Published online Apr 27, 2024. doi: 10.4240/wjgs.v16.i4.1078
Peer-review started: December 19, 2023
First decision: January 9, 2024
Revised: January 30, 2024
Accepted: March 15, 2024
Article in press: March 15, 2024
Published online: April 27, 2024
Processing time: 125 Days and 9.3 Hours
Benign gallbladder diseases have become a high-prevalence condition not only in China but also worldwide. The main types of benign gallbladder diseases include gallbladder polyps, acute and chronic cholecystitis, and gallstones, with gallstones being the most common, accounting for over 70% of cases. Although the mortality rate of benign gallbladder diseases is low, they carry obvious potential risks. Studies have shown that an increased incidence of benign gallbladder diseases can increase the risk of cardiovascular diseases and gallbladder cancer, resulting in a substantial disease burden on patients and their families.
To assess the medical utility of the Configuration-Procedure-Consequence (CPC) three-dimensional quality evaluation model in modulating the prognosis of laparoscopic cholecystectomy patients.
A total of 98 patients who underwent laparoscopic cholecystectomy in our hospital from February 2020 to January 2022 were selected as the subjects. According to the random number table method, they were divided into a study group and a control group, with 49 patients in each group. The control group received routine perioperative care, while the study group had the addition of the CPC three-dimensional quality evaluation. The postoperative recovery-related indicators (time to first flatus, time to oral intake, time to ambulation, hospital stay), stress indicators (cortisol and adrenaline levels), distinctions in anxiety and depression status, and the incidence of perioperative complications were compared.
The time to first flatus, time to oral intake, time to ambulation, and hospital stay of the study group patients were obviously lower than those of the control group patients, with statistical significance (P < 0.05). On the 1st day after admission, there were no obvious distinctions in cortisol and adrenaline levels in blood samples, as well as in the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) scores between the study group and the control group (P > 0.05). However, on the 3rd day after surgery, the cortisol and adrenaline levels, as well as SAS and SDS scores of the study group patients, were obviously lower than those of the control group patients (P < 0.05). The study group had 2 cases of incisional infection and 1 case of pulmonary infection, with a total incidence of complications of 6.12% (3/49), which was obviously lower than the 20.41% (10/49) in the control group (P < 0.05).
Implementing the CPC three-dimensional quality evaluation model for patients undergoing laparoscopic cholecystectomy can help accelerate their perioperative recovery process, alleviate perioperative stress symptoms, mitigate anxiety, depression, and other adverse emotions, and to some extent, reduce the incidence of perioperative complications.
Core Tip: The study aimed to explore the clinical value of a three-dimensional quality evaluation model in adjusting the prognosis of patients undergoing laparoscopic cholecystectomy. Results showed that patients in the study group had significantly lower anal exhaust time, postoperative eating time, postoperative bed activity time, and length of hospital stay compared to the control group. There were no significant differences in cortisol, adrenaline levels, and anxiety and depression scores between the two groups on the first day after admission. However, on the third day after surgery, the study group showed significantly lower cortisol and adrenaline levels, as well as lower anxiety and depression scores than the control group. The study group had a lower incidence of perioperative complications compared to the control group. In conclusion, implementing a three-dimensional quality evaluation model in patients undergoing laparoscopic cholecystectomy can help expedite their perioperative recovery, alleviate perioperative stress symptoms, mitigate anxiety and depression, and reduce the incidence of perioperative complications.
- Citation: Zhou Y, Chen ZQ. Research on the prognostic value of adjusting intraperitoneal three-dimensional quality evaluation mode in laparoscopic cholecystectomy patients. World J Gastrointest Surg 2024; 16(4): 1078-1086
- URL: https://www.wjgnet.com/1948-9366/full/v16/i4/1078.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i4.1078
Benign gallbladder diseases have become a high-prevalence condition not only in China but also worldwide[1,2]. The main types of benign gallbladder diseases include gallbladder polyps, acute and chronic cholecystitis, and gallstones, with gallstones being the most common, accounting for over 70% of cases[3]. Although the mortality rate of benign gallbladder diseases is low, they carry obvious potential risks. Studies have shown that an increased incidence of benign gallbladder diseases can increase the risk of cardiovascular diseases and gallbladder cancer, resulting in a substantial disease burden on patients and their families[4]. Early surgical intervention is the most common, rapid, and thorough treatment for benign gallbladder diseases.
In 1985, German physician Muhe performed the first laparoscopic cholecystectomy, which rapidly popularized the use of laparoscopic techniques worldwide and ushered in a new era of minimally invasive surgery[5]. Compared to traditional open surgery, laparoscopic surgery has the advantages of minimal trauma, faster patient recovery, and lower postoperative pain, making it the "gold standard" for treating benign gallbladder diseases[6]. However, medical practice has found that patients undergoing laparoscopic cholecystectomy still have a relatively high incidence of perioperative complications. It has been reported that the preoperative anxiety rate in patients undergoing laparoscopic cholecystectomy is as high as around 76%, and the likelihood of postoperative incision infection and stress reactions is also relatively high[7,8], which to some extent affects the patients' postoperative recovery process.
The Configuration-Procedure-Consequence (CPC) three-dimensional quality evaluation model is a nursing model proposed by Donabedian in the late 1960s. In this model, structure refers to the attributes of the nursing environment, including material resources, staffing, etc. Process primarily focuses on how to apply the structural attributes to practical activities, while outcome represents the results brought about by the process and aims to evaluate the success of the program[9,10]. This study, through the establishment of a control group, found that the CPC three-dimensional quality evaluation model helps accelerate the perioperative recovery process of patients undergoing laparoscopic cholecystectomy and alleviate their anxiety and depression symptoms.
For this study, a total of 98 patients who underwent laparoscopic cholecystectomy were chosen. In the research group, there were 26 males and 23 females, with an average age of (44.02 ± 9.78) years. In the control group, there were 29 males and 20 females, with an average age of (46.64 ± 9.77) years. There were no obvious distinctions in baseline medical data (P > 0.05). This study has been approved by the hospital's ethics committee.
(1) Age ≥ 18 years old; (2) Inpatients scheduled for elective laparoscopic cholecystectomy for uncomplicated gallstones or gallbladder polyps; and (3) Complete and comprehensive baseline medical data.
(1) Patients who required conversion to open surgery during the operation; (2) Patients with severe cardiovascular diseases; (3) Patients with malignant tumors; (4) Patients with intellectual disabilities that affect communication; (5) Patients with recent symptoms of anxiety or depression; (6) Patients with cognitive impairments; and (7) Patients who have been included in other medical studies and have not completed them.
Patients in the control group received routine perioperative care for laparoscopic cholecystectomy, including actively establishing patient records upon admission, improving preoperative examination measures, providing patients with health education brochures, informing patients about relevant knowledge of laparoscopic cholecystectomy, allowing patients to fully understand their own conditions, possible prognosis, and risks of complications, and improving patient compliance.
Patients in the research group received the CPC three-dimensional quality evaluation model in addition to the routine care provided to the control group.
(1) Establishment of a nursing intervention team, consisting of the head nurse of the Hepatobiliary Surgery Department, attending physician, responsible nurse, and psychologist. The team members were trained collectively in advance to fully understand the relevant knowledge of the CPC three-dimensional quality evaluation model. The nurse was responsible for convening the team members for training. The attending physician was responsible for preoperative and postoperative assessment of patients. The responsible nurse was responsible for conducting health assessments (such as psychological status, underlying diseases), recording rehabilitation progress, and data statistics. The psychologist was responsible for conducting psychological assessments and interventions for patients.
(2) Structure evaluation: Evaluate the treatment environment and resources for inpatients. Through literature review and review of medical records, fully understand the common complications and intraoperative precautions of laparoscopic cholecystectomy. Evaluate the hospital resources based on the concept of anticipatory nursing, including whether there are conditions to prevent complications, whether there are facilities for providing psychological counseling to patients, and whether there are conditions for follow-up visits to patients.
(3) Process evaluation: This step focuses on specifying the detailed intervention measures. For example, conduct psychological assessments of patients upon admission to understand their understanding of the disease. Based on the assessment results, intervene accordingly. For patients with mild anxiety or depression, provide psychological comfort. For patients with severe anxiety or depression, seek assistance from their family members or friends while implementing psychological interventions to provide social support. In terms of complications prevention, actively assess the condition of the incision in the postoperative period and perform timely dressing changes.
And (4) Outcome evaluation: Evaluate the results from several aspects, including patients' recovery status (recorded as time to first passage of flatus, time to oral intake after surgery, time to ambulation after surgery, length of hospital stay), stress indicators (cortisol and adrenaline levels in blood samples taken within 1 d after admission and 3 d after surgery), changes in anxiety and depression [evaluated using the Self-Rating Anxiety Scale (SAS)[11] and Self-Rating Depression Scale (SDS)[12]], and the incidence of complications such as wound infection and pulmonary infection during the perioperative period in both groups.
Data collection was conducted using EXCEL 2021, and data processing and analysis were performed using SPSS 19.0. Continuous data were expressed as the mean with the corresponding standard deviation, and distinctions between groups were assessed using t-tests. Categorical data were displayed as percentages (%) and distinctions between groups were analyzed using chi-square tests. A significance level of P < 0.05 was considered obvious.
General medical data, including gender, age, operation time, laboratory indicators (ALT, AST, FBG, CREA, etc.), comorbidities, smoking and alcohol consumption, were collected and compared. The results showed no obvious distinctions (P > 0.05) (Table 1).
| Baseline medical data | Research group (n = 49) | Control group (n = 49) | P value | |
| Gender | Male | 26 (53.06) | 29 (59.18) | 0.541 |
| Female | 23 (46.94) | 20 (40.82) | ||
| Mean age (yr) | 44.02 ± 9.78 | 46.64 ± 9.77 | 0.188 | |
| Mean operation time (min) | 59.38 ± 10.67 | 58.06 ± 10.22 | 0.533 | |
| ALT (U/L) | 30.34 ± 4.57 | 30.32 ± 5.18 | 0.984 | |
| AST (U/L) | 36.16 ± 10.90 | 35.67 ± 11.75 | 0.831 | |
| FBG (mmol/L) | 4.81 ± 0.98 | 4.99 ± 0.91 | 0.348 | |
| CREA (μmol/L) | 74.94 ± 15.26 | 74.60 ± 14.48 | 0.910 | |
| CK (U/L) | 185.58 ± 114.33 | 191.46 ± 100.04 | 0.787 | |
| UA (μmol/L) | 346.74 ± 89.00 | 368.21 ± 87.36 | 0.231 | |
| Concurrent diseases | ||||
| Hypertension | 5 (10.20) | 6 (12.24) | 0.102 | |
| Diabetes | 4 (8.16) | 5 (10.20) | 0.122 | |
| Smoking | 7 (14.29) | 6 (12.24) | 0.089 | |
| Drinking | 6 (12.24) | 5 (10.20) | 0.102 | |
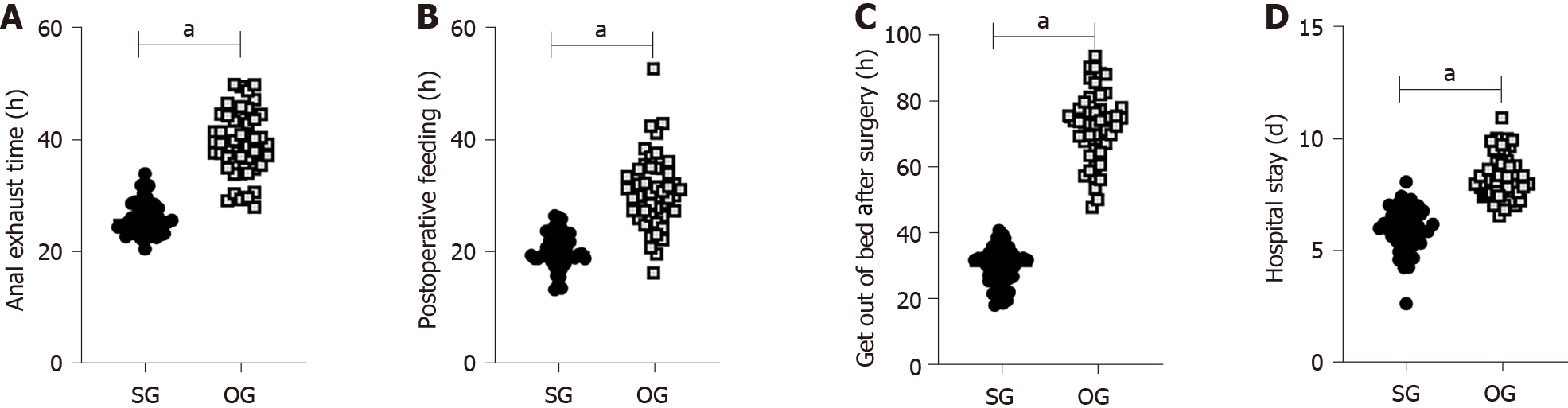
The anal exhaust time (Figure 1A), postoperative diet time (Figure 1B), postoperative ambulation time (Figure 1C), and length of hospital stay (Figure 1D) in the research group were obviously lower than the control, with obvious distinctions (P < 0.05) (Table 2).
| Groups | Cases | Anal exhaust time (h) | Postoperative feeding time (h) | Postoperative ambulation time (h) | Length of stay (d) |
| Research group | 49 | 26.14 ± 2.85 | 20.30 ± 3.11 | 29.25 ± 5.58 | 5.99 ± 1.00 |
| Control group | 49 | 39.33 ± 5.66 | 30.80 ± 6.49 | 72.27 ± 10.67 | 8.33 ± 0.99 |
| t | - | 14.570 | 10.213 | 25.010 | 11.640 |
| P value | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
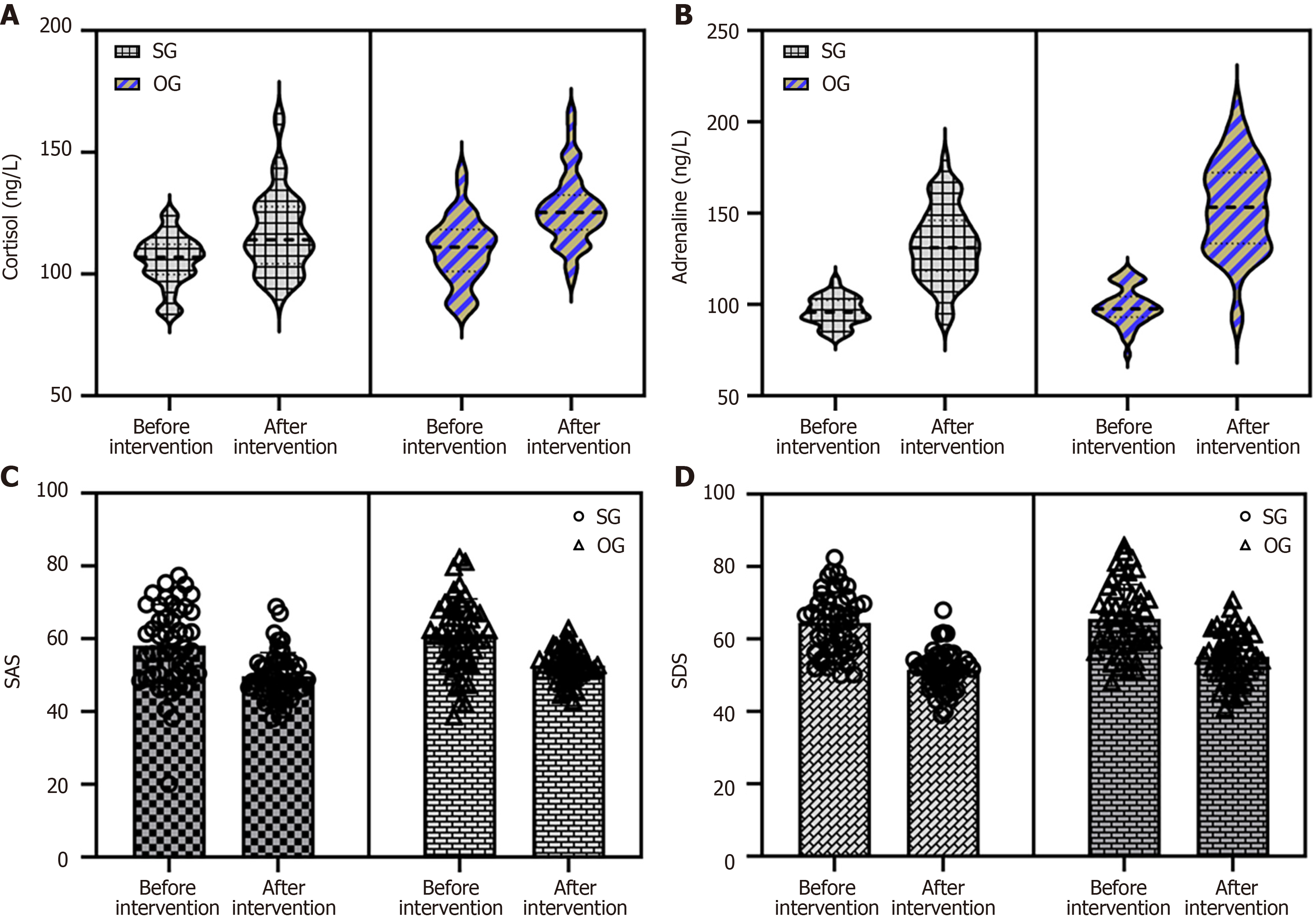
At postoperative day 1, there was no obvious distinction in cortisol and adrenaline levels between the research group and the control group (P > 0.05). However, at postoperative day 3, the cortisol and adrenaline levels in the research group were obviously lower than the control (P < 0.05) (Table 3, Figure 2A and B).
| Groups | Cases | Cortisol (ng/L) | Epinephrine (ng/L) | ||
| Day 1 of admission | 3 d after surgery | Day 1 of admission | 3 d after surgery | ||
| Research group | 49 | 105.55 ± 10.31 | 116.65 ± 16.47 | 96.18 ± 7.72 | 132.50 ± 20.28 |
| Control group | 49 | 110.08 ± 13.73 | 126.69 ± 14.77 | 99.01 ± 10.24 | 153.36 ± 25.92 |
| t | - | 1.847 | 3.177 | 1.545 | 4.437 |
| P value | - | 0.068 | 0.002 | 0.126 | < 0.001 |
There was no obvious distinction in cortisol levels between the two patient groups at postoperative day 1 (P > 0.05). However, at postoperative day 3, the research group had obviously lower cortisol levels compared to the control group (P < 0.05).
There was no obvious distinction in adrenaline levels between the two patient groups at postoperative day 1 (P > 0.05). However, at postoperative day 3, the research group had obviously lower adrenaline levels compared to the control group (P < 0.05).
At postoperative day 1, there was no obvious distinction in SAS and SDS scores between the research group and the control group (P > 0.05). However, at postoperative day 3, the SAS and SDS scores of the research group were obviously lower than those of the control group (P < 0.05) (Table 4, Figure 2C and D).
| Groups | Cases | SAS | SDS | ||
| Day 1 of admission | 3 d after surgery | Day 1 of admission | 3 d after surgery | ||
| Research group | 49 | 58.11 ± 11.30 | 49.74 ± 6.45 | 64.46 ± 8.45 | 51.44 ± 5.54 |
| Control group | 49 | 61.18 ± 9.82 | 52.62 ± 4.32 | 65.51 ± 9.57 | 55.09 ± 6.86 |
| t | - | 1.435 | 2.597 | 0.027 | 2.898 |
| P value | - | 0.154 | 0.011 | 0.978 | 0.005 |
There was no obvious distinction in SAS scores between the two patient groups at postoperative day 1 (P > 0.05). However, at postoperative day 3, the research group had obviously lower SAS scores compared to the control group (P < 0.05).
There was no obvious distinction in SDS scores between the two patient groups at postoperative day 1 (P > 0.05). However, at postoperative day 3, the research group had obviously lower SDS scores compared to the control group (P < 0.05).
In the research group, there were 2 cases of surgical site infection and 1 case of lung infection, with a total complication rate of 6.12% (3/49). This was obviously lower than the control group, which had a complication rate of 20.41% (10/49). The distinction was obvious (P < 0.05) as shown in Table 5.
| Groups | Cases | Incision infection | Pulmonary infection | Ascites | Incidence rate |
| Research group | 49 | 2 (4.08) | 1 (2.04) | 0 (0.00) | 3 (6.12) |
| Control group | 49 | 5 (10.20) | 3 (6.12) | 2 (4.08) | 10 (20.41) |
| χ2 | - | - | - | - | 4.346 |
| P value | - | - | - | - | 0.037 |
Gallstone in the common bile duct is a common and prevalent disease in hepatobiliary surgery, and its incidence increases with age. Although small gallstones can be spontaneously discharged from the bile duct, the condition can progress to acute obstructive suppurative cholangitis or gallstone pancreatitis, posing a certain threat to patient safety[13,14]. Traditional open choledochotomy for stone extraction is associated with a larger trauma, longer postoperative recovery period, and higher incidence of complications[15]. In medical practice, it has been found that routine perioperative care for patients undergoing laparoscopic cholecystectomy lacks scientific planning and coherence, which may impact[16].
In this study, the value of applying the CPC three-dimensional quality evaluation model to patients undergoing laparoscopic cholecystectomy was analyzed through the establishment of a control group. The results showed that compared to the control group that received routine care, the research group that received the CPC three-dimensional quality evaluation model showed obviously better postoperative recovery indicators, such as shorter time to first bowel movement, time to first oral intake, time to ambulation, and shorter hospital stay. The authors of this study analyzed that traditional perioperative care for patients undergoing laparoscopic cholecystectomy lacks integrity, and there may be a lack of coordination among healthcare providers, which can affect the surgical and subsequent recovery processes of patients. On the other hand, the CPC three-dimensional quality evaluation model prepared adequately before nursing interventions, including information collection on available hospital resources and common postoperative complications, making the entire nursing process organized and systematic[17,18]. Based on this, specific measures for patient intervention were defined, such as active postoperative assessment and intraoperative warming, laying a solid foundation for.
The study also compared the distinctions in adverse emotions of patients after intervention. The results showed that compared to the control group that received routine care, the research group that received the CPC three-dimensional quality evaluation model nursing had obviously lower SAS and SDS scores at postoperative day 3, indicating that the research group had milder postoperative anxiety and depression. The authors of this study analyzed that anxiety and depression are common adverse emotions during the perioperative period in patients undergoing laparoscopic cholecystectomy, which may be related to patients' lack of disease-related knowledge and disease stress responses. Mild adverse emotions can improve patients' treatment compliance, but excessive anxiety and depression can not only affect their endocrine system but also lower their medical adherence, and even induce conflicts between patients and healthcare providers. Therefore, it is necessary to pay sufficient attention to patients' adverse emotions[19,20]. The CPC three-dimensional quality evaluation model implemented in this study focused on improving patients' adverse emotions as the primary evaluation outcome, employing proactive psychological counseling, social support, family encouragement, and health education to correct patients' misperceptions and increase their treatment confidence, ultimately reducing their anxiety and depression levels[21].
Lastly, the results of the study also suggested that the CPC three-dimensional quality evaluation model is helpful in improving the perioperative stress status and reducing the incidence of complications in patients undergoing laparoscopic cholecystectomy. The authors of this study analyzed that this is also related to the fact that the model can accelerate patients' postoperative recovery process, reduce their adverse emotions. Previous studies have demonstrated that adverse emotions put individuals in a state of stress, affecting their hormone secretion levels, suppressing their immune status, and thus increasing the occurrence rate of infections and other events, and the results of this study indirectly confirm this viewpoint[22,23].
In conclusion, the CPC three-dimensional quality evaluation model complements nursing services. Good structure facilitates the advancement of processes, and smooth processes lay the foundation for the outcomes. Implementing the CPC three-dimensional quality evaluation model for patients undergoing laparoscopic cholecystectomy helps accelerate their perioperative recovery process, alleviate their perioperative stress symptoms, relieve their anxiety and depression, and to some extent, reduce the incidence of perioperative complications. However, this study also has certain limitations, such as a single source of the included sample, a small sample size, and a lack of follow-up. Conducting multicenter, large-sample follow-up studies in the future will provide more theoretical references for accelerating the perioperative recovery of patients undergoing laparoscopic cholecystectomy.
This study introduced a three-dimensional quality evaluation model of configuration program result to evaluate the prognosis of patients undergoing laparoscopic cholecystectomy. The implementation of a three-dimensional quality assessment model seems to improve the recovery process of patients undergoing laparoscopic cholecystectomy, reduce stress symptoms, and potentially reduce the incidence of complications.
The main topic of this research is the implementation and evaluation of the Configuration-Procedure-Consequence (CPC) three-dimensional quality assessment model in the context of laparoscopic cholecystectomy. The key problems to be solved in this study are: (1) Inadequate patient outcomes: Reducing postoperative complications, enhancing patient satisfaction, and optimizing recovery; and (2) Fragmented approach to patient care: The current approach to patient care often focuses on the surgical procedure itself. This fragmented approach may limit the potential for improving patient outcomes and experiences. The significance of solving these problems for future research in this field are: (1) Enhanced patient outcomes; (2) Improved patient satisfaction; (3) Advancement of surgical care models; and (4) Integration of holistic care approaches. Overall, solving the key problems in laparoscopic cholecystectomy through the implementation of the CPC model can have a significant impact on improving patient outcomes, advancing surgical care models, and promoting holistic care approaches in healthcare.
The research objectives for this study are as follows: (1) To assess the effectiveness of the CPC three-dimensional quality assessment model in improving the outcomes of patients undergoing laparoscopic cholecystectomy; (2) To compare the postoperative recovery outcomes between the study group receiving care based on the CPC model and the control group receiving standard care; (3) To evaluate the physiological impact of the CPC model on patients by measuring cortisol and adrenaline levels; and (4) To assess the psychological impact of the CPC model on patients through self-report questionnaires. The objectives that were realized in this study include: (1) Determining whether the CPC model can lead to improved postoperative recovery outcomes compared to standard care; (2) Establishing the impact of the CPC model on physiological indicators such as cortisol and adrenaline levels; and (3) Evaluating the psychological impact of the CPC model on patients' well-being. The significance of realizing these objectives for future research in this field are: (1) Providing evidence on the effectiveness of the CPC model in enhancing the outcomes of laparoscopic cholecystectomy patients; (2) Contributing to the development and refinement of the CPC model by identifying its strengths, weaknesses, and areas for improvement; (3) Informing future research on the integration of the CPC model in other surgical procedures or healthcare settings to enhance patient care and outcomes; and (4) Promoting a holistic approach to patient care.
This study utilizes a randomized controlled trial design to evaluate the effectiveness of the CPC three-dimensional quality assessment model in patients undergoing laparoscopic cholecystectomy. Participants are assigned to either the study group receiving care based on the CPC model or the control group receiving standard care. Several measures, including first bowel movement time, oral intake time, walking time, and length of hospital stay, are assessed to evaluate postoperative recovery. Physiological indicators such as cortisol and adrenaline levels, as well as self-report questionnaires, are used to assess psychological impact.
The research findings of this study contribute to the field by demonstrating the potential benefits of implementing the CPC three-dimensional quality assessment model in laparoscopic cholecystectomy patients. The results indicate that the use of this model is associated with improved postoperative recovery outcomes, reduced stress levels, and potentially lower complication rates. Specifically, the study found that patients in the study group had significantly shorter first flatus time, oral intake time, ambulation time, and hospital stay compared to the control group. Moreover, on the third day after surgery, patients in the study group exhibited significantly lower levels of cortisol and epinephrine, as well as lower anxiety and depression scores, compared to the control group. However, there are still some remaining problems to be solved. The study involved a relatively small sample size, which may limit the generalizability of the findings. Additionally, longer-term follow-up evaluations are needed to assess the sustained effects of implementing the model. Furthermore, the cost-effectiveness and feasibility of incorporating this model into routine clinical practice need to be further investigated. In conclusion, the research results highlight the potential benefits of the CPC three-dimensional quality assessment model in facilitating the recovery process, reducing stress symptoms, and potentially lowering complication rates in laparoscopic cholecystectomy patients.
This study demonstrates the application value of the process structure result three-dimensional quality evaluation regulation mode in patients undergoing laparoscopic cholecystectomy, providing new nursing measures for perioperative rehabilitation of patients undergoing laparoscopic cholecystectomy at the theoretical level. The new method of this study is a nursing intervention that integrates structural assessment process assessment and structural assessment, achieving a perfect cycle of planning, argumentation, re-evaluation, and correction, providing new nursing measures for perioperative rehabilitation of patients undergoing laparoscopic cholecystectomy.
The direction of future research in this study could focus on further validating the CPC three-dimensional quality assessment model in larger and more diverse patient populations.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pignatta S, Italy S-Editor: Yan JP L-Editor: A P-Editor: Yu HG
| 1. | Gutt C, Schläfer S, Lammert F. The Treatment of Gallstone Disease. Dtsch Arztebl Int. 2020;117:148-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 2. | Di Ciaula A, Wang DQ, Portincasa P. An update on the pathogenesis of cholesterol gallstone disease. Curr Opin Gastroenterol. 2018;34:71-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 156] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 3. | Alemi F, Seiser N, Ayloo S. Gallstone Disease: Cholecystitis, Mirizzi Syndrome, Bouveret Syndrome, Gallstone Ileus. Surg Clin North Am. 2019;99:231-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | Mueck KM, Wei S, Pedroza C, Bernardi K, Jackson ML, Liang MK, Ko TC, Tyson JE, Kao LS. Gallstone Pancreatitis: Admission Versus Normal Cholecystectomy-a Randomized Trial (Gallstone PANC Trial). Ann Surg. 2019;270:519-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Schepers NJ, Hallensleben NDL, Besselink MG, Anten MGF, Bollen TL, da Costa DW, van Delft F, van Dijk SM, van Dullemen HM, Dijkgraaf MGW, van Eijck CHJ, Erkelens GW, Erler NS, Fockens P, van Geenen EJM, van Grinsven J, Hollemans RA, van Hooft JE, van der Hulst RWM, Jansen JM, Kubben FJGM, Kuiken SD, Laheij RJF, Quispel R, de Ridder RJJ, Rijk MCM, Römkens TEH, Ruigrok CHM, Schoon EJ, Schwartz MP, Smeets XJNM, Spanier BWM, Tan ACITL, Thijs WJ, Timmer R, Venneman NG, Verdonk RC, Vleggaar FP, van de Vrie W, Witteman BJ, van Santvoort HC, Bakker OJ, Bruno MJ; Dutch Pancreatitis Study Group. Urgent endoscopic retrograde cholangiopancreatography with sphincterotomy versus conservative treatment in predicted severe acute gallstone pancreatitis (APEC): a multicentre randomised controlled trial. Lancet. 2020;396:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 6. | Haal S, Guman MSS, Bruin S, Schouten R, van Veen RN, Fockens P, Dijkgraaf MGW, Hutten BA, Gerdes VEA, Voermans RP. Risk Factors for Symptomatic Gallstone Disease and Gallstone Formation After Bariatric Surgery. Obes Surg. 2022;32:1270-1278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 7. | Di Ciaula A, Garruti G, Frühbeck G, De Angelis M, de Bari O, Wang DQ, Lammert F, Portincasa P. The Role of Diet in the Pathogenesis of Cholesterol Gallstones. Curr Med Chem. 2019;26:3620-3638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Kube I, Zwanziger D. Thyroid Dysfunction and Cholesterol Gallstone Disease. Exp Clin Endocrinol Diabetes. 2020;128:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Xu Y, Wang H, Yang M. Preoperative nursing visit reduces preoperative anxiety and postoperative complications in patients with laparoscopic cholecystectomy: A randomized clinical trial protocol. Medicine (Baltimore). 2020;99:e22314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Lan L, Zhu X, Ye B, Jiang H, Huang Y. Effects of Individualized Nursing Based on Zero-Defect Theory on Perioperative Patients Undergoing Laparoscopic Cholecystectomy. Dis Markers. 2022;2022:5086350. [PubMed] [DOI] [Full Text] |
| 11. | Li S, Bai J, Wei W, Liu X, Shen Y. Effect of systematic nursing on the stress response and recovery of gastrointestinal function in patients undergoing laparoscopic cholecystectomy. Am J Transl Res. 2021;13:9647-9654. [PubMed] |
| 12. | Liu X, Luan Y, Zhang L, Li Y. Influence of aromatic essential oil nursing on mental state of patients undergoing laparoscopic cholecystectomy: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2022;101:e29122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | da Silva Schulz R, Santana RF, Dos Santos CTB, Faleiro TB, do Amaral Passarelles DM, Hercules ABS, do Carmo TG. Telephonic nursing intervention for laparoscopic cholecystectomy and hernia repair: A randomized controlled study. BMC Nurs. 2020;19:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Wang P, Ma S, Yu L. Study on the application effect of personalized nursing in the operating room of laparoscopic cholecystectomy for gallstone. Panminerva Med. 2022;64:302-303. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Lu YJ, Lee MC, Chen CY, Liang SY, Li YP, Chen HM. Effect of Guided Imagery Meditation During Laparoscopic Cholecystectomy on Reducing Anxiety: A Randomized Controlled Trial. Pain Manag Nurs. 2022;23:885-892. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Gach T, Bogacki P, Markowska B, Bonior J, Paplaczyk M, Szura M. Quality of life in patients after laparoscopic cholecystectomy due to gallstone disease - evaluation of long-term postoperative results. Pol Przegl Chir. 2021;93:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Gao Y, Huang J, Zheng Y, Han J. Effect of comfort nursing on postoperative quality of life, negative emotions and nursing satisfaction in patients undergoing laparoscopic surgery. Am J Transl Res. 2021;13:13825-13834. [PubMed] |
| 18. | Jokar M, Larti N, Zarei M, Melali H, Zabihirad J, Maraki F, Jazini Dorcheh S, Kelidari B. Comparative Study of the Incidence of Port Site Infection in Disposable Ports and Reprocessed Disposable Ports in Laparoscopic Cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2022;32:650-654. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Markers D. Retracted: Effects of Individualized Nursing Based on Zero-Defect Theory on Perioperative Patients Undergoing Laparoscopic Cholecystectomy. Dis Markers. 2023;2023:9785270. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Vaysburg DM, Delman AM, Turner KM, Salvator A, Frasier LL. Laparoscopic Appendectomy and Cholecystectomy Timing Predicts Hand-Offs but Not Miscounts. J Surg Res. 2022;280:55-62. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Salimi Zadak R, Khalili G, Motamedi M, Bakhtiari S. The effect of chamomile on flatulence after the laparoscopic cholecystectomy: A randomized triple-blind placebo-controlled clinical trial. J Ayurveda Integr Med. 2023;14:100735. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Chiang HY, Lin KR, Hsiao YL, Huang HC, Chang SN, Hung CH, Chang Y, Wang YC, Kuo CC. Association Between Preoperative Blood Glucose Level and Hospital Length of Stay for Patients Undergoing Appendectomy or Laparoscopic Cholecystectomy. Diabetes Care. 2021;44:107-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 23. | Sözen KK, Karabulut N. Efficacy of Hand and Foot Massage in Anxiety and Pain Management Following Laparoscopic Cholecystectomy: A Controlled Randomized Study. Surg Laparosc Endosc Percutan Tech. 2020;30:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |