Published online Jun 27, 2024. doi: 10.4240/wjgs.v16.i6.1939
Revised: April 28, 2024
Accepted: May 23, 2024
Published online: June 27, 2024
Processing time: 129 Days and 22.9 Hours
Colonoscopy is the most frequently used diagnostic and therapeutic tool for the treatment of colorectal diseases. Although the complication rate is low, it can be potentially serious. Intussusception is a rare and severe complication often associated with polypectomy. Only a handful of post-colonoscopy intussusception cases have been reported, making this study a valuable addition to the medical literature.
Case 1: A 61-year-old man underwent colonoscopy with polypectomy for chronic abdominal pain. The patient experienced abdominal pain 11 hours later but was still discharged after pain management. He was readmitted due to recurring pain. Computed tomography (CT) showed colo-colonic intussusception. Initial conservative management and attempts at endoscopic reduction failed; therefore, laparoscopic right hemicolectomy was performed. Histopathological examination revealed tubular adenomas in the polyps and inflammation in the resected specimens. Case 2: A 59-year-old woman underwent colonoscopy with poly
Post-colonoscopy intussusception in adults is rare, and polypectomy may contribute to its occurrence. Early diagnosis is crucial, with prompt CT exami
Core Tip: This study discusses two rare cases of colo-colonic intussusception as a complication of colonoscopy with polypectomy in adults. A 61-year-old man and 59-year-old woman developed intussusception after polyp removal during colonoscopy. Both patients underwent unsuccessful conservative and endoscopic reduction interventions, leading to surgical procedures. These findings highlight the importance of early detection using computed tomography and suggest that polypectomy may increase the risk of intussusception. Conservative management should be attempted before surgical resection, assuming that malignancy has been ruled out. This study highlights the importance of awareness and prompt management of this rare complication.
- Citation: Xiang SH, Xu GQ. Colo-colonic intussusception as a rare complication of colonoscopy with polypectomy: Two case reports. World J Gastrointest Surg 2024; 16(6): 1939-1947
- URL: https://www.wjgnet.com/1948-9366/full/v16/i6/1939.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i6.1939
Colonoscopy is the most frequently used diagnostic and therapeutic tool for colorectal diseases including colorectal tumors, inflammatory bowel disease, and lower gastrointestinal bleeding. The incidence of complications associated with colonoscopy is very low at < 1%[1]. Polypectomy performed during colonoscopy is generally considered safe. However, multiple colonoscopy-related complications may still occur, with the most common being gastrointestinal bleeding, perforation, and cardiopulmonary events, and over 85% of serious complications are reported in patients undergoing colonoscopy with polypectomy[1,2]. Intussusception after colonoscopy in adults is extremely rare and often associated with polypectomy. To the best of our knowledge, only 15 cases of post-colonoscopy intussusception have been reported since the first description by Yamazaki et al[3] in 2000.
To raise awareness and provide more information for better management of this unusual condition, we present two cases of intussusception after colonoscopy with polypectomy in adults, followed by a short review of the literature on this condition.
Case 1: A 61-year-old man experienced colicky abdominal pain in the right lower quadrant 11 hours after colonoscopy with polypectomy. Abdominal computed tomography (CT) revealed colo-colonic intussusception.
Case 2: A 59-year-old woman presented with upper abdominal pain and distention 9 hours after colonoscopy with polypectomy. Abdominal CT revealed a colo-colonic intussusception.
Case 1: The patient presented to our hospital with a 10-month history of abdominal pain in the lower right quadrant. Abdominal CT performed 1 month previously showed no positive findings, and colonoscopy performed 7 months previously showed multiple polyps. To further investigate the cause of abdominal pain and remove the polyps, we performed CT enterography (CTE), followed by colonoscopy and polypectomy. The CTE revealed no anomalies.
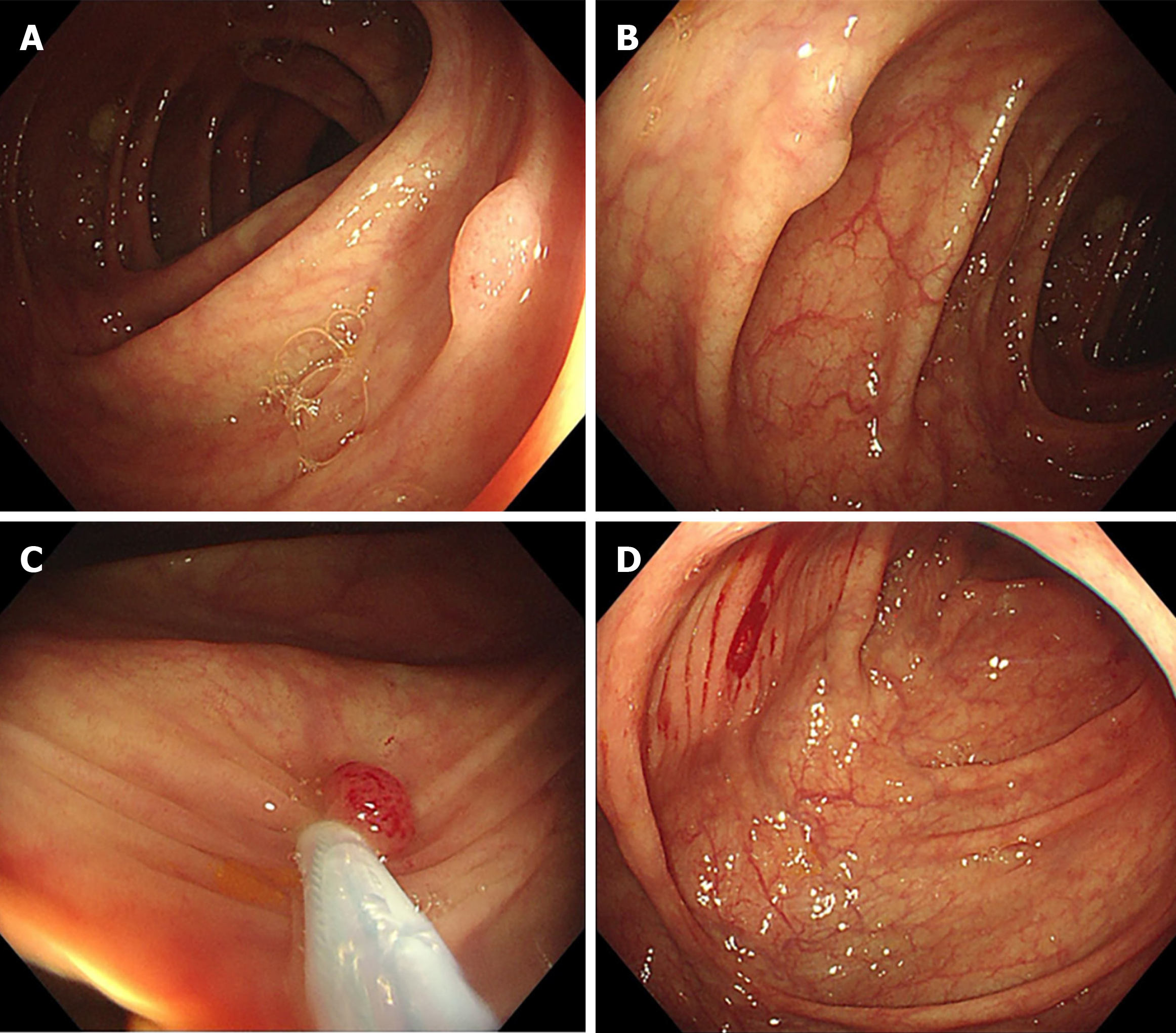
Colonoscopy was performed under intravenous anesthesia. The quality of bowel preparation was adequate, and no technical difficulties were encountered during colonoscopy. The colonoscopy took 25 minutes, including 11 minutes for intubation and 14 minutes for withdrawal. The terminal ileum was intubated. Three polyps in the sigmoid colon, sized 4-6 mm, were discovered during intubation and removed from the spot by cold snare polypectomy (CSP). Two polyps in the ascending colon near the hepatic flexure, sized 4-5 mm, were discovered during withdrawal and removed by CSP (Figure 1). No other abnormalities were found during colonoscopy. The patient regained consciousness approximately 6 minutes after the procedure and felt well without obvious abdominal discomfort.
Eleven hours later, the patient started to experience colicky abdominal pain in the right lower quadrant with tenderness, but no rebound tenderness. The patient rated the pain as 3 on a scale of 1–10. The pain lasted for 1 hour and was still not relieved; therefore, the doctor on duty administered 10 mg of anisodamine intramuscularly. The patient’s pain was relieved. However, only 4 hours later, the pain recurred without tenderness or rebound tenderness. The patient was administered a second intravenous dose of anisodamine (10 mg). The pain was relieved, and the patient was discharged 2 hours later. However, 8 hours after the patient was sent home, he returned to the emergency room because of recurring colicky abdominal pain in the right lower quadrant.
Case 2: The patient visited our hospital because a polyp was found in the transverse colon during routine colonoscopy three months prior to presentation.
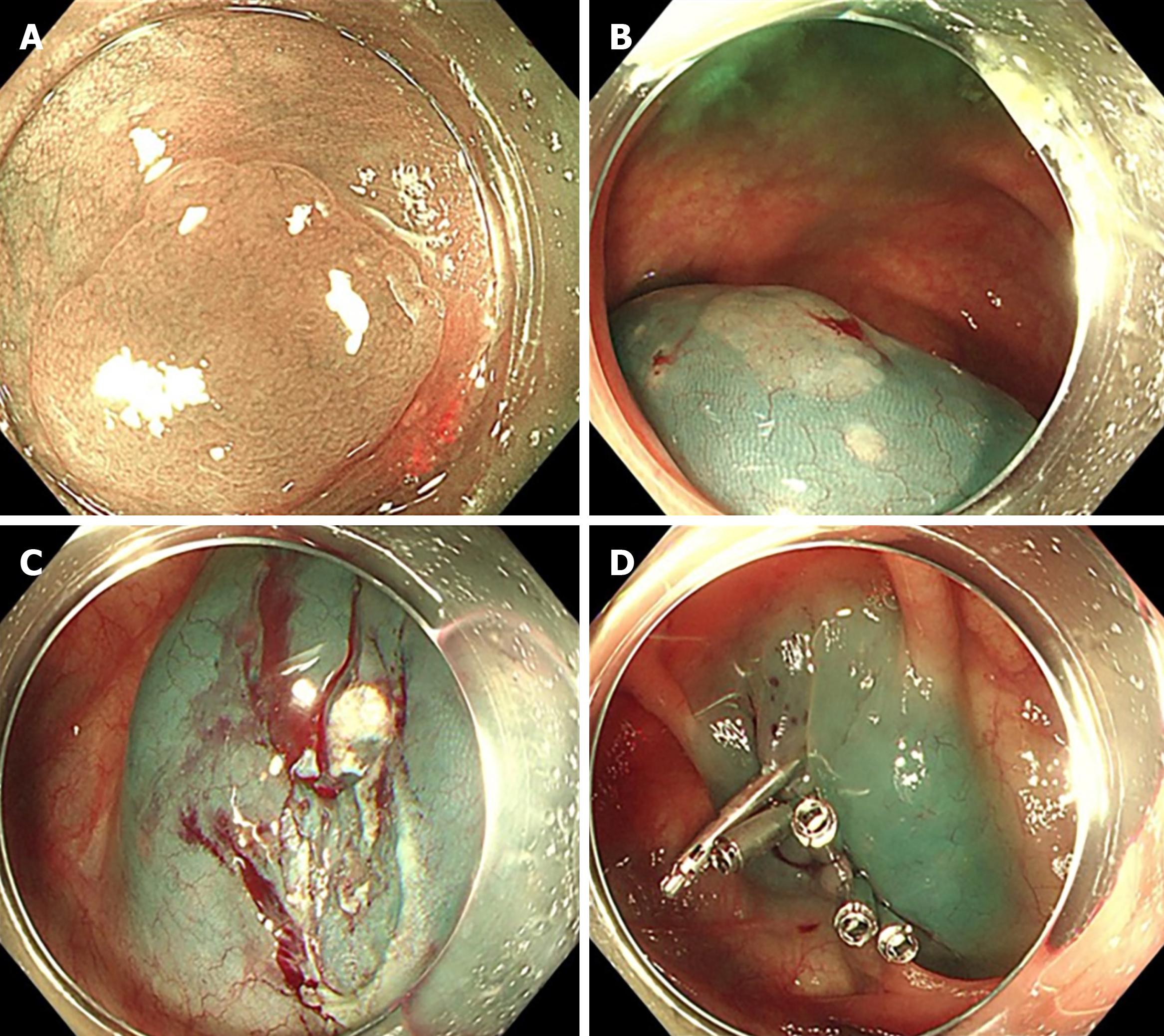
Colonoscopy and endoscopic polypectomy were performed under intravenous anesthesia. The quality of bowel preparation was adequate, and no technical difficulties were encountered during colonoscopy. The terminal ileum was not intubated. Colonoscopy took 36 minutes, including 10 minutes for intubation of the cecum and 26 minutes for withdrawal and polypectomy. A flat polyp measuring 12 mm in the transverse colon near the hepatic flexure was discovered and removed using endoscopic mucosal resection. The mucosal defect was closed using five metal clips (Figure 2). No other abnormalities were found during colonoscopy. Histopathological examination of the resected polyp revealed hyperplasia.
Nine hours after colonoscopy, the patient began to experience pain and distention in the upper abdomen. The pain worsened in the next 2 hours, and the patient rated it 7 on a scale of 1–10. A glycerin enema and antispasmodics (anisodamine and magnesium sulfate) were administered. The pain was briefly alleviated and then intensified again, accompanied by fever, nausea, and vomiting.
Case 1: Past medical history included chronic hepatitis B for 5 years and hepatocellular carcinoma surgery 4 years previously.
Case 2: The patient had a history of cesarean section surgery 30 years previously, and ectopic pregnancy surgery 22 years previously.
Both patients’ personal and family history was unremarkable.
Case 1: Upon returning to the emergency room, an abdominal physical examination revealed moderate tenderness with peritoneal signs in the right lower quadrant. The patient’s body temperature was 38 °C, heart rate 93 beats/minute (bpm), respiratory rate 20 breaths/minute, and blood pressure was 101/63 mmHg.
Case 2: Initially, the patient exhibited moderate upper abdominal tenderness. After the pain intensified and the patient became febrile, with accompanying nausea and vomiting, the vital signs were recorded as follows: Temperature, 38 °C; heart rate, 106 bpm; respiratory rate, 22 breaths/minute; and blood pressure, 169/91 mmHg. Further examination revealed tenderness and rebound tenderness of the upper abdomen.
Case 1: Laboratory examinations demonstrated an elevated white blood cell count of 14.9 × 109/L (normal 4.0-10.0 × 109/L), with a predominance of neutrophils (90.9%). The C-reactive protein level was normal (5.07 mg/L; normal 0-8 mg/L).
Case 2: Laboratory examinations demonstrated an elevated white blood cell count of 12.5 × 109/L (normal 4.0-10.0 × 109/L), with a predominance of neutrophils (77.9%). The C-reactive protein level was normal (1.21 mg/L; normal 0-8 mg/L) at that point and was found to be significantly elevated to 76.92 mg/L 13 hours later, while the complete blood cell count remained similar.
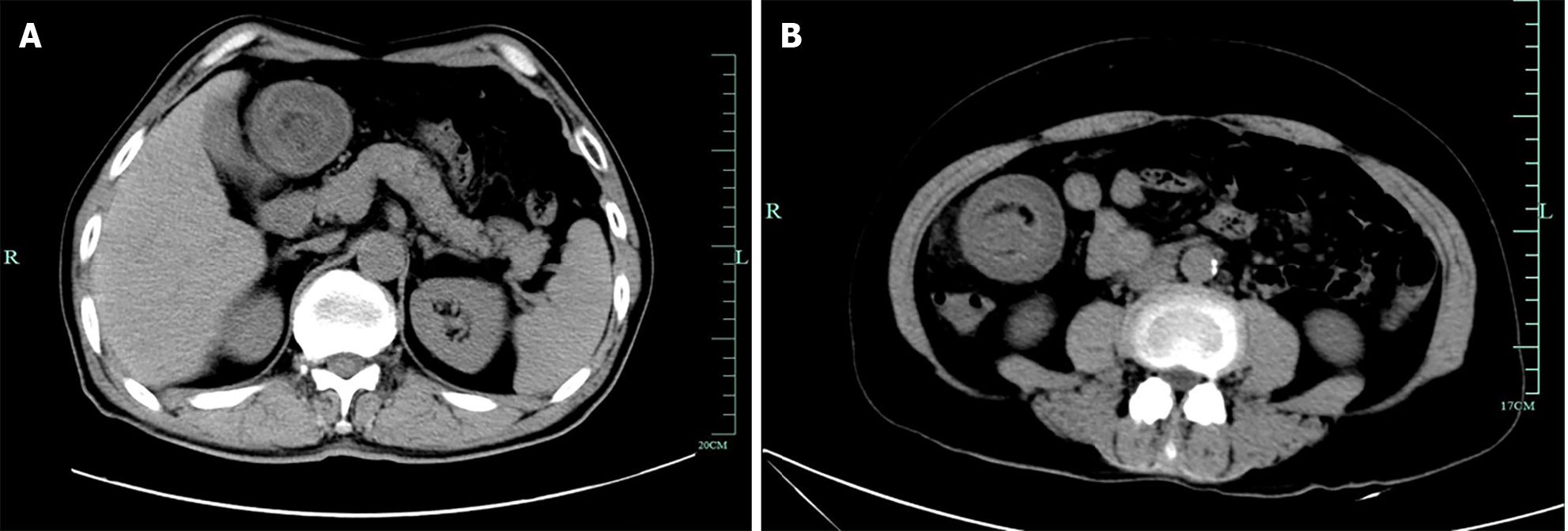
Case 1: Urgent abdominal CT revealed a colo-colonic intussusception near the hepatic flexure: The bowel near the hepatic flexure was dilated and the proximal colon was invaginated into it, which appeared as a target-like lesion (Figure 3A). There were no signs of bowel obstruction, perforation, or masses.
Case 2: Emergency abdominal CT revealed metal clips near the hepatic flexure and a target-like lesion with thickened intestinal walls in the distal colon near the clips, indicative of colo-colonic intussusception (Figure 3B).
Both patients were diagnosed with colo-colonic intussusception.
The patient was readmitted and initially managed conservatively with fasting and the maintenance of intravenous fluids, analgesics (pethidine), antispasmodics (anisodamine), antibiotics (meropenem), antipyretics (indomethacin), and parenteral nutrition. However, the abdominal pain persisted, and the patient passed approximately 20 mL of dark red bloody stool 4 hours after readmittance.
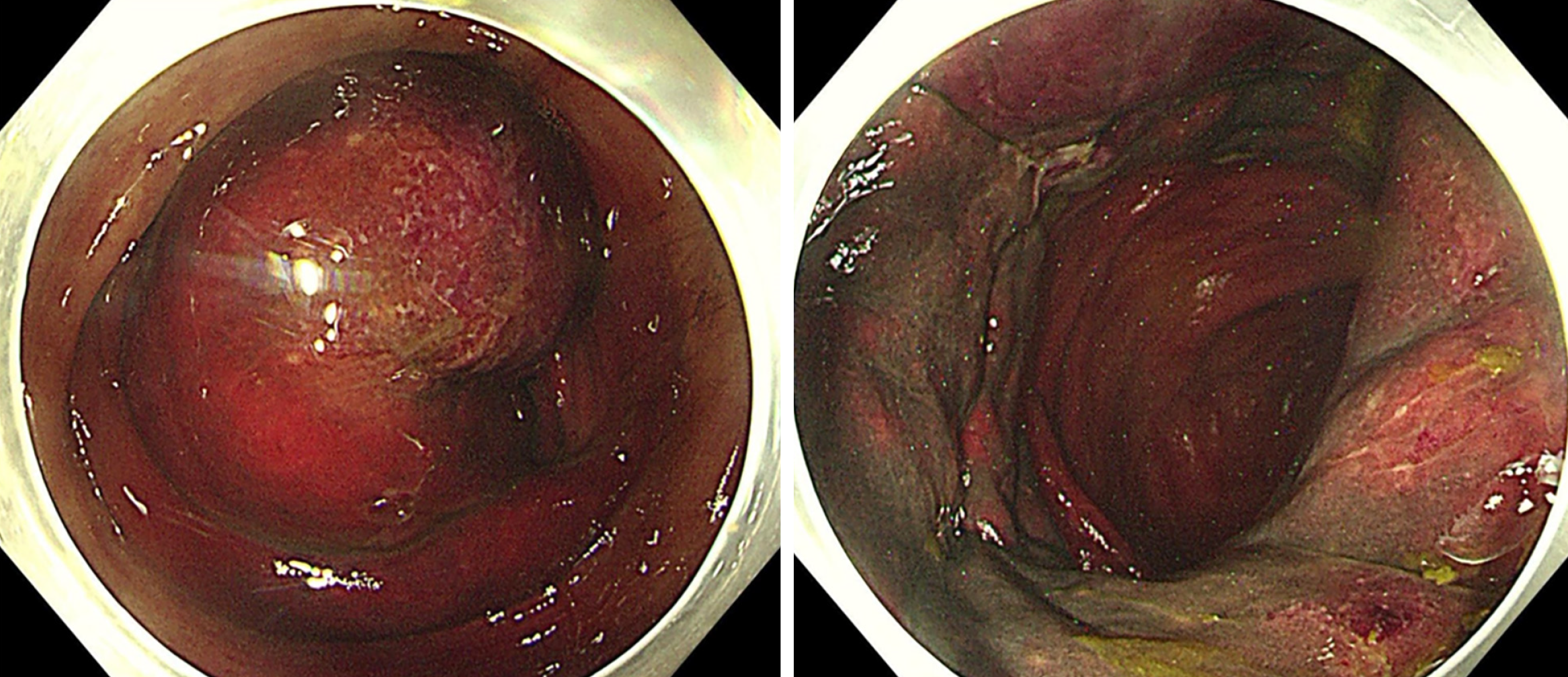
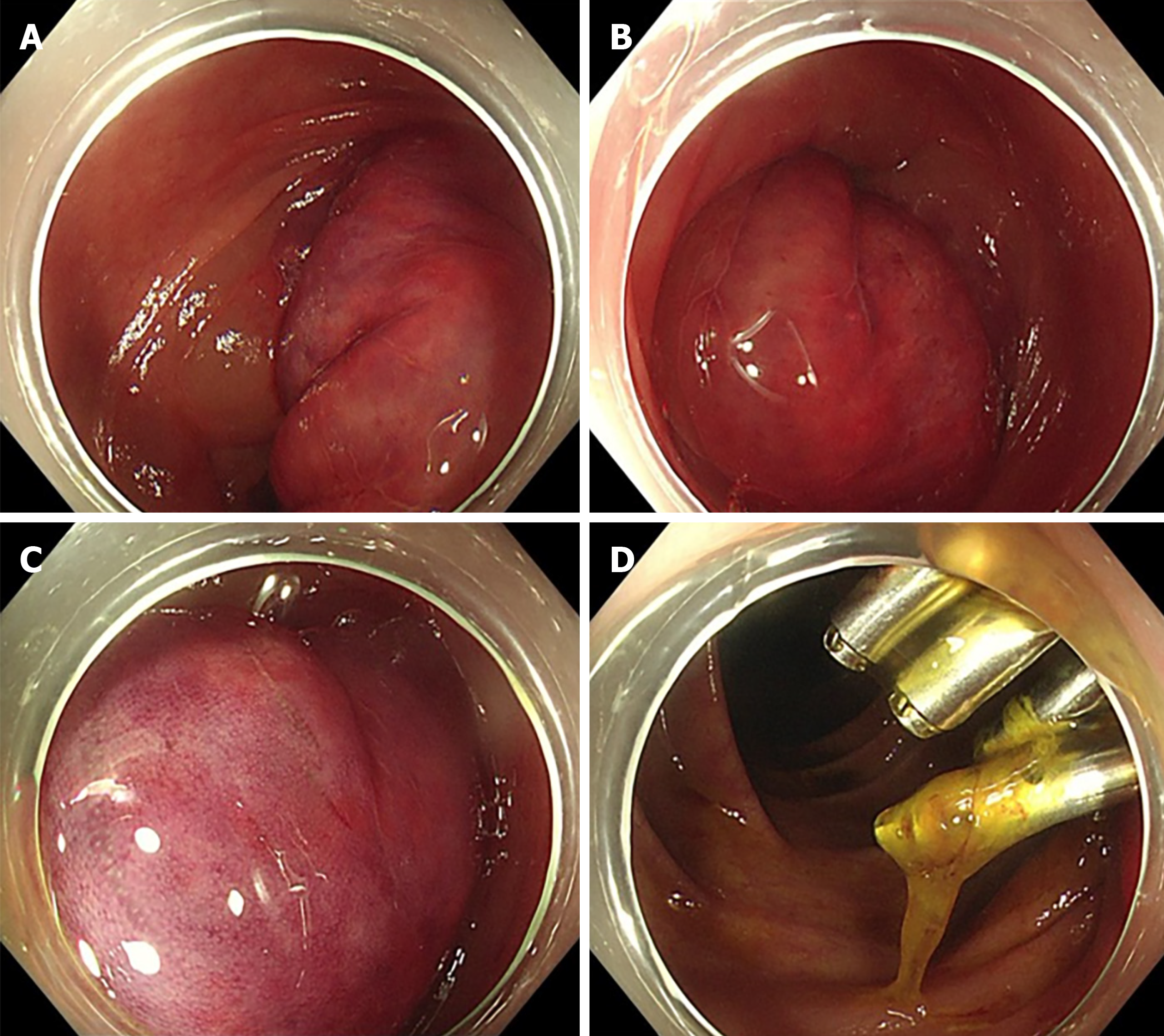
Emergency colonoscopy was performed to attempt endoscopic reduction. Colonoscopy revealed a congested, swollen, purple-red-colored mucosa in the ascending colon near the hepatic flexure invaginating the distal bowel (Figure 4). Repeated attempts to reduce the colo-colonic intussusception by pumping water and air failed.
The patient was then transferred to the operating room for laparoscopic surgery. Intraoperative findings included colo-colonic intussusception in the ascending colon near the hepatic flexure, with significant inflammation and exudation. Due to concerns about possible intestinal necrosis, a laparoscopic right hemicolectomy with intracorporeal anastomosis was performed.
Emergency colonoscopy was performed to reduce endoscopic intussusception. Colonoscopy revealed a congested, swollen, and purple-red-colored mucosa in the transverse colon that invaginated the distal bowel. The post-polypectomy wound with metal clips was located approximately 5 cm above the inflamed mucosa and was unaffected by intussusception (Figure 5). Repeated attempts to reduce colo-colonic intussusception by changing the position and pumping water and air failed.
Owing to the patient’s unwillingness to undergo surgery, conservative treatment was administered. However, the patient’s condition did not improve, and a repeat abdominal CT showed no signs of improvement. Twelve hours after the emergency colonoscopy, the patient was transferred to the operating room for laparoscopic surgery. The intraoperative findings included colo-colonic intussusception in the transverse colon near the hepatic flexure with edema and inflammation. The intussusception was laparoscopically reduced.
The patient’s postoperative recovery was uneventful, and was discharged 11 days later. No complications occurred.
Histopathological examination of the polyps resected during the initial endoscopy revealed tubular adenomas, whereas the specimen resected laparoscopically showed inflammatory changes with no evidence of malignancy or mass.
Postoperative recovery was uneventful, and the patient was discharged 8 days later. No complications occurred.
Both patients shared their perspective that complications are best avoided, and if unavoidable, successful conservative treatment is preferred over surgery; if surgery is necessary, reduction is preferred over resection.
Intussusception after a colonoscopy is exceedingly rare in adults. To date, only 17 cases, including our two cases, have been reported (Table 1)[3-17]. In these cases, the age of patients ranged from 19 to 73 years (average 47.6 years), and the sex ratio was roughly equal (8 males to 9 females). All patients experienced abdominal pain that occurred several hours after colonoscopy as the main clinical symptom, with tenderness as the main abdominal sign. Other less documented symptoms include fever, bloody stools, nausea, and vomiting. Laboratory examination results were documented in 12 cases, all showing elevated white blood cell counts ranging from 10.8 to 22 × 109/L (average 14.1 × 109/L). All diagnoses of intussusception were made by using abdominal CT. The majority (13 cases, 76.5%) were colo-colic intussusceptions, and only four cases (23.5%) were ileocolic. Almost all lesions occurred in the right colon, except in one case where it was located in the splenic flexure. Endoscopic interventions (biopsies or polypectomies) were performed during the initial colonoscopy in 14 (82.4%) of the 17 cases. Of the remaining three cases, one had a large polyp in the terminal ileum[7], which may serve as a potential cause, whereas the other two seemed normal. Regarding the treatments, four cases were successfully treated conservatively, four underwent laparoscopic reduction, one underwent successful endoscopic reduction, five underwent laparoscopic segmental bowel resection, and three underwent open segmental bowel resection. No malignant histopathological findings were observed.
| Ref. | Age (years)/sex | Endoscopic intervention | Type of intussusception | Treatment |
| Yamazaki et al[3], 2000 | 48/male | Biopsy | Cecal colo-colonic | Open resection |
| Theodoropoulou et al[4], 2009 | 19/male | No | Ileocecal | Open resection |
| Ho et al[5], 2010 | 32/male | Polypectomy | Cecal colo-colonic | Laparoscopic reduction |
| Nachnani et al[6], 2012 | 73/female | Biopsy | Ascending colo-colonic | Laparoscopic reduction |
| Lasithiotakis et al[7], 2012 | 58/male | No | Ileocecal | Open resection |
| Lee et al[8], 2013 | 47/male | Polypectomy | Cecal colo-colonic | Laparoscopic resection |
| Min et al[9], 2017 | 31/female | Biopsy | Cecal colo-colonic | Laparoscopic resection |
| Araki et al[10], 2018 | 28/male | Polypectomy | Cecal colo-colonic | Endoscopic reduction |
| Hassan et al[11], 2018 | 43/female | Biopsy | Ascending colo-colonic | Conservative management |
| He et al[12], 2020 | 54/female | Polypectomy and biopsy | Transverse colo-colonic | Conservative management |
| Ahmed et al[13], 2020 | 42/female | Polypectomy and biopsy | Transverse colo-colonic | Conservative management |
| Moon et al[14], 2022 | 58/female | Polypectomy | Hepatic flexure colo-colonic | Conservative management |
| Lee et al[15], 2022 | 69/male | Polypectomy | Ileocecal | Laparoscopic resection |
| Vadakkenchery et al[16], 2022 | 36/female | No | Splenic flexure colo-colonic | Laparoscopic reduction |
| Jastaniah et al[17], 2023 | 51/female | Polypectomy | Ileocecal | Laparoscopic resection |
| Current case 1 | 61/male | Polypectomy | Ascending colo-colonic | Laparoscopic resection |
| Current case 2 | 59/female | Polypectomy | Transverse colo-colonic | Laparoscopic reduction |
Intestinal intussusception mostly occurs in the small intestine, with only 20% of cases involving solely the large bowel[18]. Less than 5% of intussusceptions occur in adults[19]. Intussusception in adults is usually related to definable causes, with only 10%-20% of all cases being idiopathic[20]. Common causes of adult colonic intussusception include adherence, inflammatory lesions, polyps, and benign or malignant tumors[19]. The most prevalent cause is a pathological lead point in the bowel, which is malignant in half of the cases[17]. However, these causes are not usually present in post-colonoscopy intussusception.
The etiology of intussusception after colonoscopy remains unclear. Several hypotheses have been proposed to explain the phenomenon. Some scholars have suggested that edema or hematoma caused by endoscopic interventions, including biopsy and polypectomy, may serve as a lead point[14,15,17]. The metal clips used after polypectomy may also act as a lead point. This may explain the occurrence of intussusception in our first case, as the location of intussusception observed during emergent colonoscopy was consistent with the site of the prior polypectomy. As mentioned previously, biopsies or polypectomies were performed during the initial colonoscopy in 14 (82.4%) of the 17 cases. However, in our second case, the post-polypectomy wound with metal clips was located approximately 5 cm above the inflamed mucosa and was not affected by intussusception, which implies that the post-polypectomy wound and metal clips were not the lead points. Additionally, no endoscopic interventions were applied in two of the previously reported cases. This finding implies the involvement of other mechanisms. Yamazaki et al[3] speculated that the intussusception was induced by hyperperistalsis, which vents gas and empties the insufflated colon after colonoscopy[3]. Hassan et al[11] proposed that gas aspiration during colonoscope withdrawal creates a vacuum effect, leading to the collapse and invagination of the proximal colon into the distal colon, which is primarily observed in the right colon because of the mobility and freedom of movement of the cecum within the abdomen[11]. In addition, a history of abdominal surgery may predispose patients to intussusception[9]. Both of our patients underwent abdominal surgery. Another hypothesis suggests that complex bowel loops may form during colonoscopy, potentially leading to transient intussusception[6].
Because its etiology is unclear, it is challenging to determine effective preventive measures. We speculate that measures such as avoiding excessive insufflation during colonoscopy, gentle suction maneuvers, and administration of antispasmodic drugs, such as anisodamine, when hyperperistalsis is observed may potentially reduce the incidence of post-colonoscopy intussusception.
Compared to prevention, early diagnosis may be more practical. Early diagnosis of intussusception improves the prognosis. Prompt CT examination is the key to early diagnosis. In our two cases, the severity of the situation was not initially recognized, resulting in delays in performing abdominal CT scans and instead administering pain management, which led to a delayed diagnosis of intussusception. In our first case, laparoscopic resection was performed instead of reduction because of the potential ischemic necrosis, which could have been avoided if the intussusception had been identified earlier. This served as an important cautionary measure. If abdominal pain accompanied by tenderness occurs within hours to days after colonoscopy, particularly after a polypectomy, abdominal CT should be performed promptly. Additional manifestations, including elevated white blood cell count, fever, and bloody stools, further indicate the need for urgent CT evaluation.
Traditionally, laparoscopic or open bowel resection has been the standard approach for treating bowel intussusception in adults to allow the examination of specimens for any potential malignancy[18,19]. However, in cases of post-colonoscopy intussusception in which the colon has already been examined and malignancy has been ruled out, we believe that conservative management should be considered prior to surgery. If surgical treatment is necessary, after the exclusion of bowel ischemic necrosis or perforation, reduction should be prioritized over resection. Multiple reports have suggested that intussusceptions with a short-affected segment and no lead-point mass can be managed using a 'wait and see' strategy with regular clinical and imaging evaluations to monitor spontaneous resolution[19]. Endoscopic reduction is seldom performed to treat adult intussusception[19,20]. Only 1 of the 17 patients underwent successful endoscopic reduction, whereas this failed in our two cases. We look forward to the future development of endoscopic reduction techniques with high efficacy, which would be the ideal treatment approach for post-colonoscopy intussusception.
This study has several limitations. First, there have been multiple reports on this condition prior to our report. Second, images obtained during surgery were not preserved. Third, we were unable to identify the exact etiology in the two cases. Finally, we failed to provide preventive measures with definite efficacy. Nevertheless, our report of the two cases provides more detailed information, including details of the initial colonoscopies, abundant original images, and the entire process of disease development, diagnosis, and treatment. This study adds to our knowledge of this rare condition and emphasizes the importance of early recognition. Patient perspectives were also reported in our study. Additionally, we conducted a short review of previous reports on this entity.
Intussusception after colonoscopy is rare in adults. The etiology of this condition remains unclear. An edema or hematoma caused by a biopsy or polypectomy may serve as the lead point. No preventive measures have been established. Early diagnosis plays a crucial role in the management of this condition, and prompt CT examination is crucial for early diagnosis. If malignancy is ruled out by the initial colonoscopy, conservative management should be considered before surgery. If surgery is necessary, reduction should be prioritized over resection after excluding bowel ischemic necrosis or perforation.
We extend our heartfelt gratitude to the patients and their families for their cooperation throughout the processes of data collection, treatment, and subsequent follow-up.
| 1. | Fisher DA, Maple JT, Ben-Menachem T, Cash BD, Decker GA, Early DS, Evans JA, Fanelli RD, Fukami N, Hwang JH, Jain R, Jue TL, Khan KM, Malpas PM, Sharaf RN, Shergill AK, Dominitz JA; ASGE Standards of Practice Committee. Complications of colonoscopy. Gastrointest Endosc. 2011;74:745-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 229] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 2. | Church J. Complications of colonoscopy. Gastroenterol Clin North Am. 2013;42:639-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Yamazaki T, Okamoto H, Suda T, Sakai Y, Hatakeyama K, Hokari I, Toyoda S, Souma T. Intussusception in an adult after colonoscopy. Gastrointest Endosc. 2000;51:356-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Theodoropoulou A, Konstantinidis K, Kteniadakis S, Tribonias G, Tzanoudakis G, Vardas E, Karmiris K, Psillakis K, Zois E, Tzortzakakis E, Paspatis GA. Intussusception following enteroscopy and ileo-colonoscopy in an adult with acquired immune deficiency syndrome. Endoscopy. 2009;41 Suppl 2:E162-E163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Ho MM, Park JJ, Prasad LM. Post Colonoscopy Colonic Intussusception Reduced via a Laparoscopic Approach. JSLS. 2010;14:596-599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Nachnani J, Burns E, Margolin D, Clarkston WK. Colocolonic intussusception after colonoscopy. Gastrointest Endosc. 2012;75:223-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Lasithiotakis K, Grisbolaki E, Filis D, Athanasakis I, Zoras O, Chalkiadakis G. Ileocolic intussusception precipitated by diagnostic colonoscopy: a case report. Surg Laparosc Endosc Percutan Tech. 2012;22:e161-e163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Lee CK, Shim JJ, Jang JY. Ceco-colic intussusception with subsequent bowel infarction as a rare complication of colonoscopic polypectomy. Endoscopy. 2013;45 Suppl 2 UCTN:E106-E107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Min MX, Sklow B, Vaughn BP. Intussusception after Routine Colonoscopy: A Rare Complication. ACG Case Rep J. 2017;4:e63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Araki O, Fukuda A, Kusaka T, Seno H. A case of cecocolonic intussusception after endoscopic submucosal dissection of a cecal adenoma. Gastrointest Endosc. 2018;87:1589-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Hassan WAW, Teoh W. Intussusception after Colonoscopy: A Case Report and Review of Literature. Clin Endosc. 2018;51:591-595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | He H, Rambhujun V, DeMaria M, Ali M, Vrabie R. Early Postendoscopic Transverse Colo-Colonic Intussusception. Case Rep Gastroenterol. 2020;14:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 13. | Ahmed A, Zhang J, Anas K. Intussusception in a Routine Colonoscopy. ACG Case Rep J. 2020;7:e00422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Moon JY, Lee MR, Yim SK, Ha GW. Colo-colonic intussusception with post-polypectomy electrocoagulation syndrome: A case report. World J Clin Cases. 2022;10:8939-8944. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Lee GH, Noh CK. Ileocolonic Intussusception Due to Hematoma After Snare Polypectomy. Am J Gastroenterol. 2022;117:1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Vadakkenchery Varghese E, Steen C, Juszczyk K, An V. Splenic flexure intussusception: a rare complication post colonoscopy. ANZ J Surg. 2022;92:1545-1546. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Jastaniah A, AlBusaidi N, Bandegi P, Grushka J. Intussusception after colonoscopic polypectomy: a rare complication. BMJ Case Rep. 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Hong KD, Kim J, Ji W, Wexner SD. Adult intussusception: a systematic review and meta-analysis. Tech Coloproctol. 2019;23:315-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 19. | Panzera F, Di Venere B, Rizzi M, Biscaglia A, Praticò CA, Nasti G, Mardighian A, Nunes TF, Inchingolo R. Bowel intussusception in adult: Prevalence, diagnostic tools and therapy. World J Methodol. 2021;11:81-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (4)] |
| 20. | Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal Intussusception: Etiology, Diagnosis, and Treatment. Clin Colon Rectal Surg. 2017;30:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 190] [Article Influence: 21.1] [Reference Citation Analysis (0)] |