Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3328
Revised: August 21, 2024
Accepted: August 29, 2024
Published online: October 27, 2024
Processing time: 133 Days and 0.3 Hours
Because of the mild inflammatory status in acute uncomplicated appendicitis, our team developed a novel technical protocol for single-port laparoscopic appendec
An adult male patient was admitted for persistent right lower abdominal pain with preoperative computed tomography findings suggestive of appendicitis accompanied by localized peritonitis. A modified technical protocol for SLAN based on minimally invasive surgical principles was used, and the patient was confirmed to have acute simple appendicitis by postoperative pathological ana
The modified technical protocol of SLAN may be a new minimally invasive surgical alternative for patients with acute simple appendicitis.
Core Tip: The single-port laparoscopic technique is widely used by surgeons worldwide because it results in minimal surgical stress and fast postoperative recovery. Our center first reported a modified protocol of single-port laparoscopic appen
- Citation: Chen Y, Fan ZQ, Fu XA, Zhang XX, Yuan JQ, Guo SG. Modified technical protocol for single-port laparoscopic appendectomy using needle-type grasping forceps for acute simple appendicitis: A case report. World J Gastrointest Surg 2024; 16(10): 3328-3333
- URL: https://www.wjgnet.com/1948-9366/full/v16/i10/3328.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i10.3328
Acute uncomplicated appendicitis is mild, and early surgical resection remains an indispensable treatment despite controversy over the choice of antibiotics or further appendectomy[1-3]. In 2019, based on the minimally invasive surgical concept, our center designed a novel technical protocol for single-port laparoscopic appendectomy using needle-type grasping forceps (SLAN). The initial technical protocol reduced the size of the abdominal incision to only 1 cm, resulting in satisfactory clinical results, such as mild pain response, fast postoperative recovery, and good cosmetic results, espe
However, given the 1-cm long umbilicus incision, which can contain only two 5-mm trocars simultaneously, many key technical issues, such as the difficulty of appendix retrieval, sterile gauze insertion and the instability of pneumoperitoneum pressure maintenance, are highlighted. Preliminary retrospective clinical results revealed that SLAN has a long operative time (mean 66 minutes)[6], which undoubtedly increases the burden of surgery on both patients and surgeons. Additionally, the inability to place longer Ham-o-lock clips increased the difficulty of surgery, prolonged the learning curve of surgery, and increased potential safety concerns. Therefore, our center further improved and optimized the initial technical protocol based on the concept of minimally invasive surgery.
A 56-year-old man was admitted to our hospital on April 16, 2024, with persistent right lower abdominal pain for 58 hours.
The patient had persistent right lower abdominal pain without a precipitating cause 58 hours prior, accompanied by fever, no nausea or vomiting, no shoulder back radiation pain, and no remission of abdominal pain after symptomatic treatment in the local hospital. He visited our hospital for further diagnosis and treatment.
The patient was previously healthy and had no history of abdominal surgery or surgical contraindications, such as severe cardiovascular or cerebrovascular disease.
The patient’s temperature was 38.1 °C, and the right lower abdominal muscles were tense, accompanied by tenderness and rebound tenderness of the right lower abdomen region and weak bowel sounds.
Through preoperative and postoperative 24-hour routine blood test results, interleukin 6 and C-reactive protein were detected and compared (Table 1), and the preoperative coagulation and biochemical function data were within normal ranges.
| Preoperative | Postoperative | |
| WBC (× 109/L) | 6.41 | 7.12 |
| NEU (%) | 71.4 | 60.9 |
| CRP (mg/L) | 40.23 | 42.86 |
| IL-6 (pg/mL) | 13.2 | 6.74 |
A preoperative abdominal computed tomography scan revealed appendicitis with localized peritonitis (Figure 1).
Preoperative clinical evidence suggested a diagnosis of acute appendicitis with localized peritonitis.
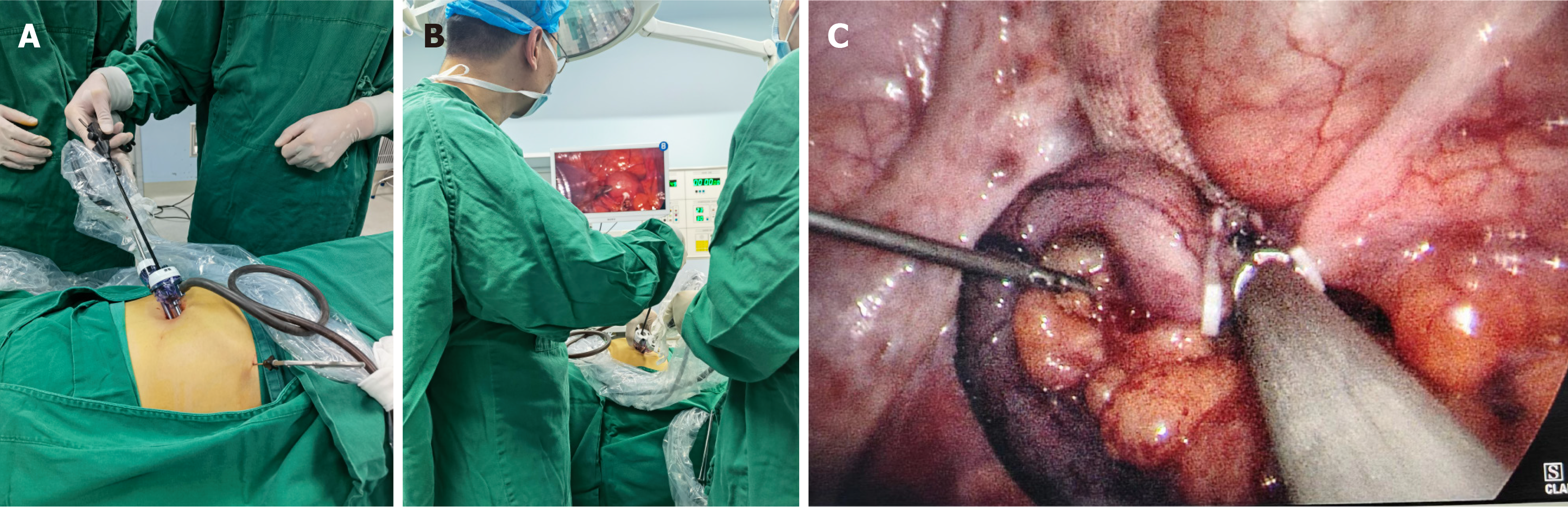
The surgical and clinical research protocols were followed, and informed consent was obtained before surgery. A modified SLAN technical protocol was used. General anesthesia was achieved with the patient lying flat, and the laparoscopic display screen was placed on the right side. A 1 cm incision was then made below the umbilicus, CO2 pneumoperitoneum was established, a 13 mmHg pressure was applied, and a 1 cm trocar was inserted into the abdominal cavity. The position of the patient was changed so that they were head-down and left-leaning, with the surgeon standing to the lower left and the assistant standing to the upper right (Figure 2). A 5 mm caliber laparoscopic lens with 30 leaners (STORZ corporation, Germany) was inserted for abdominal exploration, and no collateral injury was observed. The prececal ap
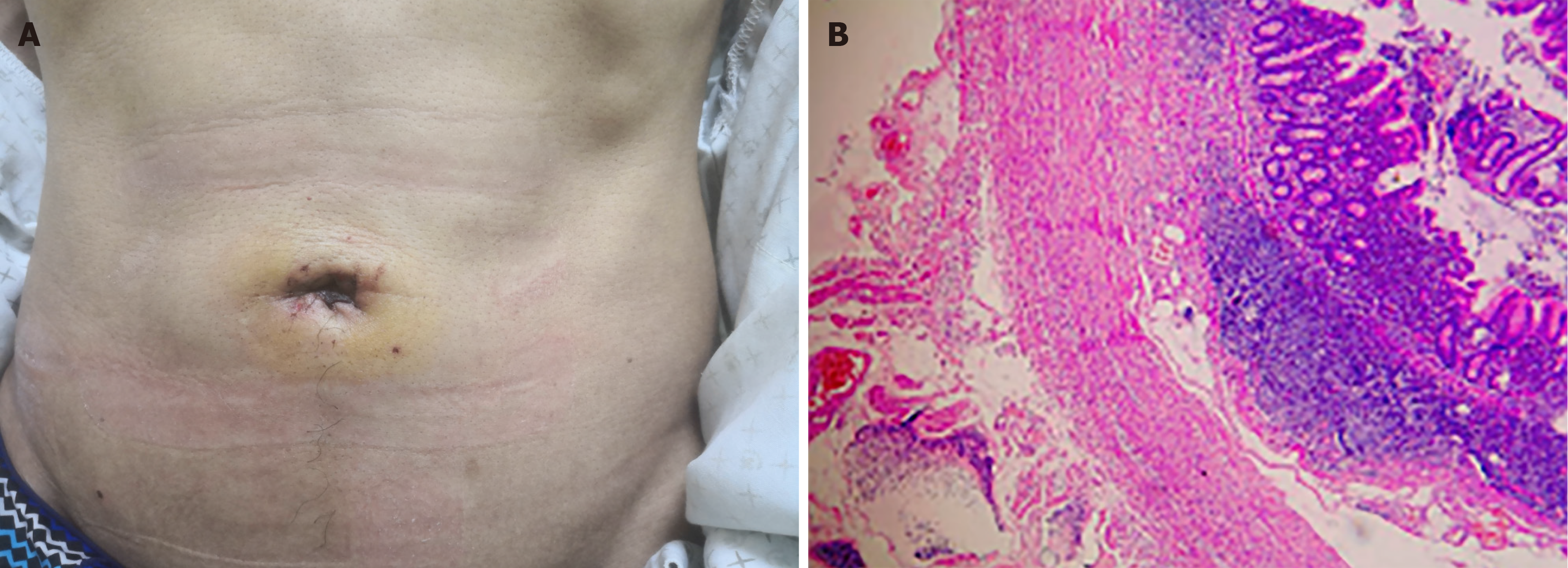
The surgical duration was 28 minutes. Postoperative 12-hour and 24-hour visual analog scale scores were all 1 point. The patient passed gas on postoperative day (POD) 1, was discharged with permission to resume daily activities and exhi
Acute appendicitis is one of the most common acute abdominal conditions worldwide, and a minimally invasive and cost-effective surgical intervention would benefit 96.5–100/100000 adult patients annually[7], especially patients with acute uncomplicated appendicitis, including acute simple appendicitis and gangrenous appendicitis, which can induce mild inflammation[8]. Therefore, our center modified the CLA technique on the basis of minimally invasive surgical methods. Although previous clinical studies have shown that SLAN is superior to CLA[1-3], the limitations and limi
Our center further optimized the previous technical protocol of SLAN based on a deep learning review of previously reported articles regarding single-port laparoscopic appendectomy[9]. A 1 cm trocar was inserted into the abdominal cavity via a 1 cm incision in the umbilicus for abdominal exploration. If severe complications are observed during the operation, the CLA protocol can be directly modified without increasing the number of unnecessary surgical incisions or the surgical duration. If a single-port laparoscopic procedure can be conducted according to the intraoperative evaluation results, the incision should be lengthened 5 mm along the left umbilicus, and a 5 mm trocar should be inserted. Co
Although this case report introduces a novel modified minimally invasive surgical protocol for an adult patient with acute simple appendicitis, its results are insufficient to fully and comprehensively demonstrate the advantages and disadvantages of this technique. There is still a long way to go in the modification of single-port laparoscopic surgery. First, key equipment needs to be further designed and improved, such as more robust and reliable needle-type grasping forceps, single-port laparoscopic puncture devices suitable for 1-1.5 cm incisions, and specialized disposable bags to avoid appendiceal curling. Second, high-quality studies, especially prospective randomized controlled studies, are warranted to evaluate the feasibility and safety of this technique.
This case report introduces the key technical points of a modified SLAN protocol, which enhances the fluency of the procedure, reduces the operative time, expands surgical indications, and increases surgical safety. Moreover, positive clinical outcomes, including postoperative passing gas time, pain response, and incision appearance, suggest better clinical application potential and generalizability. Further high-quality prospective clinical studies are warranted to obtain higher-level evidence on evidence-based medicine.
| 1. | de Almeida Leite RM, Seo DJ, Gomez-Eslava B, Hossain S, Lesegretain A, de Souza AV, Bay CP, Zilberstein B, Marchi E, Machado RB, Barchi LC, Ricciardi R. Nonoperative vs Operative Management of Uncomplicated Acute Appendicitis: A Systematic Review and Meta-analysis. JAMA Surg. 2022;157:828-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (102)] |
| 2. | Talan DA, Di Saverio S. Treatment of Acute Uncomplicated Appendicitis. N Engl J Med. 2021;385:1116-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 3. | Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De' Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De' Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 601] [Article Influence: 120.2] [Reference Citation Analysis (109)] |
| 4. | Chen Y, Yuan JQ, Guo SG, Yang ZJ. Single-port laparoscopic appendectomy using a needle-type grasping forceps for acute uncomplicated appendicitis in children: Case series. Int J Surg Case Rep. 2020;70:216-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 5. | Chen Y, Liu Y, Guo S, Yuan J, Li X. Single-port laparoscopic appendectomy using a needle-type grasping forceps for selective adult patients with acute uncomplicated appendicitis. J Surg Case Rep. 2022;2022:rjab557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 6. | Chen Y, Guo S, Liu Y, Yuan J, Fan Z. Single-port laparoscopic appendectomy using a needle-type grasping forceps compared with conventional three-port laparoscopic appendectomy for patients with acute uncomplicated appendicitis: a single-center retrospective study. J Int Med Res. 2022;50:3000605221119647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (108)] |
| 7. | Moris D, Paulson EK, Pappas TN. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA. 2021;326:2299-2311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 162] [Article Influence: 40.5] [Reference Citation Analysis (112)] |
| 8. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 685] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 9. | Chen Y, Fan Z, Zhang X, Fu X, Li J, Yuan J, Guo S. A brief overview of single-port laparoscopic appendectomy as an optimal surgical procedure for patients with acute appendicitis: still a long way to go. J Int Med Res. 2023;51:3000605231183781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |