Published online Jun 27, 2024. doi: 10.4240/wjgs.v16.i6.1726
Revised: April 29, 2024
Accepted: May 17, 2024
Published online: June 27, 2024
Processing time: 112 Days and 20.1 Hours
Endoscopic retrograde cholangiopancreatography (ERCP), with its clinical ad-vantages of less trauma and faster recovery, has become the primary treatment for choledocholithiasis.
To investigate the effects of different ERCP procedures on the sphincter of Oddi.
The clinical data of 91 patients who underwent ERCP at Yixing Hospital of Traditional Chinese Medicine between February 2018 and February 2021 were analyzed retrospectively. The patients were divided into endoscopic sphincterotomy (EST, n = 24) and endoscopic papillary balloon dilation (EPBD, n = 67) groups. The duration of operation, pancreatic development, pancreatic sphincterotomy, intubation difficulties, stone recurrence, and incidence of reflux cho
Differences in hypertension, diabetes, increased bilirubin, small diameter of the common bile duct, or ampullary diverticulum between the two groups were not significant. Statistically significant differences were observed between the two groups concerning sex and age (< 60 years). Patients with a history of choledocholithiasis, pancreatitis, and Oddi sphincter dysfunction were higher in the EST group than in the EPBD group. The number of cases of pancreatic development, pancreatic duct sphincterotomy, and difficult intubation were higher in the EST group than in the EPBD group. The number of Oddi’s sphincter manometries, ERCP surgical outcomes, and guidewires entering the pancreatic duct several times in EST group were lower than those in the EPBD group. The numbers of stone recurrences, reflux cholangitis, and cholecystitis were higher in the EST group than in the EPBD group.
In summary, common bile duct stones, pancreatitis history, and multiple guided wire introductions into the pancreatic duct are independent risk factors for EST and EPBD. Based on this evidence, this study can provide actionable insights for clinicians and researchers.
Core Tip: This study suggests that the number of cases of pancreatic development, sphincterotomy of pancreatic duct, difficulty intubation, recurrence of calculus, reflux cholangitis and cholecystitis in endoscopic sphincterotomy (EST) group were higher than those in endoscopic papillary balloon dilation (EPBD) group. Moreover, choledocholithiasis, history of pancreatitis, and multiple guides leads into the pancreatic duct are independent risk factors for EST and EPBD. Clinical re-identification of Oddi sphincter function will ensure rational and standardized patient treatment.
- Citation: Fu K, Yang YY, Chen H, Zhang GX, Wang Y, Yin Z. Effect of endoscopic sphincterotomy and endoscopic papillary balloon dilation endoscopic retrograde cholangiopancreatographies on the sphincter of Oddi. World J Gastrointest Surg 2024; 16(6): 1726-1733
- URL: https://www.wjgnet.com/1948-9366/full/v16/i6/1726.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i6.1726
Choledocholithiasis is a common and frequently occurring disease worldwide, accounting for a substantial proportion of digestive system diseases[1,2]. It affects more than 10% of the Western population[3]. In addition to genetic factors, age, sex, nutrition, obesity, rapid weight change, and exercise are closely related to the development of choledocholithiasis[3]. With a rapidly developing economy and consequently improving living standards in China[4], the choledocholithiasis incidence in China is rising yearly owing to increasingly severe population aging and obesity[5]. Endoscopic retrograde cholangiopancreatography (ERCP) has become the chief clinical treatment for choledocholithiasis because of its clinical advantages of less trauma and faster recovery in this period of advanced science and technology and improved medical technology and hospital hardware facilities. According to multicenter clinical research data, the recurrence rate in patients with choledocholithiasis after ERCP is 4%-24%[6]. Therefore, the high recurrence rate of choledocholithiasis has become the focus of attention for surgeons worldwide[6]. Presently, domestic and foreign studies on the recurrence mechanism of choledocholithiasis mainly focus on crucial issues such as biliary microecology, duodenal papilla sphincter functional damage and abnormalities caused by surgery, and individual biliary anatomical differences[7].
Choledocholithiasis is a common digestive disease occurring in the middle and lower segments of the common bile duct[8,9]. The main symptom of the disease is suppurative cholangitis, which can be severe and even life-threatening[10]. After decades of development, ERCP has many advantages, such as less trauma, less pain, faster recovery, and fewer postoperative complications, and is widely used for diagnosing and treating choledocholithiasis[10]. The primary and emerging procedures of ERCP include endoscopic sphincterotomy (EST), endoscopic papillary balloon dilation (EPBD), endoscopic sphincterotomy plus balloon dilation (ESBD), and endoscopic endoclip papilloplasty (EEPP)[11].
The delicate and complex structure of the Oddi sphincter is composed of the common bile duct, pancreatic duct, and ampullary sphincters[12]. The common bile duct sphincter is the strongest muscle fiber of the common bile duct located at its end and the main component of the Oddi sphincter[13]. Its contraction can be close to the end of the common bile duct. The Oddi sphincter is the controlling valve of the bile-pancreatic duct passage; thus, it can effectively prevent the reflux of duodenal contents, prevent bacteria and other retrograde infections, and indirectly regulate the secretion and storage of bile and pancreatic juice[14]. It plays an irreplaceable role in maintaining the normal physiological function of the bile-pancreatic duct. Protecting the function of Oddi’s sphincter during ERCP has received increasing attention from physicians[15].
This study was critical for analyzing the factors influencing post-ERCP pancreatitis (PEP), an independent risk factor for PEP, and for undertaking corresponding measures to prevent PEP. In this study, we analyzed primary indicators (common bile duct stones, history of pancreatitis, Oddi sphincter dysfunction, and pancreatic imaging) and secondary indicators (pancreatic sphincterotomy, Oddi’s sphincter manometries, and ERCP operation failure). This study investigated the effects of different ERCP techniques on the Oddi sphincter.
The clinical data of 91 patients who underwent ERCP at Yixing Hospital of Traditional Chinese Medicine between February 2018 and February 2021 were analyzed retrospectively. The patients were divided into EST (n = 24) and EPBD (n = 67) groups. All experiments were conducted in accordance with the guidelines issued by the Institutional Care and Use Committee at our hospital. All selected personnel provided informed consent.
Inclusive criteria: (1) With a complete clinical history; (2) who underwent ERCP; (3) 18-70 years old; (4) with normal serum amylase levels before the operation; and (5) with signed informed consent forms.
Exclusion criteria: (1) Combination of benign or malignant biliary stricture; (2) history of biliary pancreatitis; (3) incomplete medical or follow-up data; and (4) patients with serious diseases, such as malignant tumors, cirrhosis, leukemia, etc.
Diagnostic criteria: (1) Symptoms lasting more than 24 h, such as abdominal pain, nausea, and vomiting; (2) needs hospitalization for diagnosis and treatment or more than 2 d; (3) worsening and reappearing abdominal pain; and (4) a reported postoperative serum amylase level of > 500 U/L as in the literature[1].
Data were collected from the two groups on age, sex, hypertension, diabetes, common bile duct stones, pancreatitis, bilirubin, common bile duct diameter, ampullary diverticulum, Oddi sphincter dysfunction, pancreatic imaging, ERCP type, pancreatic sphincterotomy, Oddi sphincter manometry, operation duration (> 1 h), ERCP outcome, difficulty in intubation (> 5 times), and presence of a guidewire entering numerous times into the pancreatic duct.
Statistical analyses were performed using GraphPad Prism 7 software (GraphPad Software, Inc.). Data are presented as the mean ± SD. Differences between groups were analyzed using the Student’s t-test. Multiple groups were analyzed using one-way ANOVA. P < 0.05 was considered statistically significant.
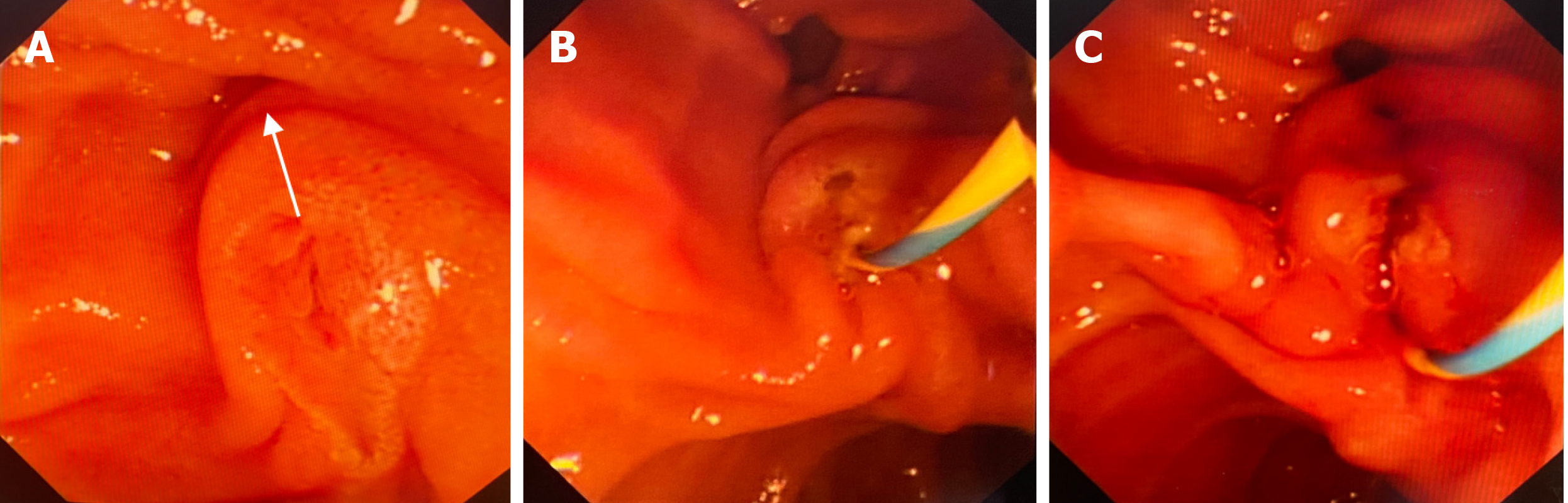
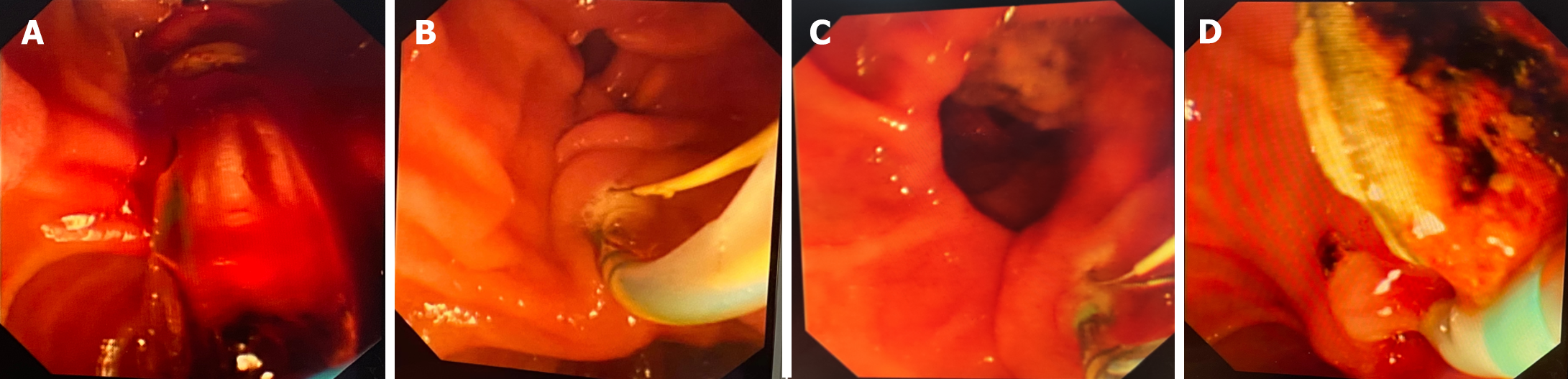
Under ERCP, EST is used to treat choledocholithiasis, and the incision diameter of the papillary sphincter is usually ≥ 1 cm (Figure 1). The specific surgical method of EPBD involves reaching the duodenal papilla through the duodenoscope inserting the guidewire into the common bile duct through the imaging catheter, and then removing the catheter. Based on the size of the stone and obstruction of the bile duct, balloon catheters with different diameters were selected for expansion (Figure 2).
Differences in hypertension, diabetes, increased bilirubin, small common bile duct diameter, and ampullary diverticulum between the two groups were nonsignificant (P > 0.05). Statistically significant differences were observed between the two groups concerning sex and age < 60 years (P < 0.05). The number of patients with a history of choledocholithiasis, pancreatitis, and Oddi sphincter dysfunction was higher in the EST group than in the EPBD group (P < 0.05; Table 1).
| Group | EST group (n = 24) | EPBD group (n = 67) |
| Gender | ||
| Man | 8 (33.33) | 35 (52.24) |
| Woman | 16 (66.67) | 32 (47.76) |
| Age (yr) | ||
| < 60 | 22 (91.67) | 33 (49.25) |
| ≥ 60 | 2 (8.33) | 34 (50.75) |
| History of hypertension | 13 (54.17) | 33 (49.25)a |
| History of diabetes | 16 (66.67) | 35 (52.34)a |
| History of choledocholithiasis | 18 (75.00) | 36 (53.73) |
| History of pancreatitis | 19 (79.17) | 28 (41.79) |
| Hyperbilirubin | 13 (54.17) | 34 (50.75) |
| Small diameter of common bile duct | 11 (45.83) | 31 (46.27) |
| Ampullary diverticulum | 10 (41.67) | 30 (44.78) |
| Oddi sphincter dysfunction | 20 (83.33) | 21 (31.34)a |
No significant differences were observed between the two groups in the ERCP type, choledochal sphincterotomy, or operation duration (> 1 h; P > 0.05). The number of pancreatic developments, sphincterotomies of the pancreatic duct, and difficult intubations was higher in the EST group than in the EPBD group (P < 0.05). Meanwhile, the number of Oddi’s sphincter manometries, ERCP surgical outcomes, and guidewires entering the pancreatic duct several times in the EST group were lower than those in the EPBD group (P < 0.05; Table 2).
| Group | EST group (n = 24) | EPBD group (n = 67) |
| Pancreatic development | 18 (75.00) | 30 (44.78)a |
| ERCP type | 12 (50.00) | 34 (50.75) |
| Sphincterotomy of pancreatic duct | 14 (58.33) | 27 (40.30)a |
| Oddi sphincter manometry | 13 (54.17) | 47 (70.15)a |
| Choledochal sphincterotomy | 6 (25.00) | 30 (44.78) |
| Operation duration (> 1 h) | 5 (20.83) | 14 (20.90) |
| ERCP surgical outcome | 2 (8.33) | 14 (20.90)a |
| difficult intubation | 16 (66.67) | 21 (31.34)a |
| The guide wire enters the pancreatic duct several times | 16 (66.67) | 64 (95.52)a |
The number of stone recurrences, reflux cholangitis, and cholecystitis cases was higher in the EST group than in the EPBD group (P < 0.05; Table 3).
Although a commonly used method for treating pancreaticobiliary system diseases, ERCP is invasive and prone to postoperative complications[16]. One such common complication is pancreatitis, which may lead to death if not treated timely[16]. The pathogenesis of PEP remains unclear; however, nipple intubation can lead to nipple water in patients, Oddi sphincter spasms, and obstruction of pancreatic juice drainage, resulting in pancreatitis[17-19]. In this study, differences in hypertension, common bile duct diameter, and ampullary diverticulum between the two groups were nonsignificant. The current study had some limitations. Large-sample clinical research on the effect of ESBD, especially EEPP, on the Oddi sphincter is still lacking, and the follow-up time for long-term complications is relatively short. This insufficiency persisted in this experiment.
The duodenal papillary sphincter, the Oddi sphincter, refers to the circular sphincter surrounding the end of the common bile duct, pancreatic ductal end, and ampulla, including the common bile duct, pancreatic duct, and ampullary sphincters[20]. It plays a “switch” role in the secretion of bile and pancreatic juice and principally maintains the fluid pressure of the biliary system, preventing the reflux of duodenal juice and the mutual communication between bile and pancreatic juice[21]. The dysfunction and structural damage of the Oddi sphincter will lead to diminished or loss of its “on-off” function, leading to cholestasis, duodenal fluid reflux, etc[22]. The clinical manifestations include biliary obstruction, biliary infection, pancreatitis, and recurrence of common bile duct stones[14,23]. In this study, the number of patients with a history of choledocholithiasis, pancreatitis, and Oddi sphincter dysfunction was higher in the EST group than in the EPBD group.
With the deepening of clinical exploration, choledocholithiasis surgery improvement, and the popularization of laparoscopy and endoscopy, laparoscopic common bile duct exploration (LCBDE) and ERCP have become the main clinical treatment methods for choledocholithiasis[24]. LCBDE is more traumatic and has a prolonged recovery period than ERCP[25]. However, regarding the long-term therapeutic effects, the stone recurrence rate was lower after LCBDE. ERCP is mainly combined with EPBD or EST, both of which are accompanied by varying degrees of damage to sphincter function and structure, leading to poor functioning of the “switch” of the Oddi sphincter postoperatively and consequently to cholestasis and infection of the biliary system, a major anatomical factor in stone recurrence[1]. In this study, the number of cases of pancreatic development, sphincterotomy of the pancreatic duct, and difficult intubation were higher in the EST group than in the EPBD group. Meanwhile, the number of Oddi’s sphincter manometries, ERCP surgical outcomes, and guidewires entering the pancreatic duct several times in the EST group were lower than those in the EPBD group.
Self-factors included age, sex, choledocholithiasis, a history of pancreatitis and Oddi sphincter dysfunction, pancreatic imaging, pancreatic sphincterotomy, Oddi sphincter manometry, ERCP failure, difficulty in intubation, and multiple access of the guidewire to the pancreatic duct[1]. Therefore, preventive measures should be implemented to reduce the incidence of PEP.
Compared with the attempt of EPBD at relaxing the duodenal papillary sphincter for stone extraction utilizing balloons, the damage to the function of the duodenal papillary sphincter caused by EPBD is considerable[26]. The long-term risk of choledocholithiasis recurrence is markedly increased because of the loss of function of the duodenal papillary sphincter after surgery[27]. EST causes irreversible damage to the duodenal papillary sphincter[28]. Therefore, surgeons should carefully consider the surgical method choice for young patients to retain sphincter function as much as possible. The reasonable selection of a surgical method to reduce functional damage to the duodenal papillary sphincter should be a crucial factor in effectively preventing the recurrence of common bile duct stones after surgery[29]. However, it is challenging to strictly grasp the surgical indications since corresponding clinical guidelines to select EST and EPBD surgical methods are lacking[30].
Using a balloon in EPBD to relax the duodenal papillary sphincter for lithotomy causes more damage to the function of the duodenal papillary sphincter than intended[26]. The long-term risk of recurrent choledocholithiasis is greatly increased due to the loss of duodenal papillary sphincter function after surgery[27]. According to retrospective studies, EST causes irreversible damage to the duodenal papilla sphincter[28]. Therefore, surgeons should carefully consider that the choice of surgery for young patients should preserve sphincter function. Reasonably, choosing the surgical method to reduce functional impairment of the duodenal papillary sphincter is an important factor in effectively preventing the recurrence of choledocholithiasis after surgery[29]. However, there is a lack of corresponding clinical guidelines for strictly determining surgical indications in terms of surgical selection for EST and EPBD. In this study, the number of stone recurrences, reflux cholangitis, and cholecystitis was higher in the EST group than in the EPBD group.
The current study had some limitations. The effect of ESBD, especially EEPP, on the Oddi sphincter is still lacking in large-sample clinical research, and the follow-up time for long-term complications is short. In the future, a large amount of clinical data is needed to confirm the advantages and disadvantages of ESBD and EEPP and their specific effects on the Oddi sphincter. With the increasing importance of Oddi sphincter function in the pathogenesis of biliary and pancreatic diseases, minimizing damage to the sphincter has become a common goal of clinicians. In clinical practice, we should re-recognize the function of the Oddi sphincter and explore the ERCP method that has the least impact on it and has the best effect so that patients can receive reasonable and standard treatment as far as possible.
In conclusion, common bile duct stones, a history of pancreatitis, Oddi sphincter dysfunction, pancreatic imaging, pancreatic sphincterotomy, Oddi’s sphincter manometries, ERCP operation failure, difficult intubation, and multiple guidewire entry into the pancreatic duct are all independent risk factors for PEP; thus, these findings allow to undertake corresponding countermeasures to prevent PEP after EST and EPBD in clinical practice.
| 1. | Park JC, Park JG. A Case of Biliary Cast Syndrome After Endoscopic and Percutaneous Management of Common Bile Duct Stone. Taehan Yongsang Uihakhoe Chi. 2022;83:224-229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Belgau I, Johnsen G, Græslie H, Mårvik R, Nymo S, Bjerkan K, Hyldmo Å, Klöckner C, Kulseng B, Hoff D, Sandvik J. Frequency of cholelithiasis in need of surgical or endoscopic treatment a decade or more after Roux-en-Y gastric bypass. Surg Endosc. 2023;37:1349-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Boni L, Huo B, Alberici L, Ricci C, Tsokani S, Mavridis D, Amer YS, Andreou A, Berriman T, Donatelli G, Forbes N, Kapiris S, Kayaalp C, Kylänpää L, Parra-Membrives P, Siersema PD, Black GF, Antoniou SA. EAES rapid guideline: updated systematic review, network meta-analysis, CINeMA and GRADE assessment, and evidence-informed European recommendations on the management of common bile duct stones. Surg Endosc. 2022;36:7863-7876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Chhabra P, On W, Paranandi B, Huggett MT, Robson N, Wright M, Maher B, Tehami N. Initial United Kingdom experience of endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography. Ann Hepatobiliary Pancreat Surg. 2022;26:318-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Gao F, Zhang C, Feng Y, Zhan Y. MRI Evaluation of Indomethacin Suppositories in the Prevention of Complications of Pancreatitis and Hyperamylasemia after Choledocholithiasis ERCP Based on Image Denoising Algorithm. Comput Math Methods Med. 2022;2022:4805185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Kattih O, Velanovich V. Comparing One-Stage vs Two-Stage Approaches for the Management of Choledocholithiasis. J Gastrointest Surg. 2023;27:534-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Ji Z, Wang Z, Li H. Abscess of ligamentum teres hepatis post-endoscopic retrograde cholangiopancreatography: A case report and a literature review. SAGE Open Med Case Rep. 2022;10:2050313X221110994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Lei Y, Lethebe BC, Wishart E, Bazerbachi F, Elmunzer BJ, Thosani N, Buxbaum JL, Chen YI, Bass S, Cole MJ, Turbide C, Brenner DR, Heitman SJ, Mohamed R, Forbes N. Test Performance Characteristics of Dynamic Liver Enzyme Trends in the Prediction of Choledocholithiasis. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 9. | Li J, Hu J, Li P, Wu Y, Wang Y, Ji M, Hua H, Ran W, Pan Y, Zhang S. Analysis of risk factors associated with endoscopic retrograde cholangiopancreatography for patients with liver cirrhosis: a multicenter, retrospective, clinical study. Chin Med J (Engl). 2022;135:2319-2325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Liu H, Pan W, Yan G, Li Z. A retrospective cohort study on the optimal interval between endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. Medicine (Baltimore). 2022;101:e29728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Lagouvardou E, Martines G, Tomasicchio G, Laforgia R, Pezzolla A, Caputi Iambrenghi O. Laparo-endoscopic management of chole-choledocholithiasis: Rendezvous or intraoperative ERCP? A single tertiary care center experience. Front Surg. 2022;9:938962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 12. | Coppola A, Piacentino F, Macchi E, Marchi G, Ierardi AM, Carrafiello G, Fontana F. First use of a scoring balloon to perform Oddi sphincteroplasty for biliary stones. Ann Gastroenterol. 2019;32:416-418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Feng Y, Zhang J, Jiao C, Zhu H, Cheng W, Xu S, Xiao B, Ni J, Chen X. Manometric Measurement of the Sphincter of Oddi in Patients with Common Bile Duct Stones: A Consecutive Study of the Han Population of China. Gastroenterol Res Pract. 2017;2017:9031438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Jia CK, Weng J, Chen YK, Yang QZ, Fu Y, Qin QF, Yu WM. Hepatectomy with primary closure of common bile duct for hepatolithiasis combined with choledocholithiasis. World J Gastroenterol. 2015;21:3564-3570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Chen CC, Wu SD, Tian Y, Siwo EA, Zeng XT, Zhang GH. Sphincter of Oddi-preserving and T-tube-free laparoscopic management of extrahepatic bile duct calculi. World J Surg. 2011;35:2283-2289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Long J, Li J, Liu L, Zhou X, Lu X. Analysis of Clinical Effects of Intubation and Sphincterotomy With Wire-guided Incision Knife Plus Balloon Dilatation in the Treatment of Choledocholithiasis: A Randomized Controlled Trial. Surg Laparosc Endosc Percutan Tech. 2022;32:558-563. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Minakari M, Samani RR, Shavakhi A, Jafari A, Alijanian N, Hajalikhani M. Endoscopic papillary balloon dilatation in comparison with endoscopic sphincterotomy for the treatment of large common bile duct stone. Adv Biomed Res. 2013;2:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Ding J, Li F, Zhu HY, Zhang XW. Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: An anatomic view. World J Gastrointest Endosc. 2015;7:274-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Tsai TJ, Lin CK, Lai KH, Chan HH, Wang EM, Tsai WL, Cheng JS, Yu HC, Chen WC, Hsu PI. Does preserved sphincter of Oddi function prevent common bile duct stones recurrence in patients after endoscopic papillary balloon dilation? J Chin Med Assoc. 2018;81:311-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Leszczyszyn J. Choledocholithiasis diagnostics - endoscopic ultrasound or endoscopic retrograde cholangiopancreatography? J Ultrason. 2014;14:125-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Masoni L, Mari FS, Pietropaolo V, Onorato M, Meucci M, Brescia A. Laparoscopic treatment for unsuspected common bile duct stones by transcystic sphincter of Oddi pneumatic balloon dilation and pressure-washing technique. World J Surg. 2013;37:1258-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Poincloux L, Rouquette O, Privat J, Gorce D, Abergel A, Dapoigny M, Bommelaer G. Large-balloon dilation of the sphincter of Oddi after sphincterotomy or infundibulotomy to extract large calculi or multiple common bile duct stones without using mechanical lithotripsy. Scand J Gastroenterol. 2013;48:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Turner GA, Ing AJ, Connor SJ. Endoscopic large balloon sphincteroplasty is a useful, safe adjunct for difficult to treat choledocholithiasis. ANZ J Surg. 2016;86:395-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Lu HS, Yang TC, Chang CY, Huang YH, Hou MC. The risk of variceal bleeding during endoscopic retrograde cholangiopancreatography. J Chin Med Assoc. 2022;85:896-900. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Lu R, Luthra A, Han S. Combined EUS-guided gallbladder drainage with rendezvous ERCP for treatment of concomitant cholecystitis, cholelithiasis, and choledocholithiasis. VideoGIE. 2022;7:250-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Wu JH, Kang JW, Wang YS, Lin HJ, Chen CY. Comparison of Different Endoscopic Methods Used for Managing Choledocholithiasis in Patients with End-Stage Renal Disease Undergoing Hemodialysis. Dig Dis Sci. 2022;67:5239-5247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Mok SR, Arif M, Diehl DL, Khara HS, Ho HC, Elfant AB. Safety and efficacy of minimal biliary sphincterotomy with papillary balloon dilation (m-EBS+EPBD) in patients using clopidogrel or anticoagulation. Endosc Int Open. 2017;5:E157-E164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 384] [Article Influence: 42.7] [Reference Citation Analysis (1)] |
| 29. | Chung JW, Chung JB. Endoscopic papillary balloon dilation for removal of choledocholithiasis: indications, advantages, complications, and long-term follow-up results. Gut Liver. 2011;5:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Park CH, Jung JH, Nam E, Kim EH, Kim MG, Kim JH, Park SW. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc. 2018;87:43-57.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |