Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.616
Peer-review started: November 8, 2023
First decision: December 6, 2023
Revised: December 18, 2023
Accepted: January 25, 2024
Article in press: January 25, 2024
Published online: February 27, 2024
Processing time: 108 Days and 22.2 Hours
The overlap of imaging manifestations among distinct splenic lesions gives rise to a diagnostic dilemma. Consequently, a definitive diagnosis primarily relies on his
A 41-year-old female, with a history of pulmonary tuberculosis, was admitted to our hospital with multiple indeterminate splenic lesions. Gray-scale ultrasonography demonstrated splenomegaly with numerous well-defined hypoechoic ma
Percutaneous US-guided coaxial CNB is an excellent and safe option for obtaining precise splenic tissue samples, as it significantly enhances sample yield for exact pathological analysis with minimum trauma to the spleen parenchyma and sur
Core Tip: Multiple splenic lesions caused by infection, lymphoma, sarcoid, metastasis and infarction may have similar imaging features. The overlapping imaging characteristics of splenic lesions cause a diagnostic dilemma. Consequently, a definitive diagnosis primarily relies on histological results. We describe a case of multiple indeterminate splenic lesions and confirmed the diagnosis with an ultrasound (US)-guided coaxial core needle biopsy (CNB). US-guided CNB is a safe and efficient puncture technique providing valuable diagnostic information and patient treatment guidance.
- Citation: Pu SH, Bao WYG, Jiang ZP, Yang R, Lu Q. Percutaneous ultrasound-guided coaxial core needle biopsy for the diagnosis of multiple splenic lesions: A case report. World J Gastrointest Surg 2024; 16(2): 616-621
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/616.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.616
Multiple splenic lesions can be caused by a variety of benign or malignant diseases, including infection, primary tumor, and metastasis[1]. Non-specific characteristics on imaging frequently pose a diagnostic dilemma[2,3]. Histological exa
A 41-year-old female was admitted to our hospital with focal splenic lesions discovered during routine abdominal ultrasonography as a part of health checkup.
The patient was in good health and did not report any discomfort.
One year ago, the patient was admitted to the tuberculosis (TB) medical unit due to recurrent fever and cough, and was diagnosed with pulmonary TB. Subsequently, 2HRZE/7HRE (strengthening period: Isoniazid 300 mg, rifampicin 450 mg, pyrazinamide 0.75 g, ethambutol 0.75 g, once a day, given for 2 months; consolidation period: Isoniazid 300 mg, rifam
Patient and family histories were negative.
The patient did not complain of any abdominal pain or distension.
Carbohydrate antigen 125 was mildly elevated, and other tumor markers including alpha-fetoprotein, carcinoembryonic antigen, and carbohydrate antigen 199 were within the normal range. Other biochemical results were unremarkable.
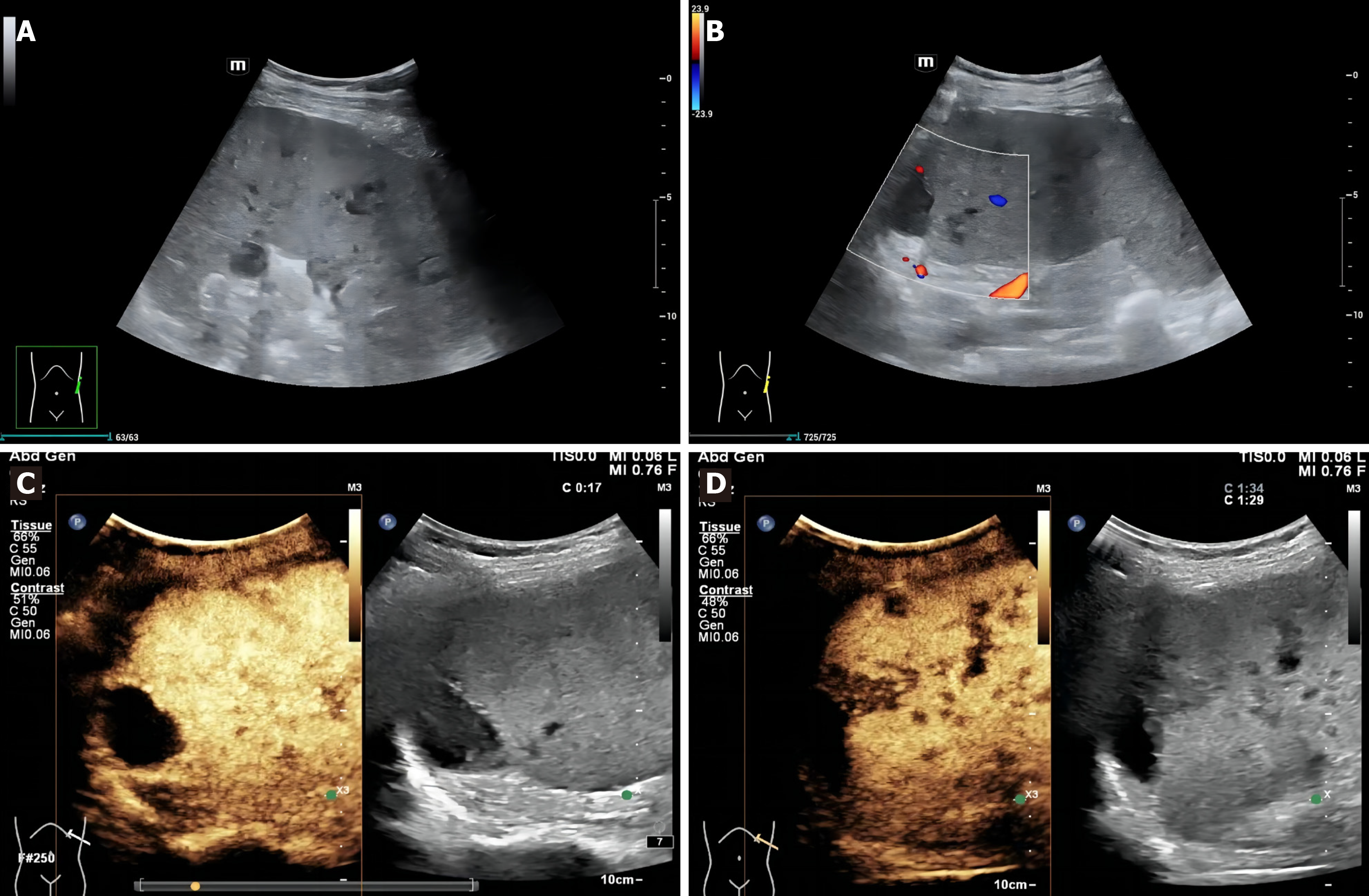
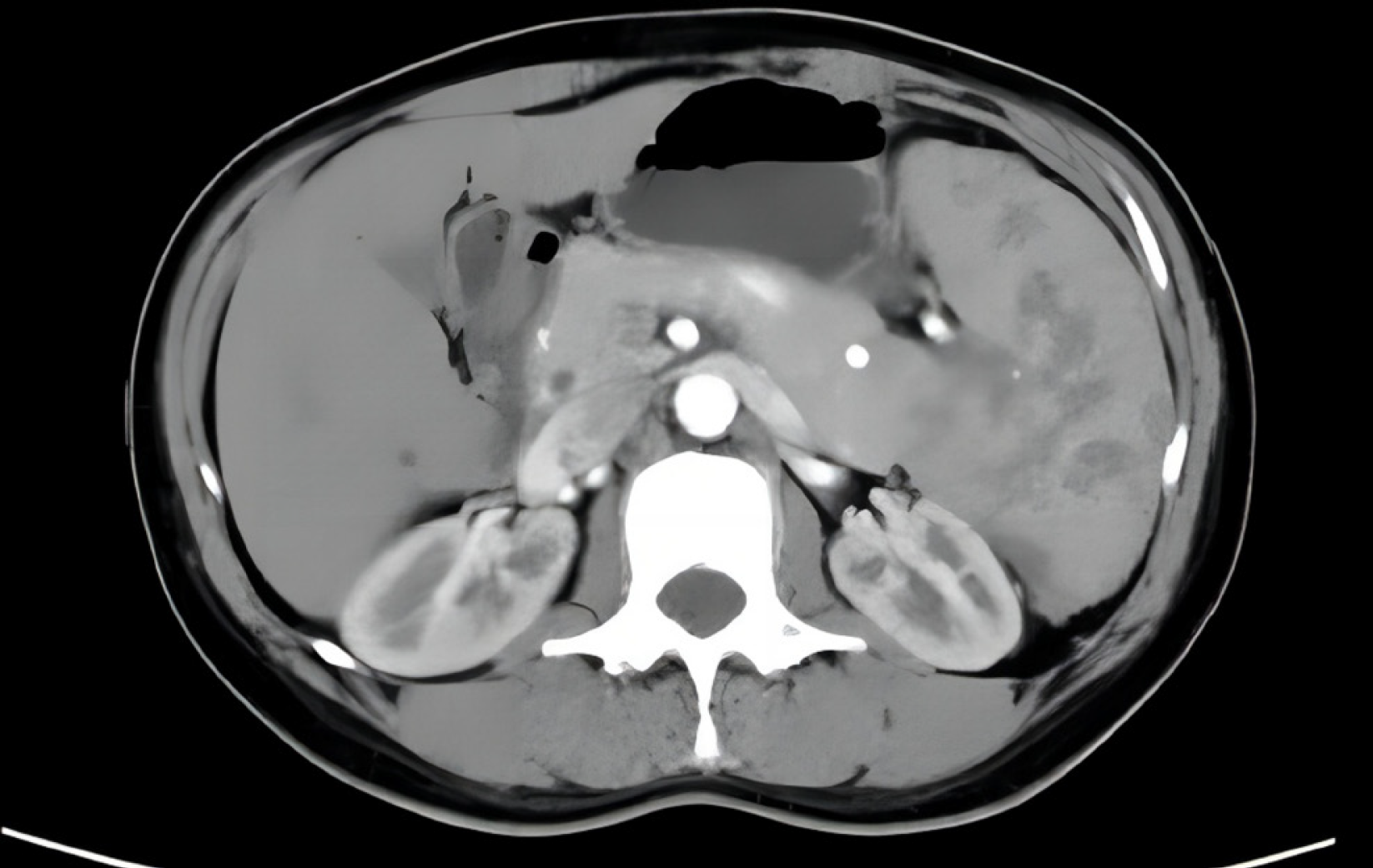
Grayscale US demonstrated splenomegaly with numerous well-defined hypoechoic masses (Figure 1A). Color Doppler imaging indicated no significant blood flow signals within these lesions (Figure 1B). Contrast-enhanced US (CEUS) sh
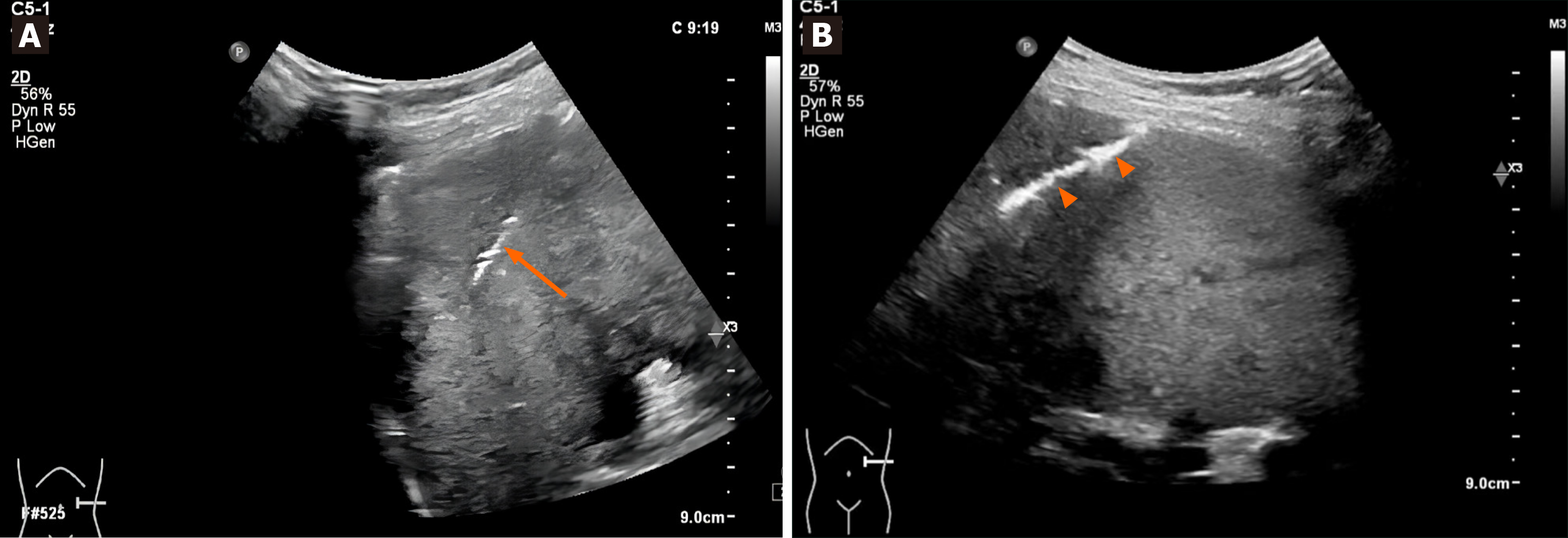
The differential diagnoses based on clinical and radiological results included splenic tuberculosis, fungal infection, metastasis, lymphoma and hemangioma. For further diagnostic analyses, the US-guided coaxial CNB for histological diagnosis was performed by a doctor with over 5 years of experience in interventional US. Platelet count and pro
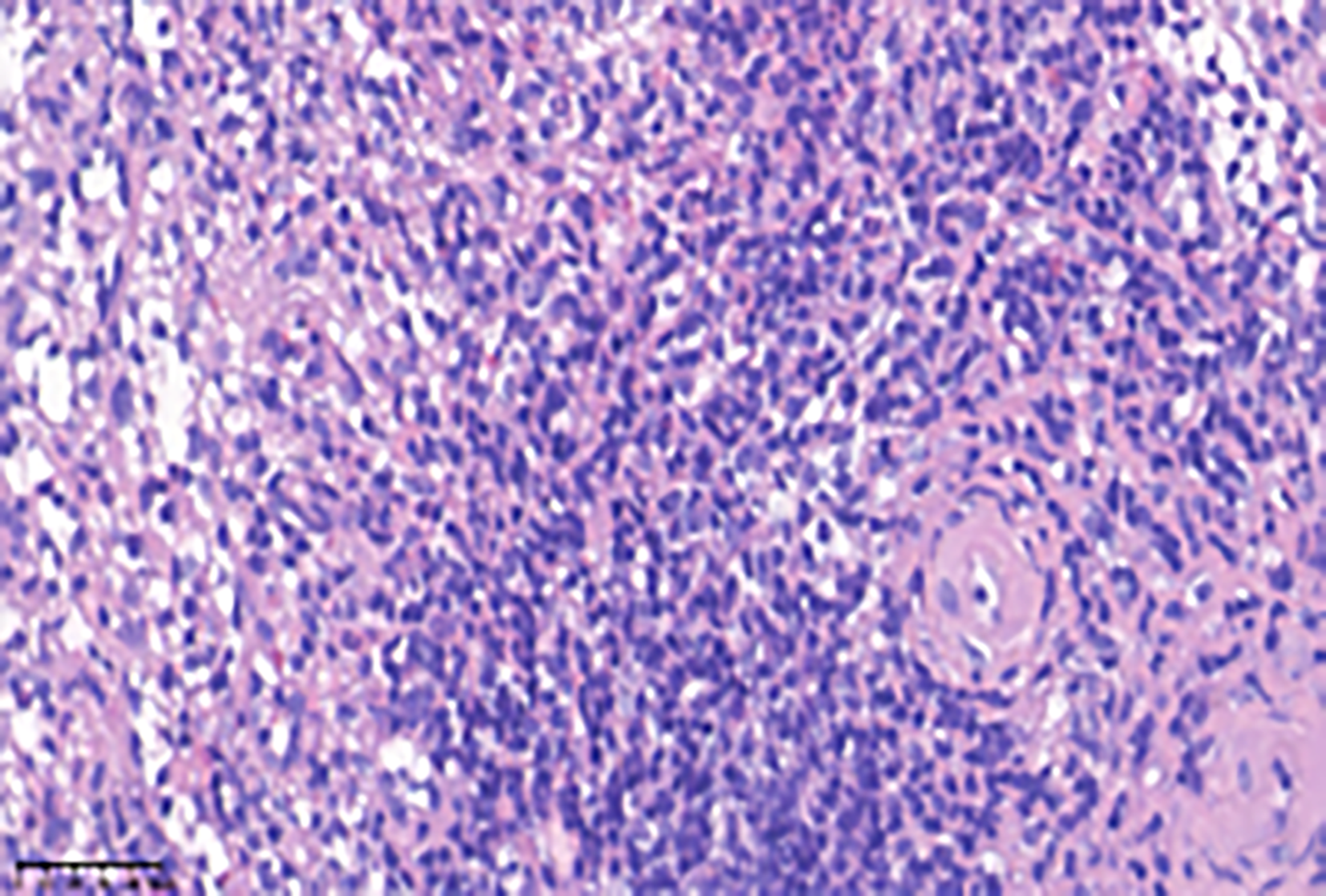
Histological analysis showed no evidence of malignancy, but the proliferation of fibrous tissue and hyaline degeneration were observed in some areas. Granulomas were noted in focal areas, accompanied by peripheral lymphoid hyperplasia involving infiltration of neutrophils, monocytes, and plasma cells (Figure 4). Immunohistochemistry revealed CD20+ and CD3+ cells, in addition to some CD8+ cells. Acid-fast and methenamine silver stain did not reveal any pathogens. No mycobacterium TB DNA fragments were observed in the TB-quantitative real-time polymerase chain reaction. These findings supported the diagnosis of chronic granulomatous inflammation with necrosis, but did not exclude specific infections (TB).
The patient opted for follow-up observation and underwent regular conventional US for ongoing monitoring.
Follow-up US 6 months later revealed that the lesions found on the initial examination were unchanged. The patient is presently in good physical condition without any discomfort.
Multiple splenic lesions caused by infection, lymphoma, sarcoid, metastasis and infarction may have similar imaging features[1]. The overlapping imaging characteristics of splenic lesions cause a diagnostic dilemma[2,3]. Hence, there is a need for confirmation by tissue biopsy. The US-guided coaxial CNB is considered a valuable technique for obtaining ample tissue for definitive diagnosis and to reduce puncture-related complications[8,9].
Spleen tissue samples can be obtained by splenectomy or percutaneous biopsy[4]. Splenectomy is an invasive tech
Percutaneous biopsy is performed under US or CT guidance. US guidance is sometimes preferred over CT due to real-time guidance and no radiation risk. US-guided coaxial CNB demonstrates a high diagnostic accuracy, reduces complications and provides a specific therapeutic direction for patients[7,13-15]. The coaxial technique has had a positive impact on percutaneous image-guided biopsy since its introduction. The outer cannula is inserted into the spleen, and on the one hand, specimen collection yields can be improved using the same path by making slight adjustments to the angle of the introducer needle; on the other hand, changes in tissue cutting length can be achieved by adjusting the degree to which the introducer needle protrudes the outer cannula[16]. Adequate tissue samples ensure comprehensive pathological ana
US-guided coaxial CNB for the diagnosis of multiple splenic lesions is rarely performed clinically, and this case report provides a direction for clinical patient management and treatment. However, we lack the support of corresponding research data, which may not be very convincing.
US-guided coaxial CNB is a safe and efficient puncture technique for the diagnosis of multiple splenic lesions. It not only provides valuable diagnostic information but guides patient treatment based on histological analysis.
Thank Bao WYG, Jiang ZP and Lu Q for their suggestions on revising the draft.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eysselein VE, United States S-Editor: Qu XL L-Editor: A P-Editor: Qu XL
| 1. | Dhyani M, Anupindi SA, Ayyala R, Hahn PF, Gee MS. Defining an imaging algorithm for noncystic splenic lesions identified in young patients. AJR Am J Roentgenol. 2013;201:W893-W899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Kamaya A, Weinstein S, Desser TS. Multiple lesions of the spleen: differential diagnosis of cystic and solid lesions. Semin Ultrasound CT MR. 2006;27:389-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Tan M, Low HM, Shelat V, Tan CH. Imaging patterns in non-traumatic spleen lesions in adults-a review. Jpn J Radiol. 2022;40:664-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | McInnes MD, Kielar AZ, Macdonald DB. Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy. Radiology. 2011;260:699-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Long B, Koyfman A, Gottlieb M. Complications in the adult asplenic patient: A review for the emergency clinician. Am J Emerg Med. 2021;44:452-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Cadili A, de Gara C. Complications of splenectomy. Am J Med. 2008;121:371-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Olson MC, Atwell TD, Harmsen WS, Konrad A, King RL, Lin Y, Wall DJ. Safety and Accuracy of Percutaneous Image-Guided Core Biopsy of the Spleen. AJR Am J Roentgenol. 2016;206:655-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Liang P, Gao Y, Wang Y, Yu X, Yu D, Dong B. US-guided percutaneous needle biopsy of the spleen using 18-gauge versus 21-gauge needles. J Clin Ultrasound. 2007;35:477-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Muraca S, Chait PG, Connolly BL, Baskin KM, Temple MJ. US-guided core biopsy of the spleen in children. Radiology. 2001;218:200-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Strnad BS, Itani M, Middleton WD. Detection and management of bleeding in the setting of image-guided percutaneous needle biopsy. Abdom Radiol (NY). 2022;47:2681-2696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Singh AK, Shankar S, Gervais DA, Hahn PF, Mueller PR. Image-guided percutaneous splenic interventions. Radiographics. 2012;32:523-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Tam A, Krishnamurthy S, Pillsbury EP, Ensor JE, Gupta S, Murthy R, Ahrar K, Wallace MJ, Hicks ME, Madoff DC. Percutaneous image-guided splenic biopsy in the oncology patient: an audit of 156 consecutive cases. J Vasc Interv Radiol. 2008;19:80-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Gómez-Rubio M, López-Cano A, Rendón P, Muñoz-Benvenuty A, Macías M, Garre C, Segura-Cabral JM. Safety and diagnostic accuracy of percutaneous ultrasound-guided biopsy of the spleen: a multicenter study. J Clin Ultrasound. 2009;37:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Patel N, Dawe G, Tung K. Ultrasound-guided percutaneous splenic biopsy using an 18-G core biopsy needle: our experience with 52 cases. Br J Radiol. 2015;88:20150400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Sangiorgio VFI, Rizvi H, Padayatty J, Thayur N, Fujiwara T, Anyanwu FA, Calaminici M. Radiologically guided percutaneous core needle biopsy of the spleen: a reliable and safe diagnostic procedure for neoplastic and reactive conditions. Histopathology. 2021;78:1051-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Habibi HA, Cevener M, Yilmaz S. Image-guided percutaneous cutting needle biopsy in difficult locations. Jpn J Radiol. 2022;40:560-567. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Kunin H, Wijetunga NA, Erinjeri JP, Noy A, Deipolyi AR. Predictors of Major Hemorrhage After Spleen Core Biopsy in Cancer Patients. J Vasc Interv Radiol. 2022;33:1055-1060.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Guo RQ, Li XG. Seven case reports on the prevention of hemorrhage after percutaneous computed tomography-guided core-needle biopsy of the spleen. J Cancer Res Ther. 2020;16:1182-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Civardi G, Vallisa D, Bertè R, Giorgio A, Filice C, Caremani M, Caturelli E, Pompili M, De Sio I, Buscarini E, Cavanna L. Ultrasound-guided fine needle biopsy of the spleen: high clinical efficacy and low risk in a multicenter Italian study. Am J Hematol. 2001;67:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 93] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Handke NA, Koch DC, Muschler E, Thomas D, Luetkens JA, Attenberger UI, Kuetting D, Pieper CC, Wilhelm K. Bleeding management in computed tomography-guided liver biopsies by biopsy tract plugging with gelatin sponge slurry. Sci Rep. 2021;11:24506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Uller W, Müller-Wille R, Grothues D, Schelling J, Zausig N, Loss M, Stroszczynski C, Wohlgemuth WA. Gelfoam for closure of large percutaneous transhepatic and transsplenic puncture tracts in pediatric patients. Rofo. 2014;186:693-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |