Published online May 27, 2024. doi: 10.4240/wjgs.v16.i5.1461
Revised: March 13, 2024
Accepted: April 10, 2024
Published online: May 27, 2024
Processing time: 106 Days and 20.4 Hours
Hem-o-lok clips are typically used to control the cystic duct and vessels during laparoscopic cholecystectomy (LC) and common bile duct exploration for stones in the bile duct and gallbladder. Here, we report a unique example of Hem-o-lok clip movement towards the duodenal bulb after LC, appearing as a submucosal tumor (SMT). Additionally, we provide initial evidence of gradual and evolving endoscopic manifestations of Hem-o-lok clip migration to the duodenal bulb wall and review the available literature.
A 72-year-old man underwent LC for gallstones, and Hem-o-lok clips were used to ligate both the cystic duct and cystic artery. Esophagogastroduodenoscopy (EGD) 2 years later revealed an SMT-like lesion in the duodenal bulb. Due to the symptomatology, the clinical examination did not reveal any major abnormalities, and the patient was followed up as an outpatient. A repeat EGD performed 5 months later revealed an SMT-like lesion in the duodenal bulb with raised edges and a central depression. A third EGD was conducted, during which a Hem-o-lok clip was discovered connected to the front side of the duodenum. The clip was extracted easily using biopsy forceps, and no complications occurred. Two mon
Clinicians should be aware of potential post-LC complications. Hem-o-lok clips should be removed if symptomatic.
Core Tip: Migration of Hem-o-lok clips to the duodenal bulb may manifest as a slightly raised lesion resembling a sub
- Citation: Liu HY, Yin AH, Wei Z. Hem-o-lok clip migration to duodenal bulb post-cholecystectomy: A case report. World J Gastrointest Surg 2024; 16(5): 1461-1466
- URL: https://www.wjgnet.com/1948-9366/full/v16/i5/1461.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i5.1461
Migration of a Hem-o-lok clip to the duodenal bulb after laparoscopic cholecystectomy (LC) is rare in clinical practice[1]. Herein, we report on a gradual and evolving process of Hem-o-lok clip movement towards the duodenal bulb subsequent to LC. In addition, we have examined the research papers on the migration of Hem-o-lok clips to the duodenal bulb post-LC that were indexed in the PubMed database. We conducted the search using keywords including “Hem-o-lok clip”, “migration”, “duodenum”, “laparoscopic cholecystectomy”, and “laparoscopic common bile duct exploration”. Approximately 6 cases were retrieved, and we provide a summarization and analysis of them in detail.
A 72-year-old man presented with a complaint of abdominal pain, which had persisted over the previous 10 d.
The patient had undergone LC for symptomatic gallstone disease 2 years previously and presented to the hospital com
The patient had a clinical history of primary esophageal, hypopharyngeal, and lung cancers. Additionally, he had hy
The patient had a history of excessive tobacco use and consumption of alcoholic beverages.
Vital signs were stable for the patient. He also showed no tenderness or rebound tenderness upon palpation, and the abdomen was flat and soft.
Routine coagulation test and tumor marker test results were within normal limits.
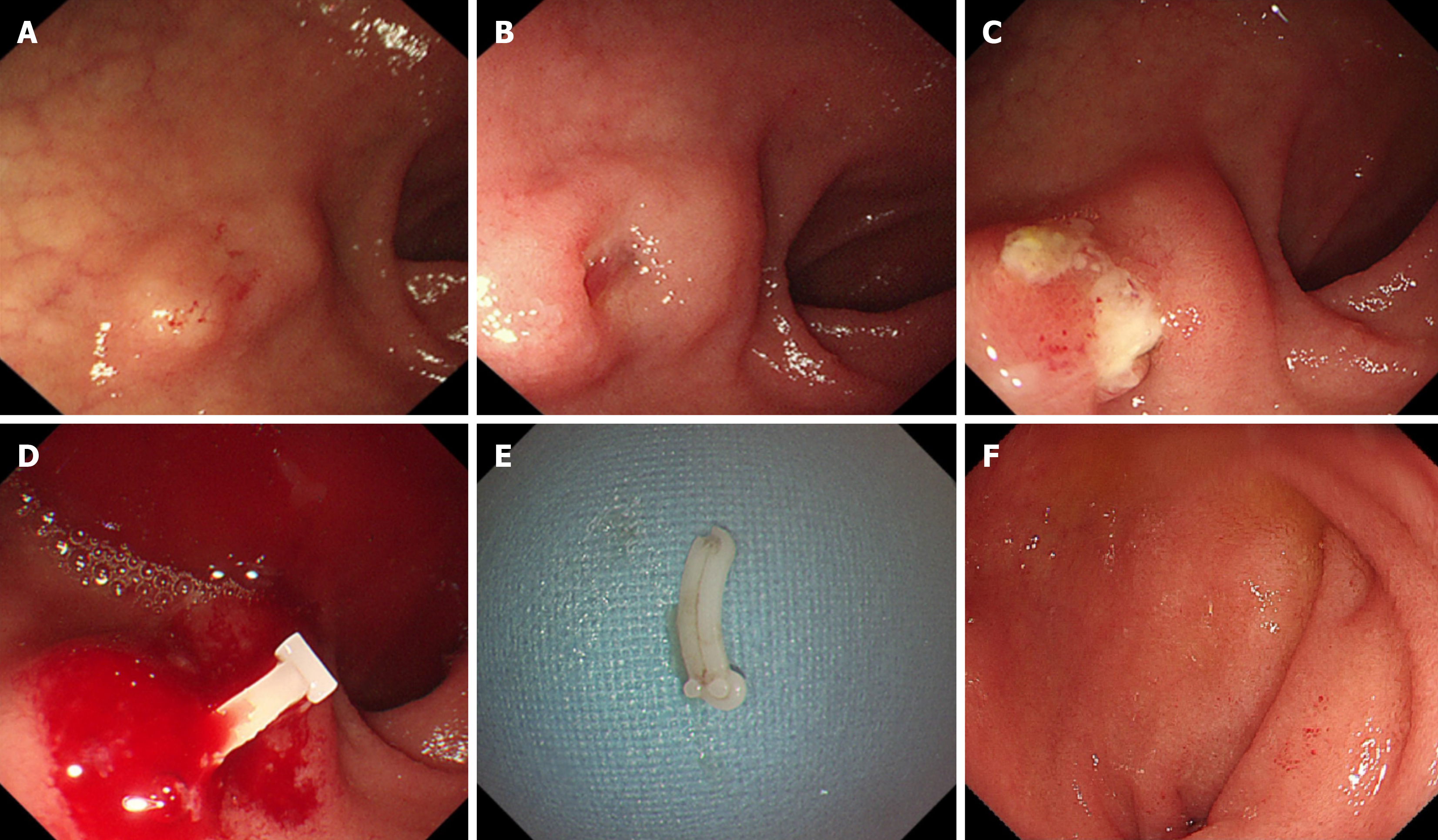
An SMT-like lesion, with a fixed foreign body, covered by white exudates, was observed in the duodenal bulb during the third EGD (Figure 1C). Around the lesion, erosions and edema were observed in the duodenum. When the biopsy forceps were used to touch the lesion, it was hard and active. Abdominal computed tomography (CT) revealed that the foreign body had migrated into the duodenal bulb (Figure 2).
The patient was diagnosed as foreign body in duodenal bulb.
Olympus grasping forceps were used to remove the foreign body (Figure 1D), which was the Hem-o-lok clip (Figure 1E). The patient was discharged from the hospital the next day without complications such as hemorrhage and perforation.
After 2 months, we performed another EGD. The clip was no longer visible, and the duodenum exhibited a healthy mucosal covering (Figure 1F).
Since the Hem-o-lok clip’s inception in 1999, it has been used for a wide variety of applications in the urinary tract, hepatobiliary, and gastrointestinal surgeries. Complications associated with postoperative Hem-o-lok clip displacement have been reported[2-5]. Postoperative clip displacement can lead to various complications, such as rectal elevated lesion caused by Hem-o-lok clip migration after prostate cancer surgery, abscess in the fallopian tube caused by Hem-o-lok clip migration after laparoscopic appendectomy, and dysphagia caused by Hem-o-lok clip migration into the esophagus sub
Migration of the Hem-o-Lok clip to the duodenal bulb can manifest as various endoscopic findings, including ulcers, erosions of the mucosa, and lesions resembling SMTs[14,15]. In this particular instance, the Hem-o-lok clip migrated to the duodenal bulb following LC and presented as a lesion resembling an SMT, requiring differentiation from polyps, cysts, stromal tumors, ectopic pancreatic lipomas, and carcinoids. Initially, the patient exhibited a gradual and evolving endoscopic presentation of Hem-o-lok clip movement towards the wall of the duodenal bulb.
After conducting a thorough search in the PubMed database, we discovered a total of 6 cases (4 women/2 men) since 2010 where Hem-o-lok clip migration to the duodenal bulb occurred following a LC. These cases are documented in Table 1 with corresponding references. The latest migration occurred 2 years post-LC and LCBDE, and the earliest occurred at nearly at 4 months. Minimum and maximum ages were 41 years and 67 years, respectively[14]. Of these, 1 patient was asymptomatic and 5 were symptomatic (e.g., melena or abdominal pain). The clinical manifestations of clip migration to duodenal bulb were also atypical, including abdominal pain, nausea, vomiting, gastrointestinal bleeding, and anemia. It is easy to miss diagnosis and misdiagnosis[1,15]. The clip was discharged spontaneously without com
| Ref. | Patients, n | Age in yr | Sex | Clips | Type of surgery | Time from surgery | Symptoms | Diagnosis | Treatment |
| Mantoo et al[13], 2010 | 1 | 57 | F | Hem-o-lok | LC | 1 yr | Melena | EGD | Endoscopic removal |
| Seyyedmajidi et al[14], 2013 | 1 | 41 | M | Hem-o-lok | LC | 8 months | Abdominal pain | EGD | Endoscopic removal |
| Soga et al[15], 2016 | 1 | 66 | F | Hem-o-lok | LC | 13 months | Asymptomatic | EGD + CT | PPI/spontaneous detachment |
| Padmanabhan et al[18], 2016 | 1 | 59 | F | Hem-o-lok | LC | 2 yr | Melena | EGD + CT | ND |
| Zheng et al[19], 2018 | 1 | 54 | M | Hem-o-lok | LC + LCBDE | 4 months | Abdominal pain | EGD | Observation |
| Yang et al[20], 2023 | 1 | 67 | F | Hem-o-lok | LC | ND | Abdominal pain | EGD + CT | Endoscopic removal |
However, there is no clear etiology or exact incidence for clip migration[16-18]. We considered three possible mecha
There is no clear consensus on the management of clip migration to the duodenal bulb after LC. According to earlier findings, the majority of Hem-o-lok clips that migrated postoperatively were typically extracted using endoscopic me
Migration of the Hem-o-lok clip to the duodenal bulb after LC is uncommon in clinical practice and may manifest as a lesion resembling SMT, slightly protruding in the duodenal bulb. Clinicians need to be aware of the potential complications post-LC. While the Hem-o-lok clip has migrated, clinicians can adopt a watch-and-wait strategy post-LC if the patient is asymptomatic. Clips should be removed if symptomatic.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade B
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade B
P-Reviewer: Ghannam WM, Egypt; Lamichane SR, Nepal S-Editor: Chen YL L-Editor: A P-Editor: Xu ZH
| 1. | Barabino M, Luigiano C, Piccolo G, Pellicano R, Polizzi M, Giovenzana M, Santambrogio R, Pisani Ceretti A, Andreatta E, Palamara MA, Giacobbe G, Consolo P, Opocher E. Hem-o-Lok clip migration into the duodenum after laparoscopic digestive surgery: a systematic review. Minerva Chir. 2019;74:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Kiremit MC, Koseoglu E, Acar O, Kilic M, Kordan Y, Canda AE, Balbay MD, Esen T. Distal ureteral stone formation over migrated Hem-o-lok clip after robot-assisted partial nephrectomy. Int J Surg Case Rep. 2019;58:201-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Liu DR, Wu JH, Shi JT, Zhu HB, Li C. Hem-o-lok clip migration to the common bile duct after laparoscopic common bile duct exploration: A case report. World J Clin Cases. 2022;10:6548-6554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | Dibitetto F, Russo P, Marino F, Ragonese M, Nigro D, Foschi N. Staghorn Caliceal Hem-o-Lok Stone: a long-term complication of robotic partial nephrectomy: a case report and literature review. Urol Int. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Wu X, Yan H, Zhao S, Zhang X, Zhu K. Clip migration complicated by choledocholithiasis after laparoscopic biliary surgery: a report of four cases. J Int Med Res. 2023;51:3000605231190766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 6. | Zhang Q, Deng D, Chen C, Liu J, Chen W, Wang L, Chai H. Endoscopic submucosal dissection treatment of a case of Hem-o-lok® clip migration into the rectum submucosa. Rev Esp Enferm Dig. 2022;114:683-684. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Feng TY, Jan HC, Chou SJ, Wang SC. Migration of Hem-O-Lok clip to the fallopian tube after laparoscopic appendectomy: A case report. Asian J Surg. 2021;44:1570-1571. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kordzadeh A, Charalabopoulos A, Lorenzi B. Transmural migration of azygous vein Hem-O-lok clip causing food bolus 3 months following uneventful minimally invasive oesophagectomy. Acta Chir Belg. 2018;118:270-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Armellini E, Metelli F, Anderloni A, Cominardi A, Aragona G, Marini M, Pace F. Lumen-apposing-metal stent misdeployment in endoscopic ultrasound-guided drainages: A systematic review focusing on issues and rescue management. World J Gastroenterol. 2023;29:3341-3361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 10. | Agarwal PK, Golmei J, Goyal R, Maurya AP. Comparison Between Closed and Open Methods for Creating Pneumoperitoneum in Laparoscopic Cholecystectomy. Cureus. 2023;15:e35991. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Qu JW, Wang GY, Yuan ZQ, Li KW. Hem-o-lok Clips Migration: An Easily Neglected Complication after Laparoscopic Biliary Surgery. Case Rep Surg. 2017;2017:7279129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Liu Y, Ji B, Wang Y, Wang G. Hem-o-lok clip found in common bile duct after laparoscopic cholecystectomy and common bile duct exploration: a clinical analysis of 8 cases. Int J Med Sci. 2012;9:225-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Mantoo SK, Rao J. An unusual cause of upper gastrointestinal bleeding. Endoscopy. 2010;42 Suppl 2:E123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Seyyedmajidi M, Hosseini SA, Hajiebrahimi S, Vafaeimanesh J. Hem-o-Lok Clip in the First Part of Duodenum after Laparoscopic Cholecystectomy. Case Rep Gastrointest Med. 2013;2013:251634. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Soga K, Kassai K, Itani K. Duodenal Ulcer Induced by Hem-o-Lok clip after Reduced Port Laparoscopic Cholecystectomy. J Gastrointestin Liver Dis. 2016;25:95-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Park DJ, Kim BG, Jeong ID, Kim GY. Silent invasion of Hem-O-Lok clip. Ann Surg Treat Res. 2018;94:159-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Heatley MK, Nagarajan DV. The ulcer and the clip: which came first? Gut. 2002;50:129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Padmanabhan H, Wheatley D, Brookes MJ. An Unusual Cause of Postcholecystectomy Gastrointestinal Hemorrhage. Gastroenterology. 2016;150:1535-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Zheng Y, Wang Y, Bai X, Liu D, Li F. Letter to the editor on "The cystic duct and artery were clipped using a clip applier". Nonmetal clip migration after laparoscopic cholecystectomy. Asian J Surg. 2018;41:585-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Yang YQ, Gou WB. The displaced polymer clamp entered the duodenum causing an abscess: A case report. Medicine (Baltimore). 2023;102:e35783. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |