Published online Mar 27, 2024. doi: 10.4240/wjgs.v16.i3.807
Peer-review started: October 24, 2023
First decision: December 15, 2023
Revised: January 13, 2024
Accepted: February 7, 2024
Article in press: February 7, 2024
Published online: March 27, 2024
Processing time: 150 Days and 9.1 Hours
Ostomy is a common surgery usually performed to protect patients from clinical symptoms caused by distal anastomotic leakage after colorectal cancer (CRC) surgery and perforation or to relieve intestinal obstruction.
To analyze the complications after transverse colostomy closure.
Patients who underwent transverse colostomy closure from Jan 2015 to Jan 2022 were retrospectively enrolled in a single clinical center. The differences between the complication group and the no complication group were compared. Logistic regression analyses were conducted to find independent factors for overall complications or incision infection.
A total of 102 patients who underwent transverse colostomy closure were enrolled in the current study. Seventy (68.6%) patients underwent transverse colostomy because of CRC related causes. Postoperative complications occurred in 30 (29.4%) patients and the most frequent complication occurring after transverse colostomy closure was incision infection (46.7%). The complication group had longer hospital stays (P < 0.01). However, no potential risk factors were identified for overall complications and incision infection.
The most frequent complication occurring after transverse colostomy closure surgery in our center was incision infection. The operation time, interval from transverse colostomy to reversal, and method of anastomosis might have no impact on the postoperative complications. Surgeons should pay more attention to aseptic techniques.
Core Tip: The current study was conducted to analyze the complications after transverse colostomy closure. A total of 102 patients who underwent transverse colostomy closure were enrolled in the current study. The complication group had longer hospital stay. However, no potential risk factor was identified for overall complications and incision infection. The most frequent complication occurring after transverse colostomy closure surgery in our center was incision infection. Operation time, interval from transverse colostomy to reversal and methods of anastomosis might have no impact on the postoperative complications. Surgeons should pay more attention to aseptic techniques.
- Citation: Liu F, Luo XJ, Li ZW, Liu XY, Liu XR, Lv Q, Shu XP, Zhang W, Peng D. Early postoperative complications after transverse colostomy closure, a retrospective study. World J Gastrointest Surg 2024; 16(3): 807-815
- URL: https://www.wjgnet.com/1948-9366/full/v16/i3/807.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i3.807
Ostomy is a common surgery usually performed to protect patients from clinical symptoms caused by distal anastomotic leakage after colorectal cancer (CRC) surgery and perforation or to relieve intestinal obstruction[1-3]. Given the convenience and validity of preventing anastomotic leakage, some experts have also suggested performing prophylactic ostomy[4-7]. A temporary stoma was usually recommended to be reversed at nearly 3 months after primary surgery[8,9]. However, several studies have reported a high rate of complications after ostomy closure, especially surgical site infections, with the highest rate reaching 40%[10]. Postoperative complications can lengthen hospital stays and cause heavy financial burdens, and severe complications can lead to death[11,12]. For better management of complications, several risk factors for complications have been reported, such as the interval from ostomy to reversal, operation time, blood transfusion and stapled anastomosis[13-17].
Previous studies have compared the incidence of postoperative complications between ileostomy and colostomy closure and found that patients who underwent colostomy closure were more likely to suffer from complications[18-20]. Most studies reporting complications after colostomy closure were conducted at the end of the last century, and the sample sizes were relatively small[21-23]. Furthermore, which factors, such as the time to stoma closure, affect the incidence of complications remains controversial[24-26].
Currently, colostomy, especially transverse colostomy, is still a commonly used type of ostomy. As a result, the purpose of the current study was to analyse complications after transverse colostomy closure and identify relevant risk factors for complications.
Patients who underwent transverse colostomy closure surgery from Jan 2015 to Jan 2022 at a single clinical centre were retrospectively enrolled. The ethics committee of the First Affiliated Hospital of Chongqing Medical University approved this study (number K2024-008-01), and the data used in this study were obtained from public databases. No informed consent was needed. This study was conducted in accordance with the World Medical Association Declaration of Helsinki.
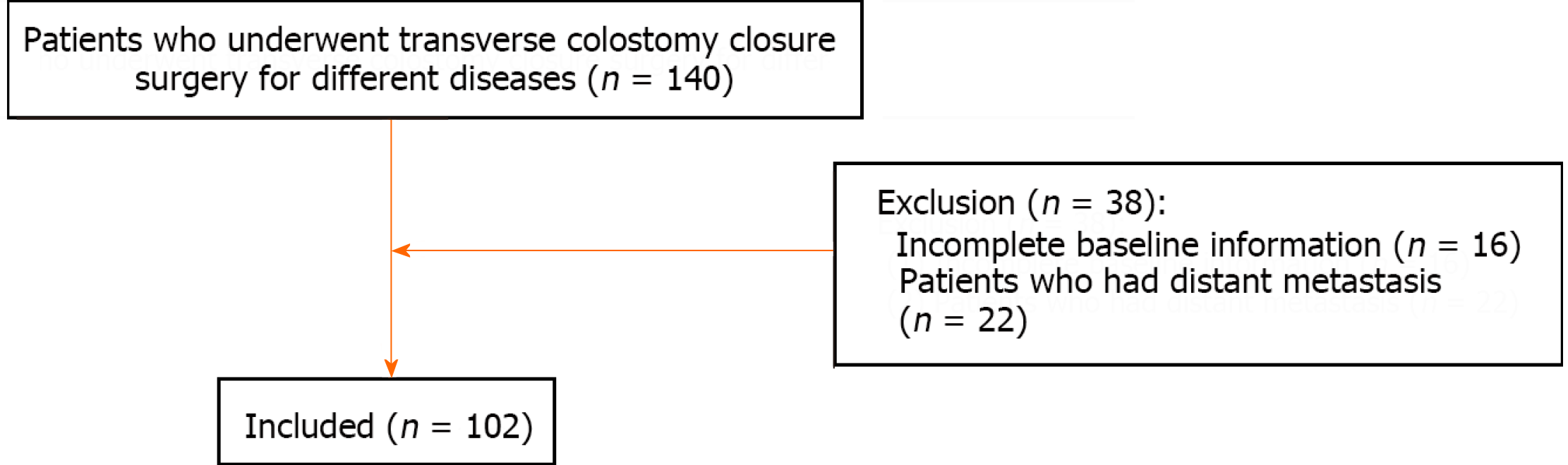
Patients who underwent transverse colostomy closure surgery for different diseases were included in this study (n = 140). The exclusion criteria were as follows: (1) Incomplete clinical records (n = 15); and (2) patients who had distant metastasis (n = 22); and 102 patients enrolled in this study (Figure 1).
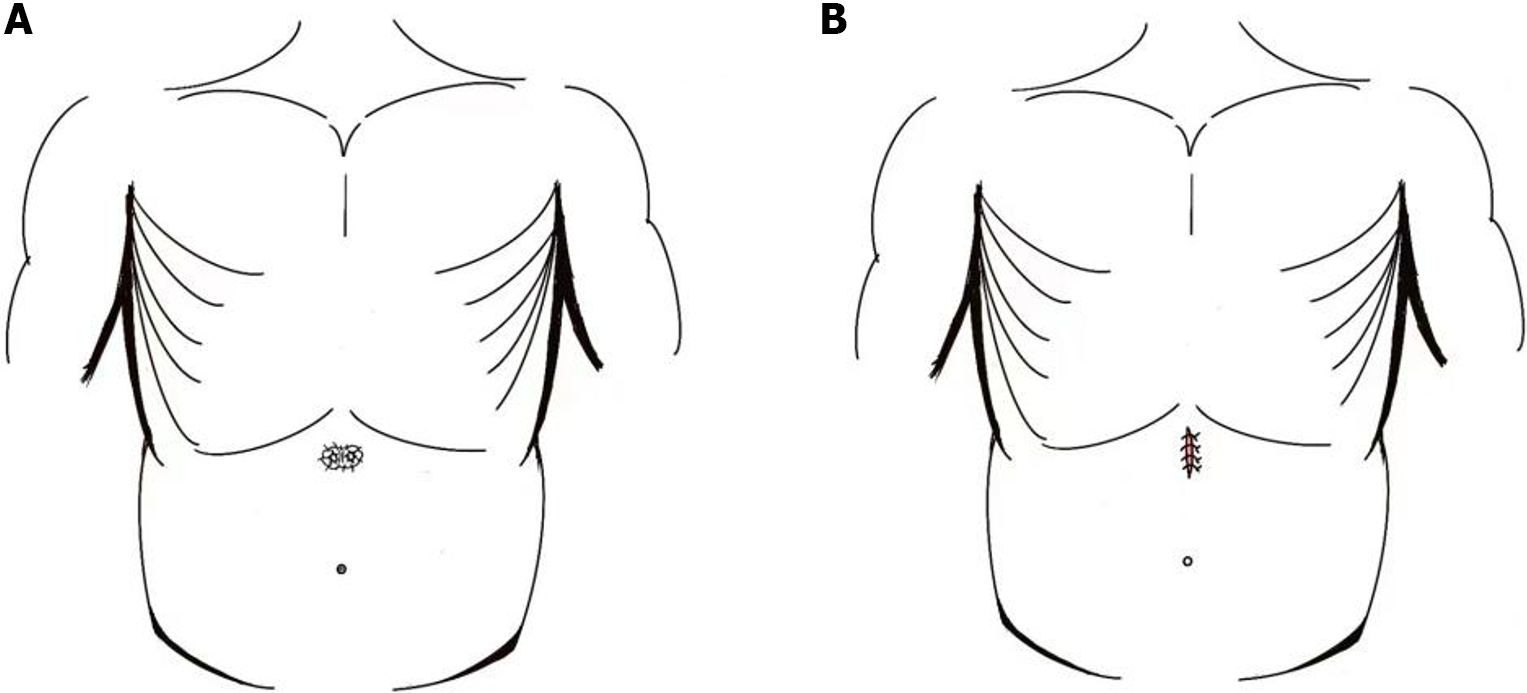
The skin and subcutaneous tissue were first incised along the stoma margin, after which the colon was dissociated from the abdominal wall, the scar tissue around the stoma margin was removed, and the bowel was trimmed. Next, the two ends of the stoma were anastomosed with an anastomosis. Finally, the abdominal wall incision was sutured intermittently with silk threads (Figure 2).
The clinical characteristics included age, sex, body mass index, smoking status, drinking status, hypertension, type 2 diabetes mellitus (T2DM), preoperative haemoglobin, preoperative albumin, interval from transverse colostomy to reversal, method of anastomosis, operation time, blood loss, hospital stay, cause of transverse colostomy and complications were obtained from the electronic medical record system. Postoperative complications were classified on the basis of the Clavien-Dindo classification[27].
Continuous variables are expressed as the mean ± SD, and an independent sample t test was used to compare the differences between the complication group and the no complication group. Categorical variables are expressed as absolute values and percentages, and the chi-square test or Fisher’s exact test was used. Logistic regression analyses were also conducted to identify independent factors for overall complications and incisional infection. The data were analysed using SPSS (version 22.0) statistical software. A bilateral P value < 0.05 was considered to indicate statistical significance.
A total of 102 patients who underwent colostomy closure surgery were enrolled in the current study. The average age of those patients was 57.7 years. Sixty-one (59.8%) patients were males, and 40 (40.2%) patients were females. Postoperative complications occurred in 30 (29.4%) patients. More information is provided in Table 1.
| Characteristics | No. (n = 102) |
| Age, yr | 57.7 ± 12.7 |
| Sex | |
| Male | 61 (59.8) |
| Female | 41 (40.2) |
| BMI, kg/m2 | 22.4 ± 3.2 |
| Smoking | 42 (41.2) |
| Drinking | 36 (35.3) |
| Hypertension | 21 (20.6) |
| T2DM | 9 (8.8) |
| Pre-operative hemoglobin, g/L | 129.6 ± 17.4 |
| Pre-operative albumin, g/L | 42.4 ± 4.4 |
| Interval from transverse colostomy to reversal, month | 7.3 ± 4.5 |
| Methods of anastomosis | |
| End-to-end anastomosis | 25 (24.5) |
| End-to-side anastomosis | 27 (26.5) |
| Side-to side anastomosis | 50 (49.0) |
| Operation time | 132.8 ± 64.0 |
| Blood loss | 43.8 ± 46.7 |
| Hospital stay | 9.4 ± 9.7 |
| Complications | 30 (29.4) |
In terms of the causes of transverse colostomy, 70 (68.6%) patients underwent surgery because of CRC-related causes, including anastomotic leakage after CRC surgery (32.4%), prophylactic transverse colostomy after CRC surgery (29.4%), and obstruction of CRC (3.9%). Other related causes involved perforation because of trauma (15.7%), obstruction (6.8%) and so on (Table 2).
| Characteristics | No. (n = 102) |
| CRC related causes | 70 (68.6) |
| Perforation of CRC | 1 (1.0) |
| Obstruction of CRC | 4 (3.9) |
| Anastomotic leakage after CRC surgery | 33 (32.4) |
| Prophylactic transverse colostomy after CRC surgery | 30 (29.4) |
| Rectovaginal fistula after CRC surgery | 1 (1.0) |
| Anastomotic bleeding after CRC surgery | 1 (1.0) |
| Other related causes | 32 (31.4) |
| Colorectal benign tumors | 3 (2.9) |
| Perforation because of trauma | 16 (15.7) |
| Rectovesical fistula | 6 (5.9) |
| Obstruction | 7 (6.8) |
The most frequent complication occurring after colostomy closure surgery was incision infection (46.7%), followed by pulmonary infection (13.3%), ileus (13.3%), anastomotic leakage (10%), abdominal infection (10%), and bleeding (6.7%). Moreover, 4 (13.3%) patients had complications ≥ grade III (requiring surgical, endoscopic or radiological intervention), including severe ileus (6.6%) and anastomotic leakage (6.6%; Table 3).
| Characteristics | No. (n = 30) |
| Grade I-II complications | 26 (86.7) |
| Pulmonary infection | 4 (13.3) |
| Abdominal infection | 3 (10.0) |
| Incision infection | 14 (46.7) |
| Anastomotic leakage | 1 (3.3) |
| Ileus | 2 (6.7) |
| Bleeding | 2 (6.7) |
| ≥ Grade III complications | 4 (13.3) |
| Anastomotic leakage | 2 (6.7) |
| Ileus | 2 (6.7) |
The complication group had longer hospital stays (P < 0.01). However, there were no differences in terms of the method of anastomosis (P = 0.63), preoperative haemoglobin concentration (P = 0.32), preoperative albumin concentration (P = 0.17), operation time (P = 0.69), blood loss (P = 0.61) or other characteristics (P > 0.05; Table 4).
| Characteristics | Complications (n = 30) | No complications (n = 72) | P value |
| Age, yr | 58.3 ± 11.3 | 57.5 ± 13.3 | 0.756 |
| Sex | 0.677 | ||
| Male | 17 (56.7) | 44 (61.1) | |
| Female | 13 (43.3) | 28 (38.9) | |
| BMI, kg/m2 | 22.3 ± 2.9 | 22.4 ± 3.3 | 0.85 |
| Smoking | 12 (40.0) | 30 (41.7) | 0.876 |
| Drinking | 13 (43.3) | 23 (31.9) | 0.273 |
| Hypertension | 6 (20.0) | 15 (20.8) | 0.924 |
| T2DM | 2 (6.7) | 7 (9.7) | 1 |
| Pre-operative hemoglobin, g/L | 126.9 ± 20.0 | 130.7 ± 16.2 | 0.322 |
| Pre-operative albumin, g/L | 41.5 ± 4.1 | 42.8 ± 4.5 | 0.174 |
| Interval from transverse colostomy to reversal, month | 7.8 ± 6.2 | 7.1 ± 3.6 | 0.452 |
| Methods of anastomosis | 0.633 | ||
| End-to-end anastomosis | 8 (26.7) | 27 (37.5) | |
| End-to-side anastomosis | 6 (20.0) | 21 (29.7) | |
| Side-to side anastomosis | 16 (53.3) | 24 (33.3) | |
| Operation time | 133.0 ± 57.3 | 132.7 ± 67.0 | 0.979 |
| Blood loss | 47.4 ± 54.9 | 42.3 ± 43.1 | 0.617 |
| Hospital stay | 15.4 ± 16.0 | 6.9 ± 2.7 | < 0.01a |
Univariate logistic regression analysis was also conducted to identify potential risk factors for overall complications and incision infection. However, no potential risk factors were identified in this study (P > 0.05; Table 5).
| Risk factors | Univariate analysis of overall complications | Univariate analysis of incision infection | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Age, yr | 1.005 (0.972-1.040) | 0.754 | 0.977 (0.935-1.021) | 0.296 |
| Sex (male/female) | 1.202 (0.507-2.850) | 0.677 | 0.802 (0.248-2.593) | 0.713 |
| BMI, Kg/m2 | 0.987 (0.862-1.129) | 0.848 | 0.988 (0.827-1.182) | 0.898 |
| Hypertension (yes/no) | 0.950 (0.329-2.742) | 0.924 | 1.061 (0.267-4.206) | 0.933 |
| T2DM (yes/no) | 0.663 (0.130-3.394) | 0.622 | 0.769 (0.089-6.669) | 0.812 |
| Smoking (yes/no) | 0.933 (0.392-2.223) | 0.876 | 2.118 (0.676-6.636) | 0.198 |
| Drinking (yes/no) | 1.629 (0.679-3.911) | 0.275 | 2.034 (0.652-6.349) | 0.221 |
| Pre-operative hemoglobin, g/L | 0.988 (0.964-1.012) | 0.320 | 0.989 (0.958-1.021) | 0.509 |
| Pre-operative albumin, g/L | 0.934 (0.847-1.031) | 0.175 | 0.957 (0.843-1.086) | 0.494 |
| Operation time, min | 1.000 (0.993-1.007) | 0.979 | 0.995 (0.984-1.007) | 0.413 |
| Blood loss, mL | 1.002 (0.993-1.011) | 0.614 | 0.995 (0.980-1.010) | 0.528 |
| Interval from transverse colostomy to reversal, month | 1.035 (0.946-1.133) | 0.454 | 1.033 (0.926-1.153) | 0.562 |
| Methods of anastomosis (Side-to side/end-to-side/end-to-end) | 1.046 (0.622-1.761) | 0.864 | 1.664 (0.734-3.774) | 0.223 |
In this study, a total of 102 patients who underwent transverse colostomy closure surgery were enrolled. Postoperative complications occurred in 30 (29.4%) patients. The most frequent complication occurring after colostomy closure surgery was incision infection, with an incidence of 13.7%. The complication group had longer hospital stays than did the no complication group. Furthermore, logistic regression analyses included factors such as operation time, interval from transverse colostomy to reversal, and method of anastomosis; however, no potential risk factors were identified for overall complications or incision infection.
Previous studies have reported complications after transverse colostomy closure surgery. Aston and Everett[24] enrolled 100 patients who had a temporary transverse loop colostomy closed between 1969 and 1982; they found that the most frequent complication was faecal fistula (10%) and stressed that closing the stoma within 3 wk was as safe as closing it within 8 wk. Henry and Everett[21] reported that fistula formation at the site of closure was the most frequent complication. However, with the development of surgical techniques and clinical management, the incidence of complications in recent years has changed. Pokorny et al[16] and Rullier et al[18] reported that wound infection was the most frequent complication, with incidences of 9.0% and 8.9%, respectively, which was in accordance with our studies. In our study, the incidence of incision infection was 13.7%. Although incisional infection after transverse colostomy closure is usually not life-threatening, it increases the cost of hospitalization and pain of patients. Gonzalez et al[28] reported that age, operation time, and cardiac risk factors were found to be independent risk factors for surgical site infection; however, our study did not identify any risk factors, possibly because of the relatively small sample size. More measures should be taken to decrease the incidence of incision infection, including better management of T2DM, purse-string skin closure, an open incision, and a large surgeon volume[26,29,30].
Although the complication group had longer hospital stays, no significant differences were found in terms of the method of anastomosis, operation time or other characteristics, and no risk factors were found. These findings prompted us to further investigate the possible reasons for complications, such as the experience of surgeons and surgical techniques.
The interval from ostomy to reversal was the most common risk factor for postoperative complications, but this topic remains controversial. In 2019, Krebs et al[25] reported that the time to stoma closure was an independent risk factor for complications after diverting stoma closure, and the optimal cut-off was 240 d[25]. Conversely, a meta-analysis of 7 randomized controlled trials demonstrated that early stoma closure (4 wk) was as safe as routine surgery (8 wk)[31]. Pokorny et al[16] and Aston and Everett[24] reported that the interval was not an independent predictor of complications. Because stoma closure was performed at different times, the conclusions might vary. Our study showed that the interval (ranging from 1.2-14 months) from transverse colostomy closure to reversal did not seem to influence the incidence of complications. The conclusion above might indicate that the time to perform transverse colostomy closure should be individualized and adjusted for various reasons, such as chemotherapy, primary disease, and complications after primary surgery.
To our knowledge, this is the first study to analyse postoperative complications and predictors, especially for patients who underwent transverse colostomy closure. Although several studies have reported complications after stoma closure and relevant risk factors, they did not separate ileostomy closure from colostomy closure. Because of the greater incidence of complications after colostomy closure than after ileostomy, the current study was necessary.
Some limitations of our study should be considered. First, the retrospective nature of the single-centre study indicated unavoidable selection bias. Second, only 102 patients were enrolled in this study, which was a small sample size. Moreover, additional parameters need to be included to identify risk factors. Thus, further multicentre prospective studies with large sample sizes are needed.
In conclusion, the most frequent complication occurring after colostomy closure surgery was incision infection. The operation time, interval from transverse colostomy to reversal, and method of anastomosis might have no impact on postoperative complications.
Previous studies comparing the incidence of postoperative complications in patients with ileostomy and colostomy closure have found that patients undergoing colostomy closure are more likely to experience complications. Most of the studies reporting post-colonostomy complications were conducted at the end of the last century with relatively small sample sizes.
At present, colostomy, especially transverse colostomy, is still a common type of colostomy.
The aim of this study was to analyze complications after transverse colostomy closure and to identify risk factors associated with complications.
This article used a retrospective study method to include 102 patients at a single clinical centre. The differences between the complication group and the no complication group were compared. Logistic regression analyses were conducted to find independent factors for overall complications or incision infection.
A total of 102 patients who underwent transverse colostomy closure were enrolled in the current study. Seventy (68.6%) patients underwent transverse colostomy because of colorectal cancer related causes. Postoperative complications occurred in 30 (29.4%) patients and the most frequent complication occurring after transverse colostomy closure was incision infection (46.7%). The complication group had longer hospital stays (P < 0.01). However, no potential risk factors were identified for overall complications and incision infection.
Finally, we found that the most common complication after colostomy closure was wound infection. Operation time, time interval between transverse colostomy and reversal, and anastomosis method had no effect on postoperative complications.
The study will conduct to analyze the overall survival after transverse colostomy closure.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baryshnikova NV, Russia S-Editor: Li L L-Editor: A P-Editor: Cai YX
| 1. | Ambe PC, Kurz NR, Nitschke C, Odeh SF, Möslein G, Zirngibl H. Intestinal Ostomy. Dtsch Arztebl Int. 2018;115:182-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 2. | Vonk-Klaassen SM, de Vocht HM, den Ouden ME, Eddes EH, Schuurmans MJ. Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual Life Res. 2016;25:125-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 276] [Cited by in RCA: 248] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 3. | Johnston LR, Bradley MJ, Rodriguez CJ, Mcnally MP, Elster EA, Duncan JE. Ostomy Usage for Colorectal Trauma in Combat Casualties. World J Surg. 2019;43:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Veenhof AA, van der Peet DL, Meijerink WJ, Cuesta MA. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2008;247:718-9; author reply 719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H; Working Group 'Colon/Rectum Carcinoma'. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg. 2005;92:1137-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 265] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 6. | Chude GG, Rayate NV, Patris V, Koshariya M, Jagad R, Kawamoto J, Lygidakis NJ. Defunctioning loop ileostomy with low anterior resection for distal rectal cancer: should we make an ileostomy as a routine procedure? A prospective randomized study. Hepatogastroenterology. 2008;55:1562-1567. [PubMed] |
| 7. | Faunø L, Rasmussen C, Sloth KK, Sloth AM, Tøttrup A. Low complication rate after stoma closure. Consultants attended 90% of the operations. Colorectal Dis. 2012;14:e499-e505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Szczepkowski M, Banasiewicz T, Krokowicz P, Dziki A, Wallner G, Drews M, Herman R, Lorenc Z, Richter P, Bielecki K, Tarnowski W, Kruszewski J, Kładny J, Głuszek S, Zegarski W, Kielan W, Paśnik K, Jackowski M, Wyleżoł M, Stojcev Z, Przywózka A. Polish consensus statement on the protective stoma. Pol Przegl Chir. 2014;86:391-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Mileski WJ, Rege RV, Joehl RJ, Nahrwold DL. Rates of morbidity and mortality after closure of loop and end colostomy. Surg Gynecol Obstet. 1990;171:17-21. [PubMed] |
| 10. | Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009;24:711-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 290] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 11. | Bada-Yllán O, García-Osogobio S, Zárate X, Velasco L, Hoyos-Tello CM, Takahashi T. [Morbi-mortality related to ileostomy and colostomy closure]. Rev Invest Clin. 2006;58:555-560. [PubMed] |
| 12. | Pittman DM, Smith LE. Complications of colostomy closure. Dis Colon Rectum. 1985;28:836-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Perez RO, Habr-Gama A, Seid VE, Proscurshim I, Sousa AH Jr, Kiss DR, Linhares M, Sapucahy M, Gama-Rodrigues J. Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum. 2006;49:1539-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surg Infect (Larchmt). 2017;18:722-735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 250] [Cited by in RCA: 535] [Article Influence: 66.9] [Reference Citation Analysis (0)] |
| 15. | Rubinkiewicz M, Witowski J, Wysocki M, Pisarska M, Kłęk S, Budzyński A, Pędziwiatr M. Investigating Risk Factors for Complications after Ileostomy Reversal in Low Anterior Rectal Resection Patients: An Observational Study. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Pokorny H, Herkner H, Jakesz R, Herbst F. Predictors for complications after loop stoma closure in patients with rectal cancer. World J Surg. 2006;30:1488-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Fonseca AZ, Uramoto E, Santos-Rosa OM, Santin S, Ribeiro M Jr. COLOSTOMY CLOSURE: RISK FACTORS FOR COMPLICATIONS. Arq Bras Cir Dig. 2017;30:231-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Rullier E, Le Toux N, Laurent C, Garrelon JL, Parneix M, Saric J. Loop ileostomy versus loop colostomy for defunctioning low anastomoses during rectal cancer surgery. World J Surg. 2001;25:274-277; discussion 277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 94] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Chudner A, Gachabayov M, Dyatlov A, Lee H, Essani R, Bergamaschi R. The influence of diverting loop ileostomy vs. colostomy on postoperative morbidity in restorative anterior resection for rectal cancer: a systematic review and meta-analysis. Langenbecks Arch Surg. 2019;404:129-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 20. | Bell C, Asolati M, Hamilton E, Fleming J, Nwariaku F, Sarosi G, Anthony T. A comparison of complications associated with colostomy reversal versus ileostomy reversal. Am J Surg. 2005;190:717-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Henry MM, Everett WG. Loop colostomy closure. Br J Surg. 1979;66:275-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Parks SE, Hastings PR. Complications of colostomy closure. Am J Surg. 1985;149:672-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Livingston DH, Miller FB, Richardson JD. Are the risks after colostomy closure exaggerated? Am J Surg. 1989;158:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Aston CM, Everett WG. Comparison of early and late closure of transverse loop colostomies. Ann R Coll Surg Engl. 1984;66:331-333. [PubMed] |
| 25. | Krebs B, Ivanecz A, Potrc S, Horvat M. Factors affecting the morbidity and mortality of diverting stoma closure: retrospective cohort analysis of twelve-year period. Radiol Oncol. 2019;53:331-336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Goret NE, Goret CC, Cetin K, Agachan AF. Evaluation of risk factors for complications after colostomy closure. Ann Ital Chir. 2019;90:324-329. [PubMed] |
| 27. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6210] [Cited by in RCA: 8608] [Article Influence: 538.0] [Reference Citation Analysis (0)] |
| 28. | Gonzalez DO, Ambeba E, Minneci PC, Deans KJ, Nwomeh BC. Surgical site infection after stoma closure in children: outcomes and predictors. J Surg Res. 2017;209:234-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Wada Y, Miyoshi N, Ohue M, Noura S, Fujino S, Sugimura K, Akita H, Motoori M, Gotoh K, Takahashi H, Kobayashi S, Ohmori T, Fujiwara Y, Yano M. Comparison of surgical techniques for stoma closure: A retrospective study of purse-string skin closure versus conventional skin closure following ileostomy and colostomy reversal. Mol Clin Oncol. 2015;3:619-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Murtaza G, Nuruddin R, Memon AA, Chawla T, Azam I, Mukhtar Y. Does primary closure increase surgical site infection after intestinal stoma reversal? A retrospective cohort study. Surg Infect (Larchmt). 2014;15:58-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Guo Y, Luo Y, Zhao H, Bai L, Li J, Li L. Early Versus Routine Stoma Closure in Patients With Colorectal Resection: A Meta-Analysis of 7 Randomized Controlled Trials. Surg Innov. 2020;27:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |