Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.622
Peer-review started: November 14, 2023
First decision: December 6, 2023
Revised: December 8, 2023
Accepted: January 8, 2024
Article in press: January 8, 2024
Published online: February 27, 2024
Processing time: 103 Days and 8.4 Hours
Gallbladder rupture is common in laparoscopic cholecystectomy because the gallbladder is usually in acute or chronic inflammation status. The gallstones may sometime be spilled into the peritoneal cavity, resulting in intra-abdominal ab
This case described a 78-year-old man who received laparoscopic cholecystectomy and gallbladder adenocarcinoma was diagnosed after surgery. After adjuvant chemotherapy, the following up abdominal CT showed several small nodules at right upper abdomen and peritoneal carcinomatosis is considered. Repeated laparoscopic surgery for the excision of seeding tumor was conducted and the pathological diagnosis of the nodules and mass was inflammatory tissues and gallbladder stone.
Spilled gallstones are a common complication during laparoscopic cholecystectomy and some gallstones fail to be retrieved due to the size or the restricted view of laparoscopic surgery. For spilled gall bladder stones, surgeons may consider regular computerized tomography follow-up, and if necessary, laparoscopic examination can be used as a means of confirming the diagnostic and treatment.
Core Tip: Gallstones spillage frequently occurs during laparoscopic cholecystectomy. Surgeons should consider complete removal of spilled gallbladder stones, and follow-up with computed tomography (CT) imaging to detect abnormal nodule or abscess formation early after operation. However, CT cannot make a good differential diagnosis of abscess or malignant tumor metastasis. Laparoscopy can effectively obtain cell and tissue for the pathological diagnosis and treatment, and is a good tool for diagnosis and treatment.
- Citation: Huang CK, Lu RH, Chen CC, Chen PC, Hsu WC, Tsai MJ, Ting CT. Spilled gallstone mimicking intra-abdominal seeding of gallbladder adenocarcinoma: A case report. World J Gastrointest Surg 2024; 16(2): 622-627
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/622.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.622
Laparoscopic cholecystectomy is now the main approach for the treatment of benign or malignant gallstone diseases. During surgery, gallbladder rupture is common because the gallbladder is usually affected by acute or chronic inflammation. Evidence suggests that iatrogenic gallbladder perforation does not increase the incidence of complications during laparoscopic cholecystectomy[1,2]. However, gallstones may sometimes spill into the peritoneal cavity, resulting in intra-abdominal abscess if the gallstones are not retrieved[3]. The diagnosis of intra-abdominal abscess caused by unretrieved gallstones can usually be correctly achieved via routine imaging methods, such as abdominal ultrasonography or computed tomography (CT)[4]. Here, we present a case in which abscess formation occurred from an unretrieved gallstone following laparoscopic cholecystectomy, which mimics the imaging findings of metastatic gallbladder ade
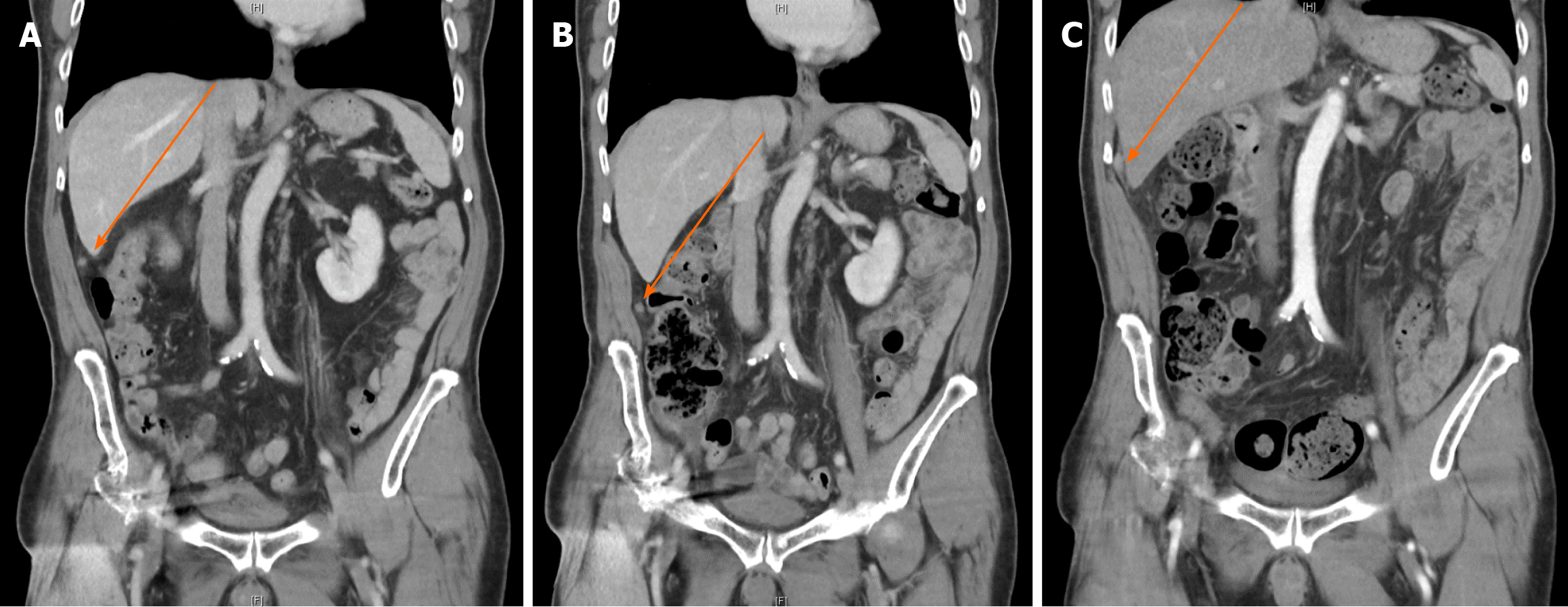
Suspect peritoneal carcinomatosis detected via abdominal CT.
This case involved a 78-year-old man who was diagnosed with gallbladder adenocarcinoma in 2022. The patient had a history of gallbladder stones for more than ten years and experienced postprandial abdominal pain for one month before seeking medical assistance at another hospital. Abdominal CT was performed. The original abdominal CT images were not obtainable. The patient was told that he had gallbladder stones and a gallbladder tumor with 1.8 cm in diameter. The patient then went to another hospital for surgical advice. Physical examination and imaging studies were also conducted to assess his condition. Laboratory findings, including alpha-fetoprotein, liver function, the tumor marker carcinoembryonic antigen (CEA), carbohydrate antigen 125 (CA125) and CA199, were unremarkable. The creatinine concentration was slightly elevated at 1.3 mg/dL (normal < 1.2 mg/dL). Abdominal echo revealed multiple gallbladder stones and a polypoid lesion 1.8 cm in length located at the gallbladder fundus. The extrahepatic bile duct was normal. Laparoscopic cholecystectomy was suggested, but the risk of malignancy and possible further surgery were considered. The patient understood the risk and decided to undergo laparoscopic cholecystectomy only first. The surgery was performed in July 2022. Pathology of the gallbladder revealed the presence of a biliary type, moderately differentiated adenocarcinoma invading the perimuscular connective tissues on the peritoneal side. The pathological stage was pT2aN1MX. Extended resection was suggested, but the patient refused. The patient came to our hospital for a second opinion. The patient still declined further surgical intervention and was willing to receive adjuvant chemotherapy only. Six cycles of standard chemotherapy, including capecitabine and gemcitabine, were administered from August 2022 to March 2023.
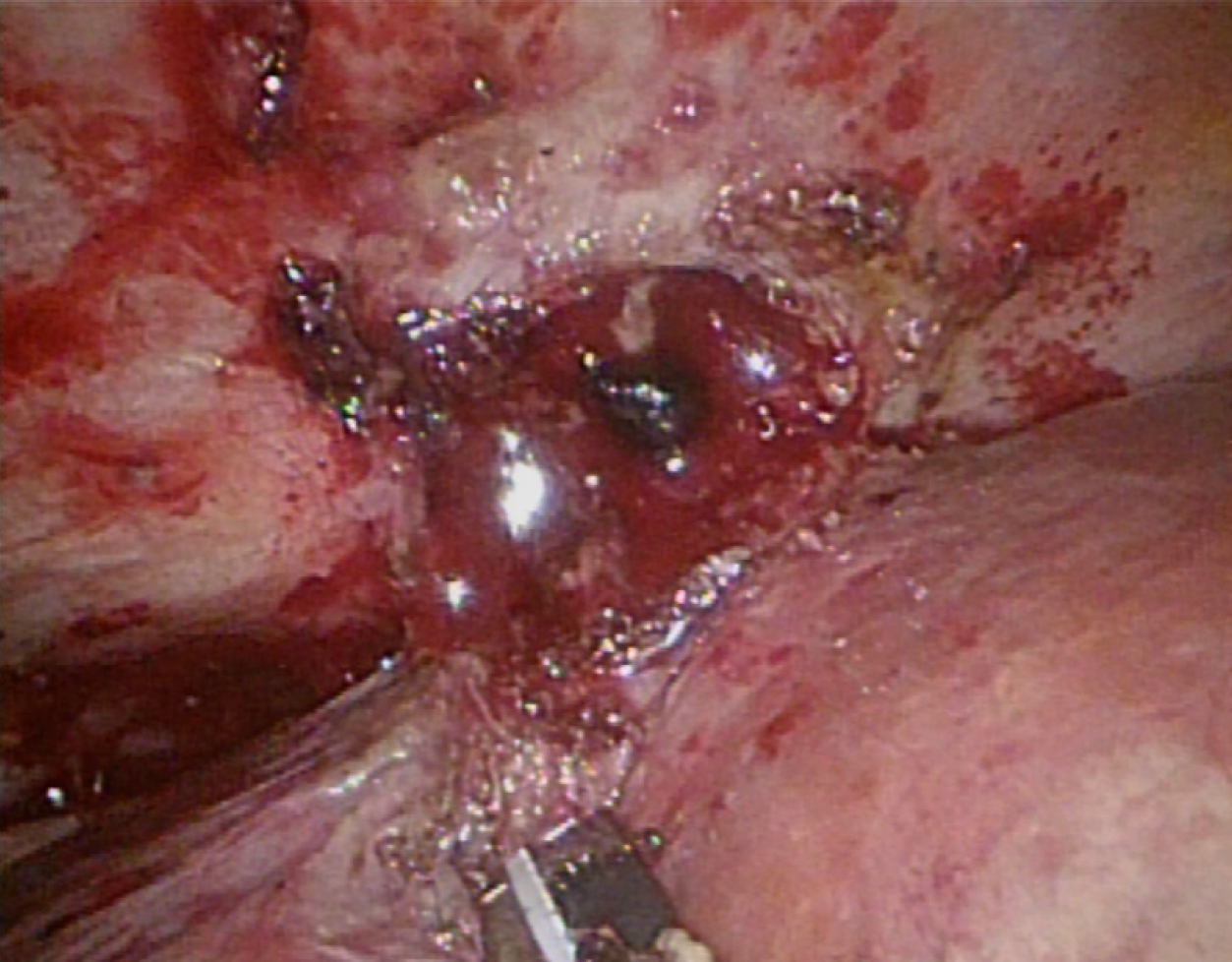
The patient’s chemotherapy regimen was changed to oral tegafur, gimeracil and oteracil. Repeat laparoscopic surgery for the excision of the seeding tumor was conducted in June 2023. During the surgery, several small nodules were found on the pelvic wall and omentum and were excised. One larger nodule was noted on the surface of the S7 segment of the liver. During excision, the liver nodule ruptured, and the content was a cholelith-like mass with abscess (Figure 1).
The patient had a history of benign prostatic hyperplasia.
He denied smoking or alcohol consumption, and did not report any family history of malignant tumors.
The patient’s vital signs were as follows: Body temperature, 36.3 °C; blood pressure, 108/56 mmHg; heart rate, 70 beats per min; respiratory rate, 17 breaths per min. The patient had clear consciousness and no skin jaundice. There was no abdominal tenderness.
From August 2022 to March 2023, the tumor marker levels, including the CEA, CA125 and CA199 levels, were within the normal ranges.
Follow-up abdominal CT was performed in August 2022 and showed several small nodules in the right upper abdomen. The largest nodule measured 1.0 cm in diameter. Peritoneal carcinomatosis was considered. Another two follow-up abdominal CT scans were performed in December 2022 and March 2023. The presence of several small nodules located near the liver was still noted. In addition, the largest nodule was 1.3 cm in diameter and had increased in size (Figure 2). Local recurrence, lymph node metastasis or peritoneal metastasis was considered. Whole-body positron emission tomography revealed several small nodules in the right subphrenic and subhepatic spaces (Figure 3). Peritoneal seeding was first considered.
Pathology revealed that the nodules and mass were inflammatory tissues and gallbladder stones, without any evidence of tumor seeding or metastasis (Figure 4).
The patient was discharged four days after surgery in stable condition.
At 6 months after surgery, the patient was still alive.
Gallstone spillage frequently occurs during laparoscopic cholecystectomy. Most of the time, spilled gallstones do not need medical treatment as long as no discomfort occurs. However, spilled gallstones can potentially lead to the formation of abscesses, and in some cases, surgical intervention may be required if the abscess persists and causes symptoms despite conservative treatment. Furthermore, spilled gallstones may also increase the risk of recurrence or metastasis of gallbladder cancer by 39%-54%[5]. The accurate diagnosis of spilled gallstones can be challenging, particularly when dealing with small abscesses. There are also instances where the presence of residual gallstones can be misinterpreted as cancerous growth or metastasis, as demonstrated in our case.
Alongside our case, we conducted a literature review of seven cases of spilled gallstones that mimicked cancerous presentations following laparoscopic cholecystectomy (Table 1). All patients initially underwent laparoscopic cholecys
| Ref. | Patient’s age and sex | Time after laparoscopic cholecystectomy | Symptoms | Imaging | Treatment | Tumor marker (CEA and CA199) |
| Dasari et al[7], 2009 | 67 yr/female | 2 yr | Repeat attack of lower abdominal pain | CT | Diagnostic laparoscopy | Normal range |
| Arai et al[8], 2012 | 65 yr/male | 4 yr | No | Ultrasound CT, MRI | Partial resection of the liver and right diaphragm | Normal range |
| McVeigh et al[9], 2012 | 37 yr/female | 3 yr | No | No | Removed during C/S | Not mentioned |
| Kim et al[10], 2016 | 59 yr/male | 5 months | Constant abdominal pain | CT, MRI | Exploratory laparotomy | Normal range |
| Suarez-Zamora et al[11], 2017 | 29 yr/female | 2 yr | No | No | Removed during C/S | Not mentioned |
| Jeong et al[12], 2018 | 59 yr/male | 3 months | No | CT, PET CT | Exploratory laparotomy | Normal range |
| Capolupo et al[13], 2018 | 73 yr/male | 6 months | No | CT | Explorative laparoscopy | Not mentioned |
In contrast to previous cases, our case involved gallbladder adenocarcinoma, stage IIIb, which necessitated surgical reintervention due to the potential risk of local recurrence or peritoneal metastases, which could not be ruled out following the initial surgery. When considering the choice of surgical method, laparoscopy may be given priority due to its advantages, including reduced postoperative pain, lower morbidity, and a shorter hospital stay than laparotomy. Furthermore, laparoscopy is particularly suitable when spilled gallstones are included among the differential diagnoses.
Currently, there is no definite consensus on whether surgeons should strive to completely remove spilled gallstones during laparoscopic surgery or switch to open surgery[6]. Given the common occurrence of gallstone spillage, physicians should consider spilled gallstones as a potential etiology of abnormal nodules or abscess formation after laparoscopic surgery.
This case report can provide physicians with valuable information. Surgeons should consider complete removal of spilled gallbladder stones and follow up with CT scans to detect abnormal nodules or abscess formation early after surgery. However, CT cannot aid in the accurate differential diagnosis of abscess or malignant tumor metastasis. Laparoscopy can be used to obtain cells and tissue effectively and is a good tool for diagnosis and treatment.
Spilled gallstones are a common complication during laparoscopic cholecystectomy, and some gallstones cannot be retrieved due to their size or a restricted view during laparoscopic surgery. In addition to trying to retrieve spilled gallstones, surgeons should obtain detailed surgical records about iatrogenic gallbladder perforation for other physicians or surgeons to have a better way to make correct differential diagnoses and provide medical treatment. For spilled gallbladder stones, surgeons may consider regular CT scan follow-up, and if necessary, laparoscopic examination can be used as a means of confirming the diagnosis and treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kim BS, South Korea S-Editor: Wang JJ L-Editor: A P-Editor: Zheng XM
| 1. | Hui TT, Giurgiu DI, Margulies DR, Takagi S, Iida A, Phillips EH. Iatrogenic gallbladder perforation during laparoscopic cholecystectomy: etiology and sequelae. Am Surg. 1999;65:944-948. [PubMed] |
| 2. | Evans L, Sams E, Naguib A, Hajibandeh S. Iatrogenic gallbladder perforation during laparoscopic cholecystectomy and outcomes: a systematic review and meta-analysis. Langenbecks Arch Surg. 2022;407:937-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 3. | Zulfikaroglu B, Ozalp N, Mahir Ozmen M, Koc M. What happens to the lost gallstone during laparoscopic cholecystectomy? Surg Endosc. 2003;17:158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Bennett AA, Gilkeson RC, Haaga JR, Makkar VK, Onders RP. Complications of "dropped" gallstones after laparoscopic cholecystectomy: technical considerations and imaging findings. Abdom Imaging. 2000;25:190-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Horkoff MJ, Ahmed Z, Xu Y, Sutherland FR, Dixon E, Ball CG, Bathe OF. Adverse Outcomes After Bile Spillage in Incidental Gallbladder Cancers: A Population-based Study. Ann Surg. 2021;273:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | Demirbas BT, Gulluoglu BM, Aktan AO. Retained abdominal gallstones after laparoscopic cholecystectomy: a systematic review. Surg Laparosc Endosc Percutan Tech. 2015;25:97-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Dasari BV, Loan W, Carey DP. Spilled gallstones mimicking peritoneal metastases. JSLS. 2009;13:73-76. [PubMed] |
| 8. | Arai T, Ikeno T, Miyamoto H. Spilled gallstones mimicking a liver tumor. Clin Gastroenterol Hepatol. 2012;10:A32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | McVeigh G, McComiskey M, McCluggage WG. Peritoneal bile granulomas identified at Cesarean section and mimicking disseminated malignancy. Int J Surg Pathol. 2012;20:89-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Kim BS, Joo SH, Kim HC. Spilled gallstones mimicking a retroperitoneal sarcoma following laparoscopic cholecystectomy. World J Gastroenterol. 2016;22:4421-4426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Suarez-Zamora DA, Barrera-Herrera LE, Caceres-Mileo R, Palau-Lazaro MA. Intraperitoneal Granulomas Unexpectedly Found during a Cesarean Delivery: A Late Complication of Dropped Gallstones. Case Rep Pathol. 2017;2017:4873273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Jeong H, Lee HW, Jung HR, Hwang I, Kwon SY, Kang YN, Kim SP, Choe M. Bile Granuloma Mimicking Peritoneal Seeding: A Case Report. J Pathol Transl Med. 2018;52:339-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Capolupo GT, Mascianà G, Carannante F, Caricato M. Spilled gallstones simulating peritoneal carcinomatosis: A case report and literature review. Int J Surg Case Rep. 2018;48:113-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |