Published online Jun 27, 2024. doi: 10.4240/wjgs.v16.i6.1933
Revised: March 7, 2024
Accepted: May 24, 2024
Published online: June 27, 2024
Processing time: 145 Days and 17.5 Hours
The combination of magnetic compression anastomosis (MCA) and endoscopy has been used to treat biliary stricture after liver transplantation. However, its use for the treatment of complex biliary obstruction after major abdominal trauma has not been reported. This case report describes the successful use of MCA for the treatment of biliary obstruction resulting from major abdominal trauma.
A 23-year-old man underwent major abdominal surgery (repair of liver rupture, right half colon resection, and ileostomy) following a car accident one year ago. The abdominal drainage tube, positioned at the Winslow foramen, was draining approximately 600-800 mL of bile per day. During the two endoscopic retrograde cholangiopancreatography procedures, the guide wire was unable to enter the common bile duct, which prevented placement of a biliary stent. MCA combined with endoscopy was used to successfully achieve magnetic anastomosis of the peritoneal sinus tract and duodenum, and then a choledochoduodenal stent was placed. Finally, the external biliary drainage tube was removed. The patient achieved internal biliary drainage leading to the removal of the external biliary drainage tube, which improved the quality of life.
Magnetic compression technique can be used for the treatment of complex biliary obstruction with minimal operative trauma.
Core Tip: In cases of severe biliary stenosis or occlusion, performing endoscopic balloon dilation or biliary stent implantation via endoscopic retrograde cholangiopancreatography is sometimes not possible. There are some research reports on the use of magnetic compression anastomosis (MCA) to treat biliary stricture or occlusion. However, the use of MCA in the treatment of complex biliary obstruction after abdominal trauma has not been reported. This study reports the successful treatment of a patient with complex biliary obstruction after abdominal trauma with MCA.
- Citation: Zhang MM, Tao J, Sha HC, Li Y, Song XG, Muensterer OJ, Dong FF, Zhang L, Lyu Y, Yan XP. Magnetic compression anastomosis to restore biliary tract continuity after obstruction following major abdominal trauma: A case report. World J Gastrointest Surg 2024; 16(6): 1933-1938
- URL: https://www.wjgnet.com/1948-9366/full/v16/i6/1933.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i6.1933
Benign biliary strictures are a common occurrence following biliary surgery or liver transplantation[1-3]. These strictures can typically be treated with endoscopic balloon dilation and biliary stent implantation[4,5]. However, in cases with severe stenosis or occlusion, endoscopic retrograde cholangiopancreatography (ERCP) treatment may not be successful[6]. Percutaneous transhepatic biliary drainage is currently the only non-surgical treatment option available for these patients. However, long-term biliary drainage adversely affects the quality of life of these patients. Magnetic compression anastomosis (MCA) has recently emerged as a potential treatment option for severe benign biliary strictures[7-10]. In this report, we present a successful case of abdominal sinus and duodenal MCA in a patient with severe biliary tract injury following abdominal trauma.
One year after undergoing surgery for abdominal trauma, the bile was draining externally for 7 months.
A 23-year-old man underwent surgery for repair of liver rupture, right half colon resection, and ileostomy following a car accident one year ago. Postoperatively, he developed a complex abdominal infection, biliary leakage, abdominal wall incision infection, and intestinal fistula. Following conservative treatment, which included anti-infection measures, nutritional support, and abdominal drainage, his condition remained stable. Seven months later, the abdominal drainage tube, positioned at the Winslow foramen, was draining approximately 600-800 mL of bile per day. A contrast agent was injected via the abdominal drainage tube to visualize the middle and upper segments of the common bile duct, hepatic duct, and intrahepatic bile duct. However, the lower segments of the common bile duct were not visualized. During the two ERCP procedures, the guide wire was unable to enter the common bile duct, which prevented the placement of the biliary stent. For further treatment, the patient was admitted to the Magnetic Surgery Clinic of the First Affiliated Hospital of Xi’an Jiaotong University.
The past medical history was unremarkable.
There was no relevant family history.
The patient's vital signs were stable. Physical examination showed no cardiorespiratory abnormalities. Abdominal examination revealed an old surgical incision scar and a partial abdominal wall defect. An abdominal tube draining brown bile was seen on the right side of the abdomen. The descending ileostomy was visible in the right lower abdomen. The abdomen was flat and soft, with no abdominal tenderness. There was no shifting dullness, and bowel sounds were normal.
Abnormal laboratory parameters included: serum alanine aminotransferase 205 U/L; aspartate aminotransferase 108 U/L; alkaline phosphatase 511 U/L; gamma glutamyl transferase 452 U/L; albumin 34.3 g/L; total bilirubin 91.3 µmol/L; direct bilirubin 70.4 µmol/L; indirect bilirubin 20.9 µmol/L.
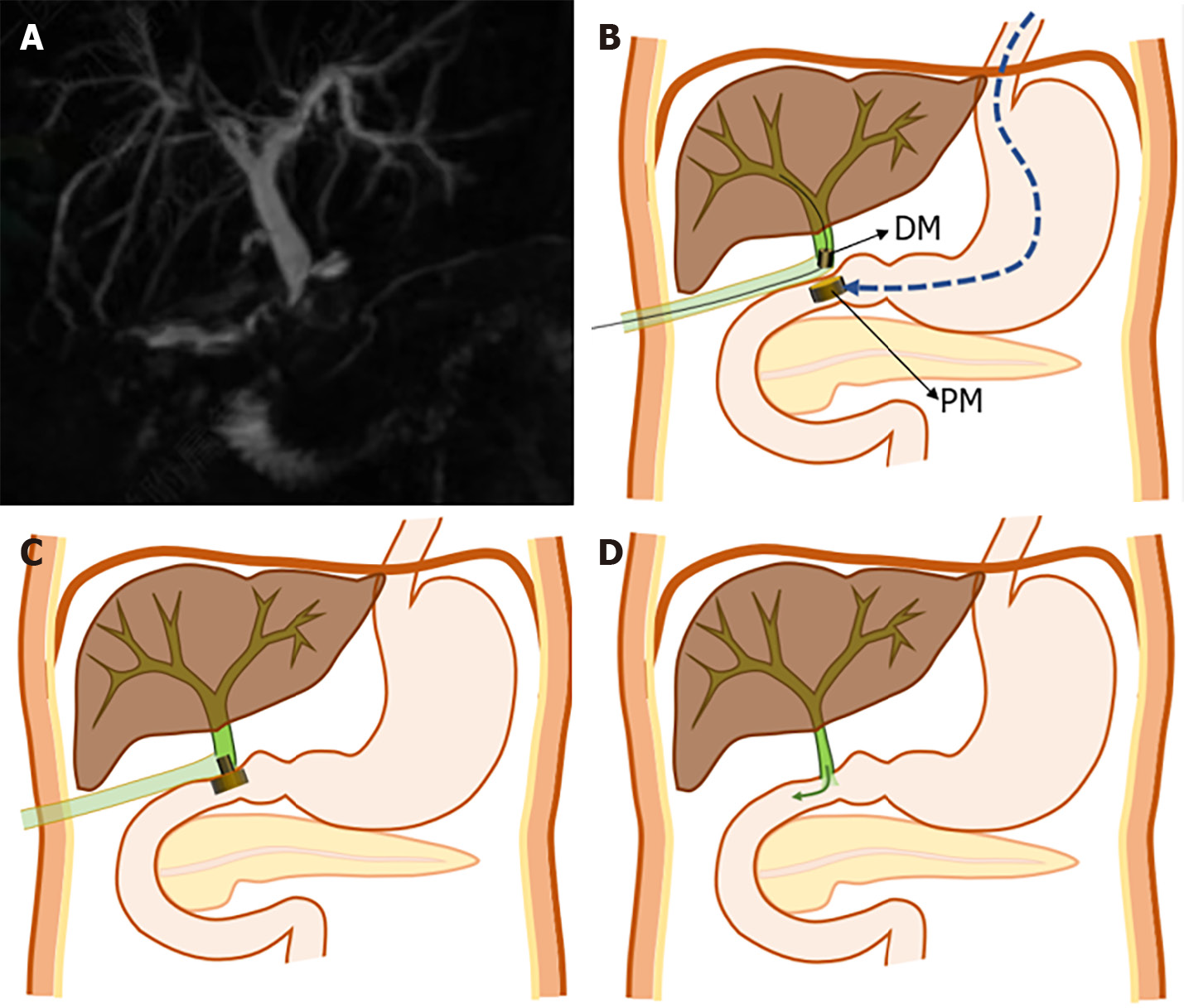
Magnetic resonance cholangiopancreatography revealed dilation of both the intrahepatic and extrahepatic bile ducts, with an unclear structure of the lower segment of the common bile duct (Figure 1A).
The final diagnosis was: Biliary obstruction, biliary fistula, ileostomy status, and right hemicolectomy status.
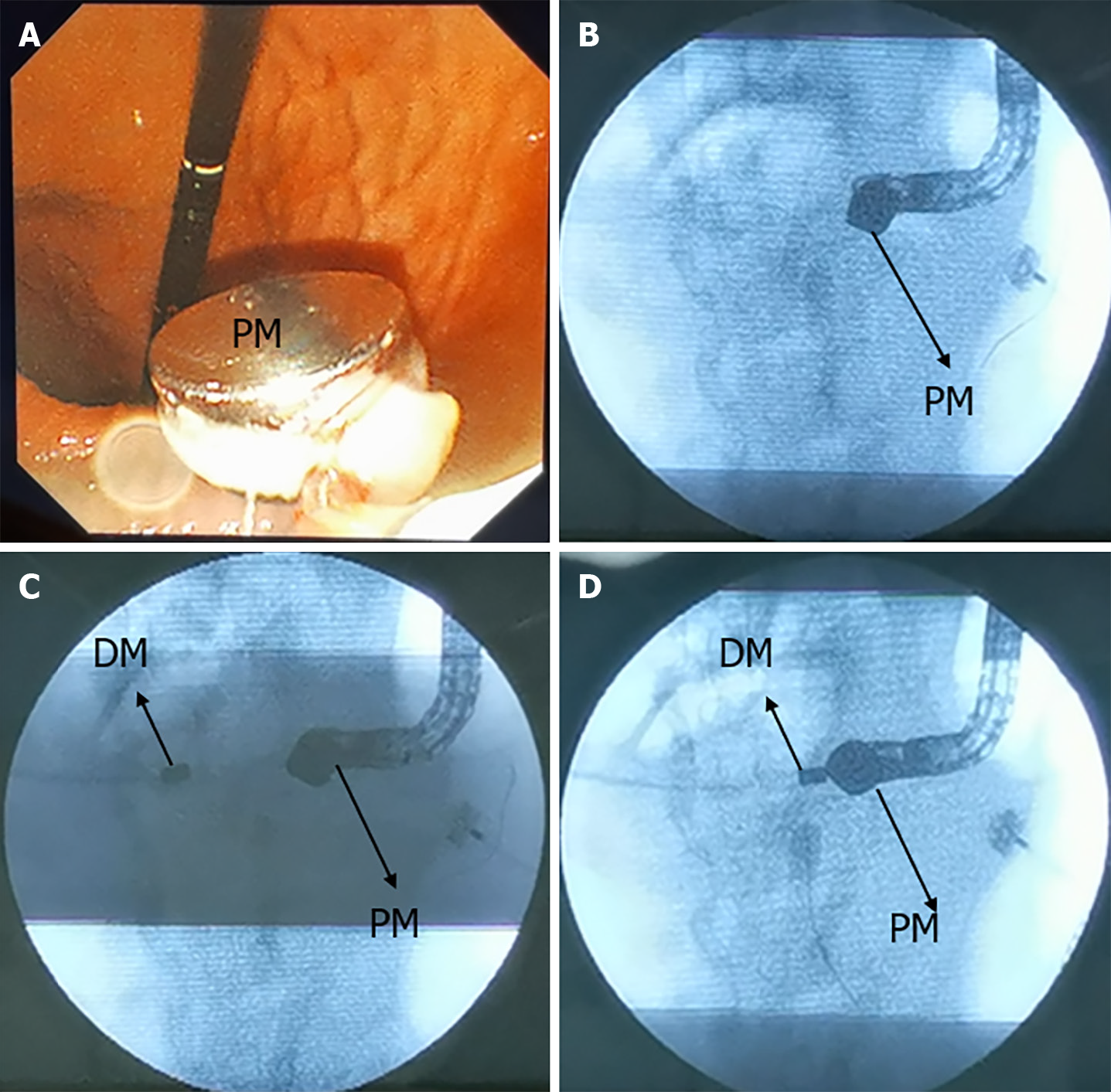
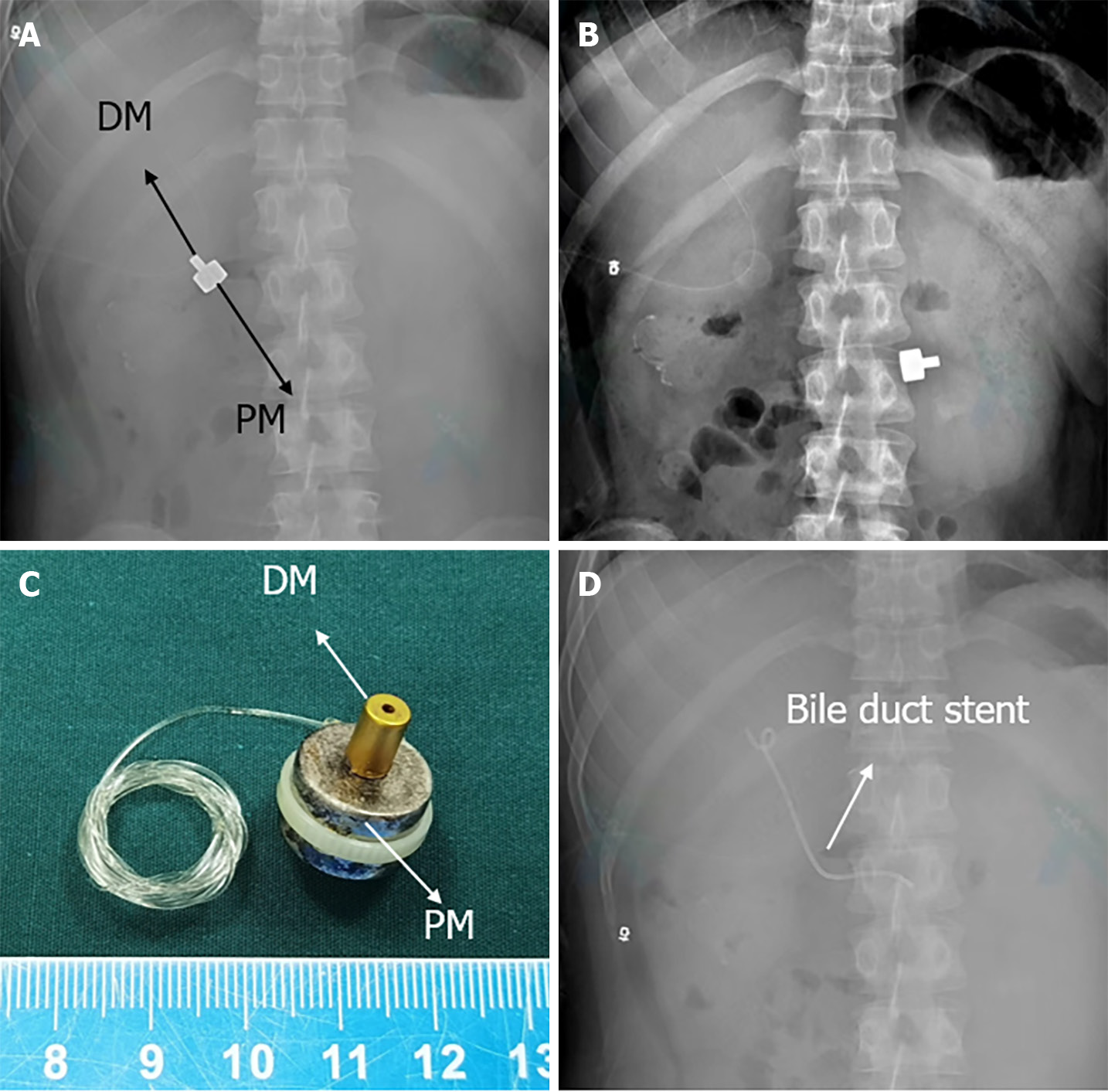
After the patient declined further abdominal surgery, a MCA was scheduled upon obtaining his informed consent. The surgical plan for the abdominal sinus-duodenal MCA is illustrated in Figure 1B-D. The parent magnet (PM) and daughter magnet (DM) were designed by the authors (Yan XP and Zhang MM) and manufactured by Jinshan Electronic Appliances Ltd. (Xi’an, China). The magnetic force test showed that the magnetic force of the DM and the PM at zero distance is 7.57 N, and the magnetic force at 5 mm is 2.81 N. The PM was guided into the duodenum using a gastroscope while being monitored by X-ray (Figure 2A and B). The DM was then inserted into the lower part of the common bile duct through the abdominal sinus (Figure 2C). The daughter magnet and parent magnet were observed to be in close apposition due to magnetism (Figures 2D and 3A). Subsequently, an indwelling external biliary drainage tube was placed via the abdominal sinus. Three days after the operation, the parent and daughter magnets were discharged from the body through the ileostomy (Figure 3B and C). Subsequently, a choledochoduodenal stent was inserted through the magnetic anastomosis channel during an ERCP procedure (Figure 3D). The external biliary drainage tube was removed after three days, and internal biliary drainage was established.
The patient's bilirubin level returned to normal after two weeks, and the serum transaminase level returned to normal after one month. The biliary stent was replaced after three months and was finally removed after 6 months. As of 18-month follow-up, the patient is in a good condition with normal liver function.
Several reports have documented the use of MCA in conjunction with ERCP for treating severe benign biliary strictures[6-8]. The magnet placement process is easier when the guide wire can pass through the stenosis. However, the surgical approach becomes more complicated when the guide wire cannot pass through the stenosis. In contrast to previously reported cases, this special case was highly complex due to the absence of the lower biliary duct structure. The patient’s only means of clearing bile was through the abdominal sinus. In this case, we used MCA to create a new channel between the abdominal sinus and duodenum instead of abdominal drainage. The establishment of this channel is facilitated using magnetic compression anastomosis, and its unique features. The patient's abdominal drainage tube was removed to allow for internal bile drainage. Follow-up assessments indicated that the patient’s overall condition was stable. To the best of our knowledge, MCA between the abdominal sinus and the duodenum has not been reported. The development of flexible magnet designs and placement methods has enabled the successful use of the MCA technique for the treatment of some complex digestive tract stenosis[11].
The successful outcome of MCA in the treatment of biliary stenosis in this patient shows the benefits of the technique. Our experience may serve as a valuable reference for treating patients with complex biliary obstruction in the future.
| 1. | Mascarenhas A, Marques HP, Coutinho J, Martins A, Nolasco F. Liver cirrhosis requiring transplantation in the context of hepaticojejunostomy stricture after a traumatic bile duct injury. Radiol Case Rep. 2024;19:835-838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Yan Q, Liu Y, Deng FW, Wang FJ, Chen HW. Effects of Preservation of Donor Liver Gastroduodenal Artery on Post-Transplant Biliary Complications in 187 Liver Transplant Recipients: A Retrospective Study. Ann Transplant. 2023;28:e941699. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Ly M, Lau NS, McKenzie C, Kench JG, Seyfi D, Majumdar A, Liu K, McCaughan G, Crawford M, Pulitano C. Histological Assessment of the Bile Duct before Liver Transplantation: Does the Bile Duct Injury Score Predict Biliary Strictures? J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Bofill A, Cárdenas A. A practical approach to the endoscopic management of biliary strictures after liver transplantation. Ann Hepatol. 2024;29:101186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Colombo M, Forcignanò E, Da Rio L, Spadaccini M, Andreozzi M, Giacchetto CM, Carrara S, Maselli R, Galtieri PA, Pellegatta G, Capogreco A, Massimi D, Khalaf K, Hassan C, Anderloni A, Repici A, Fugazza A. Endoscopic management of benign biliary strictures: Looking for the best stent to place. World J Clin Cases. 2023;11:7521-7529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 6. | Tan N, Lubel J, Kemp W, Roberts S, Majeed A. Current Therapeutics in Primary Sclerosing Cholangitis. J Clin Transl Hepatol. 2023;11:1267-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Do MY, Jang SI, Cho JH, Joo SM, Lee DK. Magnetic compression anastomosis for treatment of biliary stricture after cholecystectomy. VideoGIE. 2022;7:253-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Ödemiş B, Başpınar B, Tola M, Torun S. Magnetic Compression Anastomosis Is a Good Treatment Option for Patients with Completely Obstructed Benign Biliary Strictures: A Case Series Study. Dig Dis Sci. 2022;67:4906-4918. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Jang SI, Cho JH, Lee DK. Magnetic Compression Anastomosis for the Treatment of Post-Transplant Biliary Stricture. Clin Endosc. 2020;53:266-275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Nakaseko Y, Shiba H, Yamanouchi E, Takano Y, Sakamoto T, Imazu H, Ashida H, Yanaga K. Successful Treatment of Stricture of Duct-to-Duct Biliary Anastomosis After Living-Donor Liver Transplantation of the Left Lobe: A Case Report. Transplant Proc. 2017;49:1644-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Zhang M, He S, Sha H, Xue H, Lv Y, Yan X. A novel self-shaping magnetic compression anastomosis ring for treatment of colonic stenosis. Endoscopy. 2023;55:E1132-E1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (1)] |