0.000 |
| POD5 | 1264 (323) | 52 (285) | (-5, 108) | 0.072 | 1.15 (1.39) | -0.72 (0.92) | (-0.90, -0.54) | 0.000 |
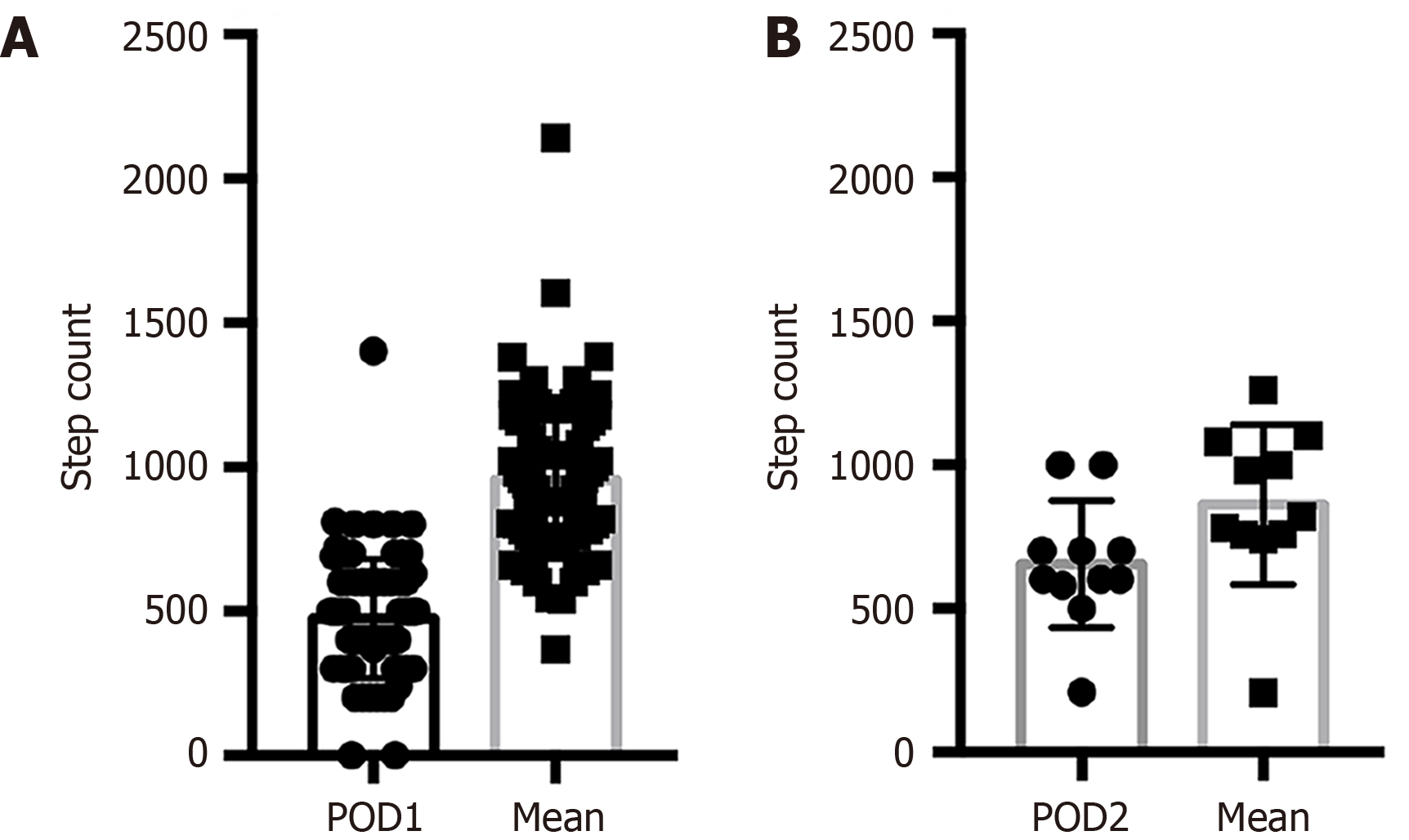
The daily change in lung ultrasound scores within 5 days after surgery suggested that 79 of the 101 patients had the largest increase (or least decrease) in score between PODs 1 and 2. In these 79 patients, the step count on POD 1 was significantly lower than the mean step count of PODs 1 to 5 (P < 0.05) (Figure 3). Eleven patients had the largest increase (or least decrease) in score between PODs 2 and 3 when the daily step count on POD 2 was significantly lower than the mean scores of PODs 1 to 5 (P < 0.05) (Figure 3).
Moreover, postoperative movement distance was negatively associated with lung ultrasound scores (r = -0.356, P < 0.05). Patients with a longer movement distance after surgery tended to have a lower lung ultrasound score and a better pulmonary outcome.
This study demonstrates that a high-risk lung ultrasound score is correlated with a higher incidence of PPCs and increased activity is correlated with a lower ultrasound score in patients who undergo colorectal surgery.
Because of the high acoustic impedance of gas, ultrasonography was not used for the lungs for a long time. In recent years, however, the understanding of ultrasound artifacts has extended the use of lung ultrasound to emergency medicine, critical care medicine, and cardiology[29]. The B line in lung ultrasound is defined as a vertical artifact spreading from the pleural line down to the bottom of the screen. A large amount of B lines is a sign of pulmonary interstitial syndrome. The B line is seen when fluid accumulates in lung parenchyma and alters the air-fluid ratio. This gives rise to a strong reverberation artifact from the air-fluid surface that can be recognized as B lines because air and fluid have different acoustic impedance[30]. Studies have shown that the B line is significantly correlated with extravascular lung water, and it has a high sensitivity for interstitial lung involvement in critical patients, such as those with pulmonary edema and interstitial fibrosis[31,32]. Through lung ultrasound, lung conditions can be promptly evaluated, and the intervention can be adjusted, helping with the recovery of patients undergoing colorectal surgery. Therefore, we first designed this prospective cohort to take advantage of smart wearable devices to monitor patients’ underground activity in real-time and quantitatively study the correlation between patients’ postoperative activity and lung ultrasound scores, predicting the incidence of PPCs.
By diagnosing many pulmonary diseases in the perioperative period, including atelectasis, pleural effusion, pulmonary edema, and pneumothorax, lung ultrasound demonstrates a similar efficiency with thoracic CT scan and a superior efficiency to CXR. Lung ultrasound also has advantages including convenience, low cost, radiation-free, and easy repetition. It can be an effective bedside evaluation method for PPCs, particularly atelectasis.
Lung ultrasound has relatively low technical and instrumental requirements. Common two-dimensional ultrasound for lung ultrasound can be accurately managed after short-term intensive training. In this study, lung ultrasonography was performed by a specially trained anesthesiologist who interpreted the scan with a trained surgeon to reduce bias in scoring. Images of the chest were recorded at 12 locations. Univariate logistic regression revealed that preoperative conditions, such as pulmonary comorbidities and smoking history, could not predict PPCs. There was no difference in significant baseline characteristics between patients with and without PPCs. The lung ultrasound score in the high-risk group was correlated with PPCs after colorectal surgery. Multivariate logistics regression showed that a lung ultrasound score of ≥ 6 is an independent risk factor for PPC. Therefore, lung ultrasound may predict the occurrence and severity of PPCs. We intend to design a randomized controlled trial to evaluate possible interventions.
Operative trauma impairs the body function of patients. Several studies have reported that preoperative decline of function level can affect the hospitalization duration and the incidence of adverse events[33]. Many researchers have recognized the importance of evaluating body function decline quantitatively after abdominal surgery. Tools of functional evaluation, such as the activities of daily living and the timed up-and-go test, have received increasing attention[33,34]. Insufficient daily activity levels of older patients can increase the risk of hospitalization and death and increase the economic burden on families and communities[35,36].
In our study, we informed patients of the advantages of early ambulation after surgery and encouraged them to increase their activity level when tolerable. The movement distance increased daily within 4 days after surgery. For most patients, the activity level increased daily with their recovery progress. The activity level peaked on POD 4, with no significant difference between PODs 4 and 5. However, most patients complained that they could not reach their preoperative activity levels.
Common reasons for a decreased postoperative activity level include pain, drainage tubes, intravenous catheters, and psychological stress. For colorectal malignancies, some studies have suggested that patients with more comorbidities and less walking distances need a longer recovery[21]. Hedrick et al[23] reported that patients with lower movement capability tended to have more postoperative complications. In the present study, postoperative movement distance was negatively associated with lung ultrasound scores. This suggests that an increased postoperative activity level may reduce the pulmonary fluid volume and prevent PPCs.
Our study had some limitations. First, it was a single-center study. Future studies should include more patients and centers to improve the quality of evidence. Second, considering the adherence, tolerability, and safety of patients, we did not conduct repeat ultrasonography by different personnel. To minimize the bias in scoring, only one specialist performed all examinations and interpreted the results with a surgeon. Third, ultrasonography was performed at the same time in the afternoon. Patients who underwent surgery in the morning and the afternoon had a difference in their recovery time by several hours. Finally, most patients in this study had CRC. The pattern of ultrasonography and postoperative ambulation may vary in different diseases, and this warrants further investigation.
To our knowledge, this is the first prospective study to use lung ultrasound in the quantitative pulmonary evaluation of patients after colorectal surgery. It is also the first correlational study to use wearable devices to monitor the perioperative activity level in real-time and investigate its relationship with lung ultrasound. Lung ultrasound can effectively evaluate pulmonary condition after colorectal surgery. The daily ambulation distance can affect the lung ultrasound score. Increased activity was associated with a lower lung ultrasound score and better pulmonary condition. In the first 2 days after colorectal surgery, patients should be encouraged to commence ambulation and respiratory function exercise early, especially for those with a lung ultrasound score of ≥ 6. These strategies may prevent PPCs and other complications after colorectal surgery, especially in patients with CRC.
We sincerely thank all the patients for their cooperation. We also thank the surgeons, physician, nurses, technical staff, and hospital administration for their contributions to this study. Moreover, we thank Dr. Wu for the advice and support.
| 1. | Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2279] [Cited by in RCA: 4709] [Article Influence: 4709.0] [Reference Citation Analysis (3)] |
| 2. | He S, Xia C, Li H, Cao M, Yang F, Yan X, Zhang S, Teng Y, Li Q, Chen W. Cancer profiles in China and comparisons with the USA: a comprehensive analysis in the incidence, mortality, survival, staging, and attribution to risk factors. Sci China Life Sci. 2024;67:122-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 89.0] [Reference Citation Analysis (0)] |
| 3. | Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum. 2005;48:2070-2075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 4. | Shariq OA, Hanson KT, McKenna NP, Kelley SR, Dozois EJ, Lightner AL, Mathis KL, Habermann EB. Does Metabolic Syndrome Increase the Risk of Postoperative Complications in Patients Undergoing Colorectal Cancer Surgery? Dis Colon Rectum. 2019;62:849-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Nikolian VC, Kamdar NS, Regenbogen SE, Morris AM, Byrn JC, Suwanabol PA, Campbell DA Jr, Hendren S. Anastomotic leak after colorectal resection: A population-based study of risk factors and hospital variation. Surgery. 2017;161:1619-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 6. | Husain F, Jeong IH, Spight D, Wolfe B, Mattar SG. Risk factors for early postoperative complications after bariatric surgery. Ann Surg Treat Res. 2018;95:100-110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Patel K, Hadian F, Ali A, Broadley G, Evans K, Horder C, Johnstone M, Langlands F, Matthews J, Narayan P, Rallon P, Roberts C, Shah S, Vohra R. Postoperative pulmonary complications following major elective abdominal surgery: a cohort study. Perioper Med (Lond). 2016;5:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Damian D, Esquenazi J, Duvvuri U, Johnson JT, Sakai T. Incidence, outcome, and risk factors for postoperative pulmonary complications in head and neck cancer surgery patients with free flap reconstructions. J Clin Anesth. 2016;28:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Abd El Aziz MA, Perry WR, Grass F, Mathis KL, Larson DW, Mandrekar J, Behm KT. Predicting primary postoperative pulmonary complications in patients undergoing minimally invasive surgery for colorectal cancer. Updates Surg. 2020;72:977-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Xue FS, Li BW, Zhang GS, Liao X, Zhang YM, Liu JH, An G, Luo LK. The influence of surgical sites on early postoperative hypoxemia in adults undergoing elective surgery. Anesth Analg. 1999;88:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung Ultrasound for Critically Ill Patients. Am J Respir Crit Care Med. 2019;199:701-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 277] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 12. | Picano E, Pellikka PA. Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J. 2016;37:2097-2104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 286] [Cited by in RCA: 284] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 13. | Brusasco C, Santori G, Bruzzo E, Trò R, Robba C, Tavazzi G, Guarracino F, Forfori F, Boccacci P, Corradi F. Quantitative lung ultrasonography: a putative new algorithm for automatic detection and quantification of B-lines. Crit Care. 2019;23:288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 14. | Ciumanghel A, Siriopol I, Blaj M, Siriopol D, Gavrilovici C, Covic A. B-lines score on lung ultrasound as a direct measure of respiratory dysfunction in ICU patients with acute kidney injury. Int Urol Nephrol. 2018;50:113-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Yu X, Zhai Z, Zhao Y, Zhu Z, Tong J, Yan J, Ouyang W. Performance of Lung Ultrasound in Detecting Peri-Operative Atelectasis after General Anesthesia. Ultrasound Med Biol. 2016;42:2775-2784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Bajracharya SM, Shrestha P, Sharma A. Comparison of Lung Ultrasound to X-ray for Diagnosis of Pulmonary Complications after Cardiac Surgery in Children. J Nepal Health Res Counc. 2020;18:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Touw HR, Parlevliet KL, Beerepoot M, Schober P, Vonk A, Twisk JW, Elbers PW, Boer C, Tuinman PR. Lung ultrasound compared with chest X-ray in diagnosing postoperative pulmonary complications following cardiothoracic surgery: a prospective observational study. Anaesthesia. 2018;73:946-954. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | Cantinotti M, Giordano R, Volpicelli G, Kutty S, Murzi B, Assanta N, Gargani L. Lung ultrasound in adult and paediatric cardiac surgery: is it time for routine use? Interact Cardiovasc Thorac Surg. 2016;22:208-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | From the American Association of Neurological Surgeons (AANS); American Society of Neuroradiology (ASNR), Cardiovascular and Interventional Radiology Society of Europe (CIRSE); Canadian Interventional Radiology Association (CIRA); Congress of Neurological Surgeons (CNS), European Society of Minimally Invasive Neurological Therapy (ESMINT), European Society of Neuroradiology (ESNR); European Stroke Organization (ESO); Society for Cardiovascular Angiography and Interventions (SCAI), Society of Interventional Radiology (SIR), Society of NeuroInterventional Surgery (SNIS); and World Stroke Organization (WSO); Sacks D, Baxter B, Campbell BCV, Carpenter JS, Cognard C, Dippel D, Eesa M, Fischer U, Hausegger K, Hirsch JA, Shazam Hussain M, Jansen O, Jayaraman MV, Khalessi AA, Kluck BW, Lavine S, Meyers PM, Ramee S, Rüfenacht DA, Schirmer CM, Vorwerk D. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int J Stroke. 2018;13:612-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 348] [Reference Citation Analysis (0)] |
| 20. | Ni X, Jia D, Chen Y, Wang L, Suo J. Is the Enhanced Recovery After Surgery (ERAS) Program Effective and Safe in Laparoscopic Colorectal Cancer Surgery? A Meta-Analysis of Randomized Controlled Trials. J Gastrointest Surg. 2019;23:1502-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 21. | Abeles A, Kwasnicki RM, Pettengell C, Murphy J, Darzi A. The relationship between physical activity and post-operative length of hospital stay: A systematic review. Int J Surg. 2017;44:295-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Minnella EM, Awasthi R, Gillis C, Fiore JF Jr, Liberman AS, Charlebois P, Stein B, Bousquet-Dion G, Feldman LS, Carli F. Patients with poor baseline walking capacity are most likely to improve their functional status with multimodal prehabilitation. Surgery. 2016;160:1070-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 23. | Hedrick TL, Hassinger TE, Myers E, Krebs ED, Chu D, Charles AN, Hoang SC, Friel CM, Thiele RH. Wearable Technology in the Perioperative Period: Predicting Risk of Postoperative Complications in Patients Undergoing Elective Colorectal Surgery. Dis Colon Rectum. 2020;63:538-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 24. | Low CA, Bovbjerg DH, Ahrendt S, Choudry MH, Holtzman M, Jones HL, Pingpank JF Jr, Ramalingam L, Zeh HJ 3rd, Zureikat AH, Bartlett DL. Fitbit step counts during inpatient recovery from cancer surgery as a predictor of readmission. Ann Behav Med. 2018;52:88-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 25. | Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014;12:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 234] [Cited by in RCA: 222] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 26. | Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med. 2011;183:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 420] [Cited by in RCA: 485] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 27. | Kroenke K, Lawrence VA, Theroux JF, Tuley MR. Operative risk in patients with severe obstructive pulmonary disease. Arch Intern Med. 1992;152:967-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 121] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | Tang L, Zhang H, Zhang B. A note on error bars as a graphical representation of the variability of data in biomedical research: Choosing between standard deviation and standard error of the mean. J Pancreatol. 2019;2:69-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé-Violán J, López-Rodríguez M, Herrera-Ramos E, Ruíz-Hernández J, Borderías L, Horcajada J, González-Quevedo N, Rajas O, Briones M, Rodríguez de Castro F, Rodríguez Gallego C, Esen F, Orhun G, Ergin Ozcan P, Senturk E, Ugur Yilmaz C, Orhan N, Arican N, Kaya M, Kucukerden M, Giris M, Akcan U, Bilgic Gazioglu S, Tuzun E, Riff R, Naamani O, Douvdevani A, Takegawa R, Yoshida H, Hirose T, Yamamoto N, Hagiya H, Ojima M, Akeda Y, Tasaki O, Tomono K, Shimazu T, Ono S, Kubo T, Suda S, Ueno T, Ikeda T, Hirose T, Ogura H, Takahashi H, Ojima M, Kang J, Nakamura Y, Kojima T, Shimazu T, Ikeda T, Suda S, Izutani Y, Ueno T, Ono S, Taniguchi T, O M, Dinter C, Lotz J, Eilers B, Wissmann C, Lott R, Meili MM, Schuetz PS, Hawa H, Sharshir M, Aburageila M, Salahuddin N, Chantziara V, Georgiou S, Tsimogianni A, Alexandropoulos P, Vassi A, Lagiou F, Valta M, Micha G, Chinou E, Michaloudis G, Kodaira A, Ikeda T, Ono S, Ueno T, Suda S, Izutani Y, Imaizumi H, De la Torre-Prados MV, Garcia-De la Torre A, Enguix-Armada A, Puerto-Morlan A, Perez-Valero V, Garcia-Alcantara A, Bolton N, Dudziak J, Bonney S, Tridente A, Nee P, Nicolaes G, Wiewel M, Schultz M, Wildhagen K, Horn J, Schrijver R, Van der Poll T, Reutelingsperger C, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Gayat EG, Struck J, Cariou A, Deye N, Guidet B, Jabert S, Launay J, Legrand M, Léone M, Resche-Rigon M, Vicaut E, Vieillard-Baron A, Mebazaa A, Arnold R, Capan M, Linder A, Akesson P, Popescu M, Tomescu D, Sprung CL, Calderon Morales R, Munteanu G, Orenbuch-Harroch E, Levin P, Kasdan H, Reiter A, Volker T, Himmel Y, Cohen Y, Meissonnier J, Girard L, Rebeaud F, Herrmann I, Delwarde B, Peronnet E, Cerrato E, Venet F, Lepape A, Rimmelé T, Monneret G, Textoris J, Beloborodova N, Moroz V, Osipov A, Bedova A, Sarshor Y, Pautova A, Sergeev A, Chernevskaya E, Odermatt J, Bolliger R, Hersberger L, Ottiger M, Christ-Crain M, Mueller B, Schuetz P, Sharma NK, Tashima AK, Brunialti MK, Machado FR, Assuncao M, Rigato O, Salomao R, Cajander SC, Rasmussen G, Tina E, Söderquist B, Källman J, Strålin K, Lange AL, Sundén-Cullberg JS, Magnuson AM, Hultgren OH, Davies G, Pillai S, Mills G, Aubrey R, Morris K, Williams P, Evans P, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Van der Geest P, Mohseni M, Linssen J, De Jonge R, Duran S, Groeneveld J, Miller R III, Lopansri BK, McHugh LC, Seldon A, Burke JP, Johnston J, Reece-Anthony R, Bond A, Molokhia A, Mcgrath C, Nsutebu E, Bank Pedersen P, Pilsgaard Henriksen D, Mikkelsen S, Touborg Lassen A, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Wiewel MA, Harmon MB, Van Vught LA, Scicluna BP, Hoogendijk AJ, Horn J, Zwinderman AH, Cremer OL, Bonten MJ, Schultz MJ, Van der Poll T, Juffermans NP, Wiersinga WJ, Eren G, Tekdos Y, Dogan M, Acicbe O, Kaya E, Hergunsel O, Alsolamy S, Ghamdi G, Alswaidan L, Alharbi S, Alenezi F, Arabi Y, Heaton J, Boyce A, Nolan L, Johnston J, Dukoff-Gordon A, Dean A, Molokhia A, Mann Ben Yehudah T, Fleischmann C, Thomas-Rueddel D, Haas C, Dennler U, Reinhart K, Suntornlohanakul O, Khwannimit B, Breckenridge F, Puxty A, Szturz P, Folwarzcny P, Svancara J, Kula R, Sevcik P, Caneva L, Casazza A, Bellazzi E, Marra S, Pagani L, Vetere M, Vanzino R, Ciprandi D, Preda R, Boschi R, Carnevale L, Lopez V, Aguilar Arzapalo M, Barradas L, Escalante A, Gongora J, Cetina M, Adamik B, Jakubczyk D, Kübler A, Radford A, Lee T, Singer J, Boyd J, Fineberg D, Williams M, Russell J, Scarlatescu E, Tomescu D, Droc G, Arama S, Müller M, Straat M, Zeerleder SS, Juffermans NP, Fuchs CF, Scheer CS, Wauschkuhn SW, Vollmer MV, Meissner KM, Kuhn SK, Hahnenkamp KH, Rehberg SR, Gründling MG, Yamamoto N, Ojima M, Hamaguchi S, Hirose T, Akeda Y, Takegawa R, Tasaki O, Shimazu T, Tomono K, Gómez-Sánchez E, Heredia-Rodríguez M, Álvarez-Fuente E, Lorenzo-López M, Gómez-Pesquera E, Aragón-Camino M, Liu-Zhu P, Sánchez-López A, Hernández-Lozano A, Peláez-Jareño MT, Tamayo E, Thomas-Rüddel DO, Fleischmann C, Haas C, Dennler U, Reinhart K, Adora V, Kar A, Chakraborty A, Roy S, Bandyopadhyay A, Das M, Mann Ben Yehudah T, BenYehudah G, Salim M, Kumar N, Arabi L, Burger T, Lephart P, Toth-martin E, Valencia C, Hammami N, Blot S, Vincent JL, Lambert ML, Brunke J, Riemann T, Roschke I, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Nimitvilai S, Jintanapramote K, Jarupongprapa S, Adukauskiene D, Valanciene D, Bose G, Lostarakos V, Carr B, Khedher S, Maaoui A, Ezzamouri A, Salem M, Chen J, Cranendonk DR, Van Vught LA, Wiewel MA, Cremer OL, Horn J, Bonten MJ, Schultz MJ, Van der Poll T, Wiersinga WJ, Day M, Penrice G, Roy K, Robertson P, Godbole G, Jones B, Booth M, Donaldson L, Kawano Y, Ishikura H, Al-Dorzi H, Almutairi M, Alhamadi B, Crizaldo Toledo A, Khan R, Al Raiy B, Arabi Y, Talaie H, Van Oers JA, Harts A, Nieuwkoop E, Vos P, Boussarsar Y, Boutouta F, Kamoun S, Mezghani I, Koubaji S, Ben Souissi A, Riahi A, Mebazaa MS, Giamarellos-Bourboulis E, Tziolos N, Routsi C, Katsenos C, Tsangaris I, Pneumatikos I, Vlachogiannis G, Theodorou V, Prekates A, Antypa E, Koulouras V, Kapravelos N, Gogos C, Antoniadou E, Mandragos K, Armaganidis A, Robles Caballero AR, Civantos B, Figueira JC, López J, Silva-Pinto A, Ceia F, Sarmento A, Santos L, Almekhlafi G, Sakr Y, Al-Dorzi H, Khan R, Baharoon S, Aldawood A, Matroud A, Alchin J, Al Johani S, Balkhy H, Arabi Y, Alsolamy S, Yousif SY, Alotabi BO, Alsaawi AS, Ang J, Curran MD, Enoch D, Navapurkar V, Morris A, Sharvill R, Astin J, Heredia-Rodríguez M, Gómez-Sánchez E, Peláez-Jareño MT, Gómez-Pesquera E, Lorenzo-López M, Liu-Zhu P, Aragón-Camino M, Hernández-Lozano A, Sánchez-López A, Álvarez-Fuente E, Tamayo E, Patel J, Kruger C, O’Neal J, Rhodes H, Jancik J, François B, Laterre PF, Eggimann P, Torres A, Sánchez M, Dequin PF, Bassi GL, Chastre J, Jafri HS, Ben Romdhane M, Douira Z, Kamoun S, Bousselmi M, Ben Souissi A, Boussarsar Y, Riahi A, Mebazaa MS, Vakalos A, Avramidis V, Craven TH, Wojcik G, Kefala K, McCoubrey J, Reilly J, Paterson R, Inverarity D, Laurenson I, Walsh TS, Mongodi S, Bouhemad B, Orlando A, Stella A, Via G, Iotti G, Braschi A, Mojoli F, Haliloglu M, Bilgili B, Kasapoglu U, Sayan I, Süzer Aslan M, Yalcın A, Cinel I, Vakalos A, Avramidis V, Ellis HE, Bauchmuller K, Miller D, Temple A, Chastre J, François B, Torres A, Luyt CE, Sánchez M, Singer M, Jafri HS, Nassar Y, Ayad MS, Trifi A, Abdellatif S, Daly F, Nasri R, Ben Lakhal S, Bilgili B, Haliloglu M, Gul F, Cinel I, Kuzovlev A, Shabanov A, Polovnikov S, Moroz V, Kadrichu N, Dang T, Corkery K, Challoner P, Bassi GL, Aguilera E, Chiurazzi C, Travierso C, Motos A, Fernandez L, Amaro R, Senussi T, Idone F, Bobi J, Rigol M, Torres A, Hodiamont CJ, Juffermans NP, Janssen JM, Bouman CS, Mathôt RA, De Jong MD, Van Hest RM, Payne L, Fraser GL, Tudor B, Lahner M, Roth G, Krenn C, Talaie H, Jault P, Gabard J, Leclerc T, Jennes S, Que Y, Rousseau A, Ravat F, Al-Dorzi H, Eissa A, Al-Harbi S, Aldabbagh T, Khan R, Arabi Y, Trifi A, Abdellatif. S, Daly F, Nasri R, Ben Lakhal S, Paramba F, Purayil N, Naushad V, Mohammad O, Negi V, Chandra P, Kleinsasser A, Witrz MR, Buchner-Doeven JF, Tuip-de Boer AM, Goslings JC, Juffermans NP, Van Hezel M, Straat M, Boing A, Van Bruggen R, Juffermans N, Markopoulou D, Venetsanou K, Kaldis V, Koutete D, Chroni D, Alamanos I, Koch L, Jancik J, Rhodes H, Walter E, Maekawa K, Hayakawa M, Kushimoto S, Shiraishi A, Kato H, Sasaki J, Ogura H, Matauoka T, Uejima T, Morimura N, Ishikura H, Hagiwara A, Takeda M, Tarabrin O, Shcherbakow S, Gavrychenko D, Mazurenko G, Ivanova V, Chystikov O, Plourde C, Lessard J, Chauny J, Daoust R, Shcherbakow S, Tarabrin O, Gavrychenko D, Mazurenko G, Chystikov O, Vakalos A, Avramidis V, Kropman L, In het Panhuis L, Konings J, Huskens D, Schurgers E, Roest M, De Laat B, Lance M, Durila M, Lukas P, Astraverkhava M, Jonas J, Budnik I, Shenkman B, Hayami H, Koide Y, Goto T, Iqbal R, Alhamdi Y, Venugopal N, Abrams S, Downey C, Toh CH, Welters ID, Bombay VB, Chauny JM, Daoust RD, Lessard JL, Marquis MM, Paquet JP, Siemens K, Sangaran D, Hunt BJ, Durward A, Nyman A, Murdoch IA, Tibby SM, Ampatzidou F, Moisidou D, Dalampini E, Nastou M, Vasilarou E, Kalaizi V, Chatzikostenoglou H, Drossos G, Spadaro S, Fogagnolo A, Fiore T, Schiavi A, Fontana V, Taccone F, Volta C, Chochliourou E, Volakli E, Violaki A, Samkinidou E, Evlavis G, Panagiotidou V, Sdougka M, Mothukuri R, Battle C, Guy K, Mills G, Evans P, Wijesuriya J, Keogh S, Docherty A, O’Donnell R, Brunskill S, Trivella M, Doree C, Holst L, Parker M, Gregersen M, Almeida J, Walsh T, Stanworth S, Moravcova S, Mansell J, Rogers A, Smith RA, Hamilton-Davies C, Omar A, Allam M, Bilala O, Kindawi A, Ewila H, Ampatzidou F, Moisidou D, Nastou M, Dalampini E, Malamas A, Vasilarou E, Drossos G, Ferreira G, Caldas J, Fukushima J, Osawa EA, Arita E, Camara L, Zeferino S, Jardim J, Gaioto F, Dallan L, Jatene FB, Kalil Filho R, Galas F, Hajjar LA, Mitaka C, Ohnuma T, Murayama T, Kunimoto F, Nagashima M, Takei T, Tomita M, Omar A, Mahmoud K, Hanoura S, Sudarsanan S, Sivadasan P, Othamn H, Shouman Y, Singh R, Al Khulaifi A, Mandel I, Mikheev S, Suhodolo I, Kiselev V, Svirko Y, Podoksenov Y, Jenkins SA, Griffin R, Tovar Doncel MS, Lima A, Aldecoa C, Ince C, Taha A, Shafie A, Mostafa M, Syed N, Hon H, Righetti F, Colombaroli E, Castellano G, Righetti F, Colombaroli E, Hravnak M, Chen LC, Dubrawski AD, Clermont GC, Pinsky MR, Gonzalez S, Macias D, Acosta J, Jimenez P, Loza A, Lesmes A, Lucena F, Leon C, Tovar Doncel MS, Ince C, Aldecoa C, Lima A, Bastide M, Richecoeur J, Frenoy E, Lemaire C, Sauneuf B, Tamion F, Nseir S, Du Cheyron D, Dupont H, Maizel J, Shaban M, Kolko R, Salahuddin N, Sharshir M, AbuRageila M, AlHussain A, Mercado P, Maizel J, Kontar L, Titeca D, Brazier F, Riviere A, Joris M, Soupison T, De Cagny B, Slama M, Wagner J, Körner A, Kubik M, Kluge S, Reuter D, Saugel B, Colombaroli E, Righetti F, Castellano G, Tran T, De Bels D, Cudia A, Strachinaru M, Ghottignies P, Devriendt J, Pierrakos C, Martínez González Ó, Blancas R, Luján J, Ballesteros D, Martínez Díaz C, Núñez A, Martín Parra C, López Matamala B, Alonso Fernández M, Chana M, Huber W, Eckmann M, Elkmann F, Gruber A, Klein I, Schmid RM, Lahmer T, Moller PW, Sondergaard S, Jakob SM, Takala J, Berger D, Bastoni D, Aya H, Toscani L, Pigozzi L, Rhodes A, Cecconi M, Ostrowska C, Aya H, Abbas A, Mellinghoff J, Ryan C, Dawson D, Rhodes A, Cecconi M, Cronhjort M, Wall O, Nyberg E, Zeng R, Svensen C, Mårtensson J, Joelsson-Alm E, Aguilar Arzapalo M, Barradas L, Lopez V, Cetina M, Parenti N, Palazzi C, Amidei LA, Borrelli FB, Campanale SC, Tagliazucchi FT, Sedoni GS, Lucchesi DL, Carella EC, Luciani AL, Mackovic M, Maric N, Bakula M, Aya H, Rhodes A, Grounds RM, Fletcher N, Cecconi M, Avard B, Zhang P, Mezidi M, Charbit J, Ould-Chikh M, Deras P, Maury C, Martinez O, Capdevila X, Hou P, Linde-Zwirble WZ, Douglas ID, Shapiro NS, Ben Souissi A, Mezghani I, Ben Aicha Y, Kamoun S, Laribi B, Jeribi B, Riahi A, Mebazaa MS, Pereira C, Marinho R, Antunes R, Marinho A, Crivits M, Raes M, Decruyenaere J, Hoste E, Bagin V, Rudnov V, Savitsky A, Astafyeva M, Korobko I, Vein V, Kampmeier T, Arnemann P, Hessler M, Wald A, Bockbreder K, Morelli A, Van Aken H, Rehberg S, Ertmer C, Arnemann P, Hessler M, Kampmeier T, Rehberg S, Van Aken H, Ince C, Ertmer C, Reddy S, Bailey M, Beasley R, Bellomo R, Mackle D, Psirides A, Young P, Reddy S, Bailey M, Beasley R, Bellomo R, Mackle D, Young P, Venkatesh H, Ramachandran S, Basu A, Nair H, Egan S, Bates J, Oliveira S, Rangel Neto NR, Reis FQ, Lee CP, Lin XL, Choong C, Eu KM, Sim WY, Tee KS, Pau J, Abisheganaden J, Maas K, De Geus H, Lafuente E, Marinho R, Moura J, Antunes R, Marinho A, Doris TE, Monkhouse D, Shipley T, Kardasz S, Gonzalez I, Stads S, Groeneveld AJ, Elsayed I, Ward N, Tridente A, Raithatha A, Steuber A, Pelletier C, Schroeder S, Michael E, Slowinski T, Kindgen-Milles D, Ghabina S, Turani F, Belli A, Busatti S, Barettin G, Candidi F, Gargano F, Barchetta R, Falco M, Demirkiran O, Kosuk M, Bozbay S, Weber V, Hartmann J, Harm S, Linsberger I, Eichhorn T, Valicek G, Miestinger G, Hoermann C, Faenza S, Ricci D, Mancini E, Gemelli C, Cuoghi A, Magnani S, Atti M, Laddomada T, Doronzio A, Balicco B, Gruda MC, O’Sullivan P, Dan VP, Guliashvili T, Scheirer A, Golobish TD, Capponi VJ, Chan PP, Kogelmann K, Drüner M, Jarczak D, Turani F, Belli AB, Martni SM, Cotticelli VC, Mounajergi F, Barchetta R, Morimoto S, Ishikura H, Hussain I, Salahuddin N, Nadeem A, Ghorab K, Maghrabi K, Kloesel SK, Goldfuss C, Stieglitz A, Stieglitz AS, Krstevska L, Albuszies G, Aguilar Arzapalo M, Barradas L, Lopez V, Escalante A, Jimmy G, Cetina M, Izawa J, Iwami T, Uchino S, Takinami M, Kitamura T, Kawamura T, Powell-Tuck JG, Crichton S, Raimundo M, Camporota L, Wyncoll D, Ostermann M, Hana A, De Geus HR, De Geus HR, Hana A, Aydogdu M, Boyaci N, Yuksel S, Gursel G, Cayci Sivri AB, Meza-Márquez J, Nava-López J, Carrillo-Esper R, Dardashti A, Grubb A, Maizel J, Wetzstein M, Titeca D, Kontar L, Brazier F, De Cagny B, Riviere A, Soupison T, Joris M, Slama M, Peters E, Njimi H, Pickkers P, Vincent JL, Waraich M, Doyle J, Samuels T, Forni L, Desai N, Baumber R, Gunning P, Sell A, Lin S, Torrence H, O’Dwyer M, Kirwan C, Prowle J, Kim T, O’Connor ME, Hewson RW, Kirwan CJ, Pearse RM, Prowle J, Hanoura S, Omar A, Othamn H, Sudarsanan S, Allam M, Maksoud M, Singh R, Al Khulaifi A, O’Connor ME, Hewson RW, Kirwan CJ, Pearse RM, Prowle J, Uzundere O, Memis D, Ýnal M, Gultekin A, Turan N, Aydin MA, Basar H, Sencan I, Kapuagasi A, Ozturk M, Uzundurukan Z, Gokmen D, Ozcan A, Kaymak C, Artemenko VA, Budnyuk A, Pugh R, Bhandari S, Mauri T, Turrini C, Langer T, Taccone P, Volta CA, Marenghi C, Gattinoni L, Pesenti A, Sweeney L, O’Sullivan A, Kelly P, Mukeria E, MacLoughlin R, Pfeffer M, Thomas JT, Bregman GB, Karp GK, Kishinevsky EK, Stavi DS, Adi NA, Poropat T, Knafelj R, Llopart E, Batlle M, De Haro C, Mesquida J, Artigas A, Pavlovic D, Lewerentz L, Spassov A, Schneider R, De Smet S, De Raedt S, Derom E, Depuydt P, Oeyen S, Benoit D, Decruyenaere J, Gobatto A, Besen B, Tierno P, Melro L, Mendes P, Cadamuro F, Park M, Malbouisson LM, Civantos BC, Lopez JL, Robles A, Figueira J, Yus S, Garcia A, Oglinda A, Ciobanu G, Oglinda C, Schirca L, Sertinean T, Lupu V, Kelly P, O’Sullivan A, Sweeney L, MacLoughlin R, O’Sullivan A, Kelly P, Sweeney L, Mukeria E, Wolny M, MacLoughlin R, Pagano A, Numis F, Visone G, Saldamarco L, Russo T, Porta G, Paladino F, Bell C, Liu J, Debacker J, Lee C, Tamberg E, Campbell V, Mehta S, Silva-Pinto A, Sarmento A, Santos L, Kara Ý, Yýldýrým F, Zerman A, Güllü Z, Boyacý N, Basarýk Aydogan B, Gaygýsýz Ü, Gönderen K, Arýk G, Turkoglu M, Aydogdu M, Aygencel G, Ülger Z, Gursel G, Boyacý N, Isýkdogan Z, Özdedeoglu Ö, Güllü Z, Badoglu M, Gaygýsýz U, Aydogdu M, Gursel G, Kongpolprom N, Sittipunt C, Eden A, Kokhanovsky Y, Bursztein – De Myttenaere S, Pizov R, Neilans L, MacIntyre N, Radosevich M, Wanta B, Weber V, Meyer T, Smischney N, Brown D, Diedrich D, Fuller A, McLindon P, Sim K, Shoaeir M, Noeam K, Mahrous A, Matsa R, Ali A, Dridi C, Koubaji S, Kamoun S, Haddad F, Ben Souissi A, Laribi B, Riahi A, Mebazaa MS, Pérez-Calatayud A, Carrillo-Esper R, Zepeda-Mendoza A, Diaz-Carrillo M, Arch-Tirado E, Carbognin S, Pelacani L, Zannoni F, Agnoli A, Gagliardi G, Cho R, Adams A, Lunos S, Ambur S, Shapiro R, Prekker M, Thijssen M, Janssen L, Foudraine N, Voscopoulos CJ, Freeman J, Voscopoulos CJ, Freeman J, George E, Voscopoulos CJ, Eversole D, Freeman J, George E, Muttini S, Bigi R, Villani G, Patroniti N, Williams G, Voscopoulos CJ, Freeman J, George E, Waldmann A, Böhm S, Windisch W, Strassmann S, Karagiannidis C, Waldmann A, Böhm S, Windisch W, Strassmann S, Karagiannidis C, Karagiannidis CK, Waldmann AW, Böhm SB, Strassmann S, Windisch WW, Persson P, Lundin S, Stenqvist O, Porta G, Numis F, Serra CS, Pagano AP, Masarone MM, Rinaldi LR, Amelia AA, Fascione MF, Adinolfi LA, Ruggiero ER, Asota F, O’Rourke K, Ranjan S, Morgan P, DeBacker JW, Tamberg E, O’Neill L, Munshi L, Burry L, Fan E, Mehta S, Poo S, Mahendran K, Fowles J, Gerrard C, Vuylsteke A, Loveridge R, Chaddock C, Patel S, Kakar V, Willars C, Hurst T, Park C, Best T, Vercueil A, Auzinger G, Borgman A, Proudfoot AG, Grins E, Emiley KE, Schuitema J, Fitch SJ, Marco G, Sturgill J, Dickinson MG, Strueber M, Khaghani A, Wilton P, Jovinge SM, Sampson C, Harris-Fox S, Cove ME, Vu LH, Sen A, Federspiel WJ, Kellum JA, Mazo Torre C, Riera J, Ramirez S, Borgatta B, Lagunes L, Rello J, Kuzovlev AK, Moroz V, Goloubev A, Polovnikov S, Nenchuk S, Karavana V, Glynos C, Asimakos A, Pappas K, Vrettou C, Magkou M, Ischaki E, Stathopoulos G, Zakynthinos S, Spadaro S, Kozhevnikova I, Dalla Corte F, Grasso S, Casolari P, Caramori G, Volta C, Andrianjafiarinoa T, Randriamandrato T, Rajaonera T, El-Dash S, Costa ELV, Tucci MR, Leleu F, Kontar L, De Cagny B, Brazier F, Titeca D, Bacari-Risal G, Maizel J, Amato M, Slama M, Mercado P, Maizel J, Kontar L, Titeca D, Brazier F, Riviere A, Joris M, Soupison T, De Cagny B, El Dash S, Slama M, Remmington, Fischer A, Squire S, Boichat M, Honzawa H, Yasuda H, Adati T, Suzaki S, Horibe M, Sasaki M, Sanui M, Marinho R, Daniel J, Miranda H, Marinho A, Milinis K, Cooper M, Williams GR, McCarron E, Simants S, Patanwala I, Welters I, Su Y, Fernández Villanueva J, Fernández Garda R, López Lago A, Rodríguez Ruíz E, Hernández Vaquero R, Tomé Martínez de Rituerto S, Varo Pérez E, Lefel N, Schaap F, Bergmans D, Olde Damink S, Van de Poll M, Tizard K, Lister C, Poole L, Ringaitiene D, Gineityte D, Vicka V, Norkiene I, Sipylaite J, O’Loughlin A, Maraj V, Dowling J, Velasco MB, Dalcomune DM, Dias EB, Fernandes SL, Oshima T, Graf S, Heidegger C, Genton L, Karsegard V, Dupertuis Y, Pichard C, Friedli N, Stanga Z, Mueller B, Schuetz P, Vandersteen L, Stessel B, Evers S, Van Assche A, Jamaer L, Dubois J, Marinho R, Castro H, Moura J, Valente J, Martins P, Casteloes P, Magalhaes C, Cabral S, Santos M, Oliveira B, Salgueiro A, Marinho A, Marinho R, Santos M, Lafuente E, Castro H, Cabral S, Moura J, Martins P, Oliveira B, Salgueiro A, Duarte S, Castro S, Melo M, Casteloes P, Marinho A, Gray S, Maipang K, Bhurayanontachai R, Grädel LG, Schütz P, Langlois P, Manzanares W, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Manzanares W, Langlois P, Lemieux M, Elke G, Bloos F, Reinhart K, Heyland D, Langlois P, Lemieux M, Aramendi I, Heyland D, Manzanares W, Su Y, Marinho R, Babo N, Marinho A, Hoshino M, Haraguchi Y, Kajiwara S, Mitsuhashi T, Tsubata T, Aida M, Rattanapraphat T, Bhurayanontachai R, Kongkamol C, Khwannimit B, Marinho R, Santos M, Castro H, Lafuente E, Salgueiro A, Cabral S, Martins P, Moura J, Oliveira B, Melo M, Xavier B, Valente J, Magalhaes C, Casteloes P, Marinho A, Moisidou D, Ampatzidou F, Koutsogiannidis C, Moschopoulou M, Drossos G, Taskin G, Çakir M, Güler AK, Taskin A, Öcal N, Özer S, Yamanel L, Wong JM, Fitton C, Anwar S, Stacey S, Aggou M, Fyntanidou B, Patsatzakis S, Oloktsidou E, Lolakos K, Papapostolou E, Grosomanidis V, Suda S, Ikeda T, Ono S, Ueno T, Izutani Y, Gaudry S, Desailly V, Pasquier P, Brun PB, Tesnieres AT, Ricard JD, Dreyfuss D, Mignon A, White JC, Molokhia A, Dean A, Stilwell A, Friedlaender G, Peters M, Stipulante S, Delfosse A, Donneau AF, Ghuysen A, Feldmann C, Freitag D, Dersch W, Irqsusi M, Eschbach D, Steinfeldt T, Wulf H, Wiesmann T, Kongpolprom N, Cholkraisuwat J, Beitland S, Nakstad E, Stær-Jensen H, Drægni T, Andersen G, Jacobsen D, Brunborg C, Waldum-Grevbo B, Sunde K, Hoyland K, Pandit D, Hayakawa K, Oloktsidou E, Kotzampassi K, Fyntanidou B, Patsatzakis S, Loukipoudi L, Doumaki E, Grosomanidis V, Yasuda H, Admiraal MM, Van Assen M, Van Putten MJ, Tjepkema-Cloostermans M, Van Rootselaar AF, Horn J, Ragusa F, Marudi A, Baroni S, Gaspari A, Bertellini E, Taha A, Abdullah T, Abdel Monem S, Alcorn S, McNeill S, Russell S, Eertmans W, Genbrugge C, Meex I, Dens J, Jans F, De Deyne C, Cholkraisuwat J, Kongpolprom N, Avard B, Burns R, Patarchi A, Spina T, Tanaka H, Otani N, Ode S, Ishimatsu S, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Won MH, Dakova S, Ramsheva Z, Ramshev K, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Marudi A, Baroni S, Gaspari A, Bertellini E, Orhun G, Senturk E, Ozcan PE, Sencer S, Ulusoy C, Tuzun E, Esen F, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Van Assen M, Admiraal MM, Van Putten MJ, Tjepkema-Cloostermans M, Van Rootselaar AF, Horn J, Fallenius M, Skrifvars MB, Reinikainen M, Bendel S, Raj R, Abu-Habsa M, Hymers C, Borowska A, Sivadhas H, Sahiba S, Perkins S, Rubio J, Rubio JA, Sierra R, English S, Chasse M, Turgeon A, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, Tinmouth A, Van Walraven C, Montroy K, Ziegler J, Dupont Chouinard R, Carignan R, Dhaliwal A, Lum C, Sinclair J, Pagliarello G, McIntyre L, English S, Chasse M, Turgeon A, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, Tinmouth A, Van Walraven C, Montroy K, Ziegler J, Dupont Chouinard R, Carignan R, Dhaliwal A, Lum C, Sinclair J, Pagliarello G, McIntyre L, Groza T, Moreau N, Castanares-Zapatero D, Hantson P, Carbonara M, Ortolano F, Zoerle T, Magnoni S, Pifferi S, Conte V, Stocchetti N, Carteron L, Suys T, Patet C, Quintard H, Oddo M, Rubio JA, Rubio J, Sierra R, Spatenkova V, Pokorna E, Suchomel P, Ebert N, Jancik J, Rhodes H, Bylinski T, Hawthorne C, Shaw M, Piper I, Kinsella J, Kink AK, Rätsep IR, Boutin A, Moore L, Chasse M, Zarychanski R, Lauzier F, English S, McIntyre L, Lacroix J, Griesdale D, Lessard-Bonaventure P, Turgeon AF, Boutin A, Moore L, Green R, Lessard-Bonaventure P, Erdogan M, Butler M, Lauzier F, Chasse M, English S, McIntyre L, Zarychanski R, Lacroix J, Griesdale D, Desjardins P, Fergusson DA, Turgeon AF, Goncalves B, Vidal B, Valdez C, Rodrigues AC, Miguez L, Moralez G, Hong T, Kutz A, Hausfater P, Amin D, Struja T, Haubitz S, Huber A, Mueller B, Schuetz P, Brown T, Collinson J, Pritchett C, Slade T, Le Guen M, Hellings S, Ramsaran R, Alsheikhly A, Abe T, Kanapeckaite L, Abu-Habsa M, Bahl R, Russell MQ, Real KJ, Abu-Habsa M, Lyon RM, Oveland NP, Penketh J, Mcdonald M, Kelly F, Alfafi M, Alsolamy S, Almutairi W, Alotaibi B, Van den Berg AE, Schriel Y, Dawson L, Meynaar IA, Talaie H, Silva D, Fernandes S, Gouveia J, Santos Silva J, Foley J, Kaskovagheorgescu A, Evoy D, Cronin J, Ryan J, Huck M, Hoffmann C, Renner J, Laitselart P, Donat N, Cirodde A, Schaal JV, Masson Y, Nau A, Leclerc T, Howarth O, Davenport K, Jeanrenaud P, Raftery S, MacTavish P, Devine H, McPeake J, Daniel M, Kinsella J, Quasim T, Alrabiee S, Alrashid A, Alsolamy S, Gundogan O, Bor C, Akýn Korhan E, Demirag K, Uyar M, Frame F, Ashton C, Bergstrom Niska L, Dilokpattanamongkol P, Suansanae T, Suthisisang C, Morakul S, Karnjanarachata C, Tangsujaritvijit V, Mahmood S, Al Thani H, Almenyar A, Vakalos A, Avramidis V, Sharvill R, Penketh J, Morton SE, Chiew YS, Pretty C, Chase JG, Shaw GM, Knafelj R, Kordis P, Patel S, Grover V, Kuchyn I, Bielka K, Aidoni Z, Grosomanidis V, Kotzampassi K, Stavrou G, Fyntanidou B, Patsatzakis S, Skourtis C, Lee SD, Williams K, Weltes ID, Berhane S, Arrowsmith C, Peters C, Robert S, Caldas J, Panerai RB, Robinson TG, Camara L, Ferreira G, Borg-Seng-Shu E, De Lima Oliveira M, Mian NC, Santos L, Nogueira R, Zeferino SP, Jacobsen Teixeira M, Galas F, Hajjar LA, Killeen P, McPhail M, Bernal W, Maggs J, Wendon J, Hughes T, Taniguchi LU, Siqueira EM, Vieira Jr JM, Azevedo LC, Ahmad AN, Abu-Habsa M, Bahl R, Helme E, Hadfield S, Loveridge R, Shak J, Senver C, Howard-Griffin R, Wacharasint P, Fuengfoo P, Sukcharoen N, Rangsin R, Sbiti-Rohr D, Schuetz P, Na H, Song S, Lee S, Jeong E, Lee K, Cooper M, Milinis K, Williams G, McCarron E, Simants S, Patanwala I, Welters ID, Zoumpelouli E, Volakli EA, Chrysohoidou V, Georgiou S, Charisopoulou K, Kotzapanagiotou E, Panagiotidou V, Manavidou K, Stathi Z, Sdougka M, Salahuddin N, AlGhamdi B, Marashly Q, Zaza K, Sharshir M, Khurshid M, Ali Z, Malgapo M, Jamil M, Shafquat A, Shoukri M, Hijazi M, Abe T, Uchino S, Takinami M, Rangel Neto NR, Oliveira S, Reis FQ, Rocha FA, Moralez G, Ebecken K, Rabello LS, Lima MF, Hatum R, De Marco FV, Alves A, Pinto JE, Godoy M, Brasil PE, Bozza FA, Salluh JI, Soares M, Krinsley J, Kang G, Perry J, Hines H, Wilkinson KM, Tordoff C, Sloan B, Bellamy MC, Moreira E, Verga F, Barbato M, Burghi G, Soares M, Silva UV, Azevedo LC, Torelly AP, Kahn JM, Angus DC, Knibel MF, Brasil PE, Bozza FA, Salluh JI, Velasco MB, Dalcomune DM, Marshall R, Gilpin T, Tridente A, Raithatha A, Mota D, Loureiro B, Dias J, Afonso O, Coelho F, Martins A, Faria F, Al-Dorzi H, Al Orainni H, AlEid F, Tlaygeh H, Itani A, Hejazi A, Arabi Y, Gaudry S, Messika J, Ricard JD, Guillo S, Pasquet B, Dubief E, Dreyfuss D, Tubach F, Battle C, James K, Temblett P, Davies L, Battle C, Lynch C, Pereira S, Cavaco S, Fernandes J, Moreira I, Almeida E, Seabra Pereira F, Malheiro M, Cardoso F, Aragão I, Cardoso T, Fister M, Knafelj R, Muraray Govind P, Brahmananda Reddy N, Pratheema R, Arul ED, Devachandran J, Velasco MB, Dalcomune DM, Knafelj R, Fister M, Chin-Yee N, D’Egidio G, Thavorn K, Heyland D, Kyeremanteng K, Murchison AG, Swalwell K, Mandeville J, Stott D, Guerreiro I, Devine H, MacTavish P, McPeake J, Quasim T, Kinsella J, Daniel M, Goossens C, Marques MB, Derde S, Vander Perre S, Dufour T, Thiessen SE, Güiza F, Janssens T, Hermans G, Vanhorebeek I, De Bock K, Van den Berghe G, Langouche L, Devine H, MacTavish P, Quasim T, Kinsella J, Daniel M, McPeake J, Miles B, Madden S, Devine H, Weiler M, Marques P, Rodrigues C, Boeira M, Brenner K, Leães C, Machado A, Townsend R, Andrade J, MacTavish P, McPeake J, Devine H, Kinsella J, Daniel M, Kishore R, Fenlon C, Quasim T, Fiks T, Ruijter A, Te Raa M, Spronk P, Chiew YS, Docherty P, Dickson J, Moltchanova E, Scarrot C, Pretty C, Shaw GM, Chase JG, Hall T, Ngu WC, Jack JM, Morgan P, Avard B, Pavli A, Gee X, Bor C, Akin Korhan E, Demirag K, Uyar M, Shirazy M, Fayed A, Gupta S, Kaushal A, Dewan S, Varma A, Ghosh E, Yang L, Eshelman L, Lord B, Carlson E, Helme E, Broderick R, Hadfield S, Loveridge R, Ramos J, Forte D, Yang F, Hou P, Dudziak J, Feeney J, Wilkinson K, Bauchmuller K, Shuker K, Faulds M, Raithatha A, Bryden D, England L, Bolton N, Tridente A, Bauchmuller K, Shuker K, Tridente A, Faulds M, Matheson A, Gaynor J, Bryden D; S South Yorkshire Hospitals Research Collaboration, Ramos J, Peroni B, Daglius-Dias R, Miranda L, Cohen C, Carvalho C, Velasco I, Forte D, Kelly JM, Neill A, Rubenfeld G, Masson N, Min A, Boezeman E, Hofhuis J, Hovingh A, De Vries R, Spronk P, Cabral-Campello G, Aragão I, Cardoso T, Van Mol M, Nijkamp M, Kompanje E, Ostrowski P, Omar A, Kiss K, Köves B, Csernus V, Molnár Z, Hoydonckx Y, Vanwing S, Stessel B, Van Assche A, Jamaer L, Dubois J, Medo V, Galvez R, Miranda JP, Stone C, Wigmore T, Arunan Y, Wheeler A, Bauchmuller K, Bryden D, Wong Y, Poi C, Gu C, Molmy P, Van Grunderbeeck N, Nigeon O, Lemyze M, Thevenin D, Mallat J, Ramos J, Correa M, Carvalho RT, Forte D, Fernandez A, McBride C, Koonthalloor E, Walsh C, Webber A, Ashe M, Smith K, Jeanrenaud P, Marudi A, Baroni S, Ragusa F, Bertellini E, Volakli EA, Chochliourou E, Dimitriadou M, Violaki A, Mantzafleri P, Samkinidou E, Vrani O, Arbouti A, Varsami T, Sdougka M, Bollen JA, Van Smaalen TC, De Jongh WC, Ten Hoopen MM, Ysebaert D, Van Heurn LW, Van Mook WN, Sim K, Fuller A, Roze des Ordons A, Couillard P, Doig C, Van Keer RV, Deschepper RD, Francke AF, Huyghens LH, Bilsen JB, Nyamaizi B, Dalrymple C, Molokhia A, Dobru A, Marrinan E, Ankuli A, Molokhia A, McPeake J, Struthers R, Crawford R, Devine H, Mactavish P, Quasim T, Morelli P, Degiovanangelo M, Lemos F, MArtinez V, Verga F, Cabrera J, Burghi G, Rutten A, Van Ieperen S, De Geer S, Van Vugt M, Der Kinderen E, Giannini A, Miccinesi G, Marchesi T, Prandi E. 36th International Symposium on Intensive Care and Emergency Medicine : Brussels, Belgium. 15-18 March 2016. Crit Care. 2016;20:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 261] [Cited by in RCA: 300] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 30. | Dietrich CF, Mathis G, Blaivas M, Volpicelli G, Seibel A, Wastl D, Atkinson NS, Cui XW, Fan M, Yi D. Lung B-line artefacts and their use. J Thorac Dis. 2016;8:1356-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 31. | Enghard P, Rademacher S, Nee J, Hasper D, Engert U, Jörres A, Kruse JM. Simplified lung ultrasound protocol shows excellent prediction of extravascular lung water in ventilated intensive care patients. Crit Care. 2015;19:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 122] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 32. | Öhman J, Harjola VP, Karjalainen P, Lassus J. Focused echocardiography and lung ultrasound protocol for guiding treatment in acute heart failure. ESC Heart Fail. 2018;5:120-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | van Munster CE, D'Souza M, Steinheimer S, Kamm CP, Burggraaff J, Diederich M, Kravalis K, Dorn J, Walsh L, Dahlke F, Kappos L, Uitdehaag BM. Tasks of activities of daily living (ADL) are more valuable than the classical neurological examination to assess upper extremity function and mobility in multiple sclerosis. Mult Scler. 2019;25:1673-1681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Sasani K, Catanese HN, Ghods A, Rokni SA, Ghasemzadeh H, Downey RJ, Shahrokni A. Gait speed and survival of older surgical patient with cancer: Prediction after machine learning. J Geriatr Oncol. 2019;10:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Chen S, Zheng J, Chen C, Xing Y, Cui Y, Ding Y, Li X. Unmet needs of activities of daily living among a community-based sample of disabled elderly people in Eastern China: a cross-sectional study. BMC Geriatr. 2018;18:160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 36. | Osuka Y, Kojima N, Kim M, Won CW, Suzuki T, Kim H. Exercise type and activities of daily living disability in older women: An 8-year population-based cohort study. Scand J Med Sci Sports. 2019;29:400-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |