Published online May 27, 2024. doi: 10.4240/wjgs.v16.i5.1320
Revised: April 2, 2024
Accepted: April 9, 2024
Published online: May 27, 2024
Processing time: 94 Days and 2.3 Hours
Surgery for obese patients carries a higher risk of anesthesia complications compared with surgery for nonobese patients. Thus, a safe and effective ane
To compared the effectiveness and safety of remimazolam besylate versus dex
The study cohort included 60 obese patients undergoing gastrointestinal surgery between July 2021 and April 2023, comprising 30 patients who received DEX intervention (control group) and 30 patients who received remimazolam besylate intervention (research group). Heart rate (HR), respiratory rate (RR), mean arterial pressure (MAP), blood oxygen saturation (SpO2), safety (nausea and vomiting, bradycardia, hypotension, and apnea), anesthesia and examination indices [induction time, anesthesia recovery time, and postanesthesia care unit (PACU) discharge time], sedation effect (Ramsay Sedation Scale), and postoperative pain visual analog scale were comparatively analyzed before anesthesia (T0), during anesthesia (T1), and after anesthesia (T2).
At T1, the research group showed significantly smaller changes in HR, RR, MAP, and SpO2 than the control group, with a significantly lower adverse reaction rate and shorter induction, anesthesia recovery, and PACU discharge times. Addi
Remimazolam besylate was significantly more effective than DEX in gastrointestinal surgery in obese patients and had a higher safety profile and value in clinical promotion.
Core Tip: This study primarily compared the effectiveness and safety of remimazolam besylate versus dexmedetomidine (DEX) in gastrointestinal surgery for obese patients. Our findings confirmed that remimazolam besylate was significantly more effective than DEX in gastrointestinal surgery in obese patients, with a high safety profile and value in clinical promotion, thereby providing a reliable clinical reference for anesthesia management optimization in gastrointestinal surgery for obese patients.
- Citation: Deng YF, Jiang XR, Feng ZG. Comparative observation of the effectiveness and safety of remimazolam besylate versus dexmedetomidine in gastrointestinal surgery in obese patients. World J Gastrointest Surg 2024; 16(5): 1320-1327
- URL: https://www.wjgnet.com/1948-9366/full/v16/i5/1320.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i5.1320
Obesity is a disease of abnormal or excessive accumulation of body fat and is influenced by the interaction of dietary, genetic, cultural, and socioeconomic factors[1,2]. The risk of obesity has tripled over the past 3 decades, with a prevalence as high as 28.3% and 36.5% in men and women, respectively[3]. Obesity not only impairs patients’ physical health but also increases the risk of complications, such as hypertension, diabetes, coronary artery disease, and cancer[4,5]. Current surgical treatments for obesity include gastric bypass, sleeve gastrectomy, adjustable gastric banding, and duodenal-jejunal bypass, but these all carry a higher risk of anesthesia complications compared with nonobese patients[6-9]. There
Dexmedetomidine (DEX), a central alpha-2 adrenergic agonist with analgesic, sedative, and antisympathetic effects, is a common clinical anesthetic[10] used in cardiac surgery, colorectal cancer surgery, and joint replacement in elderly patients. To a certain extent, it prevents postoperative delirium and improves the quality of arousal in patients under general anesthesia[11]. Zhang et al[12] reported that the use of DEX during bariatric surgery alleviated postoperative pain, thereby promoting postoperative rehabilitation. DEX also has the advantage of not causing respiratory depression, but it may cause adverse hemodynamic events, such as hypertension, hypotension, and bradycardia[13,14].
Remimazolam besylate is a novel benzodiazepine (BDZ) with faster onset and metabolism than remimazolam[15]. Its narcotic effect stems from its action on central γ-aminobutyric acid type A receptors, leading to the opening of channels and subsequent acceleration of chloride ion influx, which hyperpolarizes the nerve membrane and effectively inhibits neuronal activity[16]. Xu et al[17] reported that remimazolam besylate also had the advantages of a quick onset, fast recovery, high compatibility, safety, and comfortable and painless anesthesia in plastic surgery.
There are few comparative observational studies on the effectiveness and safety of remimazolam besylate and DEX in obese patients undergoing gastrointestinal surgery. Thus, this study aimed to conduct a more in-depth analysis of this aspect to contribute to anesthesia optimization in such patients.
The study cohort comprised 60 obese patients undergoing gastrointestinal surgery at Xiangtan Central Hospital between July 2021 and April 2023, including 30 cases receiving DEX intervention (control group, Con) and 30 cases receiving remimazolam besylate intervention (research group, Res).
Confirmed obese patients with a body mass index (BMI) > 28 kg/m2, no contraindications for gastrointestinal surgery, American Society of Anesthesiologists (ASA) classification I or II, good cardiopulmonary function, no allergies to narcotic drugs, no intraoperative awareness, and intact medical records were included in our study.
The exclusion criteria were recent intermittent use of BDZs or opioids, preoperative diagnosis of difficult airway (Mallampati grade ≥ III) or sleep apnea syndrome, severe hypertension or hypotension, hepatorenal insufficiency, long-term use of sedative hypnotics, psychiatric disorders, and inability to communicate due to neuromuscular disorders.
Upper-limb venous access was established in all patients, and invasive blood pressure monitoring was performed, as well as monitoring of blood oxygen saturation (SpO2), cardiac function via continuous electrocardiography, and the bispectral (BIS) index.
In the Con group, anesthesia was induced by DEX infusion at a dose of 0.5-1.0 μg/kg for 10-15 min and was maintained by continuous pump infusion at 0.2-0.7 μg/kg/h, with the BIS index kept at 45-60. Opioid analgesics and muscle relaxants were also used.
In the Res group, continuous pumping was used to induce anesthesia with remimazolam besylate at a rate of 6 mg/kg/h for ≤ 3 min, and anesthesia was maintained at 0.2-1.0 mg/kg/h. If the depth of anesthesia became insufficient, 12 mg/kg/h was added for 1 min. Opioid analgesics and muscle relaxants were also used during anesthesia induction.
Patients’ vital signs were monitored before anesthesia (T0), during anesthesia (T1), and after anesthesia (T2), including heart rate (HR), respiratory rate (RR), mean arterial pressure (MAP), and SpO2. We also observed and recorded the incidence of postoperative adverse events (nausea and vomiting, bradycardia, hypotension, and apnea) and calculated the incidence rate. Anesthesia indices, including anesthesia induction, anesthesia recovery, and postanesthesia care unit (PACU) discharge times, were also compared. The sedation effect was scored according to the Ramsay Sedation Scale (1, agitated or restless; 2, cooperative and tranquil; 3, asleep and responding to commands; 4, asleep but can be aroused; 5, sluggish response to an auditory stimulus; 6, deep sleep and no response to an auditory stimulus). Pain severity was assessed at 2 and 12 h after surgery using a visual analog scale (VAS) ranging from 0-10, with the score directly proportional to the degree of pain.
SPSS 24.0 software was used for statistical analysis of the data, and statistical significance was set at P < 0.05. Age, BMI, and other measurement data were represented as mean ± SD. Independent sample t-tests were performed to identify between-group differences, and paired t-tests were used to determine differences between two time points. Sex, ASA classification, the incidence of adverse events, and other categorical variables were expressed by numbers and percentages, and intergroup comparisons were conducted using χ2 tests.
There were no statistically significant differences between the Res and the Con groups in terms of age, sex, BMI, ASA classification, and educational level (P > 0.05; Table 1).
| Factors | Con (n = 30) | Res (n = 30) | χ2 or t-test result | P value |
| Age (yr) | 38.13 ± 6.05 | 39.38 ± 6.72 | 0.757 | 0.452 |
| Sex (male/female) | 13/17 | 14/16 | 0.067 | 0.795 |
| BMI (kg/m2) | 32.05 ± 2.80 | 32.05 ± 2.80 | 0.673 | 0.504 |
| ASA classification (I/II) | 20/10 | 17/13 | 0.635 | 0.426 |
| Educational level (below high school/high school and above) | 22/8 | 17/13 | 1.832 | 0.176 |
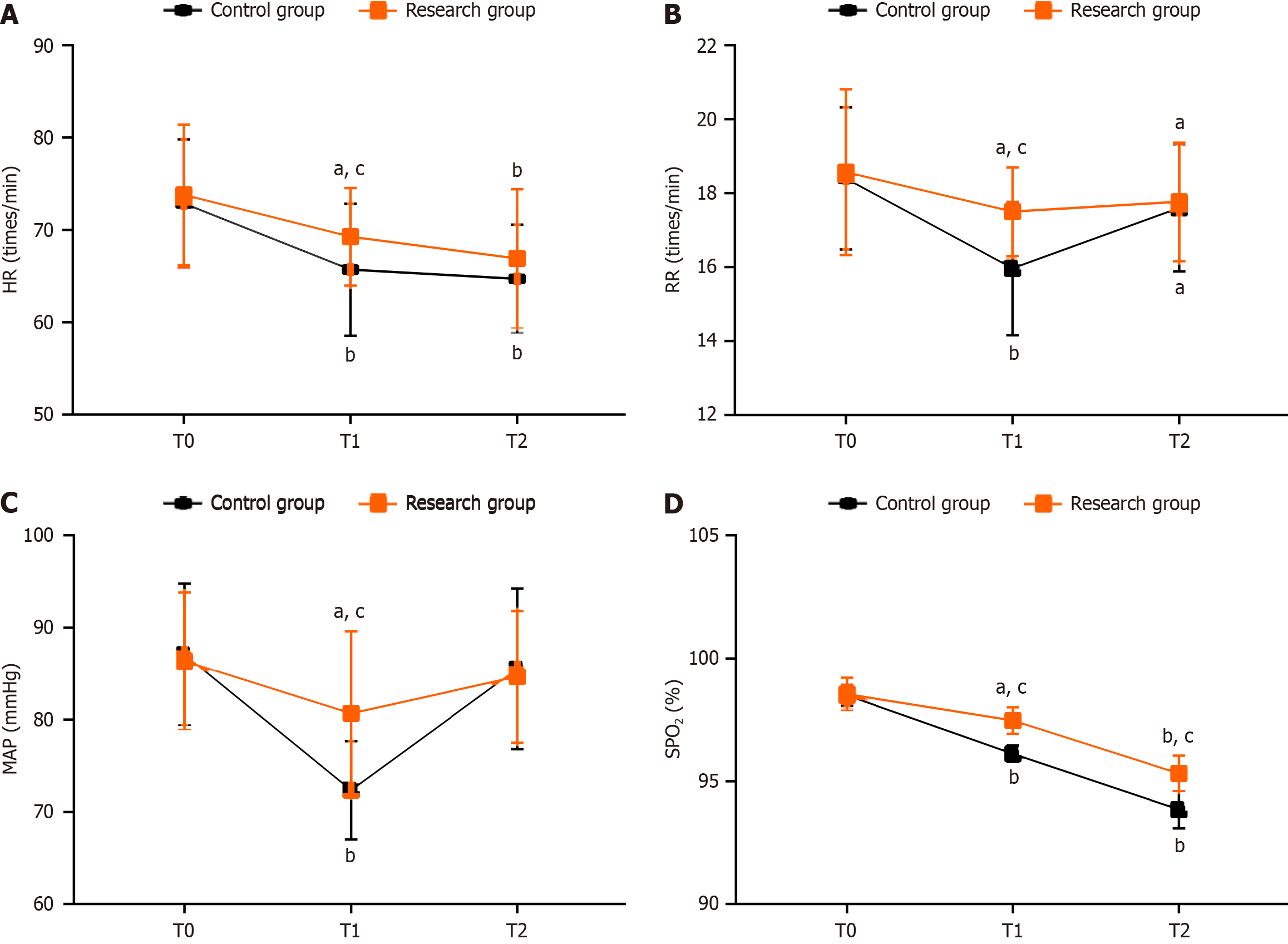
Although there were no marked differences in HR, RR, MAP, and SpO2 between the Res and the Con groups at T0 (P > 0.05), they all decreased at T1 to varying degrees (P < 0.05), with even smaller changes in the Res group (P < 0.05). At T2, the RR and MAP of both groups increased to varying degrees, but these were not significant compared with T0 or intergroup differences (P > 0.05). At T2, HR and SpO2 showed further decreases (P < 0.05), with smaller reductions in the Res group but no evident intergroup differences (P > 0.05; Figure 1).
The incidence of postoperative complications (nausea and vomiting, bradycardia, hypotension, and apnea) in the Res and Con groups were 13.33% and 36.67%, respectively, and the difference between them was statistically significant (P < 0.05; Table 2).
| Adverse event | Con (n = 30) | Res (n = 30) | χ2 | P value |
| Nausea and vomiting | 2 (6.67) | 0 (0.00) | ||
| Bradycardia | 4 (13.33) | 2 (6.67) | ||
| Hypotension | 3 (10.00) | 1 (3.33) | ||
| Apnea | 2 (6.67) | 1 (3.33) | ||
| Total | 11 (36.67) | 4 (13.33) | 4.356 | 0.037 |
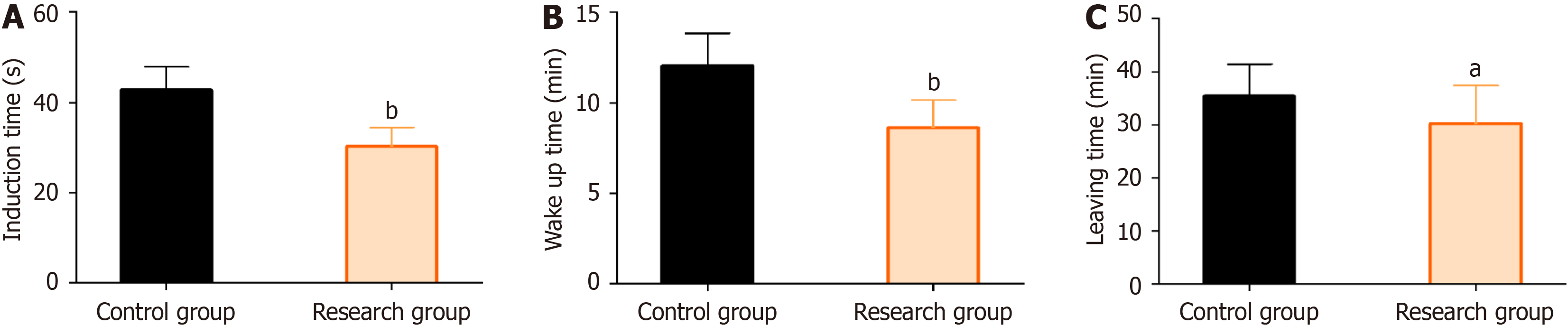
Patients in the Res group had shorter anesthesia induction, anesthesia recovery, and PACU discharge times compared with patients in the Con group (P < 0.05; Figure 2).
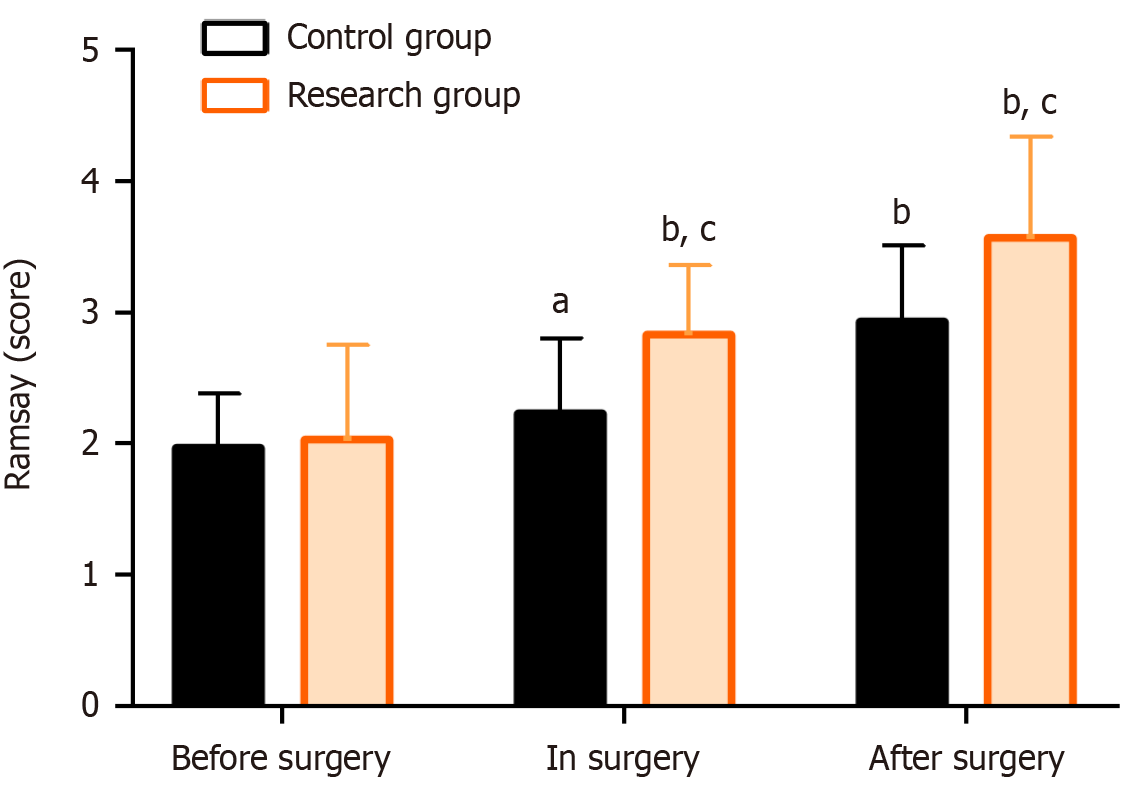
Both intraoperative and postoperative Ramsay scores were significantly increased in both groups compared with the preoperative score, with those in the Res group being significantly higher compared with the Con group (P < 0.05; Figure 3).
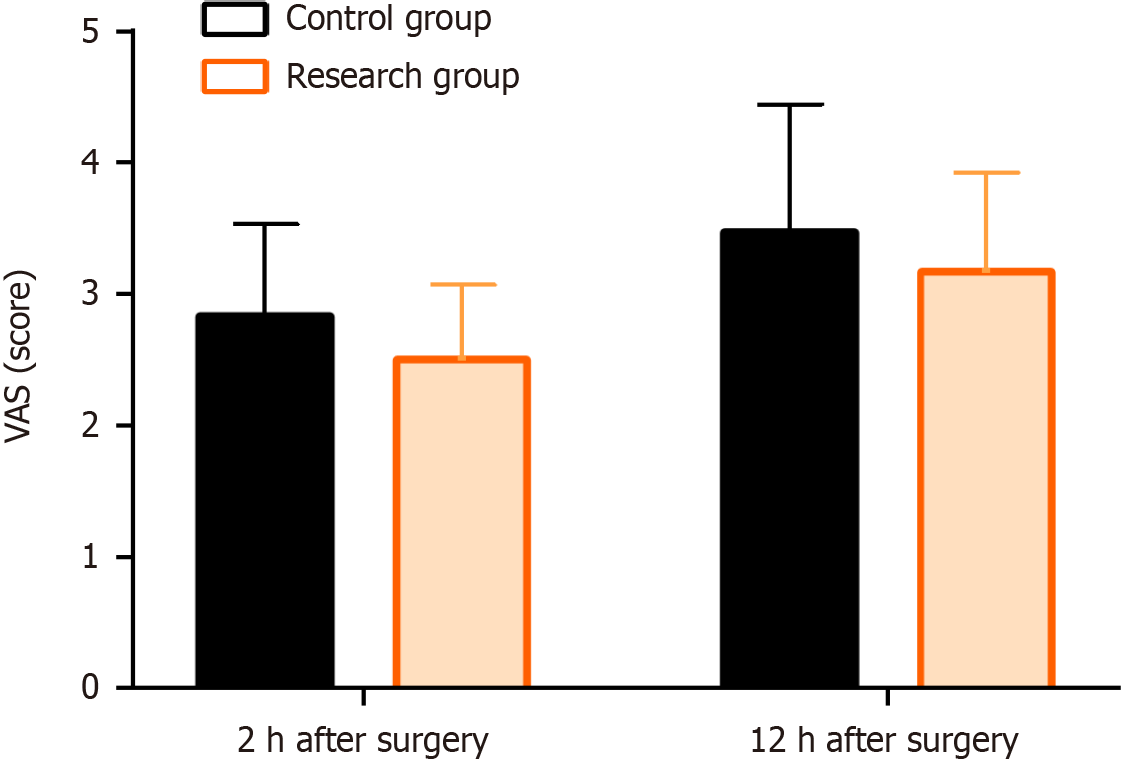
The VAS scores of the Res and Con groups were similar at 2 and 12 h after surgery (P > 0.05; Figure 4).
This comparative observational analysis studied 60 obese patients who underwent gastrointestinal surgery. Of them, 30 underwent anesthesia with DEX (Con group), and 30 underwent anesthesia with remimazolam besylate (Res group). Remimazolam besylate was clearly advantageous over DEX in obese patients undergoing gastrointestinal surgery.
To ensure good anesthesia performance, it is important to maintain hemodynamic stability by avoiding overexcitation and inhibition of sympathetic and parasympathetic nerves[18-20]. Our analysis of the patients’ vital signs (HR, RR, MAP, and SpO2) revealed smaller fluctuations of these indices in the Res group compared with the Con group at T1. Furthermore, the only significant intergroup difference at T2 was SpO2, suggesting that remimazolam besylate anesthetization exerted relatively little influence on patients’ vital signs and maintained hemodynamic stability more effectively than DEX. Anesthesia using remimazolam besylate was reported to exert a minimal effect on the circulatory system and contribute to slight HR and blood pressure fluctuations, with a certain stabilizing effect on hemodynamics[21], which agrees with our research findings. This may be because remimazolam besylate acts on γ-aminobutyric acid receptors, with rapid onset of action, fast counteraction, short half-life, high clearance rate, easy and rapid metabolism, and little variation in pharmacodynamic properties among individuals, making it more conducive to the recovery of hemodynamic stability[22]. In our study, the incidence of adverse effects (nausea and vomiting, bradycardia, hypotension, apnea, and other events) in the Res group was significantly lower than the incidence of adverse effects in the Con group, indicating a reduced risk of postoperative adverse events in obese patients undergoing gastrointestinal surgery under anesthesia with remimazolam besylate. Remimazolam besylate is metabolized by abundant plasma and nonspecific tissue esterases, independent of arbitrary organ metabolism and without significant negative effects on hemodynamics, which partially explains its high safety profile[23]. Liu et al[24] reported that remimazolam besylate exhibited a favorable safety profile in elderly outpatients undergoing colonoscopy, correlating with our research results. Yi et al[25] reported a relatively lower risk of bradycardia, nausea, vomiting, and chills in patients undergoing endoscopic retrograde cholangiopancreatography under anesthesia with remimazolam besylate, similar to our observations. Furthermore, De Cassai et al[26] pointed out that DEX caused lower blood pressure and HR after endotracheal intubation in adult patients, and these symptoms are closely related to hypotension and bradycardia, consistent with our findings. Additionally, the induction, anesthesia recovery, and PACU discharge times were significantly shorter in the Res group compared with the Con group, indicating that remimazolam besylate had a better anesthetic effect in obese patients undergoing gastrointestinal surgery. In terms of sedation effects, the Ramsay Sedation Scale scores were markedly high intra- and postoperatively in the Res group versus in the Con group, suggesting that the significant sedative effect of remimazolam besylate was better than DEX in obese patients undergoing gastrointestinal surgery. Deng et al[27] reported that remimazolam besylate used in nonintubated elderly patients after orthopedic surgery achieved sedation within the target range faster and for a longer duration compared with DEX, which supports our findings. This may be due to the readily metabolized ester composition of remimazolam besylate and its predictable pharmacokinetic and dose-dependent pharmacodynamic properties, which allow for rapid and deeper sedation shortly after injection[28,29]. Finally, the VAS scores between the two groups were comparable at 2 and 12 h after surgery, indicating that remimazolam besylate also exerted a considerable analgesic effect in obese patients undergoing gastrointestinal surgery. One study reported that remimazolam besylate was less likely to cause injection-related pain because of its water solubility[30].
This study had several limitations that require further consideration and improvement. First, the risk factors affecting the safety of obese patients undergoing gastrointestinal surgery were not thoroughly analyzed and discussed, and supplementing this analysis would help to avoid the occurrence of adverse events. Second, the sample size was limited, and potential biases or confounding factors may have affected our findings. If the study were to be extended to multiple centers and the sample size increased, the accuracy of the research results would be improved to some extent. Finally, to further enhance the understanding and management of narcotic drug regimens, it would be helpful to perform relevant animal experiments to explore the underlying mechanisms of anesthesia.
In summary, remimazolam besylate is more advantageous than DEX in the clinical application of gastrointestinal surgery in obese patients, which is reflected in its high safety profile, excellent anesthetic, sedative, and analgesic effects, and no significant impact on patients’ vital signs, and it is deserving of clinical promotion. Additionally, our findings provide a new optimized choice and a reliable clinical reference for the anesthesia management of gastrointestinal surgery in obese patients while shedding new light on current anesthesia guidelines.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade B, Grade C
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade B
P-Reviewer: Chen KT, United States; Reyna-Jeldes M, Chile S-Editor: Qu XL L-Editor: A P-Editor: Zheng XM
| 1. | Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;2014:CD003641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 497] [Cited by in RCA: 675] [Article Influence: 61.4] [Reference Citation Analysis (1)] |
| 2. | Saliba K, Cuschieri S. Amidst the COVID-19 pandemic childhood obesity is still an epidemic-spotlight on obesity's multifactorial determinants. Health Sci Rev (Oxf). 2021;1:100006. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Berghöfer A, Pischon T, Reinhold T, Apovian CM, Sharma AM, Willich SN. Obesity prevalence from a European perspective: a systematic review. BMC Public Health. 2008;8:200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 433] [Cited by in RCA: 448] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 4. | Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, Lear SA, Ndumele CE, Neeland IJ, Sanders P, St-Onge MP; American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;143:e984-e1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1107] [Cited by in RCA: 1588] [Article Influence: 397.0] [Reference Citation Analysis (0)] |
| 5. | Flora GD, Nayak MK. A Brief Review of Cardiovascular Diseases, Associated Risk Factors and Current Treatment Regimes. Curr Pharm Des. 2019;25:4063-4084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 257] [Article Influence: 51.4] [Reference Citation Analysis (0)] |
| 6. | Aminian A, Wilson R, Al-Kurd A, Tu C, Milinovich A, Kroh M, Rosenthal RJ, Brethauer SA, Schauer PR, Kattan MW, Brown JC, Berger NA, Abraham J, Nissen SE. Association of Bariatric Surgery With Cancer Risk and Mortality in Adults With Obesity. JAMA. 2022;327:2423-2433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 204] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 7. | Gasmi A, Bjørklund G, Mujawdiya PK, Semenova Y, Peana M, Dosa A, Piscopo S, Gasmi Benahmed A, Costea DO. Micronutrients deficiences in patients after bariatric surgery. Eur J Nutr. 2022;61:55-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 8. | Ruban A, Miras AD, Glaysher MA, Goldstone AP, Prechtl CG, Johnson N, Chhina N, Al-Najim W, Aldhwayan M, Klimowska-Nassar N, Smith C, Lord J, Li JV, Flores L, Al-Lababidi M, Dimitriadis GK, Patel M, Moore M, Chahal H, Ahmed AR, Cousins J, Aldubaikhi G, Glover B, Falaschetti E, Ashrafian H, Roux CWL, Darzi A, Byrne JP, Teare JP. Duodenal-Jejunal Bypass Liner for the management of Type 2 Diabetes Mellitus and Obesity: A Multicenter Randomized Controlled Trial. Ann Surg. 2022;275:440-447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 9. | Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, Clegg AJ. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1-190, 215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 607] [Cited by in RCA: 649] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 10. | Afonso J, Reis F. Dexmedetomidine: current role in anesthesia and intensive care. Rev Bras Anestesiol. 2012;62:118-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 213] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 11. | Sui X, Duan Q, Liu K, Li C. Postoperative delirium after long-term general anesthesia in elderly patients, how to reduce it?: Protocol of a double-blinded, randomized, placebo-controlled trial. Medicine (Baltimore). 2021;100:e25885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Zhang Y, Zhou Y, Hu T, Tong X, He Y, Li X, Huang L, Fu Q. Dexmedetomidine reduces postoperative pain and speeds recovery after bariatric surgery: a meta-analysis of randomized controlled trials. Surg Obes Relat Dis. 2022;18:846-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Bush B, Tobias JD, Lin C, Ruda J, Jatana KR, Essig G, Cooper J, Tumin D, Elmaraghy CA. Postoperative bradycardia following adenotonsillectomy in children: Does intraoperative administration of dexmedetomidine play a role? Int J Pediatr Otorhinolaryngol. 2018;104:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Barends CR, Absalom A, van Minnen B, Vissink A, Visser A. Dexmedetomidine versus Midazolam in Procedural Sedation. A Systematic Review of Efficacy and Safety. PLoS One. 2017;12:e0169525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 15. | Krispinsky LT, Stark RJ, Parra DA, Luan L, Bichell DP, Pietsch JB, Lamb FS. Endothelial-Dependent Vasomotor Dysfunction in Infants After Cardiopulmonary Bypass. Pediatr Crit Care Med. 2020;21:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Tang F, Yi JM, Gong HY, Lu ZY, Chen J, Fang B, Chen C, Liu ZY. Remimazolam benzenesulfonate anesthesia effectiveness in cardiac surgery patients under general anesthesia. World J Clin Cases. 2021;9:10595-10603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 17. | Xu K, Huang Y, Tan X, Sun H. Use of Remimazolam Combined With Alfentanil for Plastic Surgery Anesthesia Cases: A Clinical Trial. Ann Plast Surg. 2023;90:S221-S224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Li H, Li J, Hao C, Luan H, Zhang X, Zhao Z. Effects of anesthetic depth on perioperative T lymphocyte subsets in patients undergoing laparoscopic colorectal cancer surgery: a prospective, parallel-controlled randomized trial. BMC Anesthesiol. 2023;23:165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Matsushima M, Kimura S, Kitaura A, Hamasaki S, Iwamoto T, Mino T, Masui K, Nakao S. Propofol suppresses the His-ventricular conduction in paediatric patients. J Clin Pharm Ther. 2021;46:433-439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Kumar M, Kumar A, Yadav JBS, Bhardwaj SK, Singh AK. Anesthetic Stability of Propofol, Dexmedetomidine, and Isoflurane by Measuring Bispectral Index (BIS) and Hemodynamic Indices: A Comparative Study. Cureus. 2022;14:e24930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | De Cosmo G, Levantesi L, Del Vicario M. Sedation in digestive endoscopy: innovations for an old technique. Minerva Anestesiol. 2020;86:565-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Choi EK, Jang Y, Park SJ. Comparison of remimazolam and propofol induction on hemodynamic response in hypertensive patients. Medicine (Baltimore). 2023;102:e34358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 23. | Noor N, Legendre R, Cloutet A, Chitneni A, Varrassi G, Kaye AD. A comprehensive review of remimazolam for sedation. Health Psychol Res. 2021;9:24514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 24. | Liu X, Ding B, Shi F, Zhang Y, Liu L, Sha Y, Zhao T. The Efficacy and Safety of Remimazolam Tosilate versus Etomidate-Propofol in Elderly Outpatients Undergoing Colonoscopy: A Prospective, Randomized, Single-Blind, Non-Inferiority Trial. Drug Des Devel Ther. 2021;15:4675-4685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 25. | Yi X, Xu W, Li A. The Clinical Application of Remimazolam Benzenesulfonate Combined with Esketamine Intravenous Anesthesia in Endoscopic Retrograde Cholangiopancreatography. Biomed Res Int. 2022;2022:5628687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 26. | De Cassai A, Boscolo A, Geraldini F, Zarantonello F, Pettenuzzo T, Pasin L, Iuzzolino M, Rossini N, Pesenti E, Zecchino G, Sella N, Munari M, Navalesi P. Effect of dexmedetomidine on hemodynamic responses to tracheal intubation: A meta-analysis with meta-regression and trial sequential analysis. J Clin Anesth. 2021;72:110287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 27. | Deng Y, Qin Z, Wu Q, Liu L, Yang X, Ju X, Zhang Y. Efficacy and Safety of Remimazolam Besylate versus Dexmedetomidine for Sedation in Non-Intubated Older Patients with Agitated Delirium After Orthopedic Surgery: A Randomized Controlled Trial. Drug Des Devel Ther. 2022;16:2439-2451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 28. | Chen X, Zhang J, Yuan S, Huang H. Remimazolam besylate for the sedation of postoperative patients undergoing invasive mechanical ventilation in the ICU: a prospective dose‒response study. Sci Rep. 2022;12:19022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 29. | Sheng XY, Liang Y, Yang XY, Li LE, Ye X, Zhao X, Cui YM. Safety, pharmacokinetic and pharmacodynamic properties of single ascending dose and continuous infusion of remimazolam besylate in healthy Chinese volunteers. Eur J Clin Pharmacol. 2020;76:383-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 30. | Sneyd JR. Remimazolam: new beginnings or just a me-too? Anesth Analg. 2012;115:217-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |