Published online Apr 27, 2024. doi: 10.4240/wjgs.v16.i4.1203
Peer-review started: December 27, 2023
First decision: January 18, 2024
Revised: January 26, 2024
Accepted: March 4, 2024
Article in press: March 4, 2024
Published online: April 27, 2024
Processing time: 116 Days and 19.7 Hours
Gastric wall necrosis is a rare complication of endoscopic treatment for bleeding gastric ulcer, which may exacerbate the patient’s condition once it occurs and may even require surgical intervention for treatment.
A 59-year-old man was admitted to our department with melena. Endoscopy revealed a giant ulcer in the gastric antrum with a visible vessel in its center, which was treated with sclerosants and tissue glue injection and resulted in necrosis of the gastric wall.
Injection of sclerosants and tissue glue may lead to gastric wall necrosis, which is a serious complication. Therefore, before administering this treatment to patients, we should consider other more effective methods of hemostasis to avoid gastric wall necrosis.
Core Tip: Gastric wall necrosis is a rare but dangerous complication of endoscopic treatment for peptic ulcer. This case report describes a 59-year-old male patient who presented with melena and was found to have a giant ulcer in the gastric antrum, which developed gastric wall necrosis after injection of sclerosant and tissue glue. We should consider other more effective methods of hemostasis to avoid gastric wall necrosis.
- Citation: Li WF, Gao RY, Xu JW, Yu XQ. Endoscopic treatment of bleeding gastric ulcer causing gastric wall necrosis: A case report. World J Gastrointest Surg 2024; 16(4): 1203-1207
- URL: https://www.wjgnet.com/1948-9366/full/v16/i4/1203.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i4.1203
Bleeding is a prevalent complication of gastric ulcers, with an incidence rate of approximately 30%-50%[1]. Currently, endoscopic treatment is the preferred method for managing gastric ulcer bleeding. According to the Forrest classification, ulcers classified as Ia-IIb are at a high risk of bleeding and necessitate endoscopic intervention[2,3]. There is a variety of endoscopic treatment methods available, including the use of metal titanium clips, high-frequency electrocoagulation, drug injection, and haemostatic drug sprays. Endoscopic drug injection, in particular, is a straightforward and effective method for treating bleeding gastric ulcers. Relevant studies have demonstrated that sclerosants and tissue glue injection are effective treatment options for bleeding peptic ulcers[4,5]. However, it’s important to note that endoscopic drug injections can potentially lead to gastric wall necrosis, a rare but serious complication. In this report, we will present a case of gastric wall necrosis in a patient with a bleeding gastric ulcer who was treated with injections of sclerosants and tissue glue. We will also discuss its possible pathogenesis and preventive measures.
A 59-year-old male patient presented to the department of gastroenterology with a week-long history of melena and a two-hour syncope.
Symptoms started one week before the presentation, with an average of two black stools per day. The patient also experienced syncope two hours prior to the visit.
Three months ago, the patient underwent a physical examination at the local hospital, where a perfect ultrasound suggested alcoholic fatty liver.
Regarding personal and family history, the patient denied any family history of malignant tumors.
During the physical examination, the patient’s vital signs were recorded as follows: body temperature of 36.7 ℃, blood pressure of 103/62 mmHg, heart rate of 100 beats per minute, and respiratory rate of 20 breaths per minute. Additionally, the patient exhibited signs of anemia, such as a pale appearance, and showed no signs of pressure or rebound pain during abdominal examination.
The levels of serum tumor markers, specifically carcinoembryonic antigen (29.27 ng/mL) and carbohydrate antigen 72-4 (30.65 U/mL), were within normal range. Upon admission, the patient’s hemoglobin concentration was measured at 5.5 g/dL.
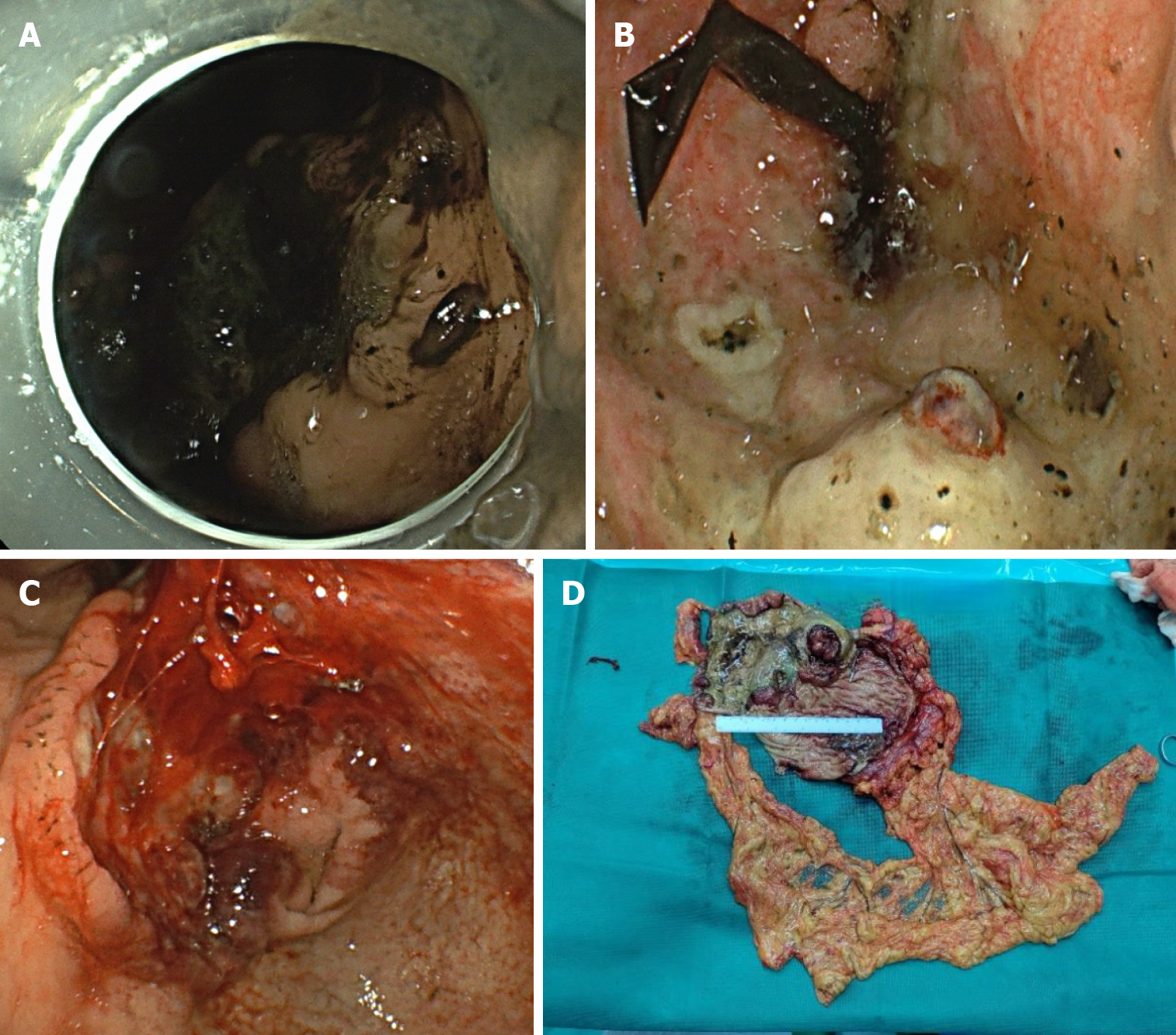
An emergency gastroscopy was performed, which revealed a large ulcer in the gastric antrum, approximately 3 cm × 4 cm in size, characterized by crater-like changes and the presence of black blood clot at the base. Notably, no active bleeding was observed (Figure 1A).
The patient’s treatment plan included the administration of proton pump inhibitors (PPIs) and a three-day fasting regimen. A follow-up gastroscopy revealed the exposure of blood vessels at the center of the previously identified gastric ulcer (Figure 1B). Despite the application of metallic titanium clips to close the vessel, active bleeding ensued. Subsequently, endoscopic injection therapy was administered, involving 1 mL of 1% lauromacrogol and 0.5 mL of tissue glue. This intervention resulted in surface hardening, and no active bleeding was observed after several minutes of monitoring (Figure 1C). Given the high risk of rebleeding and the potential malignancy of the ulcer, the patient was referred to the general surgery department for a partial gastrectomy the following day. Intraoperatively, extensive necrosis was noted in the gastric wall upon opening the abdominal cavity (Figure 1D). Histopathological examination of the resected specimen confirmed that the mass originated from a poorly differentiated Ulcerative gastric adenocarcinoma.
Combined with the patient’s medical history, the final diagnosis was stomach cancer with bleeding and gastric wall necrosis.
Postoperatively, the patient recovered well and required regular follow-up gastroscopies.
The patient demonstrated postoperative improvement and was subsequently discharged from the hospital. At 5 months postoperatively, the patient was still alive.
Gastric wall necrosis is a rare yet severe complication associated with endoscopic injections used in the treatment of gastric ulcers. Early case reports have documented instances of gastric wall necrosis following the use of sclerosing agents in managing peptic ulcer bleeding[6-8]. Dorta et al[6] and Cappelli et al[7] reported incidents of gastric wall necrosis subsequent to the application of polidocanol in treating bleeding gastric ulcers with vascular sprouts. Similarly, Chester[8] documented cases where the use of ethanolamine oleate injections in treating gastric ulcer bleeding resulted in gastric wall necrosis. Lauromacrogol, a newly developed sclerosing agent produced in China, directly damages the endothelium of blood vessels and induces thrombosis, thereby leading to vascular occlusion. To date, there have been no reported cases of gastric wall necrosis resulting from lauromacrogol injections. Tissue glue, a type of medical adhesive, solidifies upon contact with blood, effectively blocking varicose veins and achieving immediate hemostasis[9]. However, tissue glue has been observed to cause ectopic embolism, and some studies have shown that tissue glue injection can lead to gastric embolism[10].
We report a case of a bleeding giant gastric ulcer complicated by subsequent gastric wall necrosis. Despite the application of titanium clips to close the vessel, the patient continued to bleed. Hemostasis was eventually achieved through the administration of injections of lauromacrogol and tissue glue. Regrettably, this intervention was followed by necrosis of the stomach wall. We conducted an analysis of the potential causes of gastric wall necrosis, considering the injection of lauromacrogol, tissue glue, and a combination of both. Drawing on previous case reports of gastric wall necrosis induced by the injection of sclerosing agents, we noted that Cappelli et al[7] reported gastric wall necrosis following the injection of 4 mL of 1% polidocanol, and Scharnke et al[11] observed the same outcome after injecting 13 mL of 1% polidocanol. From these cases, we inferred that the overuse of sclerosing agents can lead to gastric wall necrosis. However, the sclerosing dose used in our case was relatively small. Given the absence of reports on gastric wall necrosis caused solely by tissue glue injection, we hypothesize that the gastric wall necrosis in this case was induced by the combined injection of lauromacrogol and tissue glue, a phenomenon not yet reported in the literature.
This case underscores several key considerations in the endoscopic treatment of gastric ulcer bleeding. First, for gastric ulcers with large blood vessels, titanium clip hemostasis may not be the optimal choice due to the gap between the clips, which may not ensure complete hemostasis. In such cases, the application of electrocoagulation to close the vessel could be considered as an alternative. Second, even in the presence of thick blood vessels and a high risk of rebleeding, surgical intervention may be considered for potentially malignant gastric ulcers if there is no active bleeding. Lastly, the injection of sclerosing agents and tissue glue may lead to gastric wall necrosis. This hemostatic protocol should be avoided whenever possible, and caution should be exercised with the dosage of sclerosing agents or tissue glue when used alone to minimize the risk of complications such as gastric wall necrosis, which can exacerbate the patient’s condition.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rodrigo L, Spain S-Editor: Gong ZM L-Editor: A P-Editor: Yuan YY
| 1. | Hidaka Y, Imai T, Inaba T, Kagawa T, Omae K, Tanaka S. Efficacy of vonoprazan against bleeding from endoscopic submucosal dissection-induced gastric ulcers under antithrombotic medication: A cross-design synthesis of randomized and observational studies. PLoS One. 2021;16:e0261703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107:345-60; quiz 361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 491] [Article Influence: 37.8] [Reference Citation Analysis (1)] |
| 3. | Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med. 1994;331:717-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 439] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 4. | Rutgeerts P, Rauws E, Wara P, Swain P, Hoos A, Solleder E, Halttunen J, Dobrilla G, Richter G, Prassler R. Randomised trial of single and repeated fibrin glue compared with injection of polidocanol in treatment of bleeding peptic ulcer. Lancet. 1997;350:692-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 108] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Aabakken L. Current endoscopic and pharmacological therapy of peptic ulcer bleeding. Best Pract Res Clin Gastroenterol. 2008;22:243-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Dorta G, Michetti P, Burckhardt P, Gillet M. Acute ischemia followed by hemorrhagic gastric necrosis after injection sclerotherapy for ulcer. Endoscopy. 1996;28:532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Cappelli J, Dryjski J, Rahier I, Ramdani B, Lamy V, Moisse R. Another severe complication of sclerotherapy for bleeding peptic ulcer. Endoscopy. 1993;25:431-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Chester JF, Hurley PR. Gastric necrosis: a complication of endoscopic sclerosis for bleeding peptic ulcer. Endoscopy. 1990;22:287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Taboada G, Yang K, Pereira M, Liu S, Hu Y, Karp J, Artzi N, Lee Y. Overcoming the translational barriers of tissue adhesives. Nat Rev Mater. 2020;5:310-329. [RCA] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 235] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 10. | Loffroy R, Comby PO, Guillen K, Salsac AV. N-Butyl Cyanoacrylate-Lipiodol Mixture for Endovascular Purpose: Polymerization Kinetics Differences Between In Vitro and In Vivo Experiments. Cardiovasc Intervent Radiol. 2020;43:1409-1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Scharnke W, Hust MH, Braun B, Schumm W. Complete gastric wall necrosis after endoscopic sclerotherapy for a gastric ulcer with visible arterial stump. Dtsch Med Wochenschr. 1997;122:606-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |