Published online May 27, 2024. doi: 10.4240/wjgs.v16.i5.1443
Revised: March 13, 2024
Accepted: April 12, 2024
Published online: May 27, 2024
Processing time: 131 Days and 2 Hours
The treatment of postoperative anastomotic stenosis (AS) after resection of co
We report a 72-year-old man who underwent radical resection of colorectal cancer and ileostomy one year ago. An ileostomy closure was prepared six months ago, but colonoscopy revealed a narrowing of the rectal anastomosis. Endoscopic ba
MCT is a minimally invasive method that can be used for the treatment of post
Core Tip: Endoscopic balloon dilation of postoperative anastomotic stenosis (AS) after colorectal cancer surgery is not always effective. Repeated balloon dilation can aggravate the stenosis. Magnetic compression technique (MCT) has been used for gastrointestinal anastomosis, but its use for the treatment of postoperative AS of colorectal cancer has rarely been reported. This article reports the treatment process and outcomes of MCT for the treatment of postoperative AS after colorectal cancer surgery. Our experience suggests that MCT can be an effective treatment for postoperative AS in this setting.
- Citation: Zhang MM, Sha HC, Xue HR, Qin YF, Dong FF, Zhang L, Lyu Y, Yan XP. Treatment of anastomotic stricture after rectal cancer operation by magnetic compression technique: A case report. World J Gastrointest Surg 2024; 16(5): 1443-1448
- URL: https://www.wjgnet.com/1948-9366/full/v16/i5/1443.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i5.1443
The reported incidence of anastomotic stenosis (AS) after radical resection of colorectal cancer is about 3%-30%[1]. Anastomotic fistula, infection, and ultra-low anal preservation operation are risk factors for AS[2]. The typical symptoms of rectal AS include difficulty in defecation, bloating, and anal pain[3]. As a minimally invasive treatment, endoscopic balloon dilatation is routinely performed in clinical settings[4]. However, this technique is effective only in approximately 20% of patients[5]. Repeated endoscopic balloon dilatation in patients who show poor response may aggravate stenosis. The occurrence of AS prevents ileostomy closure, greatly reducing the quality of life of patients. For patients who do not respond to endoscopic balloon dilation, we propose an endoscopy-assisted magnetic compression technique (MCT) to treat AS, which achieved satisfactory therapeutic effect after initial clinical application.
A 72-year-old man who underwent radical resection of rectal cancer one year ago presented with rectal stenosis for the past 6 months.
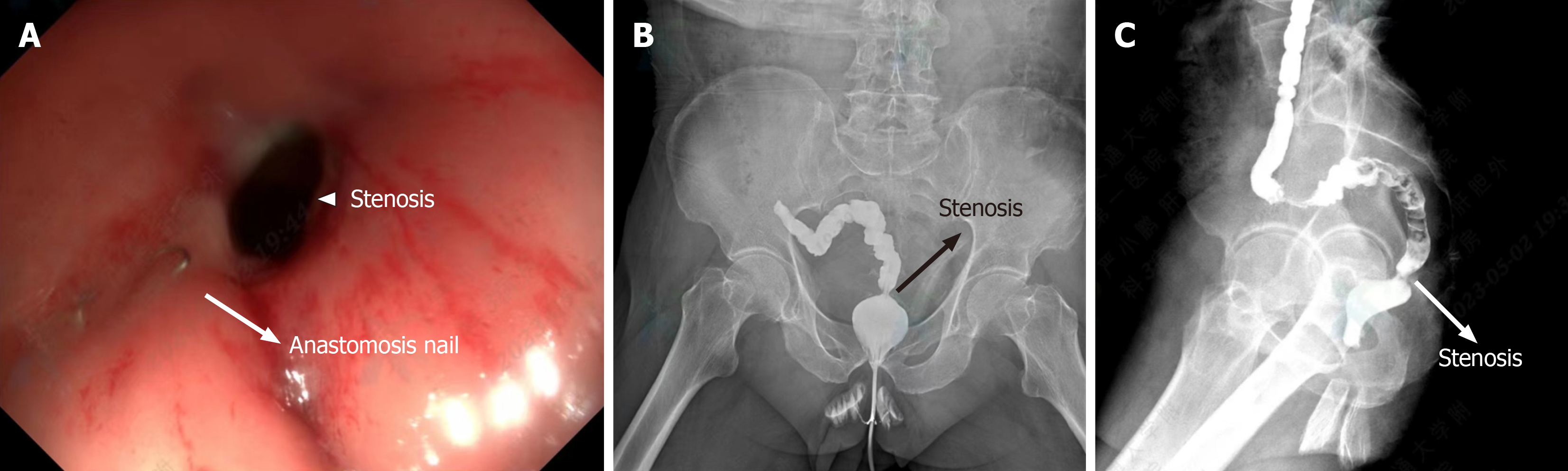
The patient underwent radical resection of rectal cancer and ileostomy one year ago for rectal cancer. A colonoscopy performed six months ago revealed a narrow rectal anastomosis, which did not meet the indications for ileostomy re
The past medical history was unremarkable.
There was no family history of this condition.
The patient’s vital signs were stable, and auscultation of the heart and lungs was normal. The abdomen was flat and soft with no tenderness. There was no mobile dullness and bowel sounds were normal. Ileostomy was visible in the lower right quadrant of the abdomen, and the intestinal mucosa of ileostomy was normal.
There were no significant abnormalities in the patient’s hematological examination.
Based on the colonoscopy and colonography findings, the patient was diagnosed as having rectal AS.
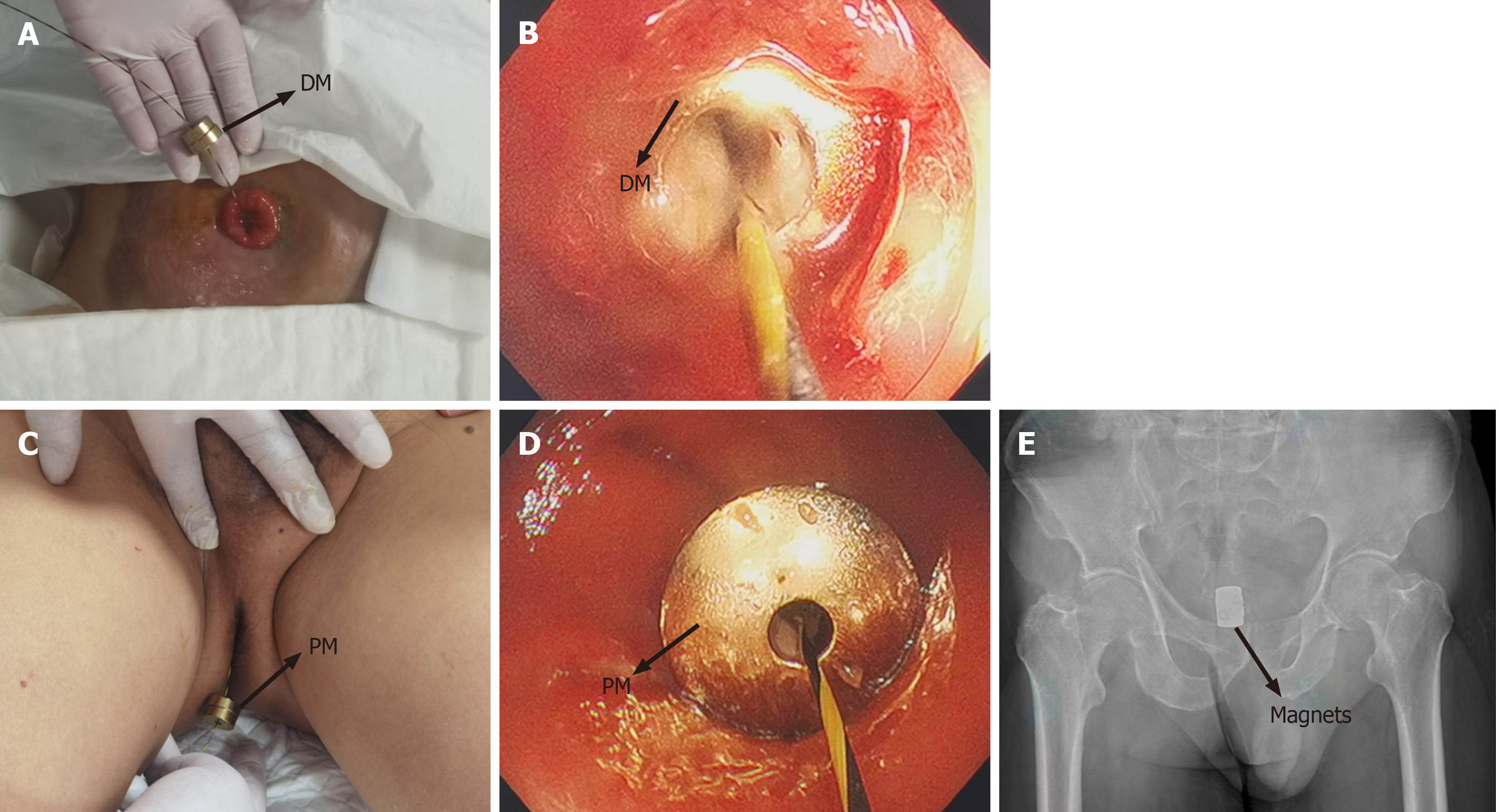
The patient signed an informed consent form for treatment. After intravenous anesthesia, the patient was placed supine. The colonoscope was inserted through the ileostomy and reached above the rectal stenosis. The zebra guide wire was inserted through the colonoscopy biopsy hole, and the zebra guide wire tip was adjusted to pass through the rectal ste
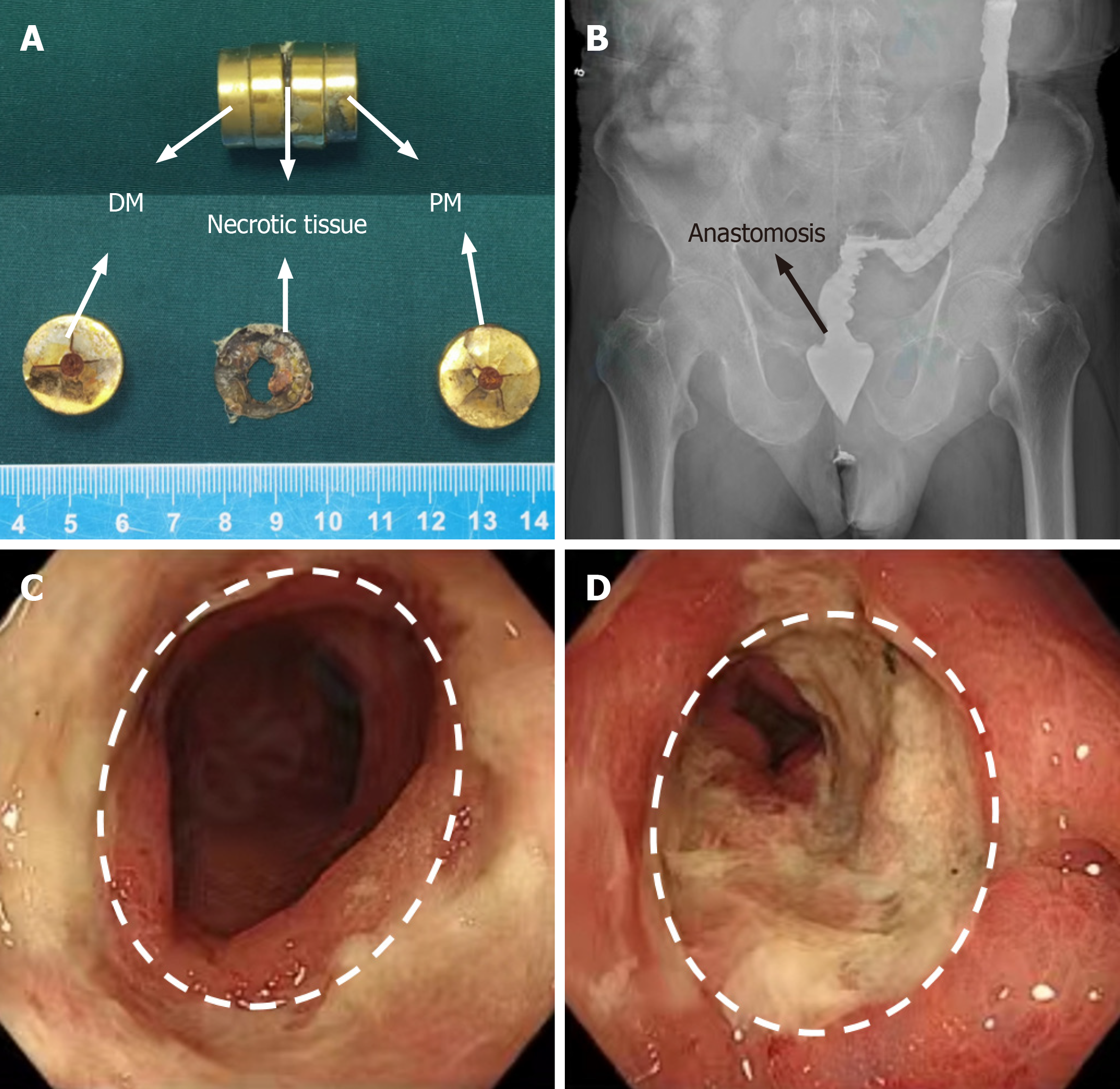
The patient recovered from anesthesia and resumed normal activities and oral intake. The patient was asked to pay attention to the discharge of the magnets. On the 11th day after surgery, the magnets were discharged through the anus, with detached necrotic tissue visible between the DMs and PMs (Figure 3A). An immediate colonography showed good patency of the lower rectum (Figure 3B). Colonoscopy showed good patency of the rectal anastomosis, and no ulcers, bleeding, or erosion at the magnetic anastomosis site (Figure 3C and D).
After discharge, the patient was asked to self-dilate with an 18-mm diameter anal dilator stick three times a day. The ileostomy closure surgery was completed one month later. The patient has been followed up for six months and has good bowel status.
MCT was first reported in 1978 for nonsuture microvascular anastomosis in experimental animals[6]. Later, this technique was used in coronary artery bypass surgery[7-9]. With further development, MCT has been used in digestive tract ana
The application of MCT in the digestive tract mainly focuses on gastrointestinal anastomosis. MCT has also been used for postoperative AS of colorectal cancer[20], but such studies have been rare, mainly due to the limited knowledge of surgeons and endoscopists about this technique. Previously, we reported the use of MCT for treating radiation-induced sigmoid stenosis with good long-term outcomes[21].
The MCT for the treatment of this patient had the following characteristics: First, this patient had an ileostomy, which can provide convenience for magnet placement. This patient had an easier procedure than those with rectal stenosis who did not have an ostomy. Second, the patient showed no response to repeated endoscopic balloon dilation, indicating a heavy scar in the stenosed area. Therefore, the magnet superposition scheme was adopted to increase the magnetic force between the DM and the PM. Third, there have been limited case reports of postoperative AS treated with MCT after rectal cancer surgery, and its long-term effect is unknown. Therefore, despite the good patency of the anastomosis after the discharge of magnets, in order to prevent restenosis, we recommended the patient to continue anal dilation.
This case indicates that MCT can be used as a new treatment method for patients with postoperative AS in whom en
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade A
Novelty: Grade A
Creativity or Innovation: Grade A
Scientific Significance: Grade A
P-Reviewer: Dimofte GM, Romania S-Editor: Chen YL L-Editor: A P-Editor: Xu ZH
| 1. | McKee R, Pricolo VE. Stapled revision of complete colorectal anastomotic obstruction. Am J Surg. 2008;195:526-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Hu C, Zhang H, Yang L, Zhao J, Cai Q, Jiang L, Meng L, Wang Z, Wen Z, Wang Y, Yu Z. Anastomotic occlusion after laparoscopic low anterior rectal resection: a rare case study and literature review. World J Surg Oncol. 2022;20:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Lee SY, Kim CH, Kim YJ, Kim HR. Anastomotic stricture after ultralow anterior resection or intersphincteric resection for very low-lying rectal cancer. Surg Endosc. 2018;32:660-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Chan RH, Lin SC, Chen PC, Lin WT, Wu CH, Lee JC, Lin BW. Management of colorectal anastomotic stricture with multidiameter balloon dilation: long-term results. Tech Coloproctol. 2020;24:1271-1276. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Kraenzler A, Maggiori L, Pittet O, Alyami MS, Prost À la Denise J, Panis Y. Anastomotic stenosis after coloanal, colorectal and ileoanal anastomosis: what is the best management? Colorectal Dis. 2017;19:O90-O96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Obora Y, Tamaki N, Matsumoto S. Nonsuture microvascular anastomosis using magnet rings: preliminary report. Surg Neurol. 1978;9:117-120. [PubMed] |
| 7. | Klima U, Maringka M, Bagaev E, Kirschner S, Haverich A. Total magnetic vascular coupling for arterial revascularization. J Thorac Cardiovasc Surg. 2004;127:602-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Klima U, MacVaugh H 3rd, Bagaev E, Maringka M, Kirschner S, Beilner J, Haverich A. Magnetic Vascular Port in minimally invasive direct coronary artery bypass grafting. Circulation. 2004;110:II55-II60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Vicol C, Eifert S, Oberhoffer M, Boekstegers P, Reichart B. Mid-term patency after magnetic coupling for distal bypass anastomosis in coronary surgery. Ann Thorac Surg. 2006;82:1452-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Zhang MM, Li CG, Xu SQ, Mao JQ, Zhang YH, Shi AH, Li Y, Lyu Y, Yan XP. Magnetic compression anastomosis for reconstruction of digestive tract after total gastrectomy in beagle model. World J Gastrointest Surg. 2023;15:1294-1303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 11. | Li GZ, Ryou M, Thompson CC, Wang J. A Preclinical Study of an Esophagojejunal Compression Anastomosis After Total Gastrectomy with Self-Forming Magnets. J Gastrointest Surg. 2023;27:1710-1712. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Ore AS, Althoff A, Kull DR, Baldwin TJ, Van Eps JL, Messaris E. Comparative early histologic healing quality of magnetic versus stapled small bowel anastomosis. Surgery. 2023;173:1060-1065. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression ostomy as new cystostomy technique in the rat: magnacystostomy. Urology. 2012;79:738-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Uygun I, Okur MH, Arayici Y, Keles A, Ozturk H, Otcu S. Magnetic compression ostomy for simple tube colostomy in rats--magnacolostomy. Adv Clin Exp Med. 2012;21:301-305. [PubMed] |
| 15. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression gastrostomy in the rat. Pediatr Surg Int. 2012;28:529-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Shlomovitz E, Copping R, Swanstrom LL. Magnetic Compression Anastomosis for Recanalization of Complete Ureteric Occlusion after Radical Cystoprostatectomy. J Vasc Interv Radiol. 2023;34:1640-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Ünal E, Çiftçi TT, Akinci D. Magnetic Compression Anastomosis of Benign Short-Segment Ureteral Obstruction. J Vasc Interv Radiol. 2024;35:398-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 18. | Gomes GF, Noda RW, Lima TMDC, Kashiwagui LY, Nakadomari TS. Magnetic compression anastomosis for the treatment of complete gastric outlet obstruction due to corrosive injury. VideoGIE. 2022;7:223-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Huberland F, Rio-Tinto R, Cauche N, Dugardeyn S, Delattre C, Sandersen C, Rocq L, van Ouytsel P, Delchambre A, Devière J, Blero D. Magnets and a self-retractable wire for endoscopic septotomies: from concept to first-in-human use. Endoscopy. 2022;54:574-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Lu G, Li J, Ren M, Ma F, Sun X, Lv Y, He S. Endoscopy-assisted magnetic compression anastomosis for rectal anastomotic atresia. Endoscopy. 2021;53:E437-E439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Zhang MM, Gao Y, Ren XY, Sha HC, Lyu Y, Dong FF, Yan XP. Magnetic compression anastomosis for sigmoid stenosis treatment: A case report. World J Gastrointest Endosc. 2023;15:745-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |