Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3155
Revised: August 16, 2024
Accepted: August 22, 2024
Published online: October 27, 2024
Processing time: 74 Days and 16.5 Hours
Fast-track surgery (FTS) is a modern nursing approach that has gained popularity in the perioperative phase of surgery.
To investigate the impact of FTS on perioperative care for hepatobiliary surgery.
A retrospective analysis was performed on 98 patients who underwent hepatobiliary surgery and were admitted to our hospital from August 2021 to October 2023. They were divided into an observation group and a control group with 49 patients in each group according to different nursing directions. The control group was treated with standard nursing and the observation group was treated with FTS concept nursing. The length of hospital stay, visual analog scale (VAS) score, wound complications, nursing satisfaction, self-rating scale (SAS) score, and SF-36 quality of life (QoL) score were compared between the two groups before and after care.
The duration of hospitalization, hospitalization cost, operation time, first im
FTS in patients undergoing hepatobiliary surgery can effectively improve negative mood, QoL, and nursing sa
Core Tip: Fast-track surgery (FTS) is a modern nursing approach that has gained popularity during the perioperative phase of surgery. In this study, we investigated the effect of FTS on the perioperative care of patients undergoing hepatobiliary surgery. The study showed that FTS in patients undergoing hepatobiliary surgery can effectively improve negative mood, quality of life, and nursing satisfaction, reduce wound complications, and accelerate patient rehabilitation.
- Citation: Wang XH, Chen FF, Pan J, Jiang YF, Yao MY, Mao JL, Xu YF. Impact of fast-track surgery on perioperative care in patients undergoing hepatobiliary surgery. World J Gastrointest Surg 2024; 16(10): 3155-3162
- URL: https://www.wjgnet.com/1948-9366/full/v16/i10/3155.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i10.3155
In recent years, with the development of modern society and changes in living habits and dietary structures, the in
In recent years, rapid rehabilitation surgery, known as fast-track surgery (FTS), has emerged as a nursing practice widely used in various surgical departments in European and American hospitals and has attracted the attention of the medical community[4]. Under the guidance of FTS, the traditional care mode for many surgical diseases has changed to significantly shorten the hospital stay of patients and reduce medical expenses[5]. FTS refers to the application of medical evidence in preoperative, intraoperative, and postoperative measures to reduce postoperative adverse and stress re
In addition, an increasing number of researchers have applied the FTS concept to hepatobiliary surgery, especially for patients undergoing liver cancer surgery, for whom the application effect is relatively satisfactory. However, few clinical reports have been published on other applications of FTS in hepatobiliary surgery research. Therefore, in this study, we discuss the clinical application of FTS in hepatobiliary surgery to provide a theoretical basis for the rapid rehabilitation of patients undergoing hepatobiliary surgery.
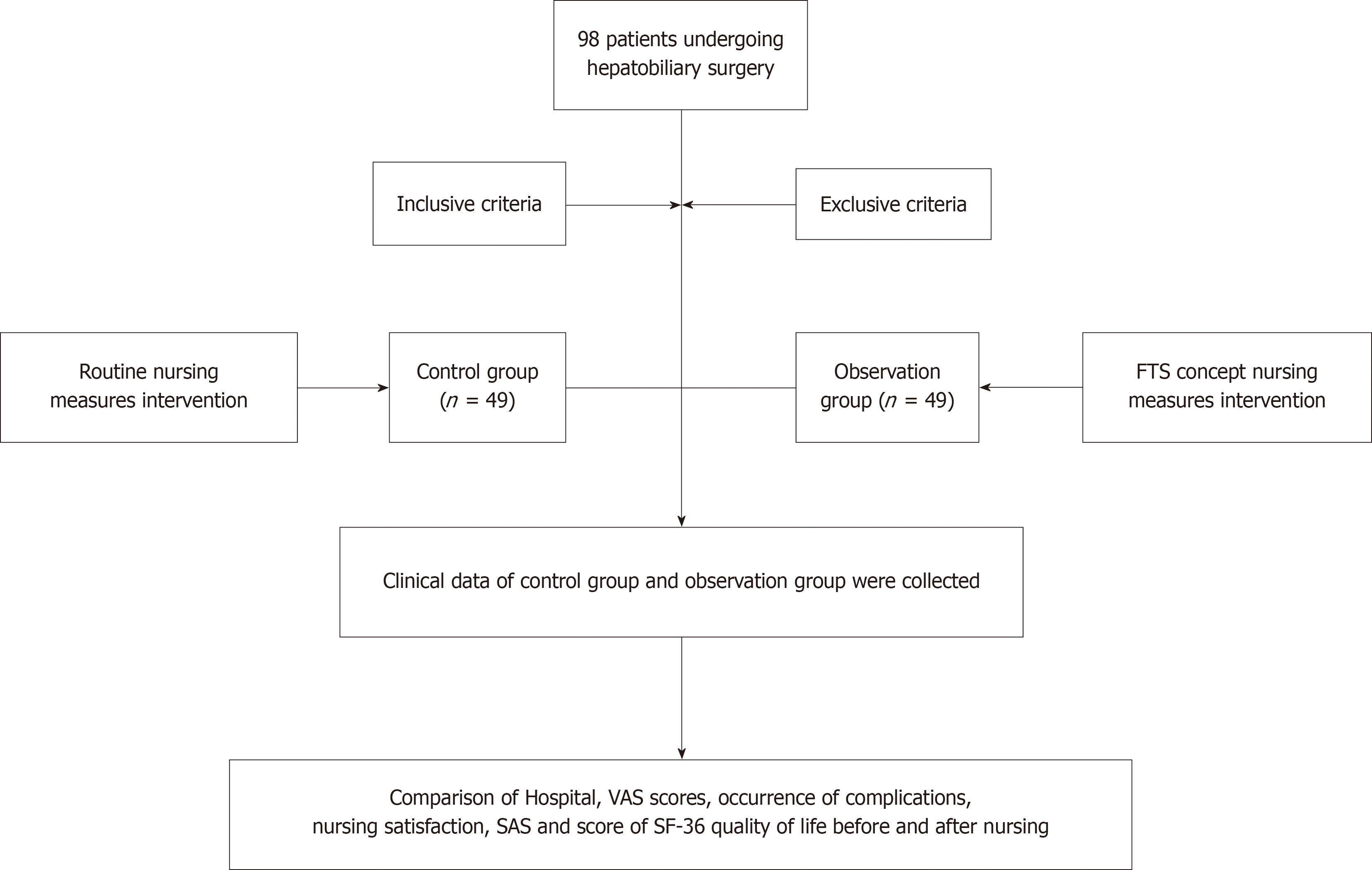
A retrospective analysis was performed on 98 patients who underwent hepatobiliary surgery and were admitted to Kecheng District People's Hospital from August 2021 to October 2023. The patients were divided into observation and control groups, with 49 patients in each group, according to the different nursing directions. The patients in the obser
The inclusion criteria were as follows: (1) All patients diagnosed with hepatobiliary surgery-related diseases by imaging and biochemical examination; (2) All patients who met the corresponding indications for surgical treatment and tolerated the operation; and (3) The study was approved by the ethics committee of the hospital.
The exclusion criteria were as follows: (1) Severe failure of the liver, heart, or other important organs; (2) Incomplete clinical data and cognitive abnormalities; (3) Inability to cooperate with investigators, pregnancy, or lactation; and (4) Malignant tumors, autoimmune diseases, or coagulation disorders.
Control group: General nursing group, including healthcare, education, observation, diet care, preoperative bowel cleaning, 4 hours before water, 12 hours fasting, postoperative analgesia, rehabilitation guidance, and discharge follow-up.
Observation group: In addition to the basic care given to the patients in the control group, the observation group un
Preoperative nursing: (1) Mainly provided patients with psychological, social, and physiological interventions. The pre
Postoperative care: (1) Pain management: Unbearable pain after surgery can affect the early implantation movements of patients. At 48 hours after surgery, analgesic drugs can be injected with intravenous or nonsteroidal anti-inflammatory painkillers, and opioid analgesics can be prohibited to reduce the occurrence of intestinal paralysis; (2) Early post
(1) Length of hospitalization, hospitalization costs, operation time, first implantation time, exhaust time, and first post
Data were analyzed using SPSS 23.0. Statistical analyses were performed separately for measurement and count data. The measurement data is represented by mean ± SD, and the comparison between groups is performed by t-test; the count data is calculated by n (%), and the comparison between groups is performed by χ2. Normality tests were conducted on continuous variables using the Shapiro-Wilk method. Statistical analyses of the measured data were performed using an independent sample t-test (two-tailed Student’s t-test). Statistical significance was set at P < 0.05.
The research route used in this study is illustrated in Figure 1. As shown in Table 1, there were no significant differences in age or disease type between the two groups.
| Group | Age (year) | Disease type (example) | |||
| Gallbladder or bile duct stones | Cholecystic polypus | Hepatic cyst | Other | ||
| Observation group (n = 49) | 47.32 ± 3.72 | 19 | 13 | 11 | 6 |
| Control group (n = 49) | 46.53 ± 3.85 | 20 | 12 | 12 | 5 |
| t/χ2 | 1.033 | 0.200 | |||
| P value | 0.304 | 0.978 | |||
The length of hospitalization, hospitalization cost, operation time, first implantation time, exhaust time, and first post
| Group | Length of stay (day) | Hospitalization cost (ten thousand yuan) | Time of surgery (min) | First time (hour) | Evacuation time (hour) | Time of the first defecation after the operation (hour) |
| Observation group (n = 49) | 7.25 ± 1.38 | 0.75 ± 0.23 | 78.52 ± 15.23 | 15.31 ± 3.53 | 22.36 ± 2.53 | 39.21 ± 6.52 |
| Control group (n = 49) | 13.12 ± 3.25 | 1.23 ± 0.51 | 103.25 ± 23.62 | 35.52 ± 5.85 | 41.52 ± 3.89 | 56.53 ± 8.75 |
| t value | 11.637 | 6.006 | 6.160 | 20.705 | 28.903 | 11.111 |
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
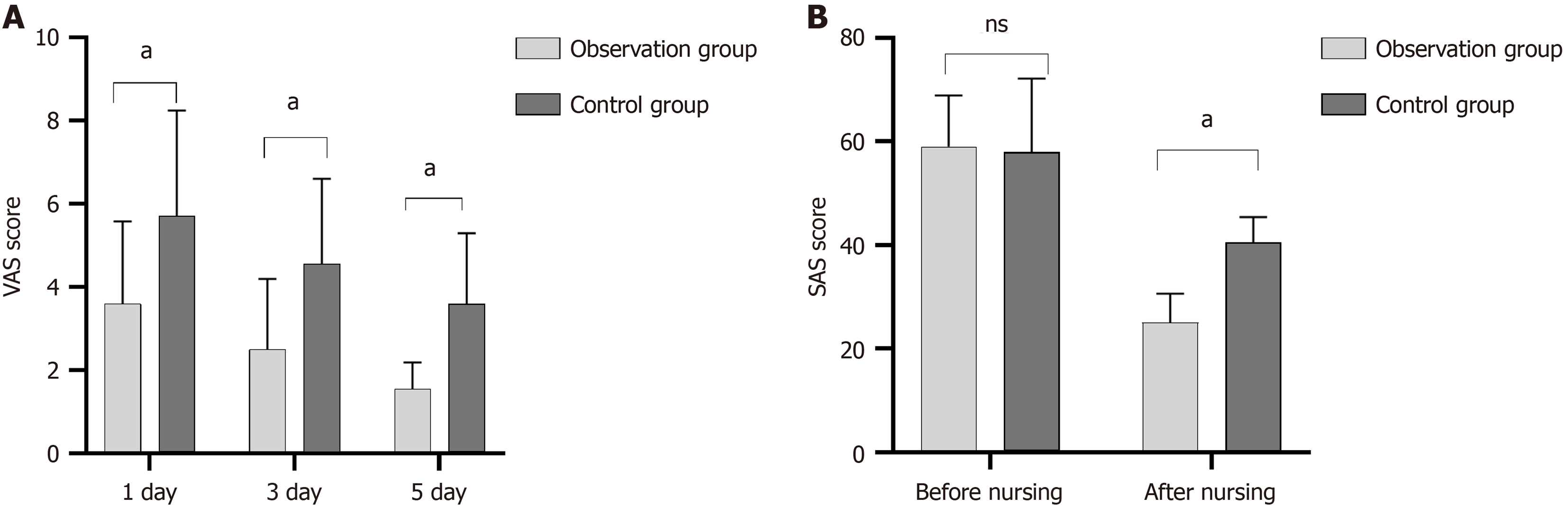
The visual analog scale (VAS) scores of the observation group on days 1, 3, and 7 were lower than those of the control group (P < 0.05; Figure 2A). The SAS scores were not significantly different between the two groups (P = 0.795) before nursing. As shown in Figure 2B, the SAS scores of both groups were lower after than before nursing, and the SAS score of the observation group was lower than that of the control group (P = 0.021).
In the observation group, the wound complication rate was 4.05%, which was significantly lower than that of the control group (18.36%; χ2 = 5.018, P = 0.025; Table 3).
| Group | Infection of incisional wound | Pressure sores | Pulmonary infection | Poor wound healing | Total incidence |
| Observation group (n = 49) | 1 (2.04) | 0 (0.00) | 0 (0.00) | 1 (2.04) | 2 (4.08) |
| Control group (n = 49) | 3 (6.12) | 2 (4.08) | 1 (2.04) | 3 (6.12) | 9 (18.36) |
| χ2 | - | - | - | - | 5.018 |
| P value | - | - | - | - | 0.025 |
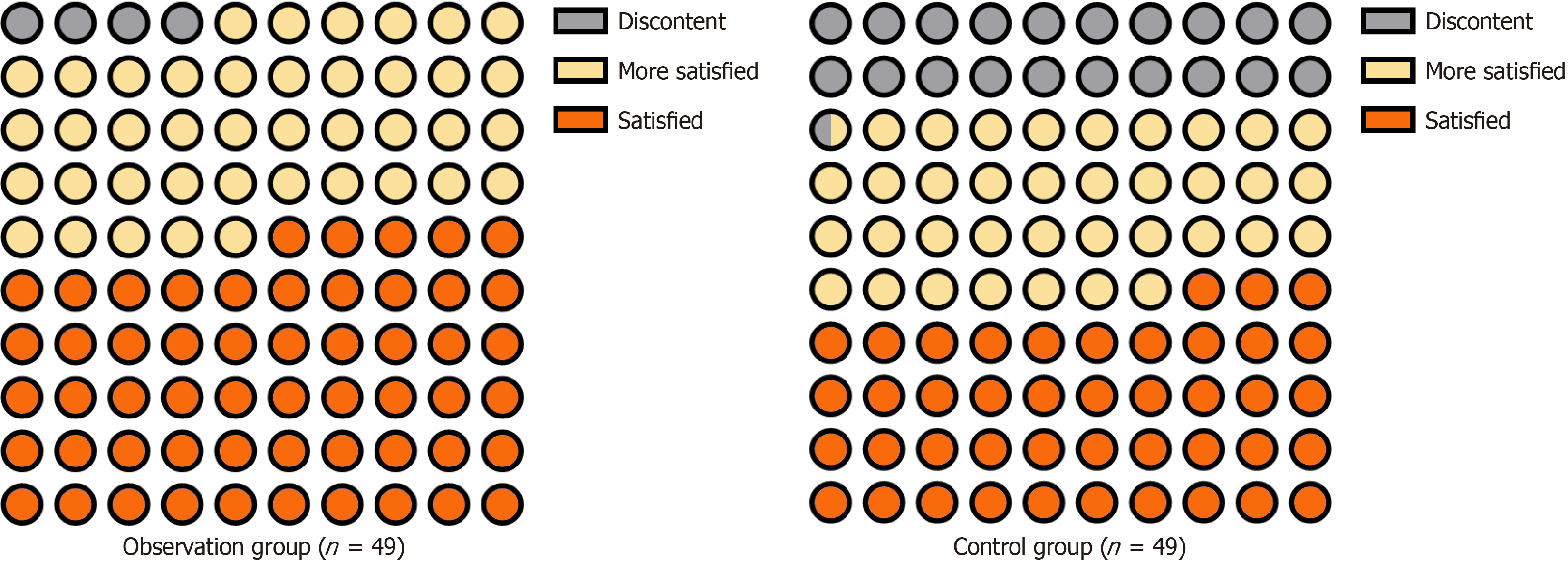
In the observation group, the nursing satisfaction was 95.92%, which was significantly higher than the 79.59% reported in the control group (χ2 = 6.078, P = 0.014; Table 4 and Figure 3).
| Group | Discontent | More satisfied | Satisfied | Segree of satisfaction |
| Observation group (n = 49) | 2 (4.08) | 20 (40.82) | 27 (55.10) | 47 (95.92) |
| Control group (n = 49) | 10 (20.41) | 18 (36.73) | 21 (42.86) | 39 (79.59) |
| χ2 | - | - | - | 6.078 |
| P value | - | - | - | 0.014 |
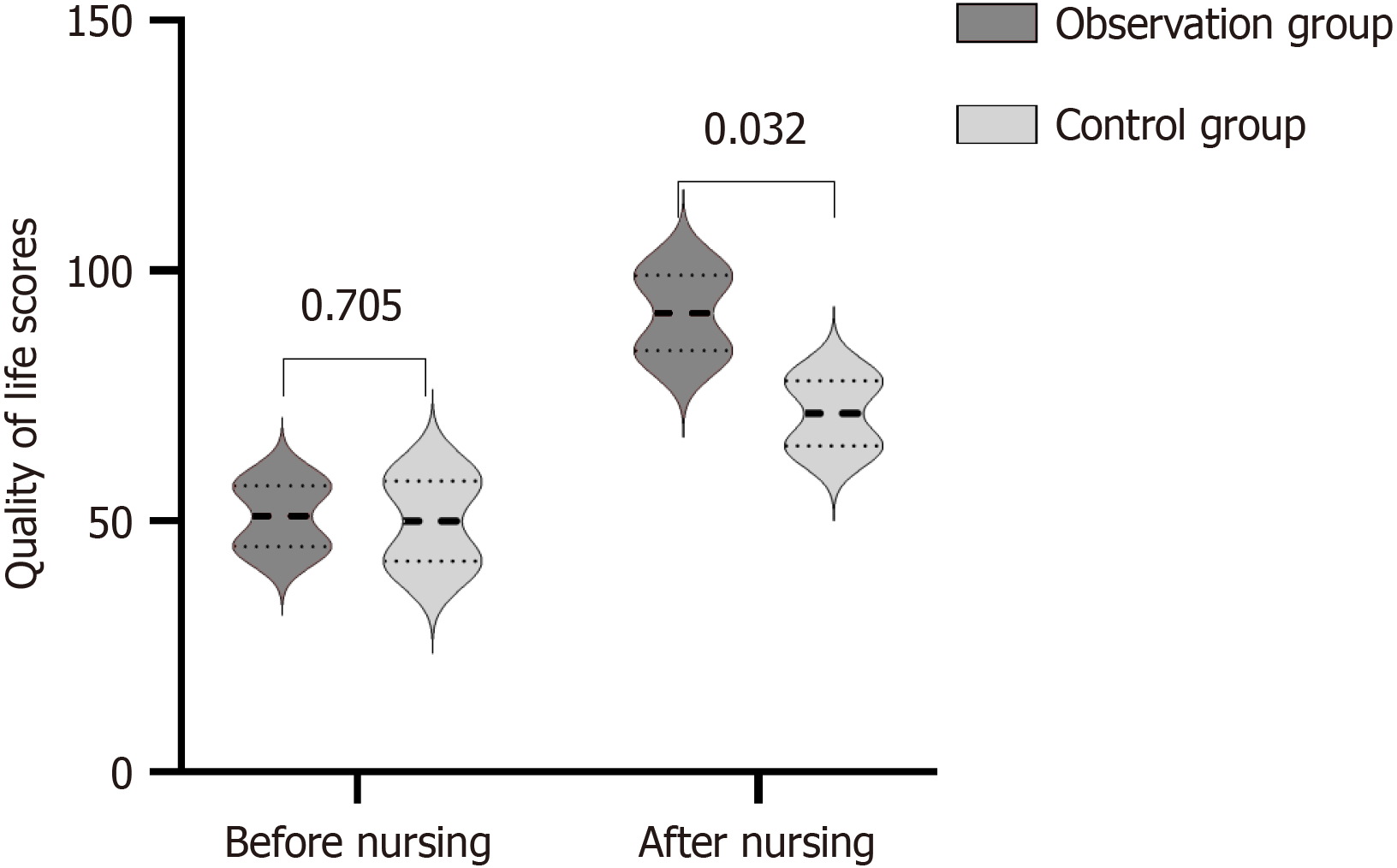
Before nursing, there was no significant difference in the QoL scores between the two groups (P = 0.705). After nursing, the QoL score of the two groups was higher in the observation group than in the control group (P = 0.032; Figure 4).
Surgery is an important treatment option for patients with hepatobiliary surgical diseases[9]. Treatment is highly targeted, has obvious effects, and can be performed accurately and quickly[10]. However, it is invasive, the anatomical structure of the hepatobiliary system is more complex, and the operation is difficult, with different degrees of stress reactions and complications common after surgery[11]. Additionally, the functional recovery of surgical patients is slow[12]. Related complications prolong hospitalization time, reduce patient confidence in treatment, increase the risk of disease, easily induce doctor-patient disputes, and affect the reputation of the hospital[13]. Therefore, effective nursing measures are particularly important to improve the QoL and prognosis of patients undergoing hepatobiliary surgery.
In this study, the length of hospitalization, hospitalization cost, operation time, first implantation time, exhaust time, and first postoperative defecation time were shorter in the FTS group than those in the control group (P < 0.05), sug
These improvements may be due to the following reasons: (1) Preoperative patient and patient health education and psychological intervention to establish a correct perception of the disease, increase confidence in fighting the disease, and reduce bad mood[14]. Moreover, it is recommended to drink appropriate amounts of sugar water or warm boiled water 2 hours before surgery, which is conducive to inhibiting postoperative catabolism; reducing the incidence of postoperative insulin resistance; relieving preoperative hunger, thirst, anxiety, and other feelings; supplementing appropriate energy for patients; and improving surgical tolerance[15]. The FTS concept does not require the insertion of a gastric tube before surgery, and the catheter can be removed 1 d after surgery to facilitate early mobilization[16]. Research has reported that conventional indwelling gastric tubes increase patients’ psychological tension, fear, and other negative emotions, can cause throat discomfort, and increase the risk of lung and throat infections[17]; (2) Paying attention to the maintenance of the patient’s body temperature during intraoperative nursing to reduce the occurrence of related complications caused by body temperature; and (3) In pain management in postoperative care, appropriate pain medication intervention can relieve pain, whereas opioid analgesics should be prohibited to reduce the occurrence of intestinal paralysis. Postope
Perioperative application of the FTS concept in patients undergoing hepatobiliary surgery can effectively improve their negative mood and QoL, reduce wound complications, improve nursing satisfaction, accelerate rehabilitation, and reduce hospitalization costs.
| 1. | Tan B, Yang QY, Fan B, Li Q, Zhang XY. Digital Subtraction Angiography-Guided Percutaneous Kyphoplasty in Treatment of Multi-Segmental Osteoporotic Vertebral Compression Fracture: A retrospective single-Center study. J Pain Res. 2023;16:169-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Cloyd JM, Mizuno T, Kawaguchi Y, Lillemoe HA, Karagkounis G, Omichi K, Chun YS, Conrad C, Tzeng CD, Odisio BC, Huang SY, Hicks M, Wei SH, Aloia TA, Vauthey JN. Comprehensive Complication Index Validates Improved Outcomes Over Time Despite Increased Complexity in 3707 Consecutive Hepatectomies. Ann Surg. 2020;271:724-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 3. | Eslami G, Salehi R, Samaee H, Habibi V, Shokrzadeh M, Moradimajd P. Relationship Between Selenium Trace and Patient Outcome After Open-Heart Surgery. Anesth Pain Med. 2020;10:e105895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Wang S, Zhang Y, Ma X, Lin L, Tian L. Nursing measures in the fast-track surgery on negative emotions in breast cancer patients: A meta-analysis. Medicine (Baltimore). 2023;102:e34896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Liu Y. Application of fast track surgery in routine nursing for patient with colorectal cancer. Saudi J Biol Sci. 2017;24:1939-1942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Song L, Jin Q, Zhu L, Liu Z, Cheng W. Application of Rapid Rehabilitation Surgical Nursing Combined With Continuous Nursing in Self-Care Ability, Medication Compliance and Quality of Life of Renal Transplant Patients. Front Surg. 2022;9:844533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Mao Y, Yang L. Clinical application of electroacupuncture in enhanced recovery after surgery. Front Rehabil Sci. 2023;4:1135618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Zhang M, Li C, Rao F. Effect Evaluation of Perioperative Fast-Track Surgery Nursing for Tibial Fracture Patients with Computerized Tomography Images under Intelligent Algorithm. Contrast Media Mol Imaging. 2022;2022:2629868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Pang Z, Wang X, Wu Y, Zhang H, Huang A, Li X. Construction and Empirical Study of Nursing Quality Evaluation Index System of Hepatobiliary Surgery Based on ERAS Concept. Comput Math Methods Med. 2022;2022:1117880. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Taha A, Eroğlu H, Demirbaş İE, Demir B, Dilektaşli E. Impact of Short-Term Weight Loss on Hemostasis and Thrombosis after Bariatric Surgery. Surg Res Pract. 2023;2023:1729167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Yan T, Lei S, Zhou B, Huang Y, Li X, Zhang J, Huang Q, Zhang L. Association between preoperative anemia and postoperative short-term outcomes in patients undergoing colorectal cancer surgery - a propensity score matched retrospective cohort study. BMC Anesthesiol. 2023;23:307. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Zhao J, Dong X, Zhang Z, Gao Q, Zhang Y, Song J, Niu S, Li T, Chen J, Wei FL. Association of Use of Tourniquets During Total Knee Arthroplasty in the Elderly Patients With Post-operative Pain and Return to Function. Front Public Health. 2022;10:825408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Turaga AH. Enhanced Recovery After Surgery (ERAS) Protocols for Improving Outcomes for Patients Undergoing Major Colorectal Surgery. Cureus. 2023;15:e41755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 14. | Liu Q, Wang J, Han J, Zhang D. Effect of Combining Operating Room Nursing Based on Clinical Quantitative Assessment with WeChat Health Education on Postoperative Complications and Quality of Life of Femoral Fracture Patients Undergoing Internal Fixation. J Healthc Eng. 2022;2022:2452820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Zhou X, Ye X, Guo X, Liu D, Xu J, Hu F, Zhai Y, Gao Y, Xu X, Dong Z, He J. Safety of SGLT2 Inhibitors: A Pharmacovigilance Study from 2013 to 2021 Based on FAERS. Front Pharmacol. 2021;12:766125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 16. | Shi BW, Xu L, Gong CX, Yang F, Han YD, Chen HZ, Li CG. Preoperative Neutrophil to Lymphocyte Ratio Predicts Complications After Esophageal Resection That can be Used as Inclusion Criteria for Enhanced Recovery After Surgery. Front Surg. 2022;9:897716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | He H, Yang G, Wang S, Han X, Li J. Fast-track surgery nursing intervention in CRC patients with laparotomy and laparoscopic surgery. Medicine (Baltimore). 2022;101:e30603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Nie N, Yin Z, Zheng J, Lin X, Chen Y, Xie X, Ding X, Li P, Yang J. Clinical Efficacy of Nutritional Intervention Combined with Muscle Exercise on Sarcopenia Patients with Femoral Fracture: A Pilot Randomized Controlled Trial. Biomed Res Int. 2023;2023:3222686. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Zhang Y, Tao K, Yu J, Chen C, Zheng Q, Lei S, Zhong X, Liu L, Wang W, Wang Q, Li E, Luo Y, Zhang G, Feng X, Li Y, Wang J. Evaluation of early liquid drinking after radical gastrectomy in gastric cancer: a Chinese multicenter propensity score matching analysis. Gastroenterol Rep (Oxf). 2023;11:goad029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |