Published online Jul 27, 2024. doi: 10.4240/wjgs.v16.i7.2232
Revised: May 7, 2024
Accepted: May 31, 2024
Published online: July 27, 2024
Processing time: 154 Days and 4.2 Hours
The incidence of cholecystolithiasis is on the rise. Use of information, motivation, and behavioral skills can play a positive role in promoting changes in individual health behaviors. However, reports on the effects of information-motivation-behavioral (IMB) skills model based high-quality nursing as a perioperative nur
To explore the application of IMB skills model based high-quality nursing in patients with gallstones.
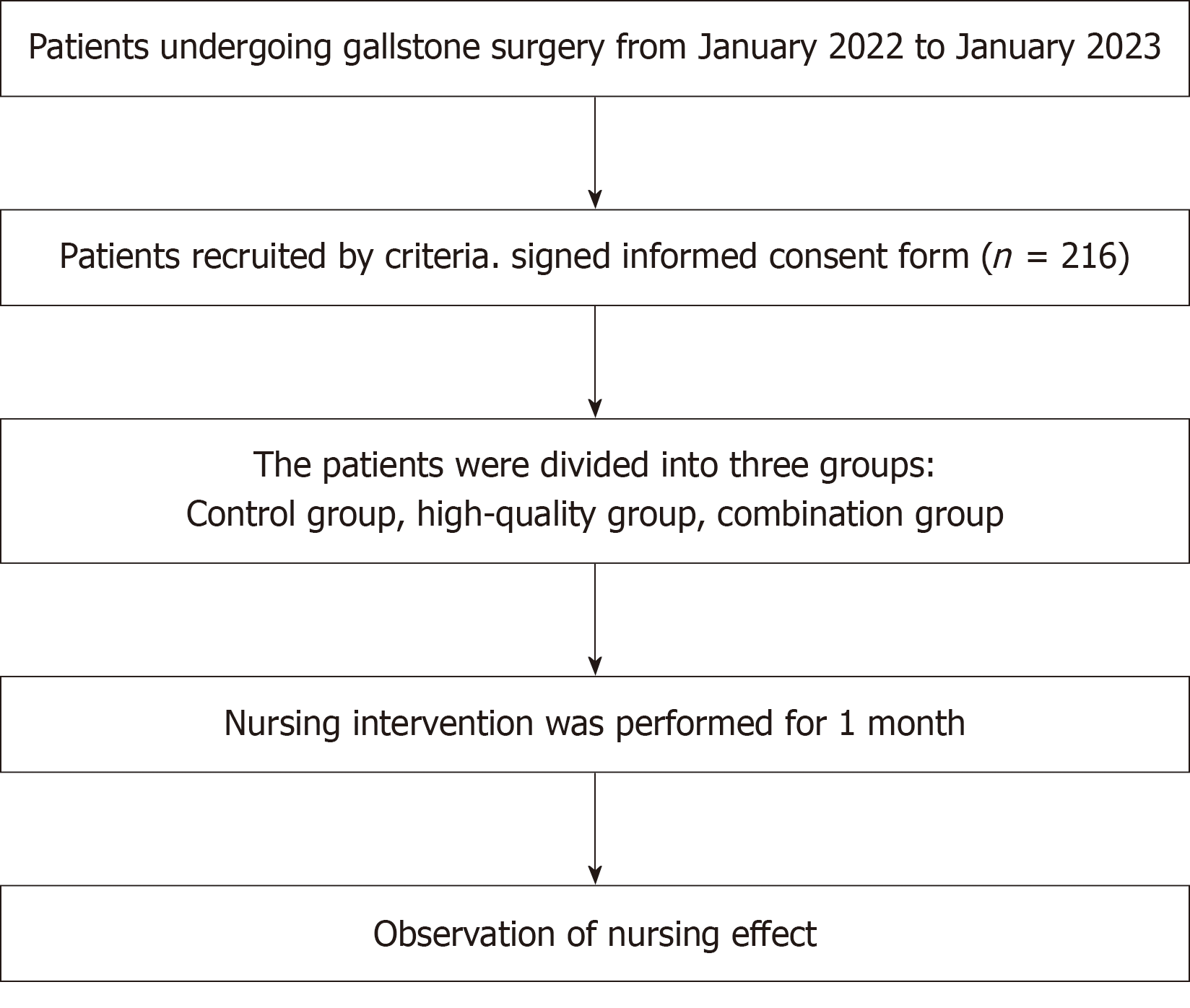
Two hundred and sixteen patients with cholecystolithiasis treated at our hospital from January 2022 to January 2023 were enrolled and divided into a control, high-quality, and combined nursing groups, with 72 patients in each group. The con
After nursing, the time to recovery of gastrointestinal function in the high-quality and combined nursing groups was significantly shorter than that of the control group, with the recovery of gastrointestinal function being the fastest in the combined nursing group (P < 0.05). After nursing intervention, cortisol and norepinephrine levels in the high-quality and combined nursing groups were closer to normal than those of the control group 24 h after surgery, with the combined nursing group having the closest to normal levels (P < 0.05). After 3 and 7 d of intervention, the patients’ pain significantly improved, which was more prominent in the high-quality and combination groups. Meanwhile, the pain score in the combination group was significantly lower than those of the control and high-quality nursing groups (P < 0.05). After nursing intervention, the emotional states of all patients improved, and the scores of patients in the combination group were significantly lower than those of the control and high-quality nursing groups. The quality of life of patients in the high-quality and combined nursing groups significantly improved after nursing intervention compared to that of the control group, with the combined nursing group having the highest quality of life score. After intervention, the incidence of complications in the high-quality and combination groups was significantly lower than that of the control group (P < 0.05), but the difference between the combination and high-quality nursing groups was not significant. Nursing satisfaction of patients in the high-quality and combination groups was significantly higher than that of the control group, with the nursing satisfaction being the highest in the combination group (P < 0.05).
IMB skills model based nursing can improve surgical stress levels, degrees of pain, emotional state, quality of life, and nursing satisfaction of patients with gallstones and reduce the incidence of complications.
Core Tip: This observational study investigates the impact of information-motivation-behavioral (IMB) skills model based high-quality nursing care during the perioperative period on pain management in gallstone patients. The findings reveal that the IMB approach significantly improves patients’ recovery times, reduces pain, alleviates stress, enhances emotional well-being, and increases quality of life compared to conventional care. The IMB skills model based nursing also leads to higher nursing satisfaction rates and lowers complication incidences, suggesting its potential as an effective strategy in enhancing perioperative care for gallstone patients.
- Citation: Ma L, Yu Y, Zhao BJ, Yu YN, Li Y. Effect of information-motivation-behavioral skills model based perioperative nursing on pain in patients with gallstones. World J Gastrointest Surg 2024; 16(7): 2232-2241
- URL: https://www.wjgnet.com/1948-9366/full/v16/i7/2232.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i7.2232
As an emergent surgical disease, gallstones are prominent in adult women, and the number of females afflicted with the disease is significantly higher than that of males[1]. Studies have shown that the main etiological factors of this disease are not only dietary habits but also obesity, diabetes, dyslipidemia, and other factors[2]. Many patients suffer from biliary colic and dull pain in the right upper abdomen and gallbladder effusion, and some also suffer from Mirizzi syndrome, which decreases the patient’s living standards[3]. Clinically, gallstones can be treated by surgery or conservatively with drugs. Conservative drug treatment renders it difficult to remove the root cause, and recurrent gallstones have an impact on the gallbladder, making it difficult to achieve a satisfactory therapeutic effect; therefore, most patients prefer surgical treatment. When patients opt for surgical treatment, they fear the surgical process and various postoperative recovery conditions; moreover, they are worried of the pain during surgery, which causes anxiety prior to the operation, further affecting diagnosis and treatment. Routine nursing, a commonly used clinical nursing measure, has certain effects on patients; however, targeted nursing is not employed according to the actual situation of patients, and psychological nursing for patients is not perfect, which impacts postoperative rehabilitation. The combination of high-quality nursing and whole-course nursing for patients with cholecystolithiasis before and after surgery can improve the quality of patient care and the nursing indicators of patients to a certain extent; therefore, it is highly accepted by patients[4]. The information-motivation-behavioral (IMB) skills model is based on the theory of behavioral changes. The logical relationship between information, motivation, and behavioral skills is analyzed, and diversified methods are added, which can play a positive role in promoting changes in individual health behaviors[5]. However, reports on the effects of IMB skills model based high-quality nursing as a perioperative nursing intervention for patients with gallstones are nonexistent. Based on this, we conducted nursing interventions for 216 patients with gallstones and observed impro
A total of 216 patients with cholecystolithiasis who received treatment at our hospital between January 2022 and January 2023 were selected as study participants. All patients were blindly selected and divided into control, high-quality nursing, and combined nursing groups, with 72 patients in each group. In the control group, the male-to-female ratio was 29:43, and the age ranged from 27 to 53 years, with an average age of (37.98 ± 6.21) years. The disease course was not < 6 mo, with an average of (1.22 ± 0.19) years. In the high-quality nursing group, the male-to-female ratio was 27:45, the age ranged from 27 to 55 years with a mean age of (38.02 ± 6.03) years, and the disease course was not < 5 mo with a mean of (1.18 ± 0.22) years. In the combination nursing group, the ratio of males to females was 30:42, the age ranged from 26 to 54 years with a mean age of (38.06 ± 6.11) years, and the disease duration was not < 5 mo with a mean of (1.21 ± 0.20) years.
The inclusion criteria were as follows: (1) Patients who satisfied the diagnostic criteria for gallstones[6] and required laparoscopic cholecystectomy; (2) No other organ lesions; (3) No language communication barriers or cognitive function effects; and (4) Patients who would like to provide informed consent.
The exclusion criteria were as follows: (1) Presence of bronchial asthma, contact dermatitis, and other immune system diseases; (2) History of abdominal surgery; (3) Presence of obvious contraindications for laparoscopy; (4) Altered consciousness and prolonged coma after surgery; (5) Mental problems; and (6) A short-term history of excessive analgesic drug use.
All patients underwent laparoscopic cholecystectomy and endotracheal intubation. Under general anesthesia, the doctors performed umbilical puncture and trocar insertion to establish a CO2 pneumoperitoneum. Fluid that accumulated in the abdominal cavity of each patient was effectively removed. During the process of locating the gallbladder duct, liver, and hepatic duct, the gallbladder was fixed with a fixation clamp, bluntly separated, and removed. Simultaneously, a silicone tube was placed under the patient’s right liver and connected to a negative-pressure drainage ball.
Basic care was provided to patients, all basic examinations were completed before surgery, and patients were advised to eat more nutritious and easily absorbed food and avoid food that easily produce gas to reduce intestinal flatulence. Nurses worked with the anesthesiologist and surgeon to complete various operations. After the patient returned to the ward, the patient and his family members were provided with postoperative education and instructed to have the patient lie flat for 6 h after the operation before returning to a comfortable position.
All patients received high-quality care based on quality care provided in the control group: (1) When the patient was admitted to the ward, an admission education was provided. If the patient felt unwell, together with his/her family members, he/she would be taken to the ward and be educated regarding the disease and living environment to allow familiarization of the sewage room, living area, catering room, and other places of the department. Moreover, the patient was introduced to the tube bed doctor and tube bed nurse. To a certain extent, the anxiety experienced by the patients and their families secondary to pain and environmental factors caused by the disease can be relieved; (2) For preoperative nursing, the nursing staff and patients communicated to allow a full understanding of the patient’s physical and mental status and treatment measures, while employing the appropriate dialects and adequate nursing knowledge to develop nursing measures for patients and to ensure that patients receive humanistic care from the nursing staff. Concurrently, after communication, the psychological condition of the patient was cared for in a targeted manner, and a detailed explanation was provided to ensure that the patient understood the basic surgical process of gallbladder surgery and possible postoperative complications. Through communication and with the aid of the patient’s family members, the patients’ psychological symptoms, such as anxiety before and during the operation, and prognosis were assessed; and (3) During the operation, the nursing staff communicated effectively with the patient many times to understand his/her needs, reduce the tension and anxiety caused by the surgery, encourage the patient to boost their confidence, and let the patient realize the humanistic care by the nursing staff. After surgery, the nursing staff should fully understand the physical condition and diet of the patient to develop appropriate dietary care, understand the treatment requirements of the doctor, and formulate personalized dietary care measures for patients with different eating habits. A diet suitable to the patient’s taste was provided so that he/she can consume enough protein to enhance their resistance to disease. Nursing staff should reassure patients who are not yet able to eat and instruct them to eat after 2 d, while providing oral care to patients to keep their lips and mouth moist and reduce bacterial growth. Nursing staff should also conduct a detailed pain assessment of the patient, understand the type and degree of pain of the patient, and perform corresponding interventions and care, such as the use of pain-relieving drugs before the occurrence of pain in the patient, and reduce the pain of the patient so that the patient can be satisfied with the care by the nursing staff, achieve emotional stability, and actively cooperate with the treatment by the medical staff.
Upon admission, a health education team was set up comprising of a head nurse, a surgeon, and no less than six specialist nurses. Education and learning were conducted using a health education manual for patients after upper urinary calculus surgery, IMB skills model education, the design of upper urinary calculus surgery, and prevention of recurrence. Simultaneously, each patient was recorded through video recording for no less than 15 min. Health education for patients consisted of the following: (1) Information intervention: During the hospitalization period, a 20-min session of face-to-face health education was conducted at least five times, and a 20-min session of concentrated education was organized twice a week. Additionally, a WeChat group was formed, and education was conducted by posting health education topics in the group; (2) Motivational intervention: Communication with patients was strengthened to allow them to understand that healthy behaviors are beneficial for their prognosis. Use of WeChat communication was necessary to achieve educational effects and allow peers to share their feelings regarding cultivating healthy behaviors with patients. Additionally, their families could strengthen the supervision of patients to ensure that they comply with nursing treatment; and (3) Behavioral skills intervention: This was conducted through WeChat education, on one hand, and through peer guidance in a variety of behavioral interventions, on the other hand, to guide and supervise the health behavior of patients. The patient was informed about the drug treatment, including the name, dosage, frequency, and use of the drug, reminded to follow the doctor’s advice and take the drug on time, and informed of the possible side effects and precautions. The patient was taught about non-pharmacological pain relief methods, such as relaxation training, hot compresses, cold compresses, and massage, with demonstrations and instructions provided when needed. The patient was assisted to develop a reasonable activity and rest plan to avoid excessive activity or prolonged sitting. After the patient recovered and was discharged from the hospital, the patient’s prognosis was evaluated through an outpatient review; moreover, phone and WeChat follow-up at least once every 2 wk and follow-up in the form of family visits were conducted. All patients were treated for 1 mo.
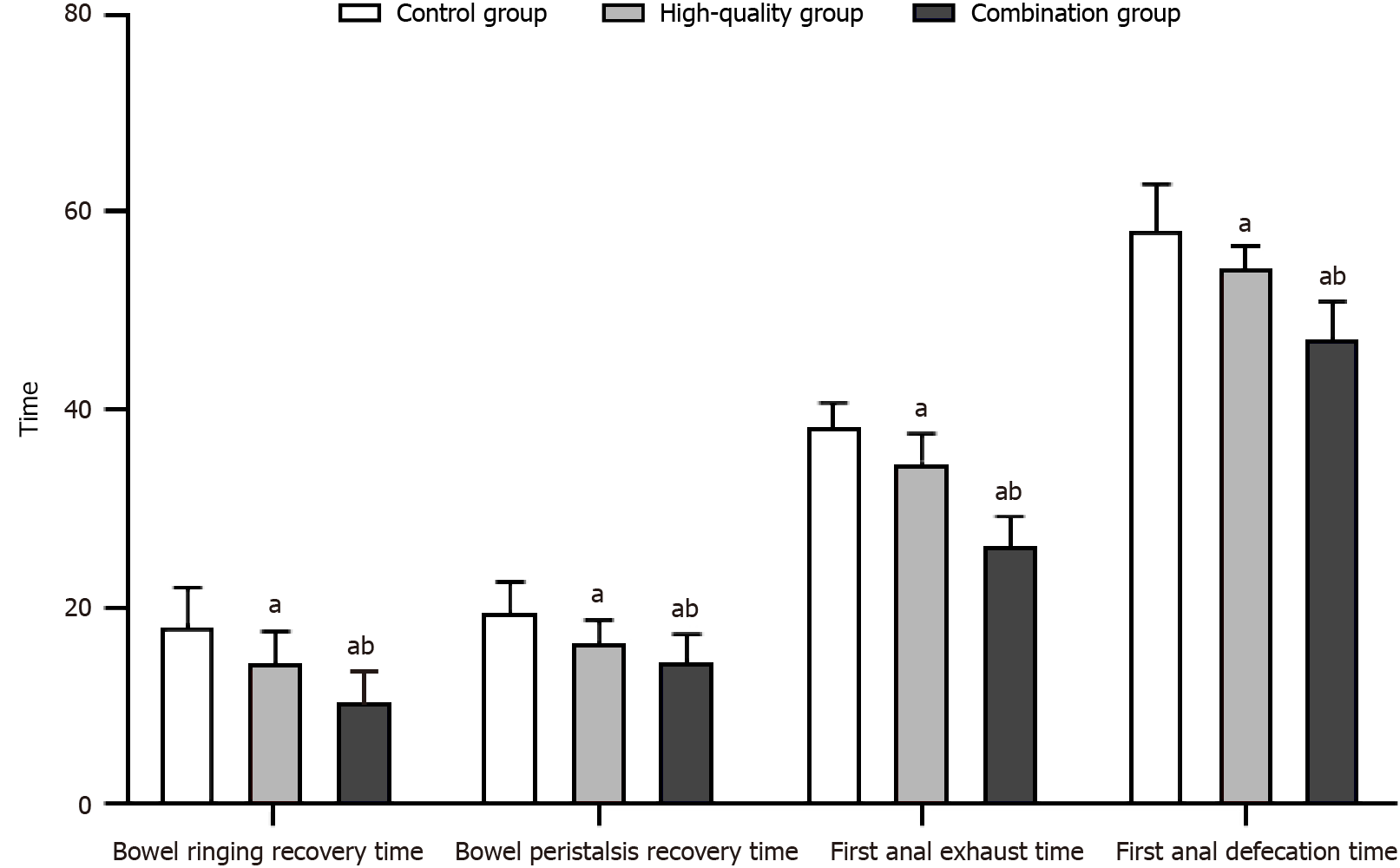
Gastrointestinal function: Time to recovery of gastrointestinal function was compared between the two groups in terms of bowel ringing, bowel peristalsis, first anal exhaust, and first anal defecation.
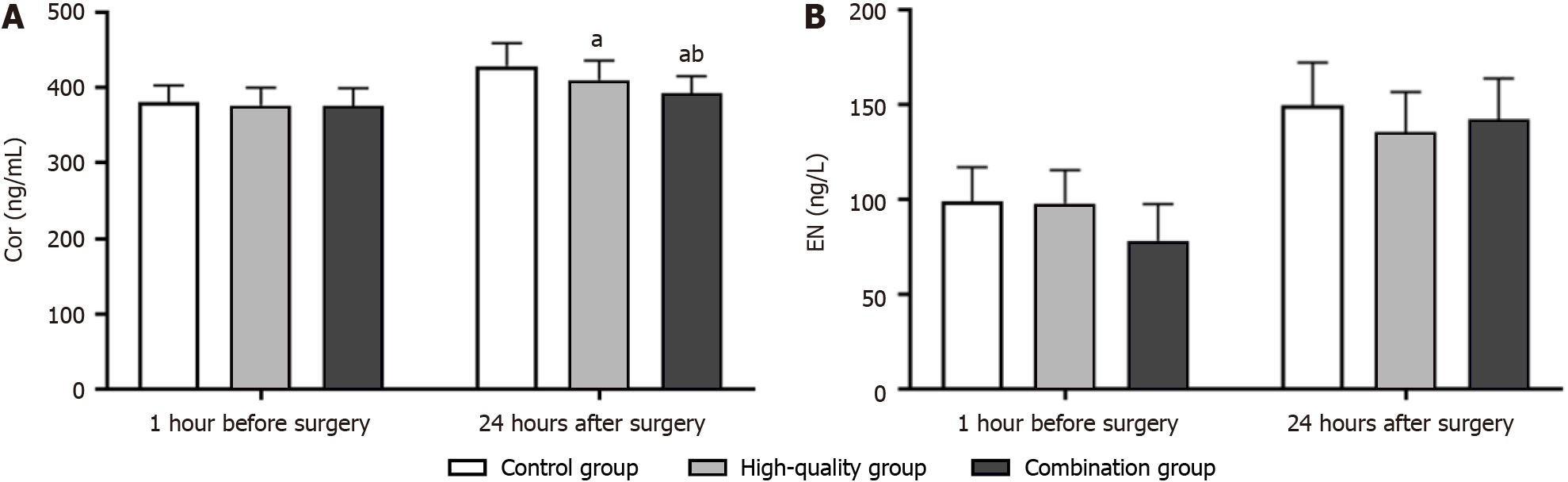
Stress levels: The levels of cortisol (Cor) and norepinephrine (NE) in the fasting venous blood of patients 1 h before surgery and 24 h after surgery were detected using commercial enzyme-linked immunosorbent assay kits purchased from Shanghai Kehansheng Biotechnology Co. Ltd.
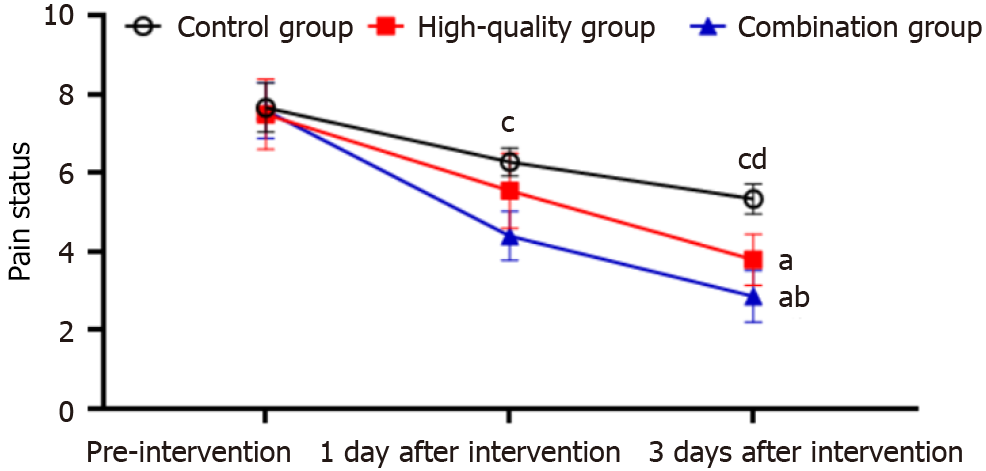
Pain situation: In terms of the degree of pain, patients were divided into three pain levels: Mild, moderate, and severe pain based on the visual analogue score[7]. The full score was 10; less than 3 indicated mild pain, 4 to 6 indicated moderate pain, and more than 7 indicated severe pain.
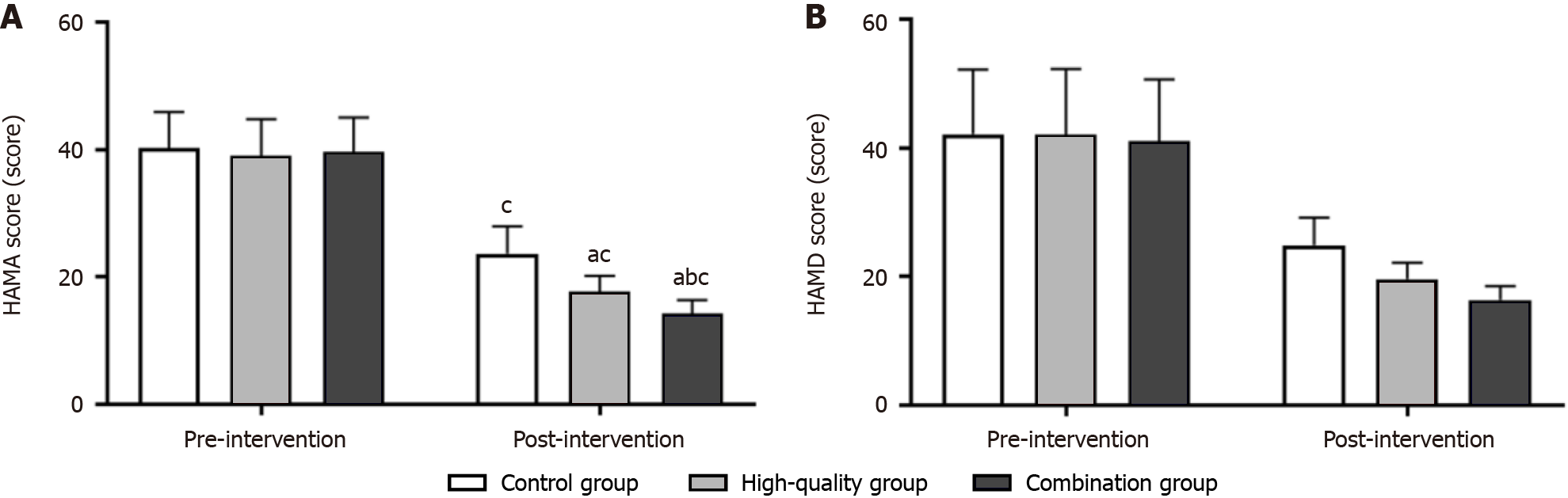
Emotional state: The degree of anxiety and depression in patients before and after the intervention was assessed using the Hamilton Anxiety Scale (HAMA)[8] and the Hamilton Depression Scale (HAMD)[9], respectively. There were 31 items in total, and patients were evaluated using a scoring system. A higher score indicated a more severe degree of anxiety and depression.
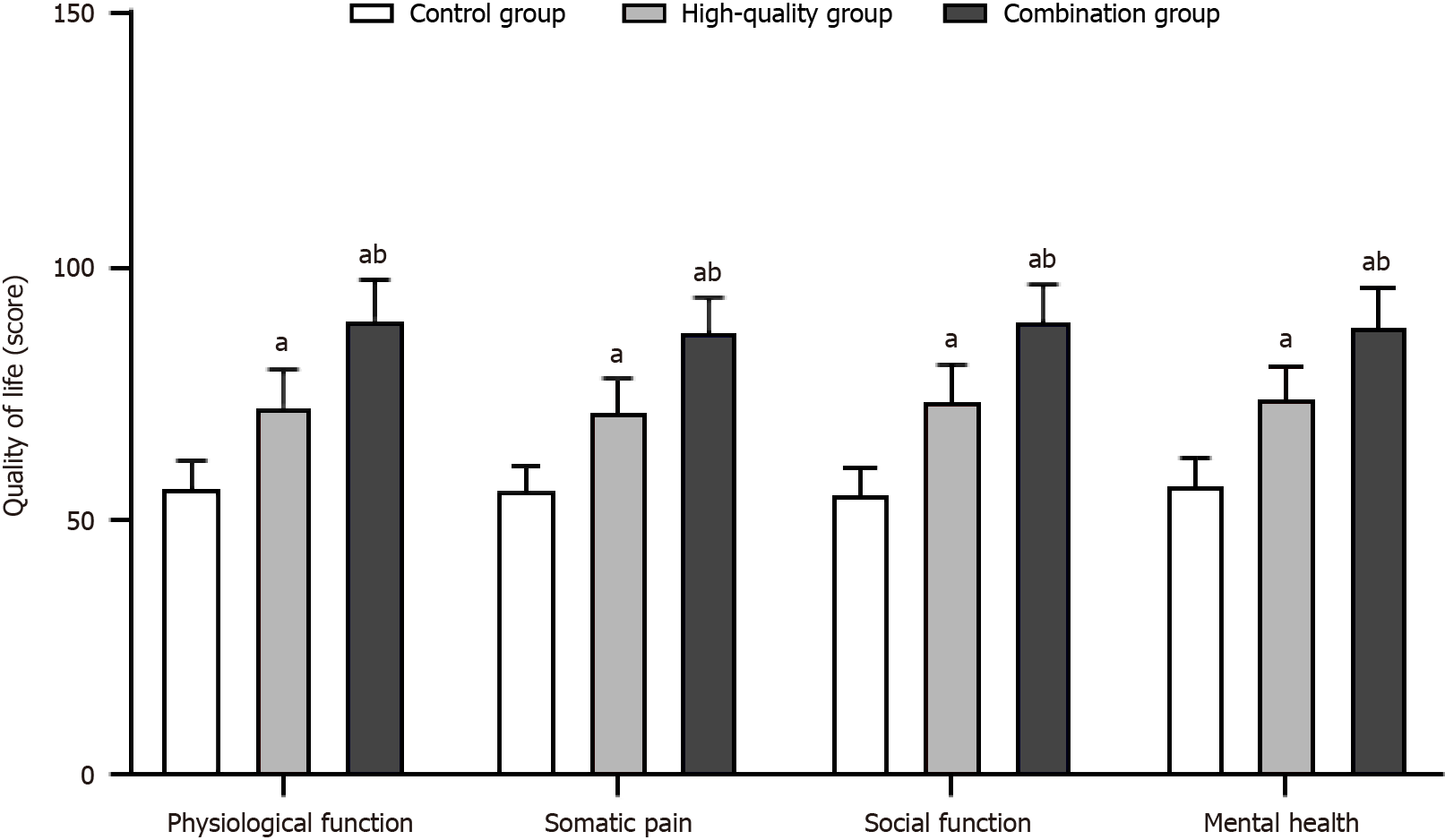
Quality of life: One month after the intervention, the SF-36[10] was used to evaluate the patients’ quality of life from four aspects: Physiological function, physical pain, social function, and mental health. The higher the score, the better the prognosis.
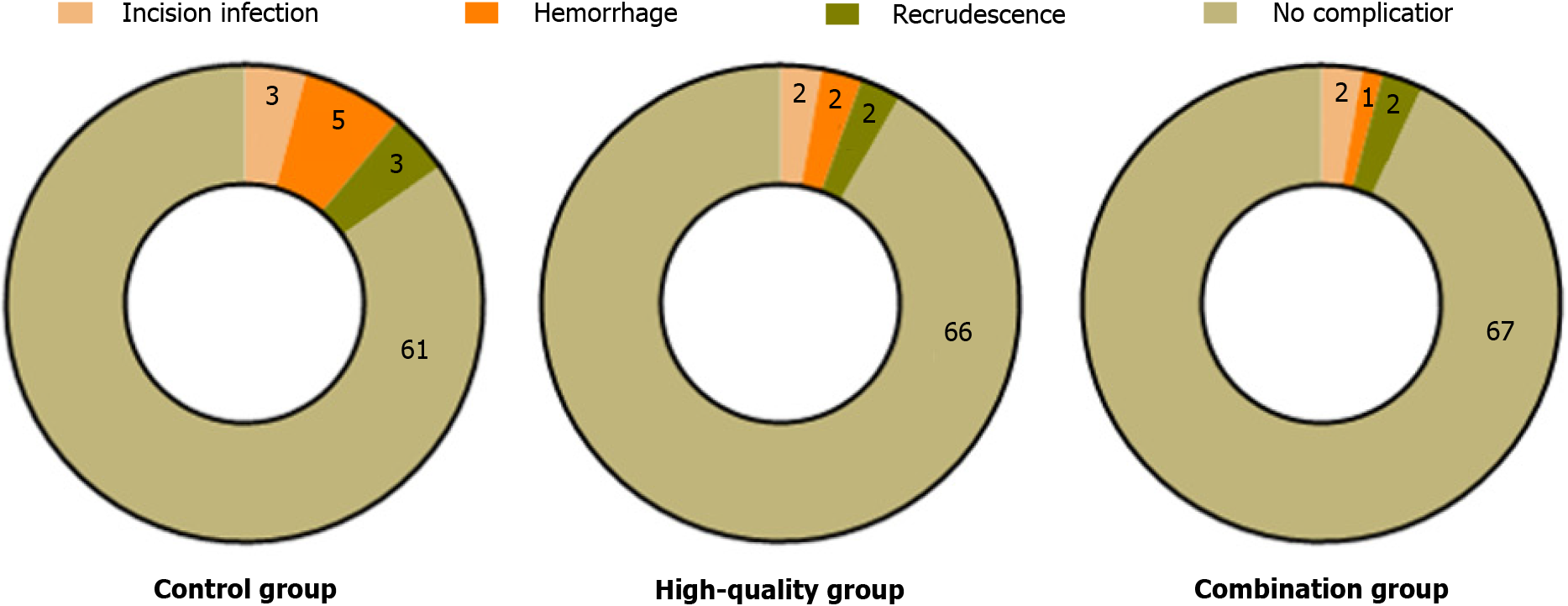
Complications: Complications were recorded during hospitalization.
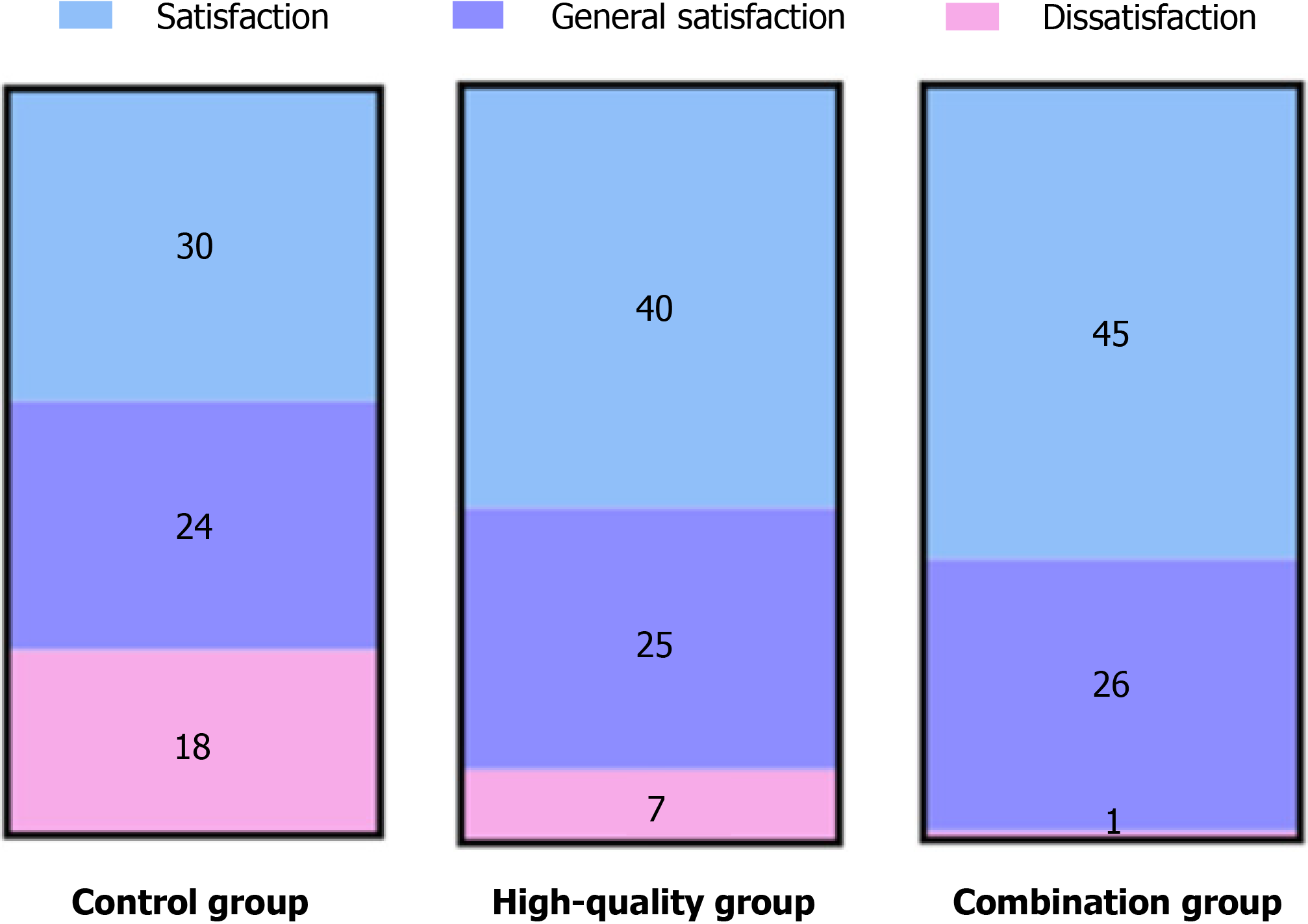
Satisfaction: The satisfaction scale developed by our hospital was used for evaluation of nursing satisfaction, and the Krumbach coefficient was 0.831, suggesting high reliability. The total score of the score was 100, and 85 points or above were considered as very satisfied, more than 60 points as satisfied, and a score of 60 or below as unsatisfied. Total satisfaction was calculated as [(number of patients who were very satisfied + number of patients who were satisfied)/total number of cases] × 100%.
All data were analyzed using SPSS21.0 and Prism, and measurement data are presented as the mean ± SD. The F-test was used to compare the differences among multiple groups. Count data are expressed as [n (%)] and were compared between groups using the χ2 test. Statistical significance was set at P < 0.05.
After nursing intervention, the time to recovery of gastrointestinal function in the high-quality and combined nursing groups was significantly shorter than that of the control group (P < 0.05), with the combined nursing group having the fastest recovery. Detailed results are shown in Figure 2.
No significant difference was found in the stress levels between the two groups before surgery (P > 0.05). At 24 h after surgery, Cor and NE levels in the high-quality and combined nursing groups were closer to normal values than those of the control group, with the combined nursing group having the closest to normal values. Detailed results are shown in Figure 3.
Prior to nursing intervention, no significant difference was found in the patients’ pain status (P > 0.05). After 3 and 7 d of intervention, the pain of patients significantly improved, and the performance was more obvious in the high-quality and combined nursing groups. Meanwhile, the pain score in the combined nursing group was significantly reduced compared with the control group and high-quality nursing group (P < 0.05). Detailed results are shown in Figure 4.
Before nursing intervention, no significant difference was found in the HAMA and HAMD scores between the two groups (P > 0.05). After nursing intervention, the emotional state of all patients improved; the HAMA and HAMD scores of patients in the combination nursing group were significantly lower than those of the control group and high-quality nursing group (P < 0.05). Detailed results are shown in Figure 5.
After nursing intervention, the quality of life of patients in the high-quality and combined nursing groups significantly improved compared to that of the control group, with the combined nursing group having the highest quality of life score (P < 0.05). Detailed results are shown in Figure 6.
After nursing intervention, the incidence of complications in the combined nursing group was significantly lower than that of both the high-quality nursing and control groups (P < 0.05), as illustrated in Figure 7. Furthermore, patient satisfaction with nursing care in the combined nursing group was significantly higher compared to that of the control group (P < 0.05), as shown in Figure 8.
Gallstones are a common disease entity of the biliary system and one of its main symptoms is severe abdominal pain. Perioperative nursing refers to the comprehensive nursing process after a patient receives surgical treatment, which is important for improving the quality of postoperative rehabilitation. With the progress in medical technology and the continuous advancements of nursing concepts, an increasing number of studies have shown that perioperative nursing services based on the IMB skills model and high-quality nursing have important application value in improving the patients’ degree of pain[11,12]. The IMB skills model is a theoretical model in behavioral science that contains three core elements: Information, motivation, and behavior. In perioperative nursing, by providing accurate and comprehensive information to help patients understand the surgical process and precautions, their cognition and understanding of surgery can be effectively enhanced, thus improving their enthusiasm and initiative to participate in rehabilitation behavior[13]. Additionally, fully understanding the individual differences between patients and conducting targeted interventions based on their motivation are important applications of the IMB skills model in perioperative nursing. In this study, we found that after nursing intervention, the time to recovery of gastrointestinal function was significantly shortened in the high-quality and combined nursing groups, with the fastest recovery observed in the combined nursing group (P < 0.05). This further indicates that high-quality perioperative nursing services based on the IMB skills model have high application value in improving the clinical symptoms and gastrointestinal function of patients with gallstones.
During surgery, owing to greater trauma, the body releases a variety of inflammatory mediators, which leads to a certain stress response in the body. Cor and NE are the two most common hormones involved in the stress response[14]. In further outcome observations, we found that patients in the high-quality and combination nursing groups had more significantly improved surgical stress levels those of the control group, and the levels of Cor and NE in the combination nursing group were closer to normal. This result suggests that high-quality perioperative nursing services based on the IMB skills model could effectively improve operative stress in patients. The IMB skills model provides patients with accurate and clear disease-related information; helps them understand the surgical process, possible risks, and complications; and provides them with the necessary education[15], thereby reducing patients’ uncertainty and fear of the disease to a certain extent, increasing their confidence, and thus reducing their surgical stress response.
In this study, we also focused on the changes in patients’ pain, and the results showed that the changes in the high-quality and combination nursing groups were more obvious, and the pain score in the combination nursing group was significantly lower than those of the control and high-quality nursing groups. This suggests that the IMB skills model based high-quality nursing care can effectively improve clinical pain in patients. This may be because the IMB skills model emphasizes the cultivation of behavioral skills to achieve goals[16]. In perioperative nursing, nurses teach patients effective pain management skills and strategies, such as drug use, non-drug pain relief methods (e.g., relaxation training and hot compress), reasonable activities, and rest, and provide specific guidance and training.
Furthermore, we observed that after nursing intervention, the emotional state of patients in the high-quality and combined nursing groups was significantly improved, while the quality of life was also effectively enhanced, and these changes were more significant in the combined nursing group. These results suggest that after the IMB skills model based high-quality perioperative nursing, the patients’ mental state and quality of life improved. In the nursing process, the IMB skills model pays more attention to the intrinsic motivation of patients; nurses will strengthen their communication with patients[17], listen to their needs and desires, and then formulate personalized nursing plans according to the values and expectations of patients, thus stimulating the motivation of patients to actively participate in rehabilitation. The emotional support and comfort provided by the nursing staff can also help alleviate patients’ fear and anxiety to some extent. Additionally, in the process of nursing intervention, nurses teach patients some effective self-management skills and strategies[18], such as pain management, reasonable activities, and rest, to improve patients’ self-management ability to a certain extent, and thus effectively improve the patients’ quality of life. This is consistent with the results of Lu[19].
In addition, we observed the occurrence of complications after nursing, and the results showed that all patients in the three groups had complications to a certain extent; however, compared with the control group, the incidence of complications in the high-quality and combined nursing groups was significantly lower, while the difference between the high-quality and combined nursing groups was not significant. This indicates that the IMB skills model based high-quality perioperative nursing has a high safety profile. The IMB skills model emphasizes the characteristics of providing accurate and clear information, improving patients’ intrinsic motivation, cultivating behavioral skills, helping patients master the correct operation methods, and helping them to improve immune function and overall resistance, thereby reducing the risk of complications. In addition, the nursing staff can help reduce the incidence of complications through timely monitoring and evaluation, early intervention, and resolution of potential problems.
Finally, we conducted a nursing satisfaction survey on all patients after the end of nursing and found that the nursing satisfaction of the combined nursing group was the highest, indicating that high-quality perioperative nursing based on the IMB skills model could improve the quality of clinical nursing to a certain extent. In the study of Fang et al[20], it was also indicated that the IMB skills model can improve patients’ nursing satisfaction. High-quality perioperative nursing services based on the IMB skills model can improve patients’ nursing satisfaction by providing personalized services, information dissemination and education, motivation promotion, emotional support, and care. This personalized, comprehensive nursing service helps meet the special needs of patients and improves their engagement and self-efficacy, thus improving their satisfaction with nursing services.
In summary, high-quality perioperative nursing based on the IMB skills model has high application value in patients with gallstones. It can improve the surgical stress level, degree of pain, emotional state, and quality of life of patients to a certain extent, reduce the incidence of complications in patients, and further improve nursing satisfaction of patients, which has high clinical application value.
However, this study also has some shortcomings: (1) There are limitations in sample selection, and the type and degree of gallstones in this study remained unclear, which may limit the generalization of the results; (2) During the im
| 1. | Gutt C, Schläfer S, Lammert F. The Treatment of Gallstone Disease. Dtsch Arztebl Int. 2020;117:148-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 2. | Di Ciaula A, Garruti G, Frühbeck G, De Angelis M, de Bari O, Wang DQ, Lammert F, Portincasa P. The Role of Diet in the Pathogenesis of Cholesterol Gallstones. Curr Med Chem. 2019;26:3620-3638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 3. | Portincasa P, Di Ciaula A, Bonfrate L, Stella A, Garruti G, Lamont JT. Metabolic dysfunction-associated gallstone disease: expecting more from critical care manifestations. Intern Emerg Med. 2023;18:1897-1918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 4. | Zhang LW, Zhang BY, Lu BX. [To analyze the effect and complication of high-quality nursing intervention in patients with cholecystolithiasis after laparoscopic surgery]. Zhongguo Baojian Yingyang. 2021;31. |
| 5. | Lin M, Chen T, Fan G. Current status and influential factors associated with adherence to self-monitoring of blood glucose with type 2 diabetes mellitus patients in grassroots communities: a cross-sectional survey based on information-motivation-behavior skills model in China. Front Endocrinol (Lausanne). 2023;14:1111565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 6. | Editorial Board of the Chinese Journal of Digestion. [Consensus opinion on medical treatment of chronic cholecystitis and gallstones in China (2014, Shanghai)]. Linchuang Gandanbing Zazhi. 2015;31. [DOI] [Full Text] |
| 7. | Mihai EE, Popescu MN, Iliescu AN, Berteanu M. A systematic review on extracorporeal shock wave therapy and botulinum toxin for spasticity treatment: a comparison on efficacy. Eur J Phys Rehabil Med. 2022;58:565-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Thompson E. Hamilton Rating Scale for Anxiety (HAM-A). Occup Med (Lond). 2015;65:601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 304] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 9. | Williams JB, Kobak KA, Bech P, Engelhardt N, Evans K, Lipsitz J, Olin J, Pearson J, Kalali A. The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol. 2008;23:120-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 202] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 10. | Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016;4:2050312116671725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 655] [Cited by in RCA: 631] [Article Influence: 70.1] [Reference Citation Analysis (0)] |
| 11. | Wang Q, Zhu R, Cao Y, Ning Y, Feng Y, Feng Y, Han S. Sublingual immunotherapy adherence in patients with allergic rhinitis: Effects of an intervention based on the information-motivation-behavioral skills model. Heliyon. 2023;9:e22929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Wen XF, Chen SH, Fu QX. [Effect of Otago motion-assisted IMB behavior pattern on total knee replacement patients]. Qilu Huli Zazhi. 2023;80-82. |
| 13. | Guo SY. [Effects of IMB model-based nursing intervention on rehabilitation, self-efficacy and quality of life of patients undergoing esophageal cancer surgery]. Xiandai Zhongxiyi Jiehe Zazhi. 2023;561-564. |
| 14. | Chen PP, Zhang WJ, Wang J. [Effects of retrolaparoscopic partial nephrectomy on the expression of complications, Cor, AD and NE in patients with hilar tumor]. Qvanke Yixve Linchuang Yv Jiaoyu. 2020;132-134. |
| 15. | Wang YY, Liu XF, Lv DM. [Effect of IMB model intervention mode on patients with malignant bone tumors]. Qilu Huli Zazhi. 2023;9-11. |
| 16. | Li M, Zhu H. Application of intervention of information motivation behavior skill (IMB) model in the cardiac rehabilitation of patients with coronary heart disease. Pak J Med Sci. 2022;38:1627-1632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 17. | Xu H, Wang J. An information-motivation-behavioral skills model-based intervention for patients with epilepsy. Epilepsy Behav. 2023;147:109408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 18. | Kuang J, Li Y, Deng S, Su J, Gong S, Wang Y. Effect of information-motivation-behavior skills on adherence of continuous positive airway pressure therapy in patients with obstructive sleep apnea hypopnea syndrome. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2022;47:479-487. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Lu JM. [Effect of perioperative comprehensive nursing mode on pain and prognosis of patients undergoing gallstone surgery]. Guoji Hulixve Zazhi. 2019;38:3207-3209. [DOI] [Full Text] |
| 20. | Fang Y, Zhou CR, Lu ZB, Xiao ZC, Pan CF. [Application of nursing intervention based on information-motivation-behavioral skill model in CT-guided localization of patients with isolated pulmonary nodules]. Shiyong Linchunag Yiyao Zazhi. 2023;98-104. |