Published online Jul 27, 2024. doi: 10.4240/wjgs.v16.i7.2337
Revised: May 28, 2024
Accepted: June 19, 2024
Published online: July 27, 2024
Processing time: 132 Days and 2.2 Hours
Severe bleeding as a result of a major vascular injury is a potentially fatal event commonly observed in the emergency department. Bowel necrosis and gastric ulcers secondary to ischemia are rare due to their rich blood supply. In this case, we present the case of a patient who was treated successfully following rupture of his femoral artery resulting in bowel necrosis and an unusually large gastric ulcer.
A 28-year-old male patient sustained a knife stab wound to the right thigh, causing rupture of his femoral artery and leading to massive bleeding. He underwent cardiopulmonary resuscitation and received a large blood transfusion. Abdominal surgeries confirmed bowel necrosis, and jejunostomy was performed. The necrotic intestine was removed, the remaining intestine was anastomosed, and the right thigh was amputated. After three surgeries, the patient's overall condition gradually improved, and the patient was discharged from the hospital. However, one day after discharge, the patient was admitted again due to dizzi
Trauma department physicians need to be aware of the possible serious complications involving the abdomen of trauma patients with massive bleeding.
Core Tip: This report describes a case of sequential bowel necrosis and an unusually large gastric ulcer in a patient with a ruptured femoral artery. We present this case to emphasize the importance of monitoring the abdomen and staying alert for potential complications in severely ill patients with massive blood loss. Physicians should be aware of the possible serious complications of lesions in the abdomen, even if there are no obvious signs of trauma.
- Citation: Wang P, Wang TG, Yu AY. Sequential bowel necrosis and large gastric ulcer in a patient with a ruptured femoral artery: A case report. World J Gastrointest Surg 2024; 16(7): 2337-2342
- URL: https://www.wjgnet.com/1948-9366/full/v16/i7/2337.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i7.2337
Trauma is complex, serious, intractable, and the main cause of death among adults under the age of 45[1]. Major blood vessel damage can quickly lead to shock, multiple organ dysfunction, and ultimately death. Intestinal ischemia impairs the function of the intestinal mucosal barrier and the translocation of bacteria and toxins in the intestine, leading to systemic inflammatory response syndrome, multiple organ dysfunction syndrome, and even death, and the mortality rate ranges from 62.5% to 85%[2]. We present the case of a patient with femoral artery rupture who developed sequential bowel necrosis and an unusually large gastric ulcer, which was successfully treated after three abdominal operations and prompt treatment of the large gastric ulcer.
A 28-year-old male patient presented to the emergency department due to stab wounds that caused right thigh pain and bleeding for 7 hours.
Seven hours ago, the 28-year-old male patient was stabbed in the right thigh, which caused immediate bleeding resulting in clouding of consciousness. Family members called an ambulance to the local hospital for treatment. At the hospital, he underwent endotracheal intubation, received an emergency blood transfusion, and his wounds were dressed, during which he suffered cardiac arrest. The doctor performed cardiopulmonary resuscitation. The patient regained spontaneous heartbeat after treatment, received transfusions of 12 units of red blood cells and 1600 mL of plasma, and was transferred to our hospital for further treatment. The patient has not been fed since the injury and therefore has had no bowel movements.
The patient denied any past illness history.
The patient denied any family history of the illness.
On physical examination, the vital signs were as follows: Body temperature, 36.7 °C; blood pressure, 81/35 mmHg; heart rate, 109 beats/min; respiratory rate, 25 breaths/min; eyelid conjunctiva, pale; pupil, round and equal in size, approximately 3 mm in diameter; slow reaction to light; lips, pale; tracheal tube, in place; respiratory sounds of both lungs, dry and wet rales, not heard; heart rhythm, unanimous; and no pathologic murmur, heard; the whole abdomen, dilated; intestinal sounds, not heard; a skin fissure of approximately 18 cm was observed on the medial side of the right thigh; and the right dorsalis pedis artery was not detected.
Routine blood tests revealed a white blood cell count of 13.9 × 109/L and a hemoglobin level of 43 g/L.
Because of the patient’s potentially fatal bleeding, there was no chance for him to undergo an imaging examination and be sent to the operating room after several minutes of preparation in the rescue room.
(1) Ruptured femoral artery in the right thigh; (2) Bowel necrosis; (3) Hemorrhagic shock; (4) Secondary gastric ulcer; and (5) Cardiopulmonary resuscitation after cardiac arrest.
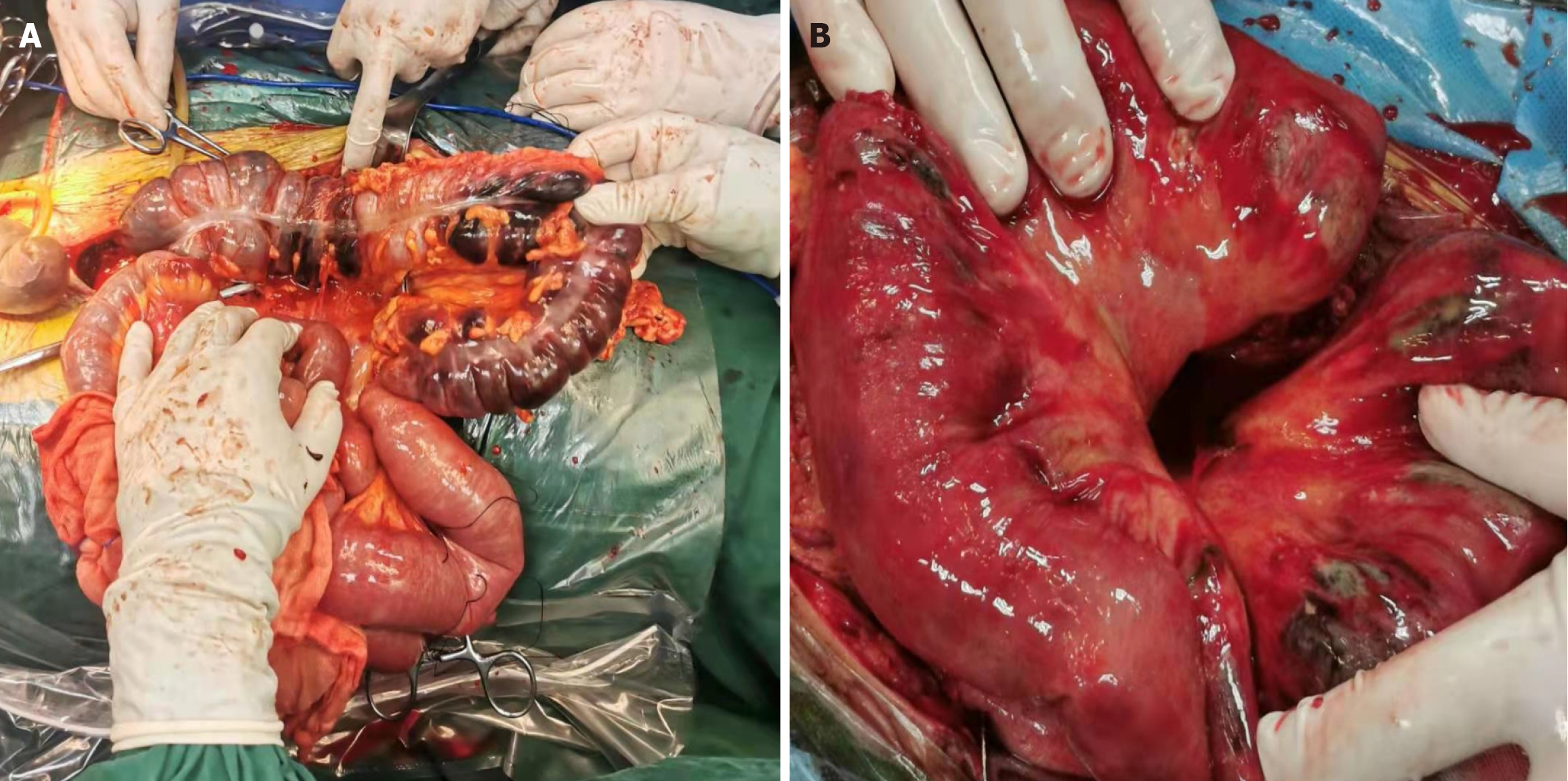
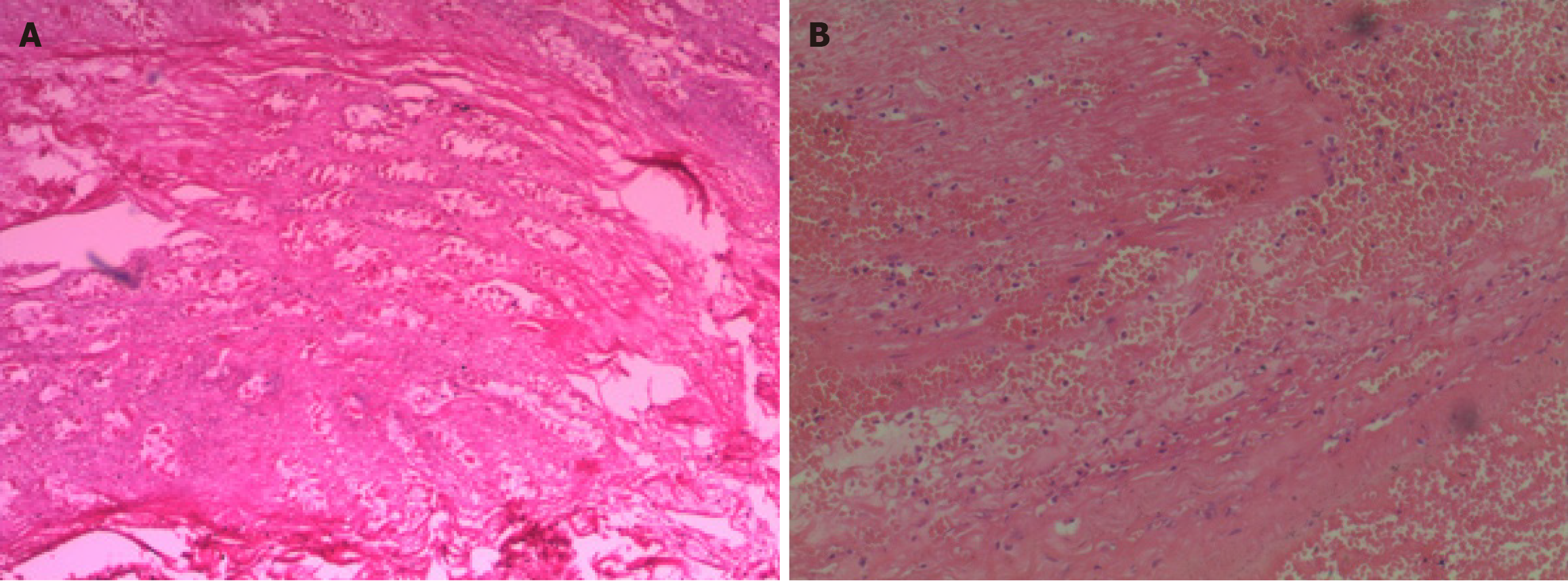
Three abdominal surgeries confirmed sequential bowel necrosis. During the first surgery, extensive necrosis was observed in the right colon and transverse colon; approximately one meter of the necrotic colon was resected, and jejunostomy was performed (Figure 1A). A total of 28 units of red blood cells and 2400 mL of plasma were transfused during this process. Subsequently, he was transferred to the intensive care unit (ICU). While receiving ICU therapy, stoma necrosis was discovered, necessitating a second surgery on his abdomen. During the surgical procedure, extensive necrosis was observed in the patient’s jejunum, which measured approximately 1.6 meters in length (Figure 1B). Therefore, the necrotic intestine was removed, and a pathologic examination was performed (Figure 2). The remaining intestine was anastomosed.
Postoperative follow-up revealed that the gastric pouch was still filled with liquid, and discharge of fecal-like material from the abdominal incision was observed, raising concerns about intestinal perforation due to necrosis. Based on a repeat abdominal computed tomography scan (Figure 3) to evaluate the possibility of intestinal damage or inflammation-induced enteric perforation, exploratory thoracotomy and bowel rupture repair surgery combined with debridement of the abdominal incision were performed. After multiple surgical interventions, the patient's overall condition gradually improved. Following femoral artery rupture and massive hemorrhage, compartment syndrome led to significant muscle necrosis of the right leg. The patient developed fever, tachycardia, and toxin absorption symptoms, resulting in progressive renal dysfunction and uncontrolled sepsis. Ultimately, his right thigh was amputated. After multiple surgeries, the patient gradually recovered his intestinal function without any significant discomfort upon eating, and he was discharged from the hospital.
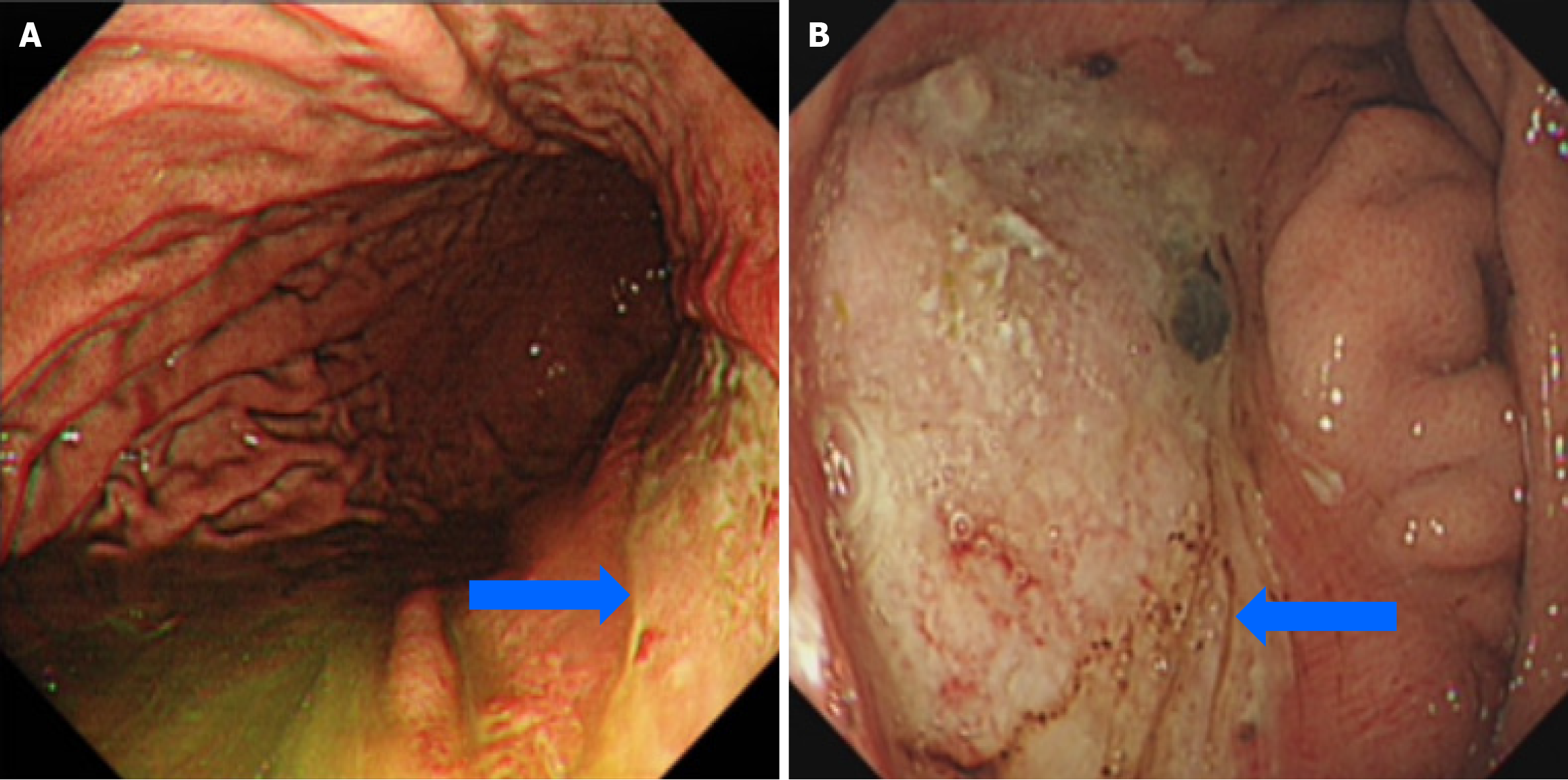
Surprisingly, one day after discharge, the patient was admitted again due to dizziness and melena. Gastroduodenoscopy revealed a giant ulcer in the patient’s stomach (Figure 4A), and the banded ulcer was 20.0 cm × 8.0 cm from the fundus and stretched to the antrum. The patient was advised to fast and received proton pump inhibitors, hemostatic agents, and nutritional support. Moreover, the patient experienced several episodes of hematemesis one week after admission, with a single bleeding volume of approximately 800 mL. Interventional abdominal arteriography was applied to control giant gastric ulcer (GGU) bleeding, but this technique was ineffective. Therefore, the previous treatment regimen was continued in parallel with a jejunal feeding tube indwelling for nutritional supplementation. A repeat gastroduodenoscopy performed 2 weeks later showed that the ulcer had decreased in size to a clean-based 4.5 cm × 2.0 cm ulcer without any deep cratering (Figure 4B). After successful removal of the jejunal nutrition tube, the patient recovered and was ultimately discharged.
Six months after the last surgery, enterostomy and reintroduction surgery were completed. The patient was fitted with a right lower limb prosthesis one year after surgery. After 3 years of follow-up, the patient was still alive and had no complaints of discomfort.
Major blood vessel damage can quickly lead to shock, multiple organ dysfunction, and ultimately death. Shock resulting in a sharp decrease in intestinal blood supply is associated with a high mortality rate. Intestinal ischemia impairs the function of the intestinal mucosal barrier and the translocation of bacteria and toxins in the intestine, leading to systemic inflammatory response syndrome, multiple organ dysfunction syndrome, and even death, and the mortality rate ranges from 62.5% to 85%[2].
A stress ulcer (SU) is acute mucosal erosion of the stomach, duodenum and esophagus and occurs in various emergency situations, especially when the patient is suffering from trauma, burns and severe diseases accompanied by shock, bleeding and infection, or serious damage to the function of important organs[3]. Although the incidence of SU is not high, at approximately 6% in critically ill patients, the mortality rate of bleeding patients is close to 50%[4]. Due to the rupture of the femoral artery with massive blood loss and the long duration of limb ischemia, amputation of his right leg was considered. Because of massive bleeding, the patient’s body was severely ischemic, especially in the gastrointestinal tract. During the ischemic process, the blood supply is interrupted, leading to ischemic damage and rapid damage to metabolically active tissues. Continuous massive blood transfusions after surgery restore the blood flow of the ischemic tissue while also triggering a cascade event called a “reperfusion injury”, which is a secondary injury associated with serious pathological reactions, causing more extensive damage to the body than ischemic injury[5].
The triad of inflammation, increased permeability, and bacterial translocation is the key factor in intestinal ischemia-reperfusion injury (IRI), which often has an insidious initial presentation and a high mortality rate. In this case, after his injury, the patient experienced massive arterial bleeding, leading to sudden cardiac arrest and gastrointestinal ischemia. In addition, prolonged surgical bleeding worsened gastrointestinal ischemia, leading to subsequent necrosis of the colon and jejunum, as well as gastric ulcer bleeding during the later treatment process. The patient’s bowel necrosis was interesting and unexpected, and three intestinal necroses and perforations occurred from the colon to the jejunum. Due to this timely discovery, all intestinal necroses were managed effectively. We believe that the patient’s sequential intestinal necroses were not caused by direct trauma but rather by the rupture of the femoral artery and severe bleeding, which initially caused excessive contraction of the blood vessels supplying the colon. At the same time, due to the presence of a considerable amount of bacteria in the colon, bowel ischemia and bacterial translocation led to early necrosis of the colon, and necrosis of the jejunum may be caused by the excessive use of the vasoconstrictor norepinephrine to reduce blood loss. Clarysse et al[6] showed that polyethylene glycol can reduce reperfusion edema, bacterial translocation, and inflammatory reactions and can be used both for the pretreatment and treatment of IRI.
One of the complications of trauma is SU. The most common symptom of gastric ulcers is pain, and the second most common symptom is internal bleeding[7]. This patient presented with melena followed by profuse hematemesis instead of abdominal pain, which is characteristic of SU. Gastroscopy was performed when the patient presented with melena, and the result was unexpected-a GGU, which is defined as an ulcer more than 3 cm in diameter, was observed. In this case, the gastric ulcer was 20.0 cm × 8.0 cm in diameter, which surprised us because there are no previous reports of such a large ulcer[8,9]. Under normal circumstances, surgical intervention is required when medical treatment is ineffective. Considering the special injury mechanism and the patient’s clinical presentation, a multidisciplinary discussion was organized and suggested that the patient’s giant ulcer was not a simple SU but was instead a manifestation of gastric ischemia caused by massive blood loss after femoral artery injury. In addition, considering that the patient had previously undergone multiple operations, gastric surgery may have induced intestinal ischemia and necrosis again. Therefore, we decided to treat the ulcer medically and to provide nutritional support via a jejunal enteral feeding tube. Fortunately, after 2 weeks of medical treatment, the patient’s gastric ulcer was significantly smaller than before, and the patient reported no abdominal pain after eating.
This report describes a case of sequential bowel necrosis and an unusually large gastric ulcer in a patient with a ruptured femoral artery. Trauma department physicians need to be aware of possible serious complications involving the abdomen of trauma patients with massive bleeding. A review of the literature as well as the results of the present case support the need for additional studies to elucidate the pathogenesis of bowel necrosis caused by ischemic-reperfusion injury and to identify effective therapies for patients with massive bleeding.
| 1. | Wang SY, Li YH, Chi GB, Xiao SY, Ozanne-Smith J, Stevenson M, Phillips MR. Injury-related fatalities in China: an under-recognised public-health problem. Lancet. 2008;372:1765-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 192] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 2. | Hou J, Strand-Amundsen R, Tronstad C, Høgetveit JO, Martinsen ØG, Tønnessen TI. Automatic Prediction of Ischemia-Reperfusion Injury of Small Intestine Using Convolutional Neural Networks: A Pilot Study. Sensors (Basel). 2021;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Ray A, Gulati K, Henke P. Stress Gastric Ulcers and Cytoprotective Strategies: Perspectives and Trends. Curr Pharm Des. 2020;26:2982-2990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Chen W, Li X, Wang A, Hao Y, Zhang J, Liang J, Yang Y, Zhao H, Gao J. Serum Hs-CRP level and clinical significance of patients with stress ulcer caused by massive blood loss after trauma. Cell Mol Biol (Noisy-le-grand). 2022;67:189-194. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Deng F, Lin ZB, Sun QS, Min Y, Zhang Y, Chen Y, Chen WT, Hu JJ, Liu KX. The role of intestinal microbiota and its metabolites in intestinal and extraintestinal organ injury induced by intestinal ischemia reperfusion injury. Int J Biol Sci. 2022;18:3981-3992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | Clarysse M, Accarie A, Panisello-Roselló A, Farré R, Canovai E, Monbaliu D, De Hertogh G, Vanuytsel T, Pirenne J, Ceulemans LJ. Intravenous Polyethylene Glycol Alleviates Intestinal Ischemia-Reperfusion Injury in a Rodent Model. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Clarke K, Adler N, Agrawal D, Bhakta D, Sata SS, Singh S, Gupta A, Pahwa A, Pherson E, Sun A, Volpicelli F, Cho HJ. Indications for the Use of Proton Pump Inhibitors for Stress Ulcer Prophylaxis and Peptic Ulcer Bleeding in Hospitalized Patients. Am J Med. 2022;135:313-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 8. | Tang C, Pan Q, Xu Z, Zhou X, Wang Y. Gastric schwannoma with giant ulcer and lymphadenopathy mimicking gastric cancer: a case report. BMC Gastroenterol. 2020;20:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Verma R, Al Elshafey M, Oza T, Azouz A, White C. A Giant Syphilitic Gastric Ulcer. ACG Case Rep J. 2022;9:e00819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |