Published online Jun 27, 2024. doi: 10.4240/wjgs.v16.i6.1948
Revised: May 10, 2024
Accepted: May 24, 2024
Published online: June 27, 2024
Processing time: 112 Days and 2.8 Hours
The management of polyps involving the appendiceal orifice (AO) presents notable challenges. Endoscopic resection is frequently hindered by operational complexities, a heightened risk of incomplete removal, and an elevated risk of procedural complications, including appendicitis. Conversely, surgical resection may entail unnecessary excision of intestinal segments, leading to potential morbidity.
Here, we reported two patients who presented with polyps deeply situated within the AO, with indistinct boundaries making it challenging to ensure completeness using traditional endoscopic resection. To overcome these challenges, we em
The application of CELS in managing polyps involving the AO is emerging as a safe and effective treatment modality.
Core Tip: Resecting polyps involving the appendiceal orifice (AO) poses a significant challenge. Endoscopic treatment risks incomplete resection and high postoperative complications, while surgery may entail excessive removal of normal intestinal segments, leading to additional damage. Here, we present two cases of deeply extended polypoid lesions in AO, where vague boundaries hindered complete resection with traditional endoscopy. Hence, we adopted a combined endo-laparoscopic surgery (CELS) approach, achieving curative resection without postoperative complications. Our experience confirms that CELS is a safe and effective method for AO polyp removal, meriting further exploration.
- Citation: Zhang YY, Lu JY, Wang Q, Yang AM. Resection of polyps involving the appendiceal orifice by combined endo-laparoscopic surgery: Two case reports. World J Gastrointest Surg 2024; 16(6): 1948-1952
- URL: https://www.wjgnet.com/1948-9366/full/v16/i6/1948.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i6.1948
Resecting polyps involving the appendiceal orifice (AO) poses a significant challenge. Endoscopic resection is hindered by a confined working space and the limited maneuverability of the endoscope. Simultaneously, this approach carries a heightened risk of incomplete resection, perforation, and post-resection appendicitis. Surgical resection faces challenges in accurately delineating the lesion border under a laparoscope. This difficulty may lead to extended surgery, potentially necessitating the removal of the right hemi-colon, resulting in excessive damage for a benign lesion.
In this context, we present two cases involving polyps extending to the AO, successfully treated with combined endo-laparoscopic surgery (CELS), which provide an effective and safe method for the resection of lesion involving the AO.
Case 1: A 71-year-old female underwent colonoscopy as part of a routine physical examination, reporting no discomfort.
Case 2: A 49-year-old male underwent colonoscopy as part of a routine health screening.
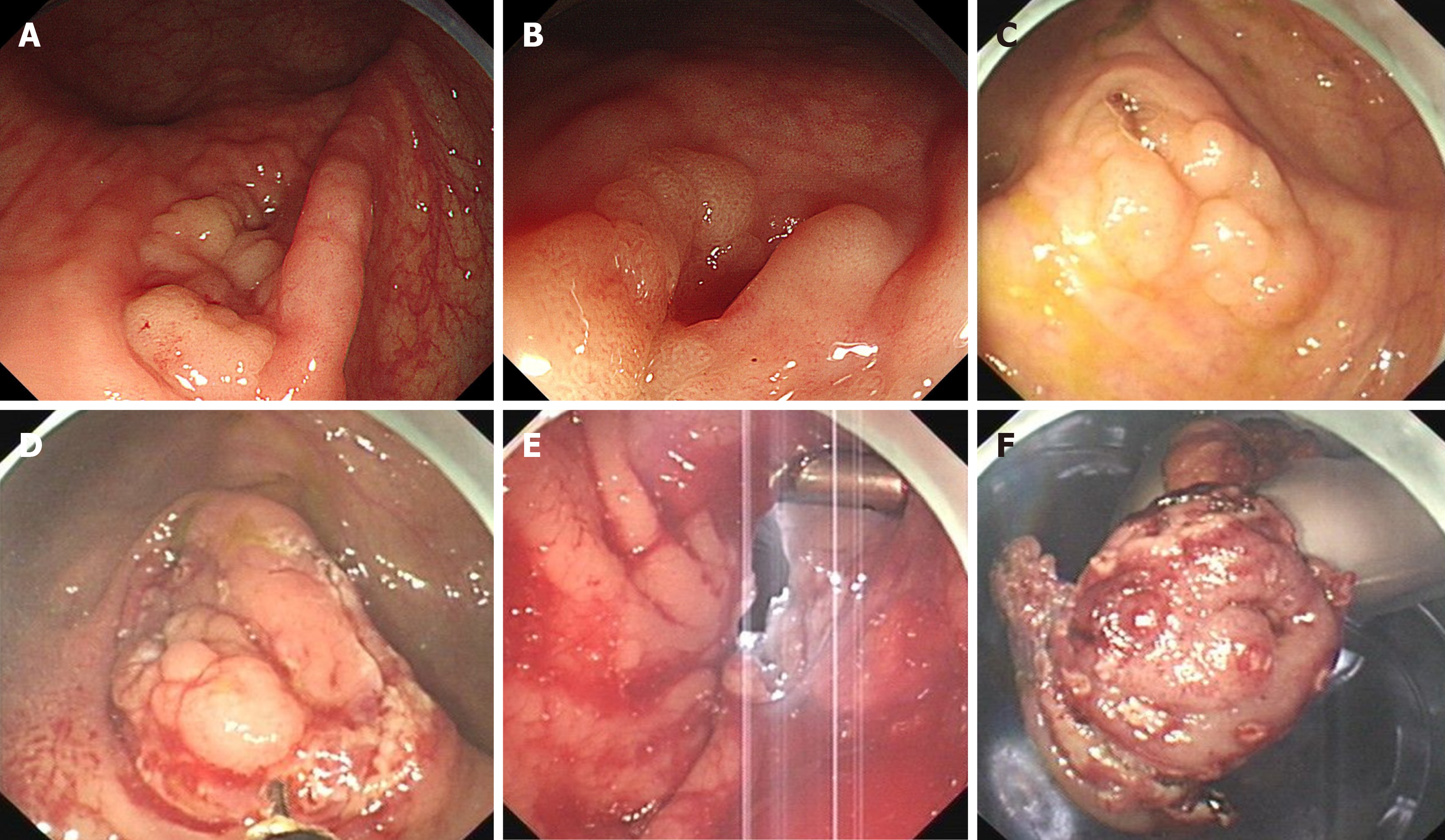
Case 1: During the examination, a 20-mm laterally spreading tumor encircling the AO was identified in the cecum, and the edge of the lesion remained invisible (Figure 1).
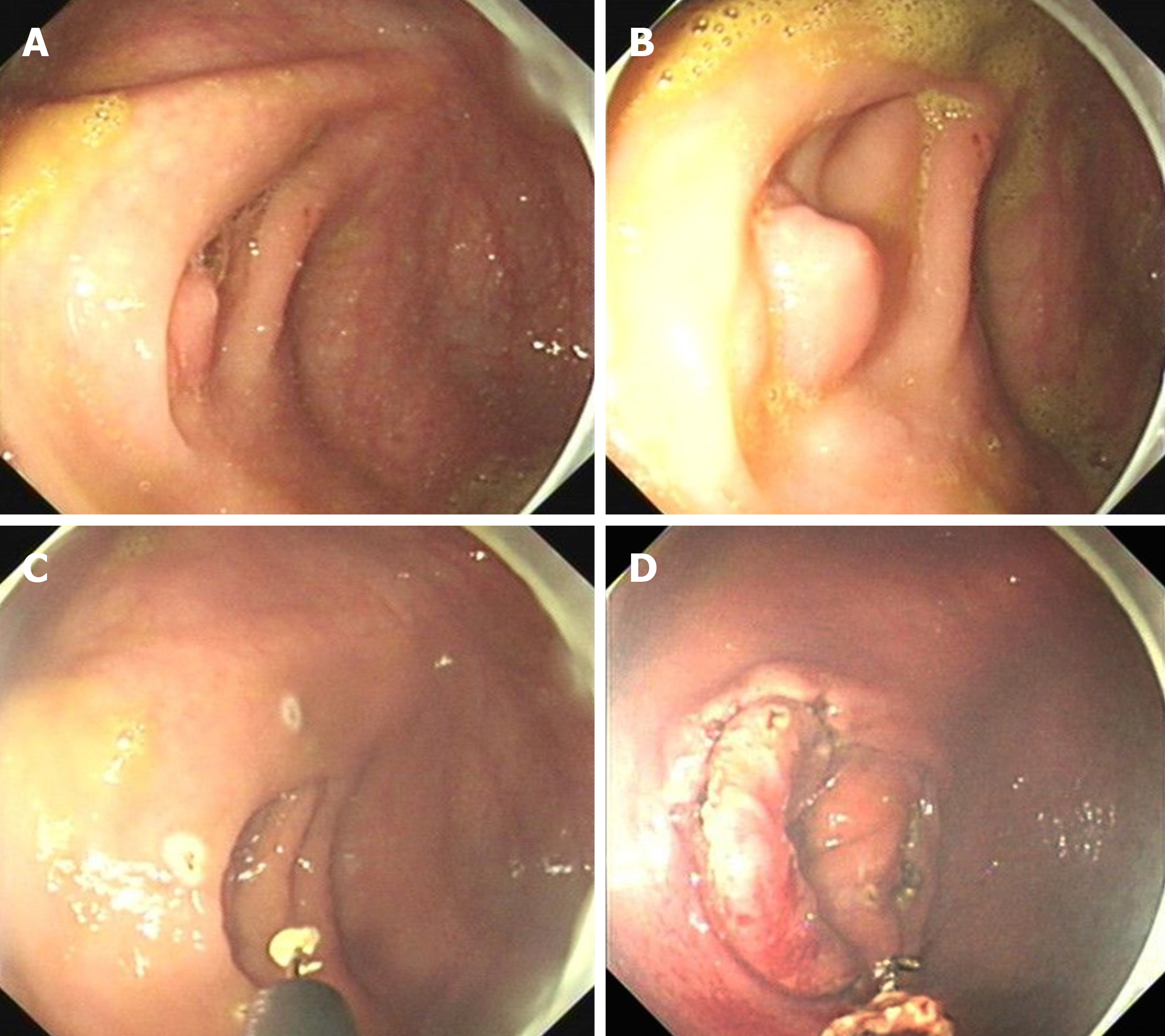
Case 2: Colonoscopy revealed multiple polyps in the AO, with the largest measuring 6mm, and the root of the polyp could not be exposed (Figure 2A and B).
Case 1: The patient had a history of hypertension and hyperlipidemia, with no reported instances of abdominal pain, rectal bleeding, or weight loss.
Case 2: The patient had a history of diabetes. He had no history of abdominal pain or weight loss.
Case 1: The patient was not aware of any family history of malignant tumors.
Case 2: The patient denied any family history of malignant tumors.
Case 1: During the physical examination, the patient had a body temperature of 36.5 °C, blood pressure of 127/73 mmHg, heart rate of 78 beats per minute, and respiratory rate of 18 breaths per minute. Abdominal examination revealed no signs of pressure or rebound pain, and no palpable abdominal masses were noted.
Case 2: During the physical examination, the patient had a body temperature of 36.2 °C, blood pressure of 118/72 mmHg, heart rate of 72 beats per minute, and respiratory rate of 19 breaths per minute. He showed no signs of pressure or rebound pain during abdominal examination. No masses were palpable.
Case 1: Histopathological examination of the lesion confirmed tubular adenoma. Other laboratory examinations yielded normal results.
Case 2: Biopsy pathology of the lesion revealed tubular adenoma.
Case 1: Aside from the endoscopic abnormality, no other abnormalities were detected on imaging examinations.
Case 2: Aside from the endoscopic abnormality, the patient had no other abnormalities on imaging examinations.
Both cases were diagnosed as tubular adenoma extending into the AO.
Given the risk of incomplete resection and subsequent appendicitis associated with traditional endoscopic submucosal dissection (ESD) due to the lesions’ obscured margins, the CELS technique was chosen for polyp removal in both patients.
Pre-operative bowel preparation was conducted for both patients a day prior to the procedure, consistent with colonoscopy requirements. The surgeries were performed under general anesthesia. After the insertion of a nasogastric tube and urinary catheter, the patient was placed in lithotomy position to facilitate colonoscopy, which was carried out with carbon dioxide insufflation.
The approach to polyp removal was largely consistent between the two patients. The endoscopist began by exploring and identifying the lesion (Figure 1C). The lesion’s borders were then marked circumferentially using a hook knife set to soft coagulation ERBE mode (Figure 2C). Then, a near-full-thickness incision was executed around the lesion using the hook knife in endocut mode (Figures 1D and 2D), aiming to visualize the lesion’s boundaries from the serosal surface during laparoscopy. Pneumoperitoneum was established to inspect the abdominal cavity, and three trocars were introduced. The marked lesion boundaries from the endoscopy were clearly visible on the serosal surface. Using an ultrasonic knife guided by the colonoscope’s cutting line, incisions were made through the layers of the cecal wall (Figure 1E). The appendix, together with a portion of the cecum, was excised to ensure complete removal of the cecal mass. The incision in the cecum was then meticulously closed using 3-0 V-lock sutures. The specimen, enclosed in a specimen bag, was extracted through the primary operating port and sent for pathological evaluation.
The gross examination of the specimen revealed markers around the lesion’s outer edge, confirming the completeness of the resection (Figure 1F). Furthermore, both pathological examinations confirmed the presence of tubular adenomas, which were completely excised with clear margins. The distance from the edge of the lesions to the resection margin was 7 mm in both cases.
Both patients abstained from oral intake for two days post-surgery, gradually resuming under close supervision thereafter. Encouragingly, neither patient encountered any postoperative complications, such as bleeding or perforation. They were both discharged from the hospital five days after the surgical procedure, indicating a smooth recovery process.
In this report, we present two cases of polyps extending into the AO, with the lesion border extending into the appendix, posing challenges in recognition. The polyp was resected using CELS, achieving R0 resection without postoperative complications. This procedure offers several advantages.
Firstly, it ensures en bloc resection and improves the R0 resection rate. The primary technical challenge in endoscopic resection of AO lesions is achieving an R0 resection due to difficulties in recognizing the lesion border, particularly for those lesions extending into the appendiceal lumen. In traditional ESD, the rate of complete histological resection was only 76.7%[1]. Traction techniques can help expose the lesion border[2], but if the lesion extends deep into the appendiceal lumen, exposing the lesion boundaries can remain challenging even with traction. By contrast, we confirmed the lesion boundary outside the appendix using colonoscopy and marked the border with a near-full-thickness resection. This enabled precise recognition of the boundary during laparoscopy, reducing the extent of surgical resection while ensuring complete lesion removal. Both gross appearance and microscopic examination confirmed the en bloc R0 resection of the lesion in both patients.
Secondly, the procedure exhibits a high level of safety. Endoscopic resection of AO lesions with complete appendix preservation poses a high risk of postoperative appendicitis. This may result from inadequate drainage of the AO post-procedure. The postoperative appendicitis rate for endoscopic full-thickness resection (EFTR) can reach as high as 17%[3]. Despite EFTR achieving a high R0 resection rate of up to 93%[3], its widespread application is severely limited by the excessively high rate of postoperative appendicitis. Since the CELS procedure removes the appendix completely, the risk of post-operative appendicitis is eliminated.
Lastly, the procedure exhibits high accessibility and reliability. Both endoscopic circumferential near-full-thickness resection of the appendix and laparoscopic appendectomy are fundamental procedures for endoscopists and surgeons. This ensures that the procedure is easily learned and can be widely adopted. There are some emerging technologies, such as endoscopic transcecal appendectomy (ETA), offering a balance between a high R0 resection rate and low complication rate[4]. ETA involves a near-circumferential full-thickness resection of the appendix, introduction of the endoscope into the abdominal cavity, dissection of the appendiceal mesentery, and ultimately complete appendectomy[5]. However, this procedure demands a high level of technical skill and a thorough understanding of abdominal anatomy from endoscopists, limiting its widespread adoption.
We present a novel procedure for treating polys involving the AO, demonstrating a high level of efficacy, safety and accessibility. We believe that CELS can be widely employed for the treatment of appendiceal polyps. However, more case reports are required to more robustly determine its efficacy and safety in the future.
| 1. | Song EM, Yang HJ, Lee HJ, Lee HS, Cha JM, Kim HG, Jung Y, Moon CM, Kim BC, Byeon JS. Endoscopic Resection of Cecal Polyps Involving the Appendiceal Orifice: A KASID Multicenter Study. Dig Dis Sci. 2017;62:3138-3148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Cignoli D, Fallara G, Aleotti F, Larcher A, Rosiello G, Rowe I, Basile G, Colandrea G, Martini A, De Cobelli F, Brembilla G, Lucianò R, Colecchia M, Lena MS, Partelli S, Tamburrino D, Zamboni G, Rubini C, Falconi M, Montorsi F, Salonia A, Capitanio U. Pancreatic metastases after surgery for renal cell carcinoma: survival and pathways of progression. World J Urol. 2022;40:2481-2488. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Ichkhanian Y, Barawi M, Seoud T, Thakkar S, Kothari TH, Halabi ME, Ullah A, Edris W, Aepli P, Kowalski T, Shinn B, Shariaha RZ, Mahadev S, Mosko JD, Andrisani G, Di Matteo FM, Albrecht H, Giap AQ, Tang SJ, Naga YM, van Geenen E, Friedland S, Tharian B, Irani S, Ross AS, Jamil LH, Lew D, Nett AS, Farha J, Runge TM, Jovani M, Khashab MA. Endoscopic full-thickness resection of polyps involving the appendiceal orifice: a multicenter international experience. Endoscopy. 2022;54:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 4. | Guo L, Ye L, Feng Y, Bethge J, Yang J, Schreiber S, Hu B. Endoscopic transcecal appendectomy: a new endotherapy for appendiceal orifice lesions. Endoscopy. 2022;54:585-590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Yuan XL, Cheung O, Du J, Ye LS, Hu B. Endoscopic transcecal appendectomy. Endoscopy. 2019;51:994-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |