Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3363
Revised: August 28, 2024
Accepted: September 13, 2024
Published online: October 27, 2024
Processing time: 190 Days and 23.9 Hours
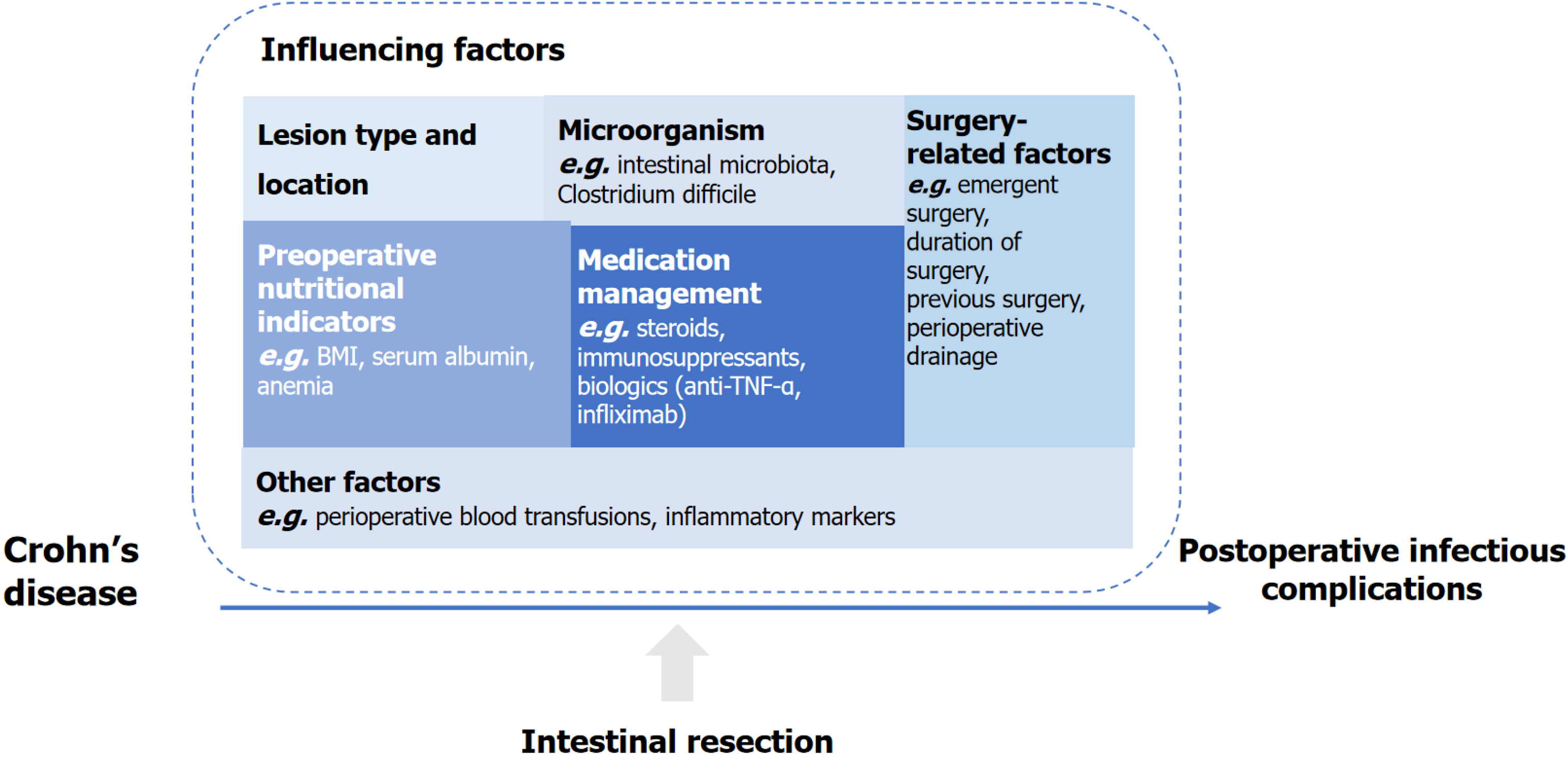
The incidence of Crohn’s disease (CD) has increased in recent years, with most patients requiring intestinal resection. Complications after intestinal resection for CD can lead to poor prognosis and recurrence, among which infectious complications are the most common. This study aimed to investigate the common risk factors, including medications, preoperative nutritional status, surgery-related factors, microorganisms, lesion location and type, and so forth, causing infectious complications after intestinal resection for CD, and to propose corresponding preventive measures. The findings provided guidance for identifying susceptibility factors and the early intervention and prevention of infectious complications after intestinal resection for CD in clinical practice.
Core Tip: Infectious complications after intestinal resection for Crohn’s disease (CD) can lead to a variety of adverse outcomes such as prolonged hospitalization, increased readmission rates, poor prognosis, and increased health-care burden in these patients. Therefore, identifying the risk factors for infectious complications and their early prevention are essential. This study aimed to investigate the risk factors, such as medications, preoperative nutritional status, and others, causing infectious complications after intestinal resection for CD, and to propose corresponding preventive measures. The findings provided guidance for reducing the occurrence of infectious complications.
- Citation: Lv SR, Huang X, Zhou LY, Shi J, Gong CC, Wang MK, Yang JS. Influencing factors and preventive measures of infectious complications after intestinal resection for Crohn’s disease. World J Gastrointest Surg 2024; 16(10): 3363-3370
- URL: https://www.wjgnet.com/1948-9366/full/v16/i10/3363.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i10.3363
Crohn’s disease (CD) is a chronic inflammatory disease of the gastrointestinal tract caused by complex interactions between genetic susceptibility, environmental factors, and alterations in the intestinal microbiota[1]. The incidence of CD has increased globally due to environmental exposure factors such as urbanization or advances in diagnostic methods[2]. As a progressive disease, most patients with CD develop complications such as strictures, fistulas, or abscesses, and approximately 80% of these patients require intestinal resection surgery[3,4]. Moreover, the incidence of postoperative complications, such as postoperative ileus, bleeding at the anastomosis site, intra-abdominal sepsis, and entero-cutaneous fistula, after surgery for CD is higher than that after other surgeries due to the disease characteristics and the fact that patients with CD are often malnourished[5]. Postoperative complications in patients with CD affect surgical outcomes, length of hospitalization, and prognosis, which are closely related to short- and long-term clinical outcomes of patients[6].
A recent study used an improved machine learning algorithm, specifically the randomized forest analysis model, in patients with CD after intestinal resection to predict the likelihood of short-term major complications, including anastomotic fistula, intra-abdominal septic complication (IASC), bleeding, and intestinal obstruction[7]. Thus, infectious complications after intestinal resection in CD are important risk factors. According to previous studies, the incidence of postoperative complications in patients with all types of CD ranges from 5.7% to 50%, with infectious postoperative complications being the most common[8,9]. The main postoperative infectious complications in CD include surgical site infections (SSIs) and extra-abdominal infections. Further, SSIs encompass superficial wound infections, deep wound infections affecting the fascia, and organ space infections such as IASCs and anastomotic leakage[10]. SSIs are a significant cause of morbidity and mortality and exert a considerable impact on both patients and the health-care system, including discomfort, prolonged hospitalization, increased readmission rates, adverse health outcomes, and increased health-care burden[11-13].
A few studies have reported on the factors influencing infectious complications after intestinal resection for CD, which mainly included preoperative nutritional status, medication, surgical methods, and so forth[14-16]. However, the results of the recent studies are still inconsistent and lack systematization. Therefore, in this study, we discussed the main influencing factors and preventive measures of infectious complications after intestinal resection for CD to provide a certain suggestion and guidance for reducing postoperative infectious complications of CD.
The PubMed databases were searched for studies published in English. The following key terms were used to identify studies related to postoperative infectious complications in CD: CD, intestinal resection, postoperative complications, infectious complications, SSIs, IASCs, and postoperative anastomotic fistula. These key terms were combined and searched using the set operators “AND” and “OR”. After removing duplicate studies, 240 studies published between Jan 2000 and Mar 2024 were retrieved. Of these, 45 discussions of testing techniques or surgical options, 11 case reports, 18 reviews, and 29 discussions of postoperative recurrence were excluded. Further, descriptive studies and studies that combined infectious complications with other complications were excluded, and ultimately 59 relevant studies were included for analysis. Further references were added by manually searching the relevant studies. For the studies considered appropriate for inclusion, the available texts were obtained and assessed in detail. The final studies were selected based on discussed consensus among all authors followed by our medical professional knowledge.
A few previous studies were conducted to predict factors affecting postoperative complications in CD using various methods. A study used univariate and multiple regression to determine the risk factors for short-term postoperative complications in CD. The findings revealed that elevated preoperative C-reactive protein (CRP) and decreased postoperative hemoglobin levels increased the possibility of postoperative complications[17]. Another French prospective study also used multivariate logistic regression analysis and found that preoperative corticosteroid treatment within the 4 weeks prior to surgery was significantly associated with an increased incidence of postoperative complications[9]. Several studies also used multivariate logistic regression analysis to explore the risk factors associated with postoperative infectious complications in CD. These studies found that preoperative albumin levels, anemia, and length of surgery were associated with postoperative infectious complications[16,18,19].
Wang et al[7], in their retrospective study, used machine learning methods, particularly random forest methods, to predict postoperative complications in CD, including anastomotic fistula, IASC, bleeding, and intestinal obstruction. They found that both nomogram and random forest performed well in predicting short-term major postoperative complications and preoperative CD activity index (CDAI) ≥ 220 reduced preoperative serum albumin levels and prolonged operative time, which were probably the most critical variables. The aforementioned findings might help identify patients at higher risk of complications and provide appropriate perioperative management to improve patient prognosis and reduce the incidence of complications, especially infectious complications.
CD can be treated with multiple medications, including steroids, immunosuppressants, biologics, and others, depending on the site and severity of its onset. As the mechanism of aforementioned medicines is immunosuppression, an increased risk of infection in patients is expected[20]. Few studies have been conducted on the effect of medications on infectious complications after intestinal resection for CD. Several studies showed that preoperative or postoperative use of steroids or immunosuppressive medicines was associated with the development of infectious complications after intestinal resection for CD[18,21,22]; on the contrary, some other studies did not report this association[23]. Biologic agents, mainly including anti-tumor necrosis factor [anti- tumor necrosis factor-α (TNF-α)], infliximab, and vedolizumab, are effective treatments for CD. However, some studies demonstrated that preoperative use of anti-TNF-α or infliximab before intestinal resection for CD, especially within 8 weeks before surgery, was associated with an increased incidence of postoperative infectious complications, including intra-abdominal abscesses and anastomotic fistulae[24-27]. Other studies, in contrast, did not find an association between anti-TNF-α, infliximab, vedolizumab, and the development of postoperative infectious complications[15,28,29]. Moreover, one study found that specific classes of biologic therapy did not independently increase the risk of postoperative infectious complications, yet combined immunosuppression increased the overall risk of infectious complications and the incidence of intra-abdominal sepsis[30]. Differences in the results of these studies might be due to the medicine type, dose, timing of medication, endpoint, and other confounding factors.
CD, as a wasting disease, is often accompanied by malnutrition, with a prevalence ranging from 20% to 85%[30]. Nutritional status is closely related to infectious diseases. Therefore, the association between preoperative nutritional status and postoperative infectious complications in patients with CD undergoing intestinal resection is important to investigate. A Chinese study found that body mass index (BMI) < 17.5 kg/m2 was a risk factor for infectious complications after intestinal resection for CD[31]. Although CD is a wasting disease, the obesity rate in its patients is similar to that in the general population[32]. Several studies have found that BMI ≥ 30 kg/m2 is also a risk factor for postoperative infectious complications in CD[18,33]. Moreover, subcutaneous fat thickness and fat distribution are important indicators for assessing the nutritional status. Two studies have demonstrated that an increase in subcutaneous fat thickness or increased proportion of subcutaneous fat relative to visceral fat volume distributed more in the thoracic vs lumbar spinal regions is a significant predictor of incisional SSI or other infectious complications after intestinal resection for CD[34,35]. Furthermore, although albumin is not a direct indicator of nutritional status, it may reflect systemic inflammation, protein loss, malnutrition, and so forth. Thus, it can indirectly reflect the preoperative nutritional status of patients. Moreover, serum albumin is important for wound healing and collagen synthesis at the anastomotic site, and hypoproteinemia may result in potentially poor wound healing and anastomotic fistulae[3]. A number of studies have shown that preoperative hypoalbuminemia (albumin < 30 g/L) is associated with a higher incidence of IASCs or SSI after intestinal resection for CD[16,22,36-38]. In addition, preoperative anemia has also been found to be a predictor of septic complications. The aforementioned studies suggest that either preoperative malnutrition or obesity is a potential risk factor for infectious complications after intestinal resection for CD.
Besides other factors in the perioperative period, factors directly related to intestinal resections for CD were also associated with postoperative infectious complications, such as emergent surgery, duration of surgery, previous surgery, perioperative drainage, and surgical approach. Urgent surgery was found to be associated with an increased risk of postoperative complications in CD, with wound infection, intra-abdominal abscesses, and anastomotic fistulae being the most common complications[39]. A Japanese study found that a surgery time of more than 180 min was associated with an increased risk of intra-abdominal sepsis after intestinal resection for CD. A Chinese study also showed that prolonged surgery time was a risk factor for SSI[19,38]. Another study explored the impact of various surgery-related factors on the occurrence of SSI after surgery for CD, and found that prolonged surgery was associated with SSI and active drainage was related to a reduced risk of organ/space SSI[40]. Preoperative percutaneous abscess drainage was also found to significantly reduce the incidence of postoperative severe IASC in patients with CD[41]. In addition, a previous history of intestinal resection was shown to be a risk factor for postoperative complications in patients with CD[42]. A meta-analysis also suggested that a history of previous surgery was associated with an incidence of postoperative IASC in CD[22].
Intestinal microorganisms play a role in the postoperative recurrence of CD and have been associated with the development of postoperative anastomotic fistulae in colorectal surgery[43,44]. Therefore, a potential relationship may be found between intestinal microorganisms and the development of infectious complications after intestinal resection for CD. A prospective cohort study used random forests to predict the impact factors for infectious complications at the surgical site after intestinal resection for CD. The findings revealed that the intestinal microbiota was the top selected variable, and the model containing 14 genera of microbiota had the largest area under the curve[45]. Clostridium difficile
CD involves a wide range of lesions, including upper gastrointestinal tract, ileum, colon, and perianal lesions, and the types of lesions are categorized as stenotic and penetrating. Different lesion locations and types may result in different risks of postoperative complications. Studies found that patients with CD combined with perianal lesions were at higher risk for re-surgery[49], and those involving upper gastrointestinal tract lesions were more likely to have IASCs after intestinal resection[37]. Moreover, a study found that patients with CD who had colonic or ileocolonic involvement were more likely to develop SSIs after intestinal resection than those with only ileal involvement[40]. According to a study, penetrating CD is associated with a higher risk of postoperative complications of intestinal resections[39]. Similarly, a retrospective Japanese study found that penetrating intestinal lesions of CD increased the risk of IASCs after intestinal resection[19]. In addition, the CDAI, which comprehensively assesses the activity level of CD, can also be used as a predictor of postoperative complications in CD. Wang et al[7] found that preoperative CDAI of ≥ 220 was a risk factor for postoperative complications after intestinal resection, including infectious complications. Another Chinese study also found that a CDAI of > 150 was a high-risk factor for anastomotic infectious complications after intestinal resection for CD[50].
Besides the aforementioned factors, other factors have been found to be associated with infectious complications after intestinal resection for CD; however, related studies are limited. For example, two studies suggested that perioperative blood transfusions could lead to an increased risk of postoperative infectious complications in CD, which might be related to transfusion-induced immunosuppression[51,52]. Moreover, inflammatory markers, including preoperative CRP and postoperative interleukin-6, can be used as infectious predictors of CD after bowel resection[16,53]. Influencing factors of infectious complications after intestinal resection for CD are summarized in Figure 1.
A few studies have proposed preventive measures for the aforementioned risk factors associated with infectious complications after intestinal resection for CD. The use of immunosuppressive medications within 4 weeks prior to intestinal resection has been associated with a higher incidence of sepsis, infectious shock, and anastomotic leakage in patients with CD. Hence, an appropriate preoperative drug-free interval may be able to reduce the risk of infection[21].
Preoperative poor nutritional status is associated with an increased risk of infectious complications after intestinal resection of CD. Patients should be assessed for malnutrition using the Malnutrition Universal Screening Tool criteria or the Nutrition Risk Screening 2002[54]. Natural dietary supplements, such as vitamins, minerals, and probiotics, should be prescribed to improve nutritional status and antioxidant, antiviral, and anti-inflammatory effects, which benefit immune regulation[55]. A meta-analysis, including multiple studies, demonstrated that preoperative enteral nutrition reduced the incidence of infectious complications after intestinal resection surgery in patients with CD[56].
The operating room environment and related equipment should be maintained strict hygiene. Medical staff should pay attention to hand hygiene, environmental disinfection, preoperative skin disinfection, and standardized aseptic operation, as these measures are essential for controlling SSIs[55]. Mechanical bowel preparation procedures could be conducted before surgery[57]. In addition, the use of a dual-ring wound protector during surgery or postoperative active drainage was a surgery-related factor that reduced infectious complications after intestinal resection[40,58].
Intestinal microbiota and microbial infections are associated with postoperative complications in CD. Therefore, therapeutic or prophylactic interventions targeting intestinal microorganisms, especially pathogenic infections such as C. difficile, can reduce the risk of postoperative complications. A randomized controlled study demonstrated that appropriate preoperative antibiotic prophylaxis can significantly reduce the incidence of postoperative incisional SSIs[57].
Beyond preventive measures targeting an individual risk factor, a retrospective study suggested that individualized prehabilitation, including nutritional support, antibiotic therapy or abscess drainage, and cessation or reduction of corticosteroid therapy, prior to intestinal resection could reduce the incidence of anastomotic complications in patients with high-risk CD[59]. Therefore, implementing personalized pre- and post-surgical preventive measures targeting the aforementioned risk factors for patients with CD with intestinal resection may be an effective way to reduce postoperative infectious complications. The multidisciplinary team can provide patients with nutritional optimization protocols, medication guidance, and so forth to reduce preoperative risk factors, and apply an individualized approach to each situation.
Infectious complications after intestinal resection for CD are influenced by a variety of factors, including preoperative nutrition, medication use, microorganisms, surgery-related factors, and others. Medication management, improving malnutrition and surgical conditions, microbial prophylaxis, and integrated strategies could be implemented in clinical practice as preventive measures to reduce the incidence of postoperative infectious complications.
We thank Xue-Lu Yu and other colleagues, the reviewers, and the editors for improving this manuscript.
| 1. | Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet. 2017;389:1741-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1121] [Cited by in RCA: 1806] [Article Influence: 225.8] [Reference Citation Analysis (111)] |
| 2. | Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46-54.e42; quiz e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3789] [Cited by in RCA: 3527] [Article Influence: 271.3] [Reference Citation Analysis (5)] |
| 3. | Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV Jr. Risk factors associated with progression to intestinal complications of Crohn's disease in a population-based cohort. Gastroenterology. 2010;139:1147-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 577] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 4. | Meima-van Praag EM, Buskens CJ, Hompes R, Bemelman WA. Surgical management of Crohn's disease: a state of the art review. Int J Colorectal Dis. 2021;36:1133-1145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Ge X, Liu H, Tang S, Wu Y, Pan Y, Liu W, Qi W, Ye L, Cao Q, Zhou W. Preoperative hypoalbuminemia is an independent risk factor for postoperative complications in Crohn's disease patients with normal BMI: A cohort study. Int J Surg. 2020;79:294-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Park DI, Hisamatsu T, Chen M, Ng SC, Ooi CJ, Wei SC, Banerjee R, Hilmi IN, Jeen YT, Han DS, Kim HJ, Ran Z, Wu K, Qian J, Hu PJ, Matsuoka K, Andoh A, Suzuki Y, Sugano K, Watanabe M, Hibi T, Puri AS, Yang SK. Asian Organization for Crohn's and Colitis and Asia Pacific Association of Gastroenterology consensus on tuberculosis infection in patients with inflammatory bowel disease receiving anti-tumor necrosis factor treatment. Part 2: Management. J Gastroenterol Hepatol. 2018;33:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Wang FT, Lin Y, Yuan XQ, Gao RY, Wu XC, Xu WW, Wu TQ, Xia K, Jiao YR, Yin L, Chen CQ. Predicting short-term major postoperative complications in intestinal resection for Crohn's disease: A machine learning-based study. World J Gastrointest Surg. 2024;16:717-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 8. | Yamamoto T, Watanabe T. Surgery for luminal Crohn's disease. World J Gastroenterol. 2014;20:78-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Fumery M, Seksik P, Auzolle C, Munoz-Bongrand N, Gornet JM, Boschetti G, Cotte E, Buisson A, Dubois A, Pariente B, Zerbib P, Chafai N, Stefanescu C, Panis Y, Marteau P, Pautrat K, Sabbagh C, Filippi J, Chevrier M, Houze P, Jouven X, Treton X, Allez M; REMIND study group investigators. Postoperative Complications after Ileocecal Resection in Crohn's Disease: A Prospective Study From the REMIND Group. Am J Gastroenterol. 2017;112:337-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 139] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 10. | Mowlah RK, Soldera J. Risk and management of post-operative infectious complications in inflammatory bowel disease: A systematic review. World J Gastrointest Surg. 2023;15:2579-2595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 11. | Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, Keohane C, Denham CR, Bates DW. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173:2039-2046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1128] [Cited by in RCA: 1295] [Article Influence: 107.9] [Reference Citation Analysis (0)] |
| 12. | Jenks PJ, Laurent M, McQuarry S, Watkins R. Clinical and economic burden of surgical site infection (SSI) and predicted financial consequences of elimination of SSI from an English hospital. J Hosp Infect. 2014;86:24-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 225] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 13. | Guo Z, Cao L, Guo F, Gong J, Li Y, Gu L, Zhu W, Li J. The Presence of Postoperative Infectious Complications is Associated with the Risk of Early Postoperative Clinical Recurrence of Crohn's Disease. World J Surg. 2017;41:2371-2377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Yamamoto T, Nakahigashi M, Shimoyama T, Umegae S. Does preoperative enteral nutrition reduce the incidence of surgical complications in patients with Crohn's disease? A case-matched study. Colorectal Dis. 2020;22:554-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 15. | Ferrante M, de Buck van Overstraeten A, Schils N, Moens A, Van Assche G, Wolthuis A, Vermeire S, D'Hoore A. Perioperative Use of Vedolizumab is not Associated with Postoperative Infectious Complications in Patients with Ulcerative Colitis Undergoing Colectomy. J Crohns Colitis. 2017;11:1353-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 16. | Ghoneima AS, Flashman K, Dawe V, Baldwin E, Celentano V. High risk of septic complications following surgery for Crohn's disease in patients with preoperative anaemia, hypoalbuminemia and high CRP. Int J Colorectal Dis. 2019;34:2185-2188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 17. | Riss S, Bittermann C, Schwameis K, Kristo I, Mittlböck M, Herbst F, Stift A. Determinants for postoperative complications after laparoscopic intestinal resection for Crohn's disease. Surg Endosc. 2012;26:933-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Cima RR, Bergquist JR, Hanson KT, Thiels CA, Habermann EB. Outcomes are Local: Patient, Disease, and Procedure-Specific Risk Factors for Colorectal Surgical Site Infections from a Single Institution. J Gastrointest Surg. 2017;21:1142-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Kanazawa A, Yamana T, Okamoto K, Sahara R. Risk factors for postoperative intra-abdominal septic complications after bowel resection in patients with Crohn's disease. Dis Colon Rectum. 2012;55:957-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Chen DM, Pritchard ML, Sandborn WJ. Serious infections and mortality in association with therapies for Crohn's disease: TREAT registry. Clin Gastroenterol Hepatol. 2006;4:621-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 654] [Cited by in RCA: 635] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 21. | Valizadeh N, Murray AC, Suradkar K, Al-Mazrou A, Kiran RP. Impact of preoperative steroid or immunosuppressant use on short-term outcomes following colectomy in Crohn's disease patients. Tech Coloproctol. 2017;21:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Huang W, Tang Y, Nong L, Sun Y. Risk factors for postoperative intra-abdominal septic complications after surgery in Crohn's disease: A meta-analysis of observational studies. J Crohns Colitis. 2015;9:293-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 136] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 23. | Canedo J, Lee SH, Pinto R, Murad-Regadas S, Rosen L, Wexner SD. Surgical resection in Crohn's disease: is immunosuppressive medication associated with higher postoperative infection rates? Colorectal Dis. 2011;13:1294-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Syed A, Cross RK, Flasar MH. Anti-tumor necrosis factor therapy is associated with infections after abdominal surgery in Crohn's disease patients. Am J Gastroenterol. 2013;108:583-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | El-Hussuna A, Krag A, Olaison G, Bendtsen F, Gluud LL. The effect of anti-tumor necrosis factor alpha agents on postoperative anastomotic complications in Crohn's disease: a systematic review. Dis Colon Rectum. 2013;56:1423-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | Yu CS, Jung SW, Lee JL, Lim SB, Park IJ, Yoon YS, Kim CW, Yang SK, Ye BD, Park SH, Han M, Kim JC. The Influence of Preoperative Medications on Postoperative Complications in Patients After Intestinal Surgery for Crohn's Disease. Inflamm Bowel Dis. 2019;25:1559-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Tang S, Dong X, Liu W, Qi W, Ye L, Yang X, Cao Q, Ge X, Zhou W. Compare risk factors associated with postoperative infectious complication in Crohn's disease with and without preoperative infliximab therapy: a cohort study. Int J Colorectal Dis. 2020;35:727-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Uchino M, Ikeuchi H, Shimizu J, Ohge H, Haji S, Mizuguchi T, Mohri Y, Yamashita C, Kitagawa Y, Suzuki K, Kobayashi M, Kobayashi M, Sakamoto F, Yoshida M, Mayumi T, Hirata K, Takesue Y. Association between preoperative tumor necrosis factor alpha inhibitor and surgical site infection after surgery for inflammatory bowel disease: a systematic review and meta-analysis. Surg Today. 2021;51:32-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Rosenfeld G, Qian H, Bressler B. The risks of post-operative complications following pre-operative infliximab therapy for Crohn's disease in patients undergoing abdominal surgery: a systematic review and meta-analysis. J Crohns Colitis. 2013;7:868-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 30. | Lightner AL, McKenna NP, Alsughayer A, Harmsen WS, Taparra K, Parker ME, Raffals LE, Loftus EV Jr. Biologics and 30-Day Postoperative Complications After Abdominal Operations for Crohn's Disease: Are There Differences in the Safety Profiles? Dis Colon Rectum. 2019;62:1352-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 31. | Zhu Y, Zhou W, Qi W, Liu W, Chen M, Zhu H, Xiang J, Xie Q, Chen P. Body mass index is a practical preoperative nutritional index for postoperative infectious complications after intestinal resection in patients with Crohn's disease. Medicine (Baltimore). 2017;96:e7113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Seminerio JL, Koutroubakis IE, Ramos-Rivers C, Hashash JG, Dudekula A, Regueiro M, Baidoo L, Barrie A, Swoger J, Schwartz M, Weyant K, Dunn MA, Binion DG. Impact of Obesity on the Management and Clinical Course of Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:2857-2863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (1)] |
| 33. | McKenna NP, Habermann EB, Zielinski MD, Lightner AL, Mathis KL. Body mass index: Implications on disease severity and postoperative complications in patients with Crohn's disease undergoing abdominal surgery. Surgery. 2019;166:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Stidham RW, Waljee AK, Day NM, Bergmans CL, Zahn KM, Higgins PD, Wang SC, Su GL. Body fat composition assessment using analytic morphomics predicts infectious complications after bowel resection in Crohn's disease. Inflamm Bowel Dis. 2015;21:1306-1313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Cai X, Shen W, Guo Z, Li Y, Cao L, Gong J, Zhu W. Thickness of Subcutaneous Fat Is a Predictive Factor of Incisional Surgical Site Infection in Crohn's Disease Surgery: A Retrospective Study. Gastroenterol Res Pract. 2018;2018:1546075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Shah RS, Bachour S, Jia X, Holubar SD, Hull TL, Achkar JP, Philpott J, Qazi T, Rieder F, Cohen BL, Regueiro MD, Lightner AL, Click BH. Hypoalbuminaemia, Not Biologic Exposure, Is Associated with Postoperative Complications in Crohn's Disease Patients Undergoing Ileocolic Resection. J Crohns Colitis. 2021;15:1142-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 37. | Zhu F, Li Y, Guo Z, Cao L, Feng D, Zhang T, Zhu W, Gong J. Nomogram to Predict Postoperative Intra-abdominal Septic Complications After Bowel Resection and Primary Anastomosis for Crohn's Disease. Dis Colon Rectum. 2020;63:629-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 38. | Liu S, Miao J, Wang G, Wang M, Wu X, Guo K, Feng M, Guan W, Ren J. Risk factors for postoperative surgical site infections in patients with Crohn's disease receiving definitive bowel resection. Sci Rep. 2017;7:9828. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 39. | Gutiérrez A, Rivero M, Martín-Arranz MD, García Sánchez V, Castro M, Barrio J, de Francisco R, Barreiro-de Acosta M, Juliá B, Cea-Calvo L, Romero C, Borruel Sainz N, Domènech E. Perioperative management and early complications after intestinal resection with ileocolonic anastomosis in Crohn's disease: analysis from the PRACTICROHN study. Gastroenterol Rep (Oxf). 2019;7:168-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 40. | Ikeshima R, Mizushima T, Takahashi H, Haraguchi N, Nishimura J, Hata T, Matsuda C, Ikenaga M, Nakajima K, Yamamoto H, Murata K, Doki Y, Mori M. The efficacy of active drainage for preventing postoperative organ/space surgical site infections in patients with Crohn's disease. Surg Today. 2018;48:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Müller-Wille R, Iesalnieks I, Dornia C, Ott C, Jung EM, Friedrich C, Schill G, Hoffstetter P, Zorger N, Schreyer AG. Influence of percutaneous abscess drainage on severe postoperative septic complications in patients with Crohn's disease. Int J Colorectal Dis. 2011;26:769-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 42. | Duan Y, Liu Y, Li Y. Previous Intestinal Resection Is Associated with Postoperative Complications in Crohn's Disease: A Cohort Study. Gastroenterol Res Pract. 2020;2020:2194382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 43. | van Praagh JB, de Goffau MC, Bakker IS, van Goor H, Harmsen HJM, Olinga P, Havenga K. Mucus Microbiome of Anastomotic Tissue During Surgery Has Predictive Value for Colorectal Anastomotic Leakage. Ann Surg. 2019;269:911-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 44. | Buisson A, Sokol H, Hammoudi N, Nancey S, Treton X, Nachury M, Fumery M, Hébuterne X, Rodrigues M, Hugot JP, Boschetti G, Stefanescu C, Wils P, Seksik P, Le Bourhis L, Bezault M, Sauvanet P, Pereira B, Allez M, Barnich N; Remind study group. Role of adherent and invasive Escherichia coli in Crohn's disease: lessons from the postoperative recurrence model. Gut. 2023;72:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 45. | Julien C, Anakok E, Treton X, Nachury M, Nancey S, Buisson A, Fumery M, Filippi J, Maggiori L, Panis Y, Zerbib P, François Y, Dubois A, Sabbagh C, Rahili A, Seksik P, Allez M, Lefevre JH; REMIND Study Group Investigators, Le Corff S, Bonnet A, Beyer-Berjot L, Sokol H. Impact of the Ileal Microbiota on Surgical Site Infections in Crohn's Disease: A Nationwide Prospective Cohort. J Crohns Colitis. 2022;16:1211-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 46. | Trifan A, Stanciu C, Stoica O, Girleanu I, Cojocariu C. Impact of Clostridium difficile infection on inflammatory bowel disease outcome: a review. World J Gastroenterol. 2014;20:11736-11742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 47. | Hellmann J, Andersen H, Fei L, Linn A, Bezold R, Lake K, Jackson K, Meyer D, Dirksing K, Bonkowski E, Ollberding NJ, Haslam DB, Denson L. Microbial Shifts and Shorter Time to Bowel Resection Surgery Associated with C. difficile in Pediatric Crohn's Disease. Inflamm Bowel Dis. 2020;26:1212-1221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 48. | Connelly TM, Holubar SD, Clancy C, Cheong JY, Jia X, Bhama AR, Lightner AL, Kessler H, Valente M, Liska D. Outcomes of clostridioides difficile infection on inflammatory bowel disease patients undergoing colonic resection: A propensity score weighted NSQIP analysis. Am J Surg. 2023;225:553-557. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 49. | Han YM, Kim JW, Koh SJ, Kim BG, Lee KL, Im JP, Kim JS, Jung HC. Patients with perianal Crohn's disease have poor disease outcomes after primary bowel resection. J Gastroenterol Hepatol. 2016;31:1436-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 50. | Wang WY, Chen CL, Chen GL, Wu CJ, Li HG, Luan SM, Zhu YB. [Analysis of risk factors for anastomotic infectious complications following bowel resection for Crohn disease]. Zhonghua Wei Chang Wai Ke Za Zhi. 2013;16:328-331. [PubMed] [DOI] [Full Text] |
| 51. | Li Y, Stocchi L, Rui Y, Liu G, Gorgun E, Remzi FH, Shen B. Perioperative Blood Transfusion and Postoperative Outcome in Patients with Crohn's Disease Undergoing Primary Ileocolonic Resection in the "Biological Era". J Gastrointest Surg. 2015;19:1842-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Lan N, Stocchi L, Li Y, Shen B. Perioperative blood transfusion is associated with post-operative infectious complications in patients with Crohn's disease. Gastroenterol Rep (Oxf). 2018;6:114-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Xie T, Zhao C, Ding C, Zhang L, Cheng M, Chun C, Yu W, Gong J, Zhu W. Postoperative Interleukin-6 Predicts Intra-abdominal Septic Complications at an Early Stage After Elective Intestinal Operation for Crohn's Disease Patients. Inflamm Bowel Dis. 2018;24:1992-2000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 54. | Wang MK, Yu XL, Zhou LY, Si HM, Hui JF, Hou DY, Li WP, Yang JS. COVID-19 and liver dysfunction: What nutritionists need to know. World J Gastroenterol. 2022;28:1526-1535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 55. | Yu XL, Zhou LY, Huang X, Li XY, Pan QQ, Wang MK, Yang JS. Urgent call for attention to diabetes-associated hospital infections. World J Diabetes. 2024;15:1683-1691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (4)] |
| 56. | Krasnovsky L, Weber AT, Gershuni V, Pettke E, Lewis JD. Preoperative Exclusive Enteral Nutrition Is Associated With Reduced Skin and Soft Tissue and Intra-abdominal Infections in Patients With Crohn's Disease Undergoing Intestinal Surgery: Results from a Meta-Analysis. Inflamm Bowel Dis. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 57. | Uchino M, Ikeuchi H, Bando T, Chohno T, Sasaki H, Horio Y, Nakajima K, Takesue Y. Efficacy of Preoperative Oral Antibiotic Prophylaxis for the Prevention of Surgical Site Infections in Patients With Crohn Disease: A Randomized Controlled Trial. Ann Surg. 2019;269:420-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 58. | Ge X, Tang S, Qi W, Liu W, Lv J, Cao Q, Zhou W, Cai X. Prevalence and predictors of surgical site infections after bowel resection for Crohn's disease: the role of dual-ring wound protector. Int J Colorectal Dis. 2019;34:879-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 59. | Ferrandis C, Souche R, Bardol T, Boivineau L, Fabre JM, Altwegg R, Guillon F. Personalized pre-habilitation reduces anastomotic complications compared to up front surgery before ileocolic resection in high-risk patients with Crohn's disease: A single center retrospective study. Int J Surg. 2022;105:106815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |