Published online Jun 27, 2024. doi: 10.4240/wjgs.v16.i6.1521
Revised: April 22, 2024
Accepted: May 8, 2024
Published online: June 27, 2024
Processing time: 177 Days and 20 Hours
In colon cancer surgery, ensuring the complete removal of the primary tumor and draining lymph nodes is crucial. Lymphatic drainage in the colon follows the vascular supply, typically progressing from pericolic to paraaortic lymph nodes. While NCCN guidelines recommend the removal of 10-12 lymph nodes for ade
Core Tip: Despite many decades of research, there is no consensus on standard surgical techniques for right-side colon cancer. The complete oncological resection is much more than simple number of harvested lymph nodes. Identifying the ileocolic vessels at their origin from superior mesenteric vessels is the central technique to serve this purpose. Complete visceral and parietal mesocolon excision removes the intact specimen. D3 lymphadenectomy removes all draining regional lymph nodes. Both principles serve the same goal with different emphases. So addressing adequate lymphadenectomy with complete negative margin R0 resection is central to this article.
- Citation: Yadav K. Laparoscopic right radical hemicolectomy: Central vascular ligation and complete mesocolon excision vs D3 lymphadenectomy - How I do it? World J Gastrointest Surg 2024; 16(6): 1521-1526
- URL: https://www.wjgnet.com/1948-9366/full/v16/i6/1521.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i6.1521
Radical right hemicolectomy remains the preferred treatment for right-sided colon cancers, with the removal of draining lymph nodes being a crucial step for long-term survival. Despite decades of research, controversies persist regarding which lymph node stations should be removed and the establishment of universal nomenclature. The Japanese classification for colon cancer categorizes regional lymph nodes into D1 (pericolic lymph nodes), D2 (pericolic and inter
An oncologically appropriate surgery with R0 resection and adequate lymphadenectomy significantly improves the survival of colon cancer patients[4,5]. Complete mesocolon excision (CME) with central vascular ligation (CVL) has been associated with a 15% better overall survival at 5 years, with this improvement reaching up to 27% in stage III cases[6]. The fundamental principle is to remove the cancer-bearing segment of the colon along with the intact fascia and lym
Before surgery, patients undergo preoperative bowel preparation with a laxative, along with prophylactic intravenous third-generation cephalosporin and metronidazole administered 30 min prior. Patients are positioned in a low lithotomy position, with a body warmer blanket and belt applied over the chest. Shoulder supports are utilized, and the legs are secured in lithotomy poles along with deep vein thrombosis pumps. A 12-mm camera port is inserted just above the um
The mesentery of the ascending colon and terminal ileum is retracted upwards and laterally, creating tension on the ICL pedicle. This maneuver induces a stretch in the midline at the origin of the ICL pedicle from the superior mesenteric vessels, facilitating identification of the superior mesenteric vein (SMV). The mesentery is incised along an appropriate line over the SMV, below the third part of the duodenum and approximately opposite the falciform ligament. Fibrofatty and lymphatic tissue are reflected towards the right, exposing the right side of the SMV. The origin of the ICL pedicle is identified, and further dissection superiorly over the SMV reveals the MCA.
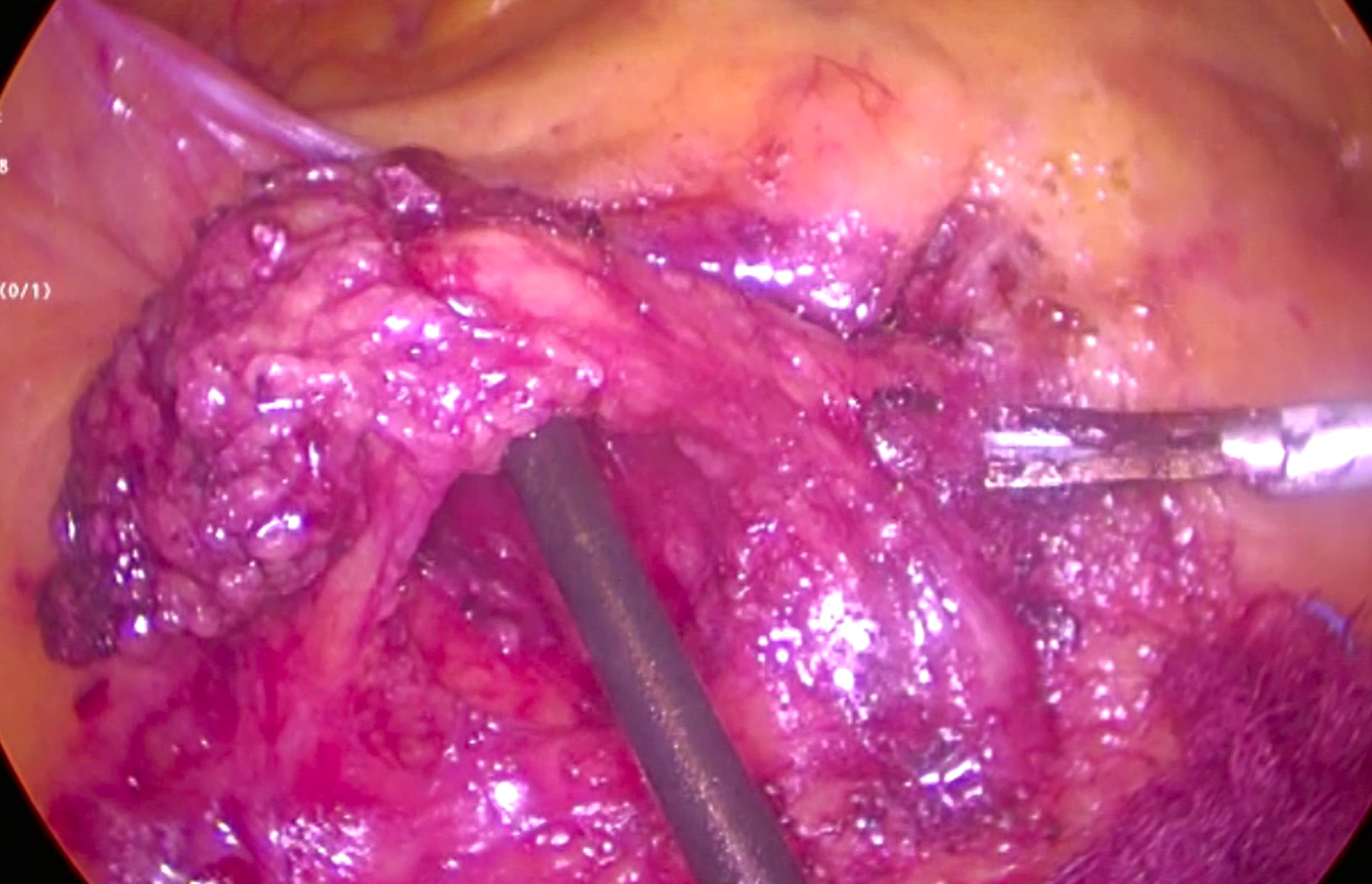
The duodenum is identified, and the mesentery overlying it is reflected, revealing an avascular plane. Continued inferior dissection over the SMV allows for the skeletonization of the ICL pedicle origin. All lymphatic tissue is reflected towards the right, and the ICL pedicle is doubly ligated at its origin with hemoclip and then cut (Figure 2).
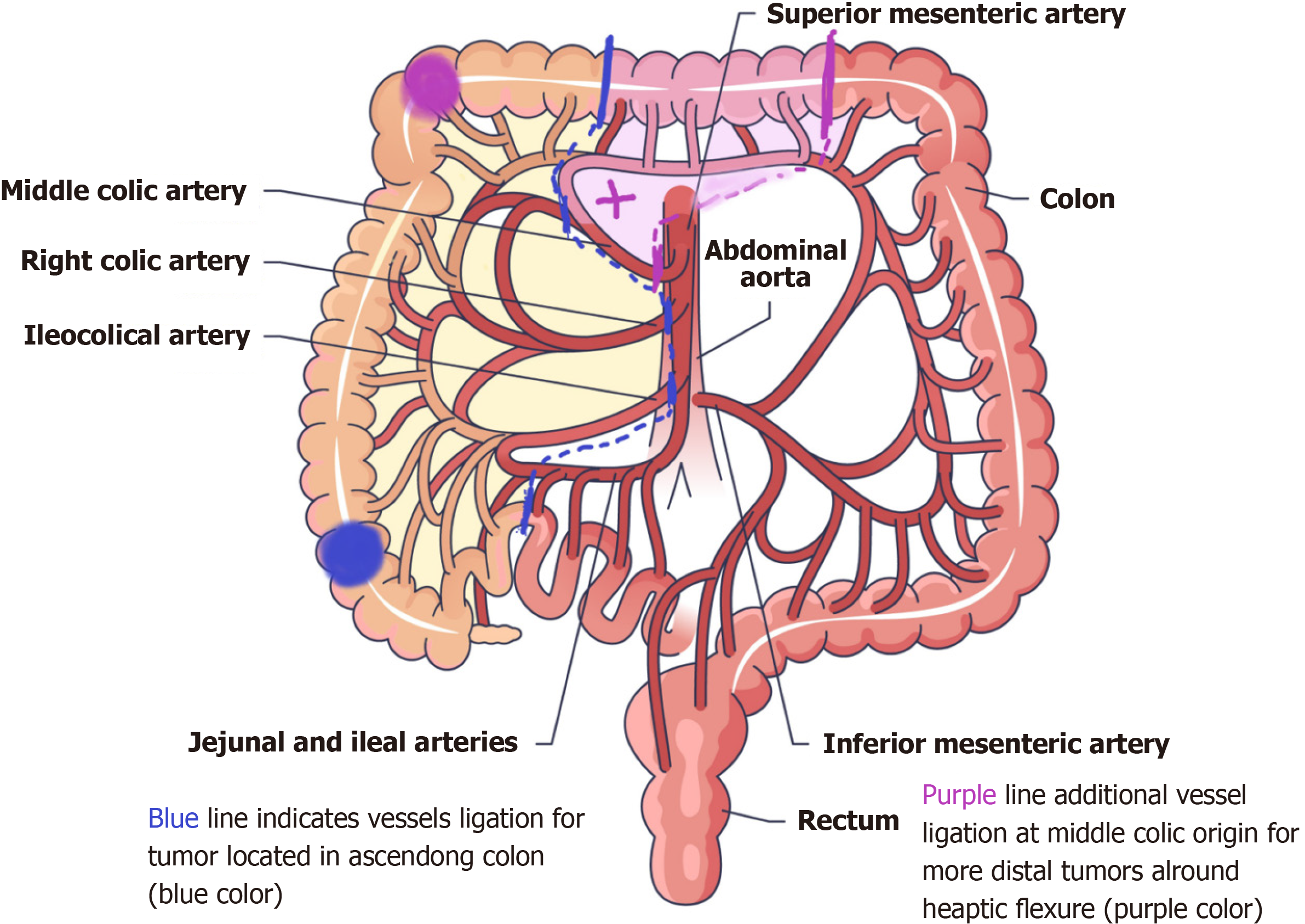
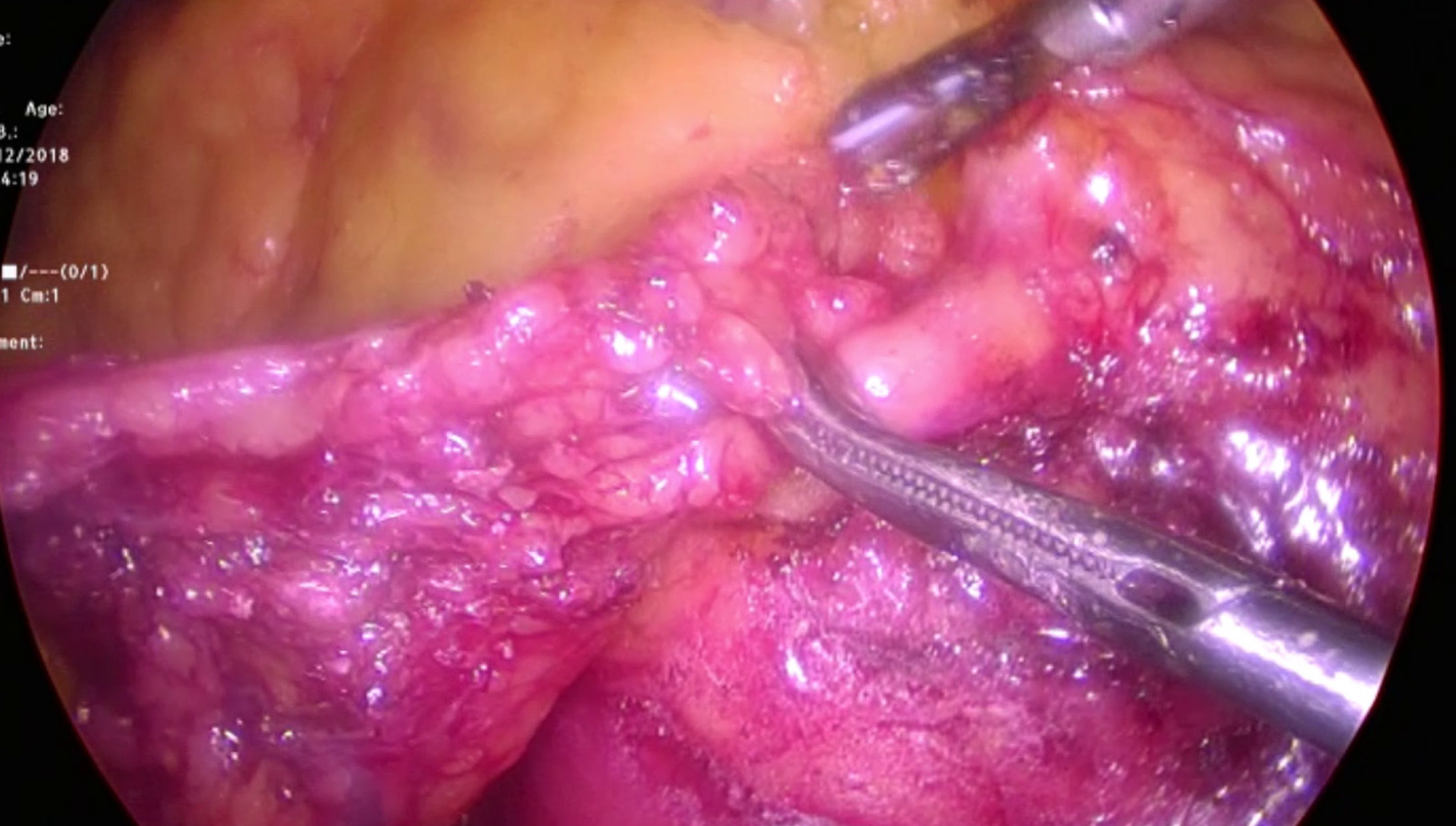
The MCA is identified through previous dissection, and the transverse colon is retracted upwards to expose both the right and left branches of the MCA. In cases where the primary tumor is located in the cecum or ascending colon, the right branch of the MCA is ligated and cut (Figure 3). Alternatively, in cases where the primary tumor is around the hepatic flexure, the MCA is ligated at its origin. These resection lines allow for the removal of all draining lymph nodes up to D3 stations (Figure 4).
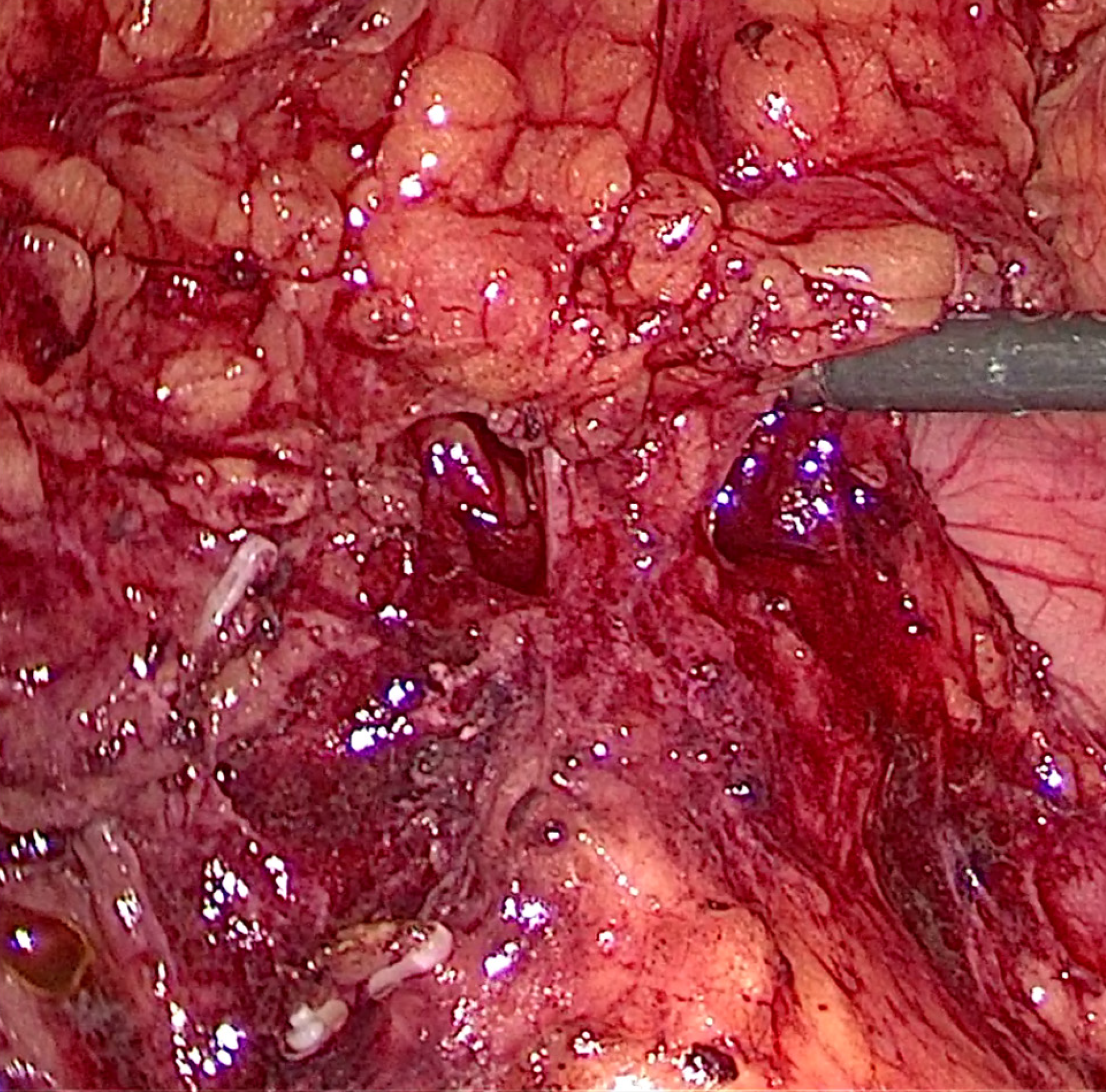
The ligated ICL pedicle is lifted upwards, and dissection is performed along the fascia above the retroperitoneum, iden
The gastrocolic omentum is divided, entering the lesser sac and completing the mobilization of the hepatic flexure. Lateral dissection of the already mobilized ascending colon along Toldt’s line is performed, completing the dissection (Video 1).
The umbilical port is enlarged by 2-3 cm, and a wound protector is applied. The mobilized colon is delivered out, me
Studies on CME have demonstrated a survival advantage of > 10% with the adoption of this technique[9]. Similarly, research focusing on D3 lymphadenectomy has shown a relative risk reduction in mortality by 18%[10]. Despite ori
Our study seeks to underscore the importance of modern surgical principles in right hemicolectomy for malignancy. In the contemporary era, all advancements should be integrated, and efforts should be made to standardize surgical tech
Surgical techniques are refined based on embryology and tumor biology, with the adoption of these techniques resulting in better survival and cure rates in oncology. We advocate for the adoption of CME + CVL with D3 lymphadenectomy as the standard approach for carcinoma of the right side of the colon. Both open and minimally invasive approaches can be utilized when performing this surgery.
| 1. | Muro K. Systemic chemotherapy for metastatic colorectal cancer -Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2016 for treatment of colorectal cancer. Nihon Shokakibyo Gakkai Zasshi. 2017;114:1217-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Kobayashi H, West NP. CME versus D3 Dissection for Colon Cancer. Clin Colon Rectal Surg. 2020;33:344-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Shimada Y, Hamaguchi T, Mizusawa J, Saito N, Kanemitsu Y, Takiguchi N, Ohue M, Kato T, Takii Y, Sato T, Tomita N, Yamaguchi S, Akaike M, Mishima H, Kubo Y, Nakamura K, Fukuda H, Moriya Y. Randomised phase III trial of adjuvant chemotherapy with oral uracil and tegafur plus leucovorin versus intravenous fluorouracil and levofolinate in patients with stage III colorectal cancer who have undergone Japanese D2/D3 lymph node dissection: final results of JCOG0205. Eur J Cancer. 2014;50:2231-2240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Enker WE, Laffer UT, Block GE. Enhanced survival of patients with colon and rectal cancer is based upon wide anatomic resection. Ann Surg. 1979;190:350-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 223] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Bokey EL, Chapuis PH, Dent OF, Mander BJ, Bissett IP, Newland RC. Surgical technique and survival in patients having a curative resection for colon cancer. Dis Colon Rectum. 2003;46:860-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 140] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | West NP, Morris EJ, Rotimi O, Cairns A, Finan PJ, Quirke P. Pathology grading of colon cancer surgical resection and its association with survival: a retrospective observational study. Lancet Oncol. 2008;9:857-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 321] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 7. | Mike M, Kano N. Laparoscopic surgery for colon cancer: a review of the fascial composition of the abdominal cavity. Surg Today. 2015;45:129-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Garcia-Granero A, Pellino G, Frasson M, Fletcher-Sanfeliu D, Bonilla F, Sánchez-Guillén L, Domenech Dolz A, Primo Romaguera V, Sabater Ortí L, Martinez-Soriano F, Garcia-Granero E, Valverde-Navarro AA. The fusion fascia of Fredet: an important embryological landmark for complete mesocolic excision and D3-lymphadenectomy in right colon cancer. Surg Endosc. 2019;33:3842-3850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Anania G, Davies RJ, Bagolini F, Vettoretto N, Randolph J, Cirocchi R, Donini A. Right hemicolectomy with complete mesocolic excision is safe, leads to an increased lymph node yield and to increased survival: results of a systematic review and meta-analysis. Tech Coloproctol. 2021;25:1099-1113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Kotake K, Mizuguchi T, Moritani K, Wada O, Ozawa H, Oki I, Sugihara K. Impact of D3 lymph node dissection on survival for patients with T3 and T4 colon cancer. Int J Colorectal Dis. 2014;29:847-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 99] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 11. | Toldt C, Dalla Rosa A, Paul E, Toldt C. An atlas of human anatomy for students and physicians. New York: Rebman Company, 1919. [DOI] [Full Text] |
| 12. | Congdon ED, Blumberg R, Henry W. Fasciae of fusion and elements of the fused enteric mesenteries in the human adult. Am J Anat. 1942;70:251-279. [RCA] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Denman AM. Principles of immunology. J Med Microbiol. 1980;13:485-485. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009;11:354-64; discussion 364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1104] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 15. | Siani LM, Garulli G. Laparoscopic complete mesocolic excision with central vascular ligation in right colon cancer: A comprehensive review. World J Gastrointest Surg. 2016;8:106-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Sica GS, Vinci D, Siragusa L, Sensi B, Guida AM, Bellato V, García-Granero Á, Pellino G. Definition and reporting of lymphadenectomy and complete mesocolic excision for radical right colectomy: a systematic review. Surg Endosc. 2023;37:846-861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 17. | Hartgrink HH, van de Velde CJ, Putter H, Bonenkamp JJ, Klein Kranenbarg E, Songun I, Welvaart K, van Krieken JH, Meijer S, Plukker JT, van Elk PJ, Obertop H, Gouma DJ, van Lanschot JJ, Taat CW, de Graaf PW, von Meyenfeldt MF, Tilanus H, Sasako M. Extended lymph node dissection for gastric cancer: who may benefit? Final results of the randomized Dutch gastric cancer group trial. J Clin Oncol. 2004;22:2069-2077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 653] [Article Influence: 31.1] [Reference Citation Analysis (0)] |