Published online Jul 27, 2024. doi: 10.4240/wjgs.v16.i7.2202
Revised: June 11, 2024
Accepted: June 24, 2024
Published online: July 27, 2024
Processing time: 75 Days and 23.8 Hours
The totally preperitoneal (TPP) approach is a new concept that was recently int
To analyze the potential applications of single-incision laparoscopic TPP (SIL-TPP) inguinal hernia hernioplasty for the treatment of inguinal hernias.
A total of 152 SIL-TPP surgeries were performed at the First Affiliated Hospital of Ningbo University from February 2019 to November 2022. A single-port, named Iconport, and standard laparoscopic instruments were used during the operation. Demographic data, intraoperative parameters and short-term postoperative out
The demographic data of 152 patients underwent SIL-TPP were shown in Table 1. The average age was 49.5 years (range from 21 to 81 years). The average body mass index was 27.7 kg/m2 (range from 17.7 kg/m2 to 35.6 kg/m2). SIL-TPP were conducted successfully in 147 patients. Three patients were converted to the SIL-transabdominal preperitoneal laparoscopic herniorrhaphy at the initial stage of the study due to a lack of experience. In 2 patients with incisional hernias, an auxiliary operation hole was added during the SIL-TPP procedure, as required for surgery. The mean operative time was 64.5 minutes (range: 36.0-110.0 minutes) for unilateral direct and femoral hernias and 81.6 minutes for indirect hernias (range: 40.0-150.0 minutes). The mean postoperative hospital stay was 3.4 days.
SIL-TPP is feasible and has advantages for inguinal hernia repair. SIL-TPP has potential benefits for patients with various abdominal wall hernias. Consequently, doctors should be encouraged to actively apply the TPP approach combined with a single incision in their daily work.
Core Tip: Totally preperitoneal (TPP) is a novel concept that was recently introduced and differs from totally extraperitoneal hernioplasty (TEP). Our previous findings suggested that the TPP approach could advance single-incision laparoscopic (SIL) inguinal hernia repair of unilateral inguinal hernias more feasibly than could SIL-TEP. The procedure was named SIL-TPP. SIL-TPP has unique characteristics and advantages. However, evidence for the characteristics of the SIL-TPP or TPP approach is scarce. SIL-TPP has potential benefits for patients with various abdominal wall hernias. In addition, the TPP approach combined with a single incision merits further research to elucidate its feasibility and advantages for treating other abdominal hernias, including emergency cases, incisional hernias, and umbilical hernias.
- Citation: Wang XJ, Fei T, Xiang XH, Wang Q, Zhou EC. Potential applications of single-incision laparoscopic totally preperitoneal hernioplasty. World J Gastrointest Surg 2024; 16(7): 2202-2210
- URL: https://www.wjgnet.com/1948-9366/full/v16/i7/2202.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i7.2202
Inguinal hernia is a common surgical disease. The operation method has evolved from open to laparoscopic surgery. The approach surgeons choose depends on the patient’s condition and the surgeon’s experience. Laparoscopic totally ex
Since Cugura et al[3] firstly reported single-incision laparoscopic totally extraperitoneal hernioplasty (SIL-TEP) with a case report in 2008, much evidence has revealed the safety and feasibility of this operation[4,5]. However, evidence also suggests that SIL-TEP has inherent disadvantages, such as limited operation space, in-line positioning of the laparoscope, and instrument conflict, among others, which cannot be overcome through improved surgical skills[5,6]. Considering that the abdominal wall consists of nine layers, we previously introduced the totally preperitoneal (TPP) approach and succee
The aim of current study was to demonstrate the safety and feasibility of SIL-TPP for inguinal hernia repair and to share our initial operation experience.
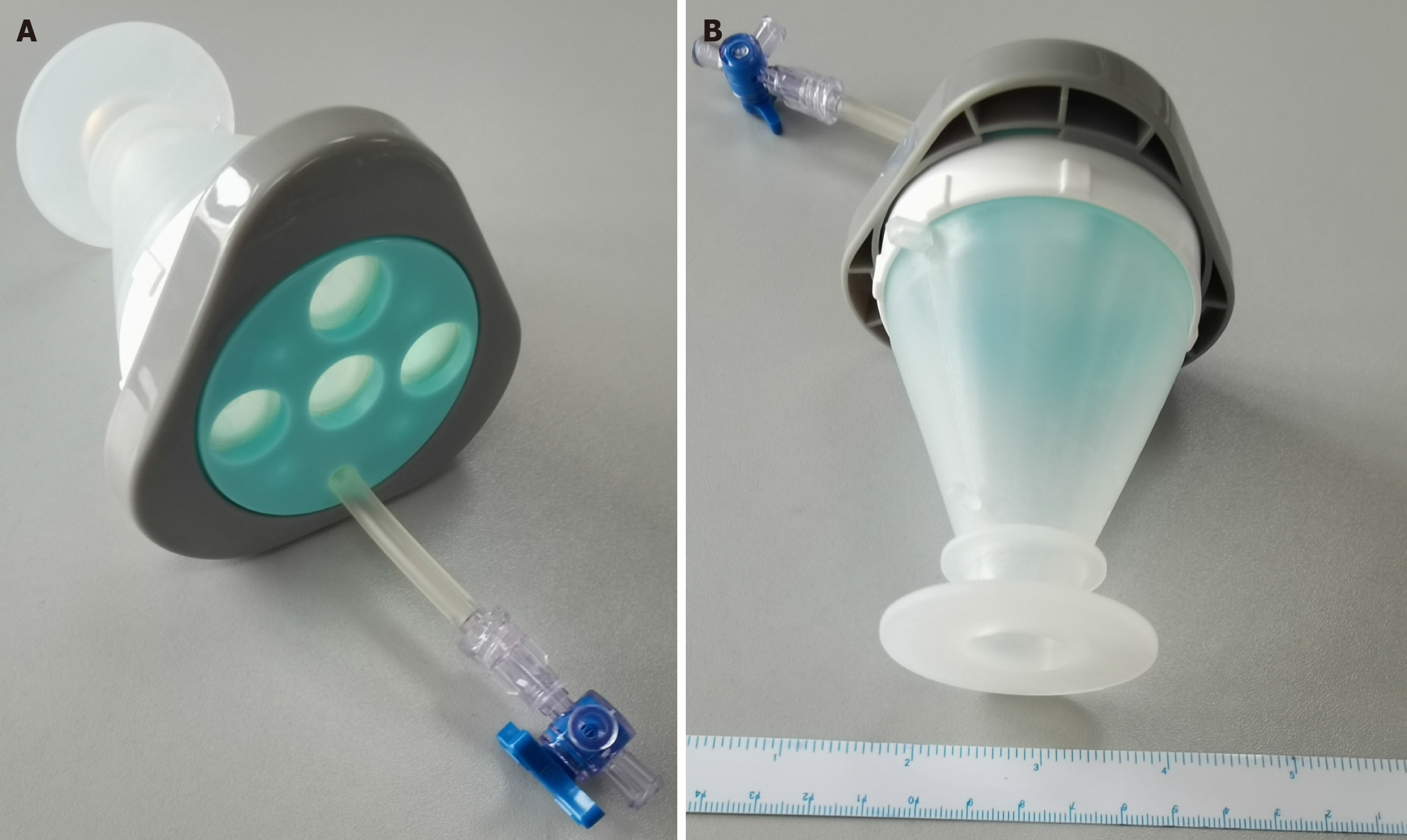
The Iconport single-hole device (Iconport, United States patent No. US9393003B2 Chinese patent No. 201110229309.4) (Figure 1) and conventional instruments, including a conventional 30-degree laparoscope (STORZ, Germany), were used to conduct SIL-TPP through a PPS single incision. The Iconport device is made up by a medical polypropylene plastic operating panel and an incision protective sleeve. The characteristics of the Iconport were described in our previous study[7].
One hundred and fifty-two patients accepted laparoscopic hernia repair during February 2019 and November 2022 at our hospital were retrospectively analyzed. All patients with an abdominal wall hernia admitted in our department were considered for SIL-TPP. These patients were excluded: (1) Aged less than 20 years; and (2) Compromised cardiopulmonary function who could not tolerate general anesthesia. These excluded patients were performed with open hernia repair. In current study, only short-term outcomes were analyzed. All operations were conducted after informed consent was obtained from the patients. Besides, the study was approved by the Institutional Review Board of hospital. This work is reported in line with the STROCSS criteria. The project’s registration number in the Chinese Clinical Trial Registry is ChiCTR1900023056.
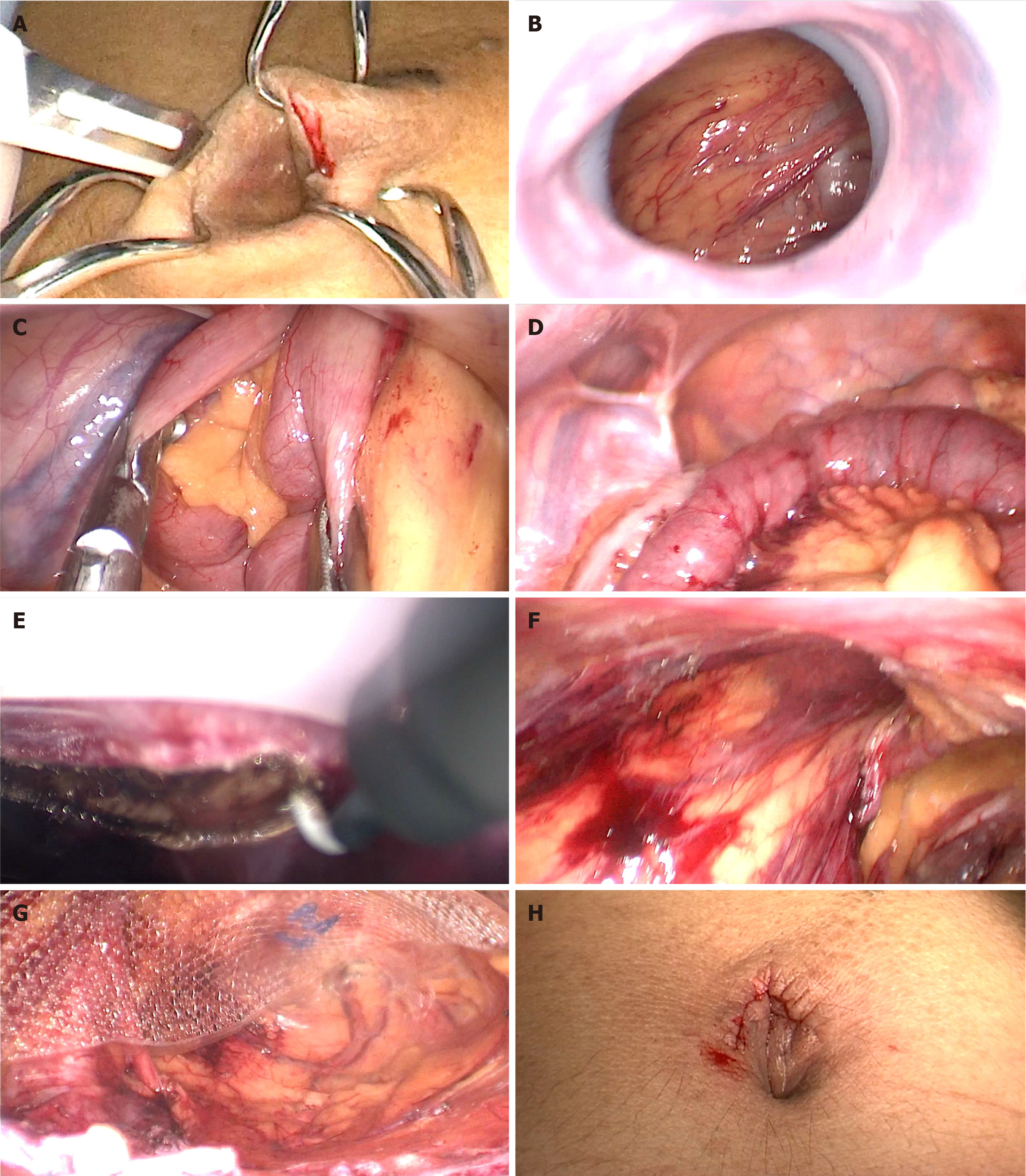
Operation was conducted with general anesthesia. Patients was in a supine position. The arm opposite to the side of the hernia was adducent along chest wall. In step 1, PPS single incision was established. A 2.5 cm skin incision along the lower umbilical border was made (Figure 2A). The aponeurotic layer was exposed after subcutaneous tissue was incised. In step 2, the aponeurotic layer was incised open thus entering the PPS single incision behind the linea alba. In step 3, the single port device was inserted into single PPS incision under the aponeurotic layer. If the peritoneum suffered rupture at the beginning of operation, abdominal exploration was performed first. After exploration, the lower abdominal peritoneum near the umbilical incision was pulled intraperitoneally and separated from posterior sheath of rectus abdominis thus creating the PPS required for SIL-TPP (Figure 2B-E). In step 4, the PPS was gradually seperated with conventional laparoscopic instruments. The primary anatomic landmarks, including the inferior epigastric vessels, pubic bone, anterior superior spine, corona mortis, and Cooper’s ligaments, were identified. Then, SIL-TPP was performed according to routine procedures[7,8] (Figure 2F). In step 5, the mesh was placed. Several types of polyester meshes were placed into the PPS (Figure 2G). In step 6, the single incision was sutured with absorbable suture. After closing the linea alba, and the skin was sutured with subcuticular methods (Figure 2H).
Sac was carefully isolated from the internal ring for indirect hernia patients. The hernia sacs were routinely ligated more than 6 cm from the spermatic cord. The uterus round ligament was routinely reserved for female patients. The rupture peritoneum or sac was closed with hemlock, endoloop or through suturing (Figure 2F).
For direct hernia patients, the hernia sac was isolated, and the defect in the transversalis fascia was reduced by suturing the defect in the transversalis fascia to the surrounding tough tissue, thus preventing seroma formation.
For umbilical hernia, a single PPS incision was established between the umbilicus and symphysis pubis. After the single incision was established, the Iconport single-port device was inserted, and the PPS underneath the posterior rectus abdominis sheath was separated. Since the umbilical hernia sac is usually gauzy and tightly attached to the sheath, it was usually transected. In addition, the lateral peritoneum exceeding the umbilicus level is usually gauzy, and there is little fatty tissue covering the peritoneum. As a result, the operation should be conducted carefully in small steps to protect the peritoneum from tearing. For the incision hernia, a single PPS incision was established at a position distinct from the hernia. The scar is usually difficult to separate, and hence, the sac is usually gauzy and tightly attached to the sheath. However, the dissected peritoneum is typically thick and the broken sac could be sutured effortlessly. After suturing the ruptured peritoneum, the mesh was placed in the PPS layer.
The age, sex, American Society of Anesthesiologists (ASA), body mass index (BMI), classification, hernia site, conversion, operative time, amount of bleeding, postoperative hospital stay duration, complications, hernia recurrence and follow-up duration were collected. A team member assessed the patients’ pain using the visual analog scale (VAS) 24 hours after surgery. A part of patients was followed up through outpatient visits, whereas other patients were followed up via phone calls. For patients who could not be contacted by phone, the findings collected from last follow-up were used in the analysis. The results are demonstrated as numbers (percentages) or the means ± SD.
A total of 152 patients were enrolled for the study. The SIL-TPP procedure was successful in 147 patients. Three patients were converted to conventional TAPP because of a lack of experience when peritoneum rupture occurred during the establishment of a single incision. In 2 patients with incisional hernias, an auxiliary operation hole was added during the SIL-TPP operation, as required for surgery. After an auxiliary operation hole was added, the operation conducted via the TPP approach was effective. Patients’ demographics data and hernia characteristics are shown in Table 1. Among these 152 patients, 25 were females and 127 were males. The average age was 49.5 years (range: 21-81). The mean BMI was 27.7 kg/m2 (range from 17.70 kg/m2 to 35.60 kg/m2). The median ASA score was 1.1 (range from 1 to 2). Three types of hernias were identified during the operation: Inguinal hernia, umbilical hernia and incisional hernia. There were 70 right inguinal hernias (69.60%, 70/180), 57 left inguinal hernias (14.71%, 15/102) and 21 bilateral inguinal hernias. Two patients with umbilical hernias and 3 patients with incisional hernia were also enrolled in the study. In addition, there was 1 patient with an umbilical hernia combined with a right indirect hernia. Inguinal hernias were also classified as the Gilbert type. There were 42 cases of indirect hernia belonging to the Gilbert I group, 53 cases belonging to the Gilbert II group, and 38 cases belonging to the Gilbert III group. Among patients with direct hernias, 17 and 19 cases were Gilbert IV and Gilbert V, respectively. Among patients with femoral hernias, 11 cases were Gilbert VII. In addition, 6 cases of scrotal inguinal hernias and 5 cases of incarcerated inguinal hernias were also recruited into the study.
| Variable | Value |
| Number of patients | 152 |
| Sex | |
| Male | 127 |
| Female | 25 |
| Mean age (year) | 49.5 (range: 21.0-81.0) |
| Mean BMI, kg/m2 | 27.7 (range: 17.7-35.6) |
| Median ASA | 1.1 (range: 1.0-2.0) |
| Main type of hernias | |
| Right inguinal hernia | 70 |
| Left inguinal hernia | 57 |
| Bilateral inguinal hernia | 20 |
| Umbilical hernia | 2 |
| Incisional hernia | 3 |
| Gilbert type (Gilbert type) | 180 |
| Indirect hernia | 133 (Gilbert I, 42; Gilbert II, 53; Gilbert III, 38) |
| Direct hernia | 36 (Gilbert IV, 17; Gilbert V, 19) |
| Femoral hernia | 11 (Gilbert VII, 11) |
| Scrotal hernia | 6 |
| Incarcerated hernia | 5 |
The operation parameters are shown in Table 2. The mean operative time was 64.5 minutes (range from 36.0 to 110.0 minutes) for direct hernias and 81.6 minutes (range from 40.0 to 150.0 minutes) for indirect hernias. The mean operative time for bilateral inguinal hernias was 113.8 minutes (range 60.0 to 210.0 minutes). The average pain VAS score on postoperative first day was 1.8 ± 0.9. The intact uterine round ligament was protected in female inguinal hernia patients. Any unintended intraoperative event that influenced the operative procedure was defined as a complication. There were 42 patients occurred intraoperative complications in 152 patients (27.63%). The intraoperative complications in the study comprised mostly unintentional peritoneum tearing, hernial sac rupture or intentional amputation of the hernial sac in patients with scrotal hernias. Three patients sustained internal spermatic vessel injury, and 2 patients sustained inferior epigastric vessel injury. These patients did not report any discomfort during the follow-up period (15 months). No other major complications, such as bleeding, bowel injury, bladder injury, or transection of the vas deferens, occurred in our study.
| Variable | Value |
| Mean operative time, minute (range) | - |
| Indirect | 81.6 (40-150) |
| Direct or femoral | 64.5 (36-110) |
| Both | 113.8 (60-210) |
| Keep the uterine round ligament intact | 25 |
| Conversation | 1.97% (3/152) |
| Add auxiliary hole | 1.31% (2/152) |
| Intraoperative complication | 27.63% (42/152) |
| Accidental peritoneal rupture | 28 |
| Hernial sac amputation | 9 |
| Ductus deferens injury | 0 |
| Internal spermatic vessel injury | 3 |
| Inferior epigastric vessel injury | 2 |
| Corona mortis bleeding | 0 |
Postoperative complications occurred in 5/152 patients (3.29%) (Table 3). Three postoperative complications occurred: 4 seromas and 1 incisional hematoma. These complications were treated conservatively. There were few patients accepted catheterization. Moreover, there was no urinary retention occurred. The VAS scores at 24 hours were 1.8 ± 0.9. The average postoperative hospital stay was 3.40 days. Remarkably, most patients’ wound pain was little when they returned home. No other significant complications, such as chronic pain, mesh infection, umbilical hernia, testicular atrophy or urinary retention, were informed during the follow-up period. Moreover, there was no recurrence and mortality.
| Variable | Data |
| Postoperative complication | 3.29% (5/152) |
| Mesh infection | 0 (0) |
| Wound infection | 0 (0) |
| Incision hematoma | < 1% (1/152) |
| Seroma | 2.63% (4/152) |
| Sanguineous apoplexy/stroke | 0 (0) |
| Delirium | 0 (0) |
| Upper respiratory infection | 0 (0) |
| Urinary retention | 0 (0) |
| Urinary tract infection | 0 (0) |
| Hydrocele of testes | 0 (0) |
| VAS score (postoperative 24 hours, mean) | 1.8 ± 0.9 |
| Postoperative hospital day | 3.40 |
| Testicular atrophy | 0 |
| Chronic pain | 0 |
| Umbilical hernia | 0 |
| Recurrence (Until June 2022) | 0 |
Both tension-free hernia repair and laparoscopic hernia repair are basic approaches for the treatment of abdominal wall hernias. For simple conditions, such as inguinal hernia, TAPP or TEP may be selected because both have comparable success rates[2]. Since the first case of SIL-TEP reported in 2008, increasing evidence has verified the safety of the procedure. However, SIL-TEP has disadvantages that cannot be overcome by improving surgical skills. Since 2018, we have attempted to successfully perform single-incision inguinal hernia repair via the TPP approach[7,8]. In addition, comparison of SIL-TPP and SIL-TEP showed that SIL-TPP could overcome the disadvantages of SIL-TEP, such as a confined operation space and adverse factors resulting from peritoneum rupture[9]. However, investigation of the SIL-TPP characteristics is still in its primary stage. The results of the present study revealed that the use of SIL-TPP is safe and feasible. In addition, we shared our initial experience.
In this study, SIL-TPP was successfully performed for 147 patients with indirect, direct, or femoral hernias. The average operative times were 64.5 minutes (range from 36.0 to 110.0 minutes) and 81.6 minutes (range from 40.0 to 150.0 minutes) for unilateral direct or femoral hernia and unilateral indirect hernia, respectively. The average operative time was 113.8 minutes (range from 60.0 to 210.0 minutes) for bilateral hernias. The operative time from our initial experience for inguinal hernia repair was comparable to that in previous SIL-TEP studies[10-12]. In addition, the incidence of intraoperative complications was 27.63%, and the majority of common intraoperative complications were tearing of the sac and peritoneum. The peritoneum tear rate was 24.34%. The peritoneum tear rate in our initial experience was comparable to that in previous studies[7]. Three patients experienced internal spermatic vessel injury, and 2 patients experienced inferior epigastric vessel injury. The complication rate was 3.27%, which was comparable to that reported in previous studies[10,13]. No other intraoperative complications occurred in the current study.
Since 2017, we have attempted to perform SIL inguinal hernia repair through the TPP approach using a self-developed laparoscopic single-incision sealing instrument (Iconport, United States patent No. US9393003B2, Chinese patent No. 201110229309.4) (Figures 1 and 2). The results suggested that SIL-TPP was a safe and feasible procedure[7,8]. In the initial stage of the study, peritoneal damage occurred in 3 patients at the beginning of the operation, and the author im
The TPP approach is a new concept we introduced to distinguish TEPs. Compared with SIL-TEP, the TPP approach for advancing SIL inguinal hernia repair is more feasible[9]. Many scholars have realized that the PPS is a whole and soft space enveloping the abdominal viscera[16,17]. TPP is a strategy to utilize the PPS. However, few reports have described laparoscopic exploration in PPS. Our previous studies verified that the TPP approach and SIL-TPP have advantages[7,9]. Consequently, the use of TPP and SIL-TPP in laparoscopic hernia repair merits further research. In the initial stage of the study, 3 patients were directly transferred from the SIL-TPP technique to the conventional TAPP technique when the peritoneum ruptured during the PPS incision due to our limited experience. These failures reminded us that SIL-TPP, SIL-TEP and SIL-TAPP, TAPP, IPOM and open surgery can be applied simultaneously in a single surgical process to complement one another. By simultaneously performing laparoscopic hernia repair using the TPP approach to TEP or TAPP, instead of exclusively performing the procedure in one or the other, the surgeon may perform various types of abdominal wall hernia surgeries using simple procedures with satisfactory therapeutic effects. Remarkably, in our study, 3 patients who experienced incisional hernia and 2 patients who experienced umbilical hernia underwent SIL-TPP. For these cases, IPOM is now the most commonly used technique. However, intraperitoneal mesh causes serious complications related to adhesions[18,19]. Consequently, a series of methods, such as endoscopic/mini-open sublay (eMILOS) repair, totally endoscopic sublay repair and the totally extraperitoneal (eTEP) approach, have been reported to avoid intraperitoneal mesh placement[20-22]. The results revealed that extraperitoneal placement is promising for avoiding complications associated with intraperitoneal mesh placement[23,24]. In the present study, we treated 3 patients with incisional hernia and 2 patients with umbilical hernia using the TPP approach via a single incision. We made use of the PPS, and the meshes were also placed in the PPS. In addition, our procedure avoided tendon tissue damage and complex procedures compared to the eTEP procedure[25]. This approach also has the advantage of avoiding disturbance of the visceral tissue compared to TAPP surgery[24]. However, in 2 patients with incisional hernias, an auxiliary operation hole was added during the SIL-TPP procedure, as required for surgery. The results suggested that SIL-TPP was also a safe and feasible procedure for incisional and umbilical hernias. In addition, an auxiliary hole could be added if necessary. Mo
The advantages of SIL-TPP are less trauma to patients and less damage to the abdominal wall during abdominal hernia repair than the conventional laparoscopic TEP procedure. The procedure makes use of PPS and differs from previously used operations. The advantages of the procedure could be amplified for ventral hernia repairs with robotic surgery in the future. We believe that this technique will benefit the majority of surgeons who treat ventral hernias after performing the TPP approach. Further studies are needed to verify the feasibility of SIL-TPP for different types of ventral hernia.
The research has several limitations as below. It is a retrospective study. The long-term results did not show in study. A long-term outcome study is needed to verify the safety of SIL-TPP for inguinal hernia repair. In addition, the number of incisional and umbilical hernias was small. More studies with larger populations of these complex hernia patients are needed to determine the characteristics and feasibility of SIL-TPP. The characteristics of the incisional and umbilical hernias were not examined in the present study.
SIL-TPP is a feasible procedure for inguinal hernia repair. We believe that SIL-TPP has potential benefits for patients with various abdominal wall hernias. Consequently, doctors should be encouraged to actively apply SIL hernia technology using the TPP approach in their daily work.
| 1. | HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1355] [Cited by in RCA: 1276] [Article Influence: 182.3] [Reference Citation Analysis (1)] |
| 2. | Stabilini C, van Veenendaal N, Aasvang E, Agresta F, Aufenacker T, Berrevoet F, Burgmans I, Chen D, de Beaux A, East B, Garcia-Alamino J, Henriksen N, Köckerling F, Kukleta J, Loos M, Lopez-Cano M, Lorenz R, Miserez M, Montgomery A, Morales-Conde S, Oppong C, Pawlak M, Podda M, Reinpold W, Sanders D, Sartori A, Tran HM, Verdaguer M, Wiessner R, Yeboah M, Zwaans W, Simons M. Update of the international HerniaSurge guidelines for groin hernia management. BJS Open. 2023;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 81] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 3. | Cugura JF, Kirac I, Kulis T, Janković J, Beslin MB. First case of single incision laparoscopic surgery for totally extraperitoneal inguinal hernia repair. Acta Clin Croat. 2008;47:249-252. [PubMed] |
| 4. | Suzuki Y, Wakasugi M, Mikamori M, Tamaoka K, Nakahara Y, Tei M, Furukawa K, Ohtsuka M, Masuzawa T, Akamatsu H. Long-term outcomes of single-incision versus multiport laparoscopic totally extra-peritoneal inguinal hernia repair: a single-institution experience of 186 consecutive cases. Surg Today. 2022;52:114-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 5. | Lee YJ, Kim JH, Kim CH, Lee GR, Lee YS, Kim HJ. Single incision laparoscopic totally extraperitoneal hernioplasty: lessons learned from 1,231 procedures. Ann Surg Treat Res. 2021;100:47-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Yang GP, Tung KL. A comparative study of single incision versus conventional laparoscopic inguinal hernia repair. Hernia. 2015;19:401-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Zhou E, Qi C, Wang X, Fei T, Huang Q. Single incision laparoscopic totally preperitoneal hernioplasty (SIL-TPP): Lessons learned from 102 procedures and initial experience. Medicine (Baltimore). 2022;101:e30882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Wang X, Fei T, Zhou E. Application of a custom-made single-incision sealing device in laparoscopic surgery for totally extraperitoneal herniorrhaphy: initial experience. Ann Transl Med. 2022;10:598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Huang Q, Wang X, Xiang X, Qi C, Fei T, Zhou E. TPP (totally preperitoneal) making single incision laparoscopic inguinal hernia repair more feasible: a comparison with single incision laparoscopic totally extraperitoneal hernioplasty (SIL-TEP). BMC Surg. 2024;24:81. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Wakasugi M, Suzuki Y, Tei M, Anno K, Mikami T, Tsukada R, Koh M, Furukawa K, Masuzawa T, Kishi K, Tanemura M, Akamatsu H. The feasibility and safety of single-incision totally extraperitoneal inguinal hernia repair after previous lower abdominal surgery: 350 procedures at a single center. Surg Today. 2017;47:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Wakasugi M, Tei M, Anno K, Mikami T, Tsukada R, Koh M, Furukawa K, Suzuki Y, Masuzawa T, Kishi K, Tanemura M, Akamatsu H. Single-incision totally extraperitoneal inguinal hernia repair as a teaching procedure: one center’s experience of more than 300 procedures. Surg Today. 2016;46:1039-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Choi BJ, Lee KJ, Lee SC. Direct application of single-port laparoscopic totally extraperitoneal (TEP) inguinal hernia repair by an experienced single-port laparoscopic surgeon who was inexperienced in conventional TEP hernia repair: initial experience with 100 cases. J Laparoendosc Adv Surg Tech A. 2014;24:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kim JH, Lee YS, Kim JJ, Park SM. Single port laparoscopic totally extraperitoneal hernioplasty: a comparative study of short-term outcome with conventional laparoscopic totally extraperitoneal hernioplasty. World J Surg. 2013;37:746-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Han YD, Park S, Kim WR, Baek SJ, Hur H, Min BS, Kim NK. Safety and Efficacy of Single-Incision Laparoscopic Totally Extraperitoneal Inguinal Hernia Repair: Comparative Study with Conventional Laparoscopic Totally Extraperitoneal Inguinal Hernia Repair. J Laparoendosc Adv Surg Tech A. 2017;27:253-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Park YY, Lee K, Oh ST, Lee J. Learning curve of single-incision laparoscopic totally extraperitoneal repair (SILTEP) for inguinal hernia. Hernia. 2022;26:959-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Read RC. Cooper’s posterior lamina of transversalis fascia. Surg Gynecol Obstet. 1992;174:426-434. [PubMed] |
| 17. | Mirilas P, Colborn GL, McClusky DA 3rd, Skandalakis LJ, Skandalakis PN, Skandalakis JE. The history of anatomy and surgery of the preperitoneal space. Arch Surg. 2005;140:90-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Henriksen NA, Montgomery A, Kaufmann R, Berrevoet F, East B, Fischer J, Hope W, Klassen D, Lorenz R, Renard Y, Garcia Urena MA, Simons MP; European and Americas Hernia Societies (EHS and AHS). Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. Br J Surg. 2020;107:171-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 188] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 19. | Patel PP, Love MW, Ewing JA, Warren JA, Cobb WS, Carbonell AM. Risks of subsequent abdominal operations after laparoscopic ventral hernia repair. Surg Endosc. 2017;31:823-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 20. | Schwarz J, Reinpold W, Bittner R. Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbecks Arch Surg. 2017;402:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 21. | Li B, Qin C, Bittner R. Totally endoscopic sublay (TES) repair for midline ventral hernia: surgical technique and preliminary results. Surg Endosc. 2020;34:1543-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Belyansky I, Daes J, Radu VG, Balasubramanian R, Reza Zahiri H, Weltz AS, Sibia US, Park A, Novitsky Y. A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc. 2018;32:1525-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 232] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 23. | Warren JA, Cobb WS, Ewing JA, Carbonell AM. Standard laparoscopic versus robotic retromuscular ventral hernia repair. Surg Endosc. 2017;31:324-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 24. | Kennedy M, Barrera K, Akcelik A, Constable Y, Smith M, Chung P, Sugiyama G. Robotic TAPP Ventral Hernia Repair: Early Lessons Learned at an Inner City Safety Net Hospital. JSLS. 2018;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Prakhar G, Parthasarathi R, Cumar B, Subbaiah R, Nalankilli VP, Praveen Raj P, Palanivelu C. Extended View: Totally Extra Peritoneal (e-TEP) Approach for Ventral and Incisional Hernia-Early results from a single center. Surg Endosc. 2021;35:2005-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |