Published online May 27, 2024. doi: 10.4240/wjgs.v16.i5.1363
Revised: March 7, 2024
Accepted: April 3, 2024
Published online: May 27, 2024
Processing time: 95 Days and 2.9 Hours
A comprehensive understanding of the extrahepatic bile duct anatomy is vital to guide surgical procedures and perform endoscopic retrograde cholangiography. Anatomical irregularities within the extrahepatic bile duct may increase susceptibility to bile duct stones.
To investigate the anatomical risk factors associated with extrahepatic bile ducts in patients diagnosed with choledocholithiasis, with a specific focus on prevent
We retrospectively analyzed the medical records of 124 patients without chole
Multivariate logistic regression analysis revealed that several factors indepen
The anatomical features of the extrahepatic bile duct were directly associated with choledocholithiasis risk. Key risk factors include an enlarged diameter of the common hepatic and bile ducts, a shorter length of the common hepatic duct, and a reduced angle of the common bile duct.
Core Tip: Comprehensive understanding of the extrahepatic bile duct anatomy is imperative to guide surgical procedures and perform endoscopic retrograde cholangiography. This study aimed to investigate the anatomical risk factors associated with the extrahepatic bile ducts in patients diagnosed with choledocholithiasis, specifically focusing on preventing stone recur
- Citation: Cao Z, Zhou J, Wei L, He HY, Li J. Effect of the extrahepatic bile duct anatomy on choledocholithiasis and its clinical significance. World J Gastrointest Surg 2024; 16(5): 1363-1370
- URL: https://www.wjgnet.com/1948-9366/full/v16/i5/1363.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i5.1363
Cholelithiasis frequently leads to biliary and pancreatic complication-related hospitalizations, with approximately 622000 individuals hospitalized annually in the United States, and approximately 15% of cases are attributed to choledocholi
Anatomically, the extrahepatic bile duct includes the left and right hepatic ducts, common hepatic and bile ducts, gallbladder, and cystic duct[9]. Contributors to the risk of choledocholithiasis recurrence include specific anatomical factors of the extrahepatic bile duct, including the shape and insertion mode of the cystic duct, as well as the diameter, angle, and shape of the common bile duct[6,7,10,11].
Both endoscopic ultrasonography (EUS) and magnetic resonance cholangiopancreatography (MRCP) serve as effective diagnostic methods for choledocholithiasis. Although EUS and MRCP exhibit higher specificity, EUS is notable for its increased sensitivity in the diagnosis of choledocholithiasis[12].
However, because proficiency in EUS may not be universal among endoscopists and MRCP has good sensitivity and is noninvasive for suspected biliary tract lesions[13,14], MRCP remains the primary method for clinically diagnosing chole
This study aimed to assess the extrahepatic bile duct anatomy through MRCP examinations in patients with suspected choledocholithiasis. Additionally, we sought to explore the relationship between various anatomical characteristics of the extrahepatic bile duct and choledocholithiasis risk. The insights reported in this study are expected to provide valuable guidance for preventing stone recurrence after surgical and endoscopic lithotomy.
We collected MRCP data from individuals aged ≥ 18 years hospitalized with suspected choledocholithiasis at our medical center between January 2022 and October 2022. Exclusions were made for patients with chronic liver disease, abnormal liver function tests associated with chronic liver conditions or hemolytic anemia, known hepatobiliary diseases (e.g., cho
Patient records provided information on the following: Demographic details: Age, sex, body mass index (BMI), and history of hypertension, diabetes, and hyperlipidemia; laboratory tests: Alanine transaminase (ALT), aspartate transami
MRCP anatomical data, demographic features, and laboratory results of patients with and without choledocholithiasis were compared. Given the retrospective and nonintrusive nature of this study, our ethics committee granted approval for the exemption from obtaining written informed consent.
Statistical analyses were performed using SPSS version 25.0. Categorical data are shown as frequencies (%), and conti
From January 2022 to October 2022, a thorough assessment of 2239 suspected choledocholithiasis cases was conducted using MRCP. Following stringent exclusion criteria, 232 patients were deemed eligible for the study, including 124 without choledocholithiasis and 108 with confirmed choledocholithiasis.
In the examination of general data, hyperlipidemia, ALT, AST, ALP, GGT, and DBil were associated with the occur
| Variable | Without CBD stones (n = 124) | With CBD stones (n = 108) | P value |
| Age (yr) | 50.88 ± 15.60 | 55.06 ± 18.00 | 0.060 |
| Sex, n (%) | 0.575 | ||
| Female | 70 (56.45) | 57 (52.78) | |
| Male | 54 (43.55) | 51 (47.22) | |
| BMI (kg/m2) | 23.79 ± 3.78 | 23.62 ± 3.71 | 0.732 |
| Hypertension, n (%) | 19 (15.32) | 9 (8.33) | 0.103 |
| Diabetes, n (%) | 12 (9.68) | 5 (4.63) | 0.141 |
| Hyperlipidemia, n (%) | 23 (18.55) | 6 (5.56) | 0.003 |
| ALT (U/L) | 24.50 (16.00, 45.25) | 100.45 (32.00, 216.25) | < 0.001 |
| AST (U/L) | 24.00 (19.00, 39.25) | 53.00 (26.00, 130.75) | < 0.001 |
| ALP (U/L) | 84.50 (70.00, 116.50) | 160.80 (104.50, 275.25) | < 0.001 |
| GGT (U/L) | 43.00 (23.00, 118.25) | 251.50 (121.50, 576.50) | < 0.001 |
| DBil (µmol/L) | 4.25 (2.98, 6.60) | 10.00 (4.90, 29.48) | < 0.001 |
| IBil (µmol/L) | 9.35 (6.47, 13.38) | 10.70 (7.50, 15.20) | 0.167 |
| Variable | Without CBD stones (n = 124) | With CBD stones (n = 108) | P value |
| CHD diameter (mm) | 4.10 (3.20, 6.03) | 9.40 (6.88, 12.50) | < 0.001 |
| CD diameter (mm) | 3.10 (2.40, 4.93) | 5.85 (3.70, 8.50) | < 0.001 |
| CBD diameter (mm) | 5.00 (3.80, 6.70) | 10.35 (8.10, 13.00) | < 0.001 |
| CHD length (mm) | 20.51 ± 8.88 | 25.12 ± 12.58 | 0.002 |
| CD length (mm) | 26.10 ± 12.76 | 35.83 ± 21.69 | < 0.001 |
| CBD length (mm) | 50.46 ± 12.87 | 52.65 ± 13.84 | 0.212 |
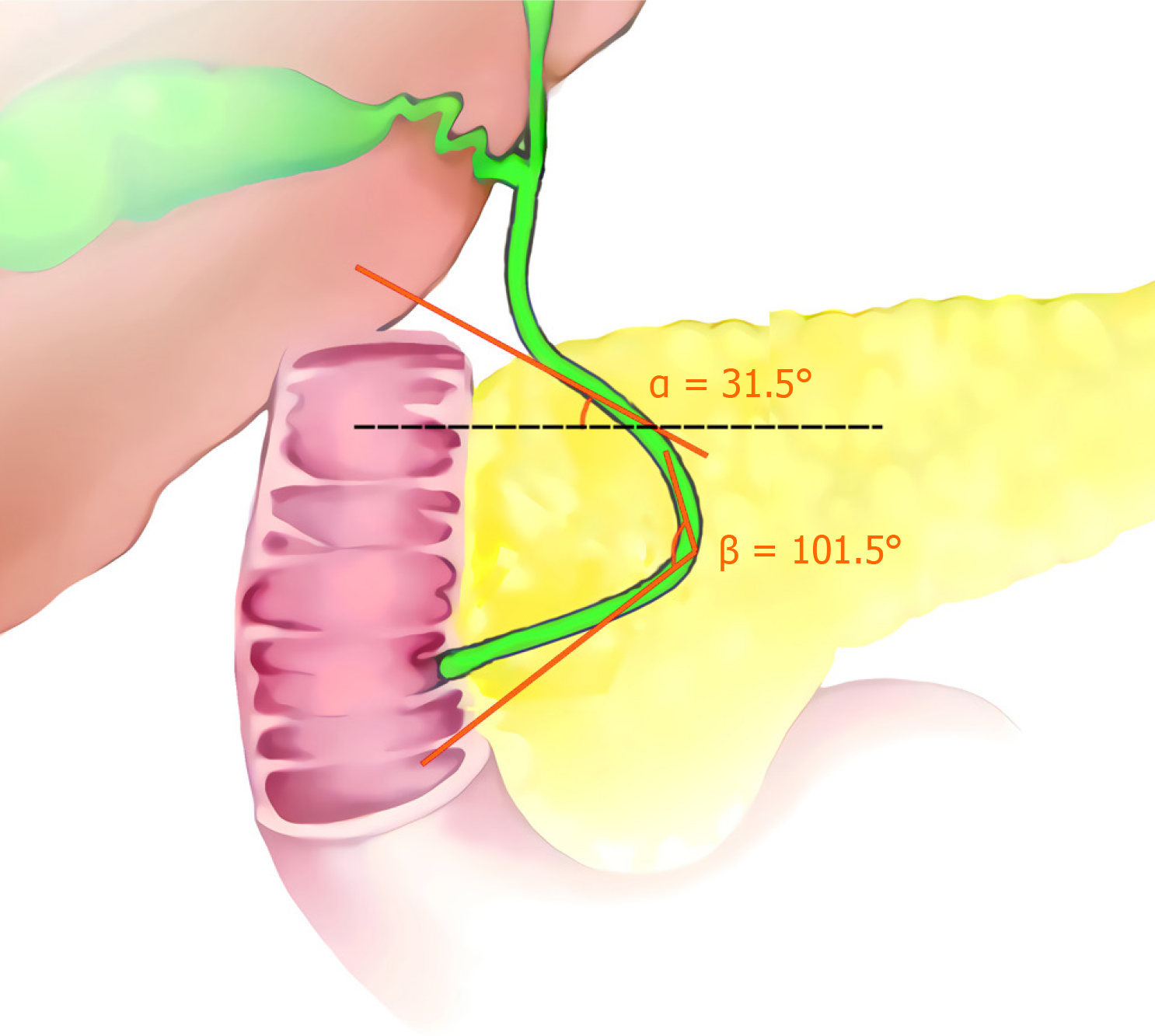
| CBD angulation (°) | 138.94 ± 19.19 | 112.79 ± 19.12 | < 0.001 |
| Oblique angle of the CBD (°) | 60.12 ± 18.54 | 47.08 ± 19.85 | < 0.001 |
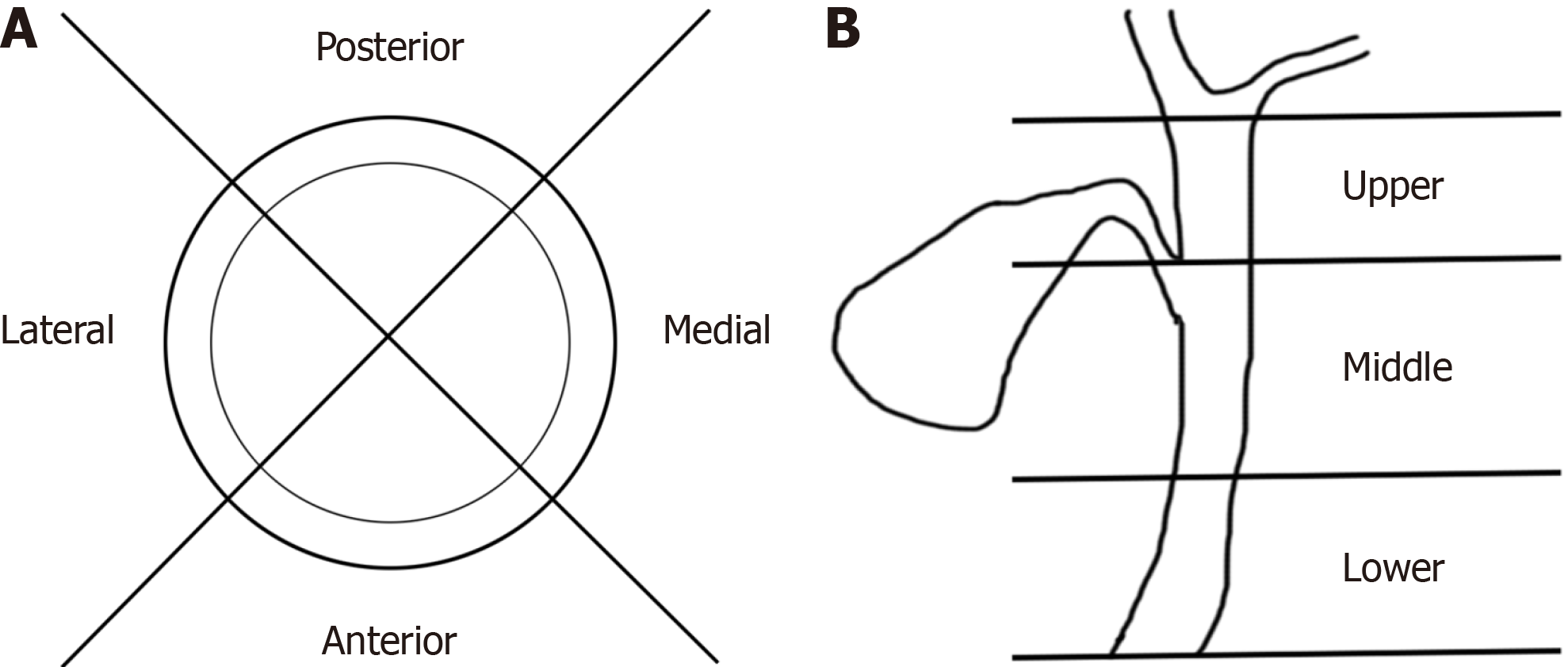
| Insertion position of CD, n (%) | |||
| Anterior | 15 (12.10) | 21 (19.44) | 0.123 |
| Posterior | 8 (6.45) | 33 (30.56) | < 0.001 |
| Lateral | 95 (76.61) | 50 (46.30) | < 0.001 |
| Medial | 6 (4.84) | 4 (3.70) | 0.920 |
| Upper | 85 (68.55) | 57 (52.78) | 0.014 |
| Middle | 38 (30.65) | 48 (44.44) | 0.030 |
| Lower | 1 (0.81) | 3 (2.78) | 0.519 |
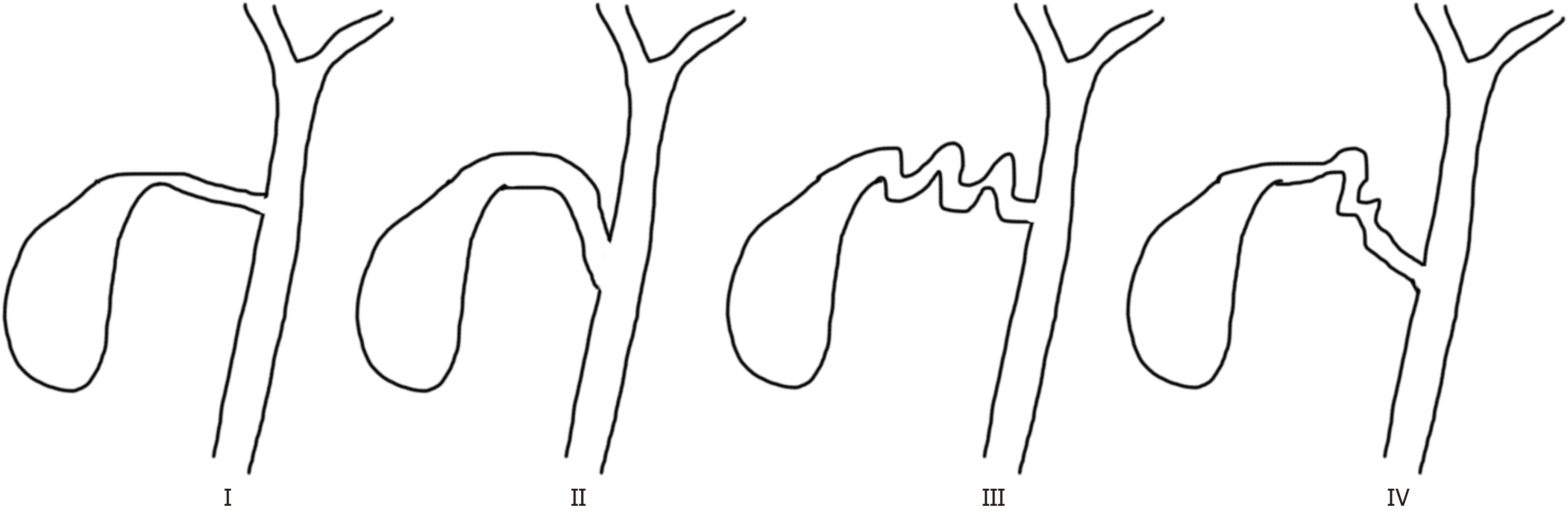
| Route of CD, n (%) | |||
| Linear type | 15 (12.10) | 8 (7.41) | 0.233 |
| Curved type | 92 (74.19) | 80 (74.07) | 0.983 |
| Spiral type | 8 (6.45) | 14 (12.96) | 0.091 |
| Complex type | 9 (7.26) | 6 (5.56) | 0.599 |
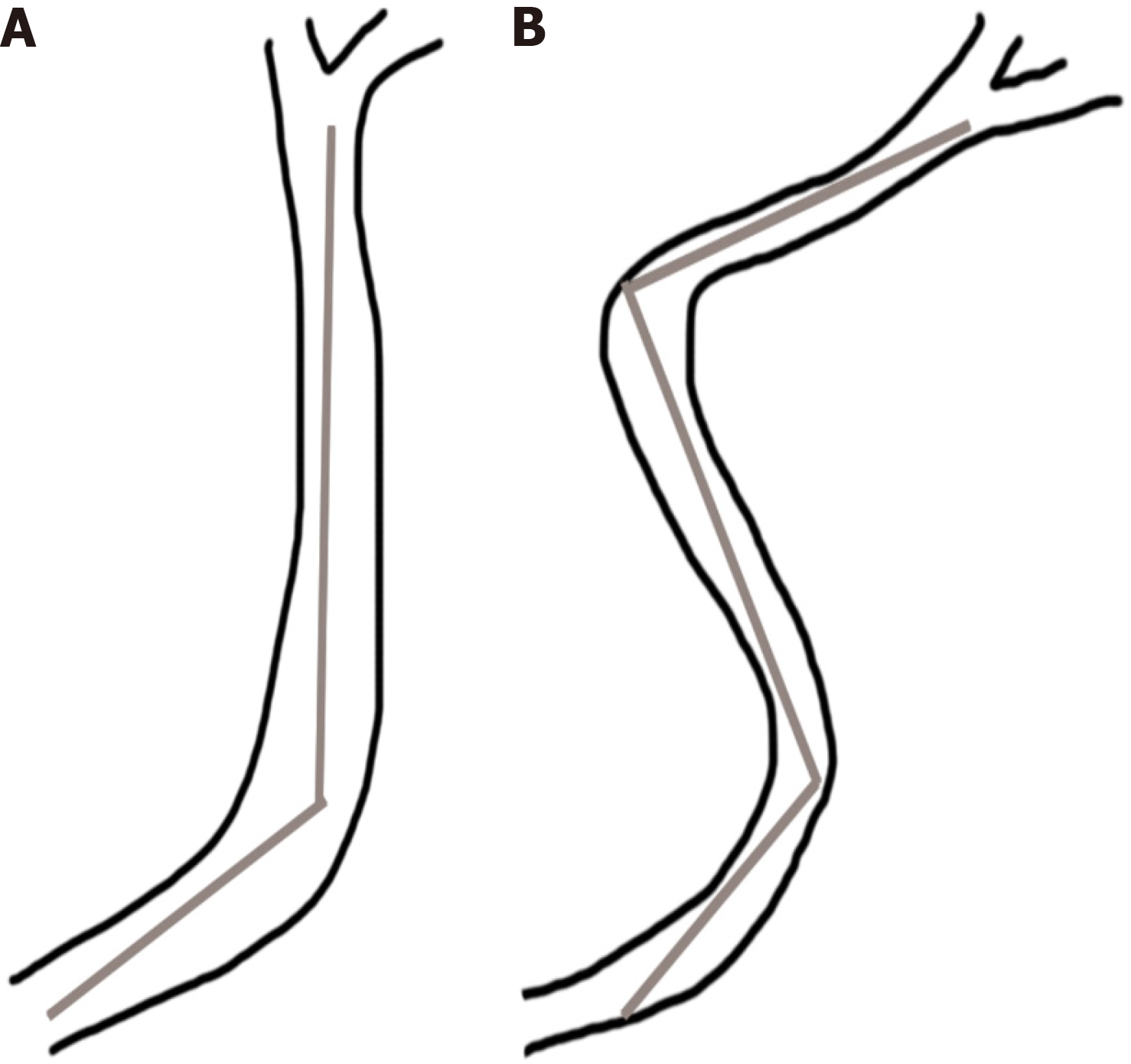
| Route of CBD, n (%) | |||
| Polyline type | 118 (95.16) | 98 (90.74) | 0.185 |
| S type | 6 (4.84) | 10 (9.26) | 0.185 |
Independent risk factors for choledocholithiasis, including the diameter [adjusted odds ratio (aOR) = 1.43, 95% confidence interval (CI): 1.07-1.92, adjusted P value = 0.016] and length (aOR = 0.92, 95%CI: 0.84-0.99, adjusted P value = 0.034) of the common hepatic duct and diameter (aOR = 1.68, 95%CI: 1.27-2.23, adjusted P value < 0.001) and angulation (aOR = 0.92, 95%CI: 0.89-0.95, adjusted P value < 0.001) of the common bile duct, were identified using multivariate logistic regression (Table 3).
| Variable | aOR (95%CI) | Adjusted P value |
| CHD diameter | 1.43 (1.07-1.92) | 0.016 |
| CBD diameter | 1.68 (1.27-2.23) | < 0.001 |
| CHD length | 0.92 (0.84-0.99) | 0.034 |
| CBD angulation | 0.92 (0.89-0.95) | < 0.001 |
In this study, we explored the impact of various risk factors on choledocholithiasis using univariate and multivariate logistic regression analyses.
Contrary to the common consideration of age as a predictor in other studies[15,16], our research did not establish statistical significance in this aspect. However, Govindan et al[17] suggested a potential correlation between age and common bile duct diameter, with an annual expansion rate of 0.07 mm. Nevertheless, the designation of age as an in
Our findings demonstrate no significant variations in the course of the cystic duct. However, Deenitchin et al[10] reported a high incidence of gallstones associated with cystic duct malformations. Currently, a comprehensive under
In contrast to previous studies[6], our multivariate logistic regression analysis indicated no significant differences in the position, direction, or route of cystic duct insertion. This suggests that cystic duct insertion characteristics may not be a substantial risk factor for choledocholithiasis. Nevertheless, we hypothesize that the development of primary and se
We identified several significant anatomical factors of the extrahepatic bile duct. Additionally, we assessed the com
Regarding diameters of the common hepatic and bile duct, diameter of the common hepatic duct increased with dilation of the common bile duct. Additionally, gallbladder dilation through the cystic duct can alleviate pressure and reduce dilatation.
No statistically significant relationship was found between low cystic duct insertion and choledocholithiasis risk. However, as the common hepatic duct length increased, choledocholithiasis risk decreased, which is consistent with the findings of Kao et al[18]. Reduced choledocholithiasis risk has been reported with an increased choledochal angle, con
While ERCP and endoscopic sphincterotomy are widely used to treat choledocholithiasis, the post-treatment recur
The primary limitation of our study lies in the single-time-point assessment of extrahepatic bile duct anatomical changes without long-term patient follow-up. Consequently, we could not ascertain the temporal trends of these changes or their correlations with underlying diseases. Additionally, our two-dimensional measurement method for the extra
In conclusion, individuals with a broader diameter of the extrahepatic bile duct, shorter length of the common hepatic duct, and smaller angle of the common bile duct are at an elevated risk of developing choledocholithiasis. Moreover, these patients are more prone to stone recurrence after surgical or endoscopic lithotomy. Thus, vigilance regarding the potential for stone recurrence is crucial in managing such cases.
We thank all medical staff and technicians of digestive endoscopy center and imaging center for their participation in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Akbulut S, Türkiye; Farooq U, United States S-Editor: Yan JP L-Editor: A P-Editor: Xu ZH
| 1. | Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology. 2009;136:376-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 418] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 2. | Lem SG, Wang SJ, Tsai CY, Sun MS. The efficacy and accuracy of endoscopic ultrasound for detecting common bile duct stones in intermediate to high‐risk patients with non‐diagnostic CT or MRCP. dv in Digest Med. 2022;9:31-37. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Fujita N, Yasuda I, Endo I, Isayama H, Iwashita T, Ueki T, Uemura K, Umezawa A, Katanuma A, Katayose Y, Suzuki Y, Shoda J, Tsuyuguchi T, Wakai T, Inui K, Unno M, Takeyama Y, Itoi T, Koike K, Mochida S. Evidence-based clinical practice guidelines for cholelithiasis 2021. J Gastroenterol. 2023;58:801-833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 51] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 4. | Chen L, Yang H, Li H, He C, Yang L, Lv G. Insights into modifiable risk factors of cholelithiasis: A Mendelian randomization study. Hepatology. 2022;75:785-796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 170] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 5. | Yuan S, Gill D, Giovannucci EL, Larsson SC. Obesity, Type 2 Diabetes, Lifestyle Factors, and Risk of Gallstone Disease: A Mendelian Randomization Investigation. Clin Gastroenterol Hepatol. 2022;20:e529-e537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 89] [Article Influence: 29.7] [Reference Citation Analysis (1)] |
| 6. | Choi SJ, Yoon JH, Koh DH, Lee HL, Jun DW, Choi HS. Low insertion of cystic duct increases risk for common bile duct stone recurrence. Surg Endosc. 2022;36:2786-2792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 7. | Ji X, Yang Z, Ma SR, Jia W, Zhao Q, Xu L, Kan Y, Cao Y, Wang Y, Fan BJ. New common bile duct morphological subtypes: Risk predictors of common bile duct stone recurrence. World J Gastrointest Surg. 2022;14:236-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Ji X, Jia W, Zhao Q, Wang Y, Ma SR, Xu L, Kan Y, Cao Y, Fan BJ, Yang Z. Common bile duct morphology is associated with recurrence of common bile duct stones in Billroth II anatomy patients. World J Clin Cases. 2021;9:7671-7681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Ober EA, Lemaigre FP. Development of the liver: Insights into organ and tissue morphogenesis. J Hepatol. 2018;68:1049-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 149] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 10. | Deenitchin GP, Yoshida J, Chijiiwa K, Tanaka M. Complex cystic duct is associated with cholelithiasis. HPB Surg. 1998;11:33-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Strnad P, von Figura G, Gruss R, Jareis KM, Stiehl A, Kulaksiz H. Oblique bile duct predisposes to the recurrence of bile duct stones. PLoS One. 2013;8:e54601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Meeralam Y, Al-Shammari K, Yaghoobi M. Diagnostic accuracy of EUS compared with MRCP in detecting choledocholithiasis: a meta-analysis of diagnostic test accuracy in head-to-head studies. Gastrointest Endosc. 2017;86:986-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 13. | ASGE Standards of Practice Committee; Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89:1075-1105.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 335] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 14. | Wani S, Keswani R, Hall M, Han S, Ali MA, Brauer B, Carlin L, Chak A, Collins D, Cote GA, Diehl DL, DiMaio CJ, Dries A, El-Hajj I, Ellert S, Fairley K, Faulx A, Fujii-Lau L, Gaddam S, Gan SI, Gaspar JP, Gautamy C, Gordon S, Harris C, Hyder S, Jones R, Kim S, Komanduri S, Law R, Lee L, Mounzer R, Mullady D, Muthusamy VR, Olyaee M, Pfau P, Saligram S, Piraka C, Rastogi A, Rosenkranz L, Rzouq F, Saxena A, Shah RJ, Simon VC, Small A, Sreenarasimhaiah J, Walker A, Wang AY, Watson RR, Wilson RH, Yachimski P, Yang D, Edmundowicz S, Early DS. A Prospective Multicenter Study Evaluating Learning Curves and Competence in Endoscopic Ultrasound and Endoscopic Retrograde Cholangiopancreatography Among Advanced Endoscopy Trainees: The Rapid Assessment of Trainee Endoscopy Skills Study. Clin Gastroenterol Hepatol. 2017;15:1758-1767.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 15. | Kadah A, Khoury T, Mahamid M, Assy N, Sbeit W. Predicting common bile duct stones by non-invasive parameters. Hepatobiliary Pancreat Dis Int. 2020;19:266-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Khoury T, Kadah A, Mari A, Kalisky I, Katz L, Mahamid M, Sbeit W. A validated score predicting common bile duct stone in patients hospitalized with acute calculus cholecystitis: a multi-center retrospective study. Surg Endosc. 2021;35:3709-3715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Govindan S, Tamrat NE, Liu ZJ. Effect of Ageing on the Common Bile Duct Diameter. Dig Surg. 2021;38:368-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Kao JT, Kuo CM, Chiu YC, Changchien CS, Kuo CH. Congenital anomaly of low insertion of cystic duct: endoscopic retrograde cholangiopancreatography findings and clinical significance. J Clin Gastroenterol. 2011;45:626-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Ryu S, Jo IH, Kim S, Kim YJ, Chung WC. Clinical Impact of Common Bile Duct Angulation on the Recurrence of Common Bile Duct Stone: A Meta-analysis and Review. Korean J Gastroenterol. 2020;76:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Han SJ, Chang JH, Gweon TG, Kim TH, Kim HK, Kim CW. Analysis of symptomatic recurrences of common bile ducts stones after endoscopic removal: Factors related to early or multiple recurrences. Medicine (Baltimore). 2022;101:e28671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Kim B, Park JS, Bae J, Hwang N. Bile Microbiota in Patients with Pigment Common Bile Duct Stones. J Korean Med Sci. 2021;36:e94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Lyu Z, Yu T, Zhang L, Xu X, Zhang Y, Li J, Li Z, Zhang W, Hou S. Analysis of the relationship between bile duct and duodenal microbiota reveals that potential dysbacteriosis is the main cause of primary common bile duct stones. Synth Syst Biotechnol. 2021;6:414-428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Wu Y, Xu CJ, Xu SF. Advances in Risk Factors for Recurrence of Common Bile Duct Stones. Int J Med Sci. 2021;18:1067-1074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |