Published online Jan 27, 2024. doi: 10.4240/wjgs.v16.i1.239
Peer-review started: October 15, 2023
First decision: November 16, 2023
Revised: November 25, 2023
Accepted: December 12, 2023
Article in press: December 12, 2023
Published online: January 27, 2024
Processing time: 102 Days and 0.5 Hours
At present, there is no unified and effective treatment for extreme corrosive esophageal stenosis (CES) with esophagotracheal fistula (ETF). This case had extreme and severe esophageal stenosis (ES) and ETF after ingesting an enzyme-based chemical detergent, resulting in a serious pulmonary infection and severe malnutrition. Upper gastrointestinal imaging showed that he had an ETF, and endoscopy showed that he had extreme and severe esophageal stricture. This case was complex and difficult to treat. According to the domestic and foreign lite
A patient came to our hospital with extreme ES, an ETF, and severe malnutrition complicated with pulmonary tuberculosis 1 mo after the consumption of an enzy
We report, for the first time, a patient with extreme CES complicated with ETF, where the endoscope could not be passed through his esophagus but he could be examined by bronchoscopy and treated by EIM, ESP, and EBD.
Core Tip: Patients who have extreme corrosive esophageal stenosis (CES) with esophagotracheal fistula (ETF) often suffer a lot and have bad quality of their lives. Currently, there are no clinical evidence-based guidelines, and there is great uncertainty regarding the best treatment approach. We report, for the first time, a patient with extreme CES complicated with ETF, where the endoscope could not be passed through his esophagus but he could be examined by bronchoscopy and treated by endoscopic incision method, esophageal stent placement, and endoscopic balloon dilation.
- Citation: Fang JH, Li WM, He CH, Wu JL, Guo Y, Lai ZC, Li GD. Endoscopic treatment of extreme esophageal stenosis complicated with esophagotracheal fistula: A case report. World J Gastrointest Surg 2024; 16(1): 239-247
- URL: https://www.wjgnet.com/1948-9366/full/v16/i1/239.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i1.239
Corrosive esophageal stenosis (CES) is rare but destructive, placing a significant burden on contemporary health systems around the world[1]. Patients who have extreme CES with esophagotracheal fistula (ETF) often suffer from typical chest pain, severe pulmonary infection-related symptoms, malnutrition, etc., which seriously affect the quality of their lives[2]. Because of the rarity of this adverse event, clinicians usually have limited personal experience with it. Currently, there are no clinical evidence-based guidelines, and there is great uncertainty regarding the best treatment approach.
For the treatment of extreme CES with ETF, there is no relevant guidelines or a relatively unified treatment plan in clinical practice. At present, the main clinical treatments for esophageal stenosis (ES) are the endoscopic incision method (EIM), endoscopic balloon dilation (EBD), gastroscope-assisted bougienage, esophageal stent placement (ESP), and local injection of glucocorticoids[3].
Recently, a patient came to our hospital with extreme ES, an ETF, and severe malnutrition complicated with pulmo
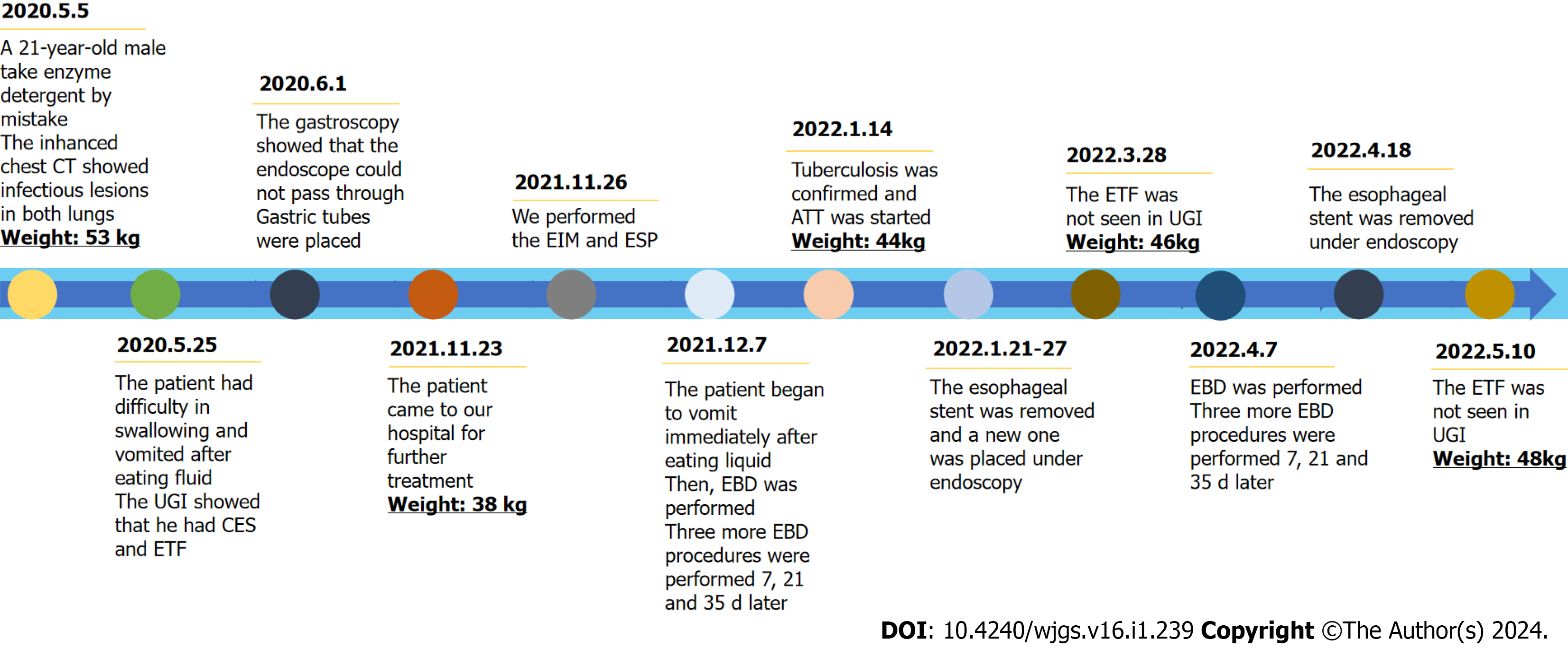
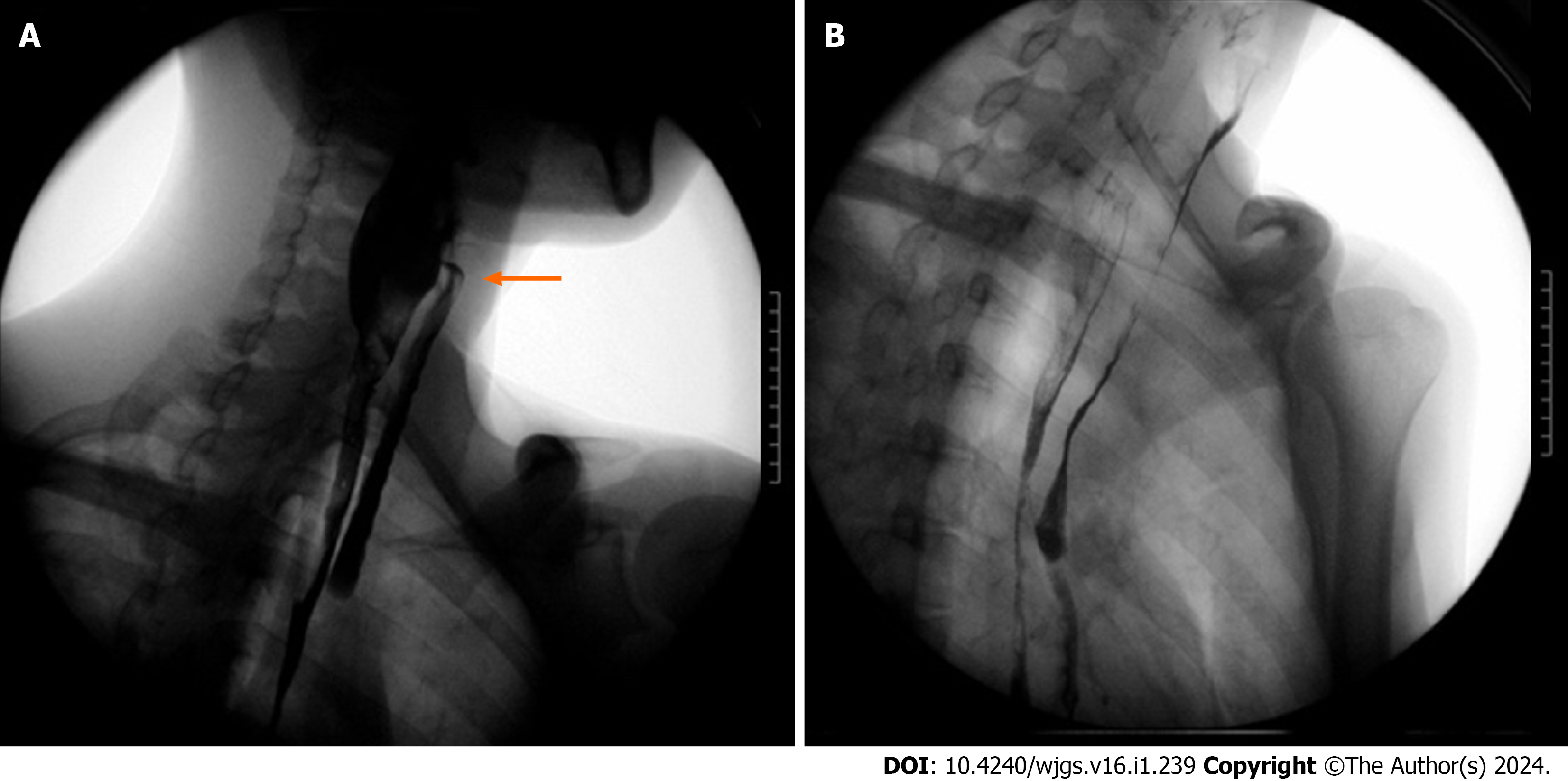
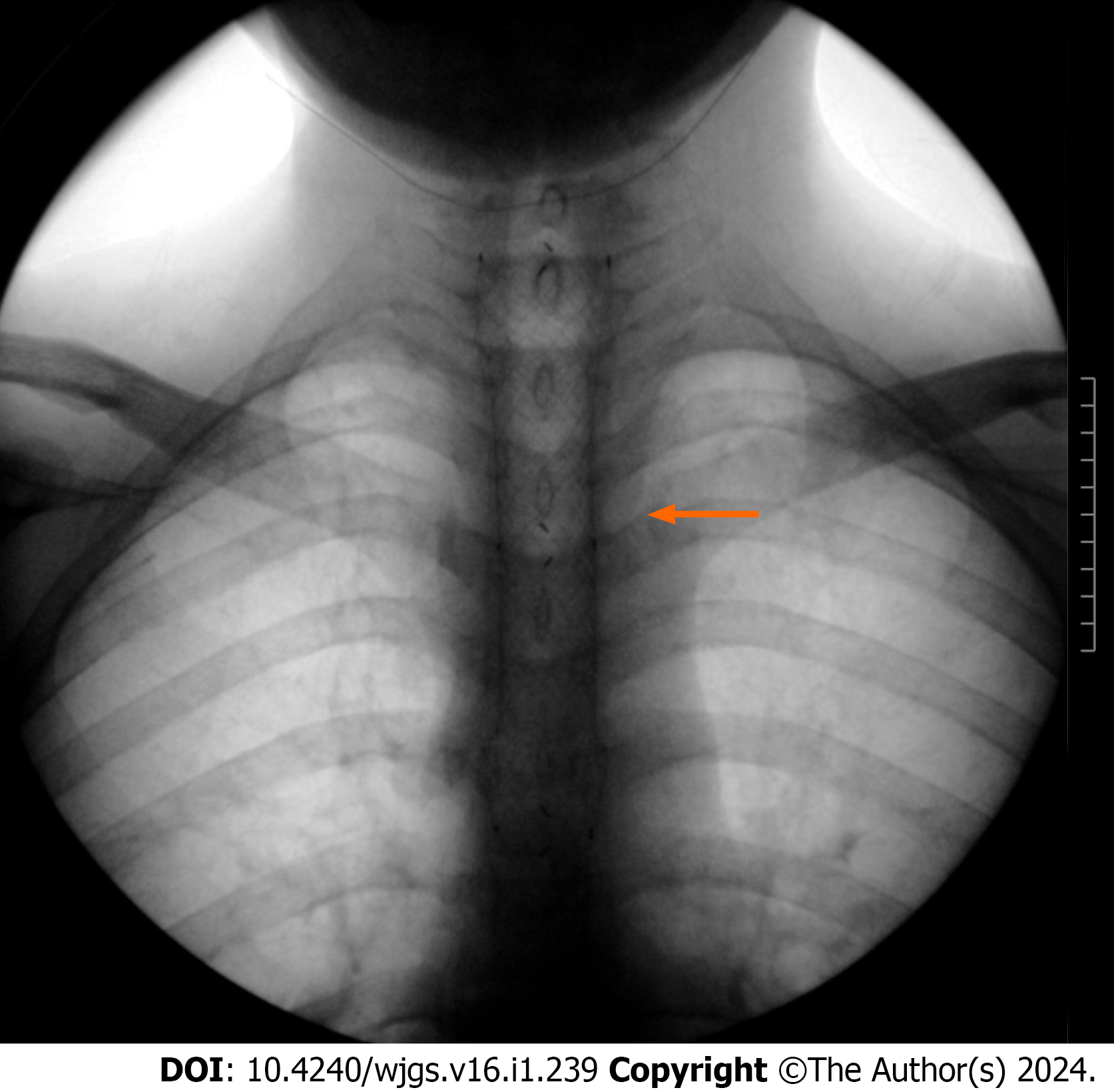
A 21-year-old man came to the Department of Gastroenterology of our hospital for "having upper gastrointestinal pain with dysphagia after mistakenly consuming an enzyme-based detergent 6 mo ago". The patient developed burning sensation and pain in the the oral, throat, and chest behind the sternum and under the xiphoid process after taking an enzyme-based detergent by mistake on May 5, 2020. The pain score was 8 (total score: 10). Contrast enhanced chest computed tomography (CT) showed infectious lesions in both lungs. Anti-infection treatment was given and the patient was discharged after improvement. On May 25, 2020, the patient had difficulty in swallowing and vomited after eating fluid food. Upper gastrointestinal imaging (UGI) showed that he had CES and pharyngeal fistula (Figure 2), but the patient decided to return to the local hospital for treatment. Gastroscopy was performed in the First Hospital of Lanzhou University on June 1, 2020, which showed that the esophagus was narrow 19 cm away from the incisors, and the endo
The patient mistakenly consumed an enzyme-based detergent 6 mo ago.
The patient was healthy in the past.
There was no remarkable personal and family history.
The Kubota water swallow test suggested that the patient had grade 5 swallowing function. The trachea was in midline, the breathing sounds in both lungs were not clear, and moist rales could be heard in the left lung. Bowel sounds at a frequency of 3-5 times/min could be heard.
The results are all shown in Table 1.
| Laboratory test | Routine blood test | Biochemical test | Tuberculosis related test | Weight (kg) | |||||||
| Hemoglobin (g/L) | Leucocytes (109/L) | High-sensitivity C-reactive protein (mg/L) | Albumin (g/L) | Preal | Apolipo | PPD test | Serum tuberculosis antibody | T-spot test | Detection of Myco | ||
| May 5, 2021 | 148 | 15.88 | 10.52 | 44.10 | 0.179 | 0.59 | - | - | - | - | 53.0 |
| November 23, 2021 | 106 | 7.71 | 80.81 | 26.30 | 0.051 | 0.63 | - | Negative | Negative | - | 38.0 |
| November 26, 2021 | 91 | 6.60 | 26.30 | 33.60 | 0.149 | 0.76 | - | Negative | Negative | Positive | 38.5 |
| Janurary21, 2022 | 112 | 6.87 | 9.0 | 32.40 | 0.091 | 0.51 | - | Negative | Negative | Positive | 44.0 |
| May 10, 2022 | 140 | 5.29 | 8.12 | 39.60 | 0.218 | 0.94 | - | - | Negative | Negative | 47.8 |
The UGI and endoscopy results are shown in the figures.
Extreme ES complicated with an ETF.
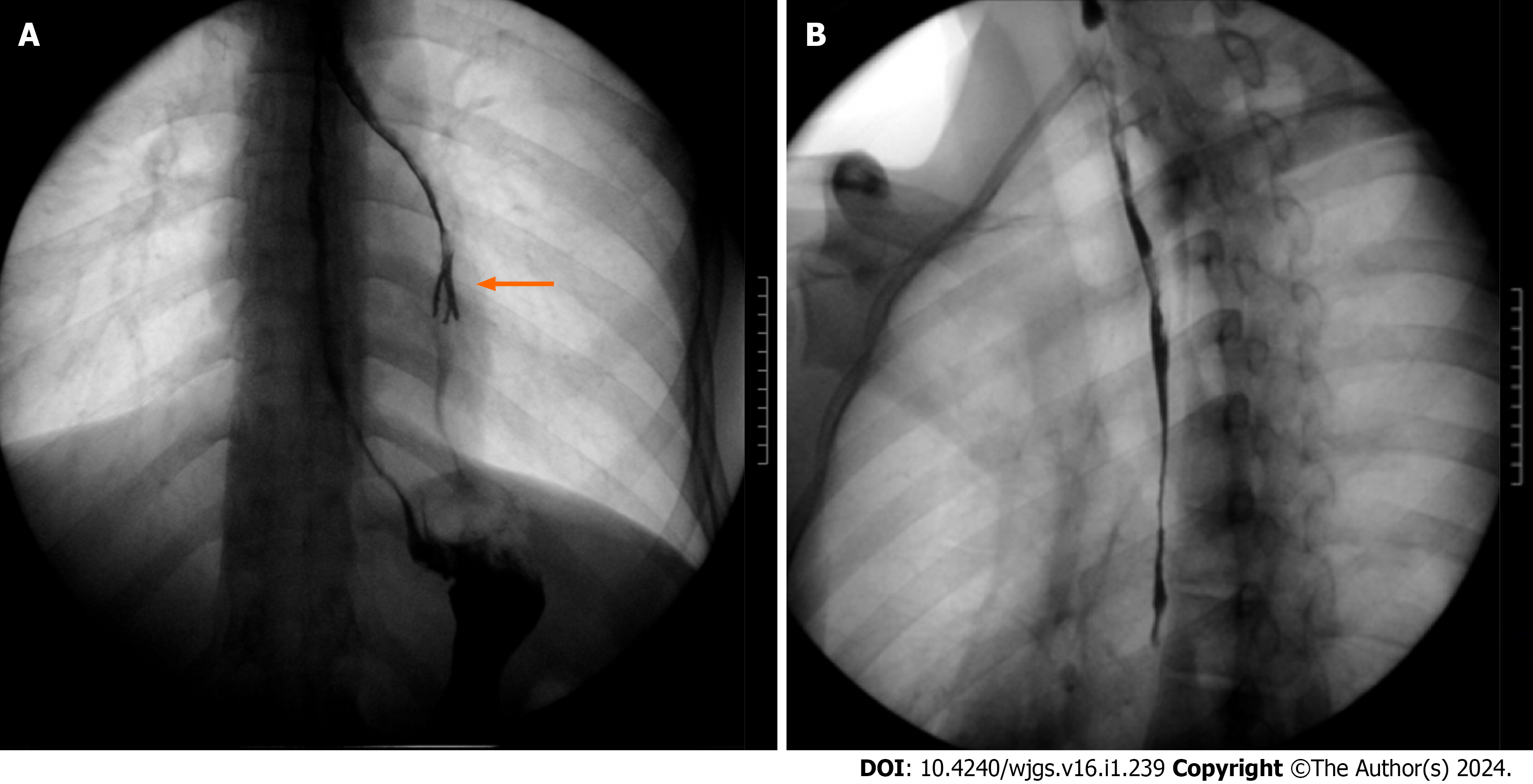
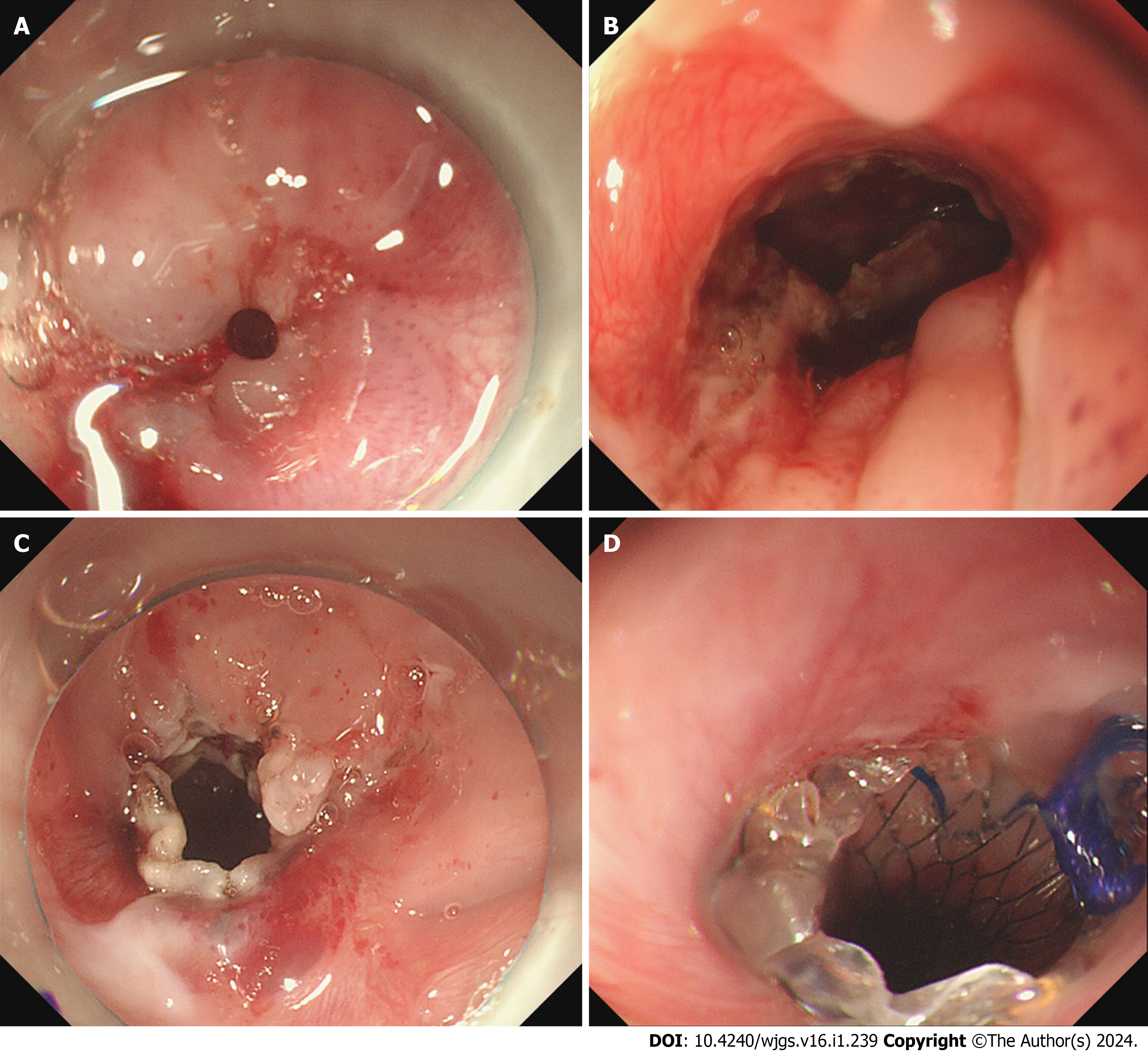
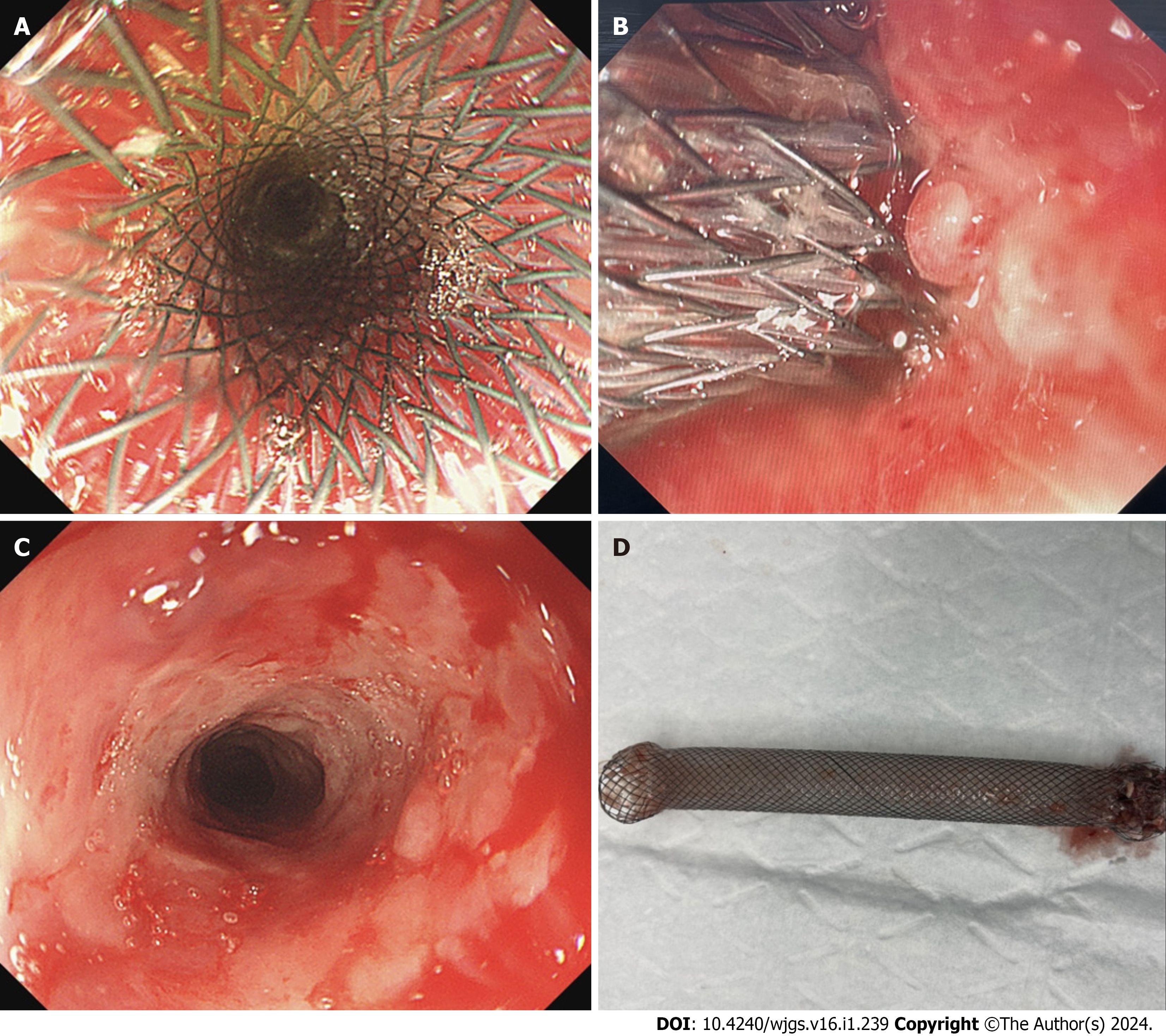
The patient was treated with nutritional support therapy and anti-infection therapy. The test results are shown in Table 1. Contrast-enhanced chest CT showed that the patient had ES. Hypopharyngeal and esophageal injury and partial gas accumulation can be seen. There were pneumonic lesions in both lungs. UGI (Figure 3) showed that the pharyngeal fistula disappeared, the esophageal mucosa was rough and disordered, the esophageal wall was irregular, an ETF appeared, and the fistula was located at the level of the 4th thoracic vertebra. After determining the location of the ETF, relevant surgical contraindications were excluded. On November 26, 2021, bronchoscopy (Olympus BF-260) instead of gastroscopy was used to evaluate the esophagus, which showed that the whole esophagus was narrow and twisted, and three fistulas were found in the upper part of the esophagus (Figure 4A and B). The obvious stenosis part was located 19 cm and 38 cm away from the incisors. The patient’s following conditions posed great challenges to the treatment: (1) The patient had total ES combined with ETF. Gastroscope could not be use to assess the condition and treat him; and (2) The length of ES in the patient is much longer than that of the existing stent.
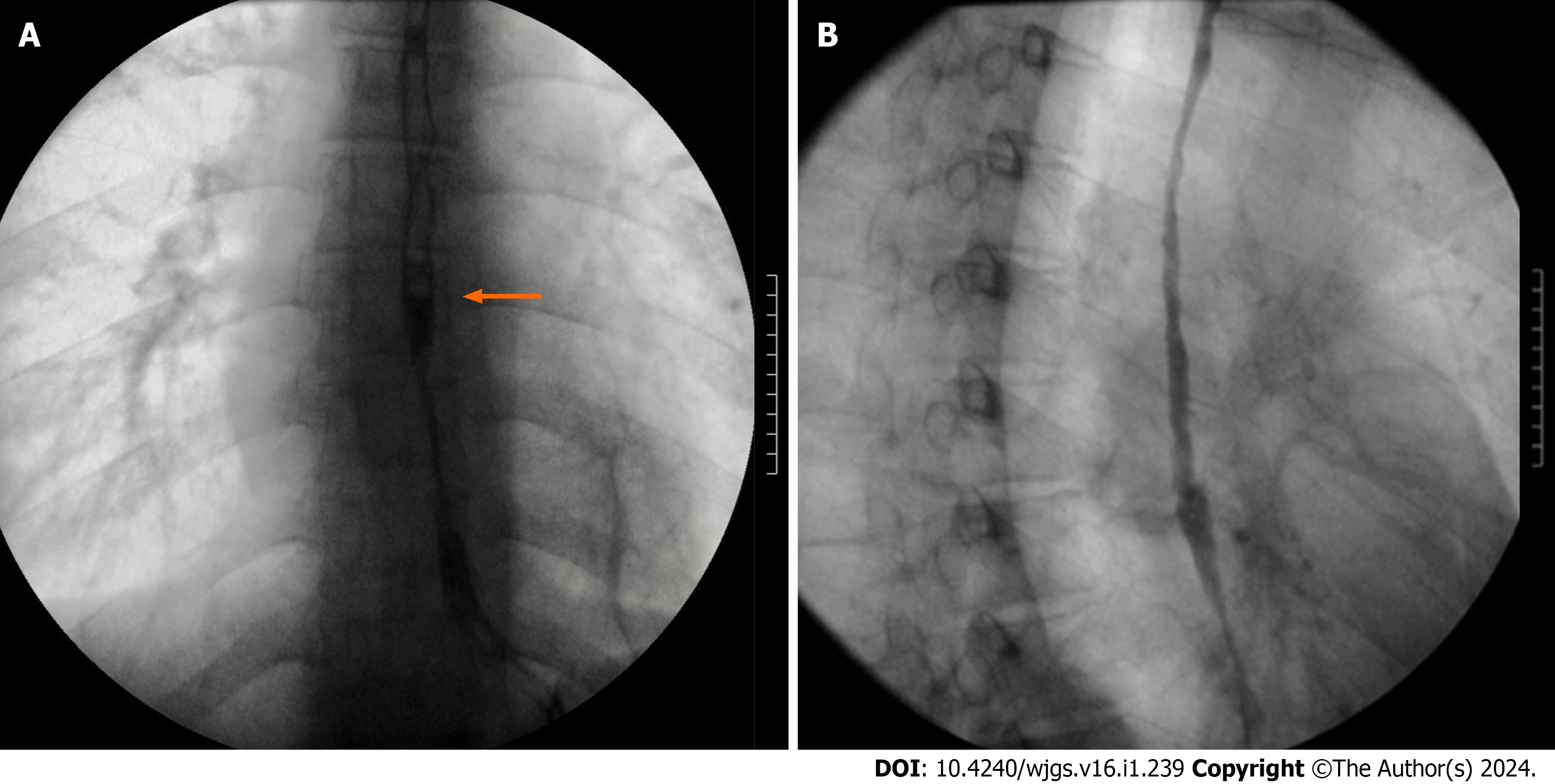
We performed EIM with a gastroscope (Olympus GIF-H290Z) at 19 cm (Figure 4C). The bronchoscope was used again to enter the gastric cavity and to insert the guidewire (AG-5043-3545, Hangzhou Honghai Medical Devices Co., Ltd.). After the bronchoscope was withdrawn, the gastroscope was placed to send the esophageal stent pusher (NES-20-120-070, Hangzhou Qianshenghui Science and Technology Ltd.) along the guidewire. Then, we released the covered stent under direct vision of the endoscope. It was found that the release position was good, the upper end was located 17 cm away from the incisors (Figure 4D), the inside of the stent was clear, and there was no obvious bleeding. On the second day after the operation, the patient had minor pharyngeal pain, with no obvious retrosternal pain and no pain under the xiphoid process. He drank fluids and had no discomfort after eating. Esophageal radiography (Figure 5) showed that the esophageal dilation was good, no contrast medium overflow was found, and the cardia opened and contracted regularly and freely. On December 7, 2021, the patient began to vomit immediately after eating liquid food. The vomitus was food. The rating grade of the Kubota water swallow test was 5. Then, EBD was performed with an endoscope (No.: ES128549). The stent was still in place. A narrow esophageal lumen could be seen 38 cm away from the incisors, and the endoscope could not pass through. A guidewire was placed through the narrow part, and a columnar dilatation balloon of the duodenal papilla (BDC-12/55-7/18, Hangzhou Weichuang Medical (Group) Co., Ltd.) was placed along the guidewire. After dilation, the mucosa was torn, and the gastroscope could enter the gastric cavity through the narrow segment. Three more EBD procedures were performed 7, 21, and 35 d later (BDC-12/55-7/18, BDC-15/55-7/18, and BDC-15/55-7/18, Hangzhou Weichuang Medical (Group) Co., Ltd.). The patient could drink fluids or semi-fluids during this period.
During hospitalization, the patient still suffered from cough and expectoration and maintained a low fever every day. Although the laboratory examination results did not support the diagnosis of pulmonary tuberculosis, we used bronchoscopy to collect bronchial lavage fluid to perform Mycobacterium tuberculosis culture. Tuberculosis was confirmed (Table 1) and four-drug antituberculosis therapy (ATT) was started. Finally, the patient's persistent pain behind the sternum and under the xiphoid process, pharyngeal pain, and other discomfort disappeared, the nutritional index in
To avoid the implantation of the stent into the esophageal mucosa, we decided to remove the esophageal stent and place a new one. We removed the stent on January 1, 2022. Seven days later, a new stent was placed. The two operations went well, upper esophageal mucosal erosion was found, the esophageal cavity dilated well, and the fistulas disappeared. ES could be seen 36 cm away from the incisors. The patient kept having semi-fluids. Sustained nutritional support and ATT were given. Since UGI showed that the fistula had been blocked, we removed the stent on April 18, 2022 (Figure 6) and four times of EBD was performed since April 7, 2022 to dilate the esophagus. A month later, UGI showed that the fistula was still blocked (Figure 7), but the esophagus was still partially narrow. The patient could have semi-fluids at that time. ETF may recur, and the patient may have to accept EIM, ESP, and EBD in the future.
Since the physiological structure of the esophagus is thin and tubular, it is prone to stenosis when subjected to major injuries, such as corrosion and surgery. The incidence of esophageal stenosis is approximately 1.1/100000 cases per year[4]. Chronic ETF is extremely rare and occurs in approximately 3% of patients with chemically CES[1]. The treatment mainly includes the repair of airway defects and esophageal reconstruction, which usually uses staged operation[5,6]. The first stage, as most clinicians think, is endoscopic esophageal dilatation (including EBD and bougienage)[7]. This case is very special for the following reasons: First, the patient was very young. If we chose surgical resection of the whole esophagus, the quality of life would be greatly reduced in the coming decades. Second, endoscopy suggested that the patient’s esophagus was entirely narrow with multiple fistulas. The guidewire was very likely to be displaced during the EBD. Even if the dilation were successful, the large balloon pressure could easily tear the fistula mucosa and cause further damage. Considering comprehensively, we immediately performed EIM, which made it possible to expand the esopha
There is no unified clinical treatment for complex CES. EIM is a new technology developed in recent years that was first used to treat recurrent Schatzki rings. Since 2012, it has gradually replaced EBD to be used to treat complex esopha
As one of the treatments for ES, ESP has many adverse events, such as chest pain, stent displacement or shedding, and tissue embedding. Fuccio et al[12] performed a meta-analysis indicating that approximately 28.6% of patients had esopha
Patients with extreme CES often have to accept EBD dozens of times. They go through a great deal, and the esophagus is easy to tear after operation. The medical cost is also high. The expansion success rate for corrosive stenosis is approximately 50%, which is significantly lower than that for other benign stenoses (75%-80%)[7]. For the stenosis part located below the esophageal stent in this case, considering the tear caused by ordinary balloon dilatation, we used the duodenal papilla columnar expansion balloon to expand the esophagus by dividing segments. We performed this three additional times at 7, 21, and 35 d after the initial EBD. The inner diameter of the balloon increased in turn during each expansion. The patient maintained a liquid and semiliquid diet during this period, without obvious tearing, perforation, bleeding, or other adverse events. For the treatment of lower ES, there are two choices: ESP or ESP after EBD. More clinical studies are needed to prove which one has better safety, efficacy, and economic benefits.
For the treatment of benign ES, Xie et al[13] believed that oral administration of glucocorticoids in patients with diabetes, hypertension, infection, tuberculosis, and other patients will lead to aggravation, so it is not recommended. The effect of glucocorticoid injection is ideal, but no drug injection has been proven to be effective for the treatment of chemi
Chemical corrosive esophageal injury should be examined by gastroscopy combined with UGI, nasal endoscopy, and even bronchoscopy when necessary. For treatment, EIM, EBD, and ESP should be chosen according to every patient’s specific situation. Due to entire CES combined with ETF having a wide range of stenosis, the treatment is extremely difficult. Clinical treatment should be taken under individualized assessment, and combined treatment should be given when necessary. In this case, we used a bronchoscope with a thinner diameter to evaluate and treat ES repeatedly instead of a gastroscope, which was rarely used in clinical practice and achieved a perfect effect. Whether the ETF and ES will recur in this patient remains to be observed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Martino A, Italy; Sintusek P, Thailand S-Editor: Lin C L-Editor: Wang TQ P-Editor: Xu ZH
| 1. | Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. Caustic ingestion. Lancet. 2017;389:2041-2052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 2. | Poincloux L, Rouquette O, Abergel A. Endoscopic treatment of benign esophageal strictures: a literature review. Expert Rev Gastroenterol Hepatol. 2017;11:53-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Chai NL, Li LS, Zhou JL. Expert consensus on endoscopic prevention and treatment of benign and malignant esophageal stenosis in China. Zhonghua Changweineijing Dianzizazhi. 2020;7:7-17. |
| 4. | Ruigómez A, García Rodríguez LA, Wallander MA, Johansson S, Eklund S. Esophageal stricture: incidence, treatment patterns, and recurrence rate. Am J Gastroenterol. 2006;101:2685-2692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Gupta V, Kurdia KC, Sharma A, Mishra AK, Yadav TD, Kochhar R. Tracheoesophageal fistula in adults due to corrosive ingestion: challenges in management. Updates Surg. 2015;67:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Yalçin Ş, Ciftci AO, Karnak I, Tanyel FC, Şenocak ME. Management of acquired tracheoesophageal fistula with various clinical presentations. J Pediatr Surg. 2011;46:1887-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19:3918-3930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 273] [Cited by in RCA: 208] [Article Influence: 17.3] [Reference Citation Analysis (7)] |
| 8. | Muto M, Ezoe Y, Yano T, Aoyama I, Yoda Y, Minashi K, Morita S, Horimatsu T, Miyamoto S, Ohtsu A, Chiba T. Usefulness of endoscopic radial incision and cutting method for refractory esophagogastric anastomotic stricture (with video). Gastrointest Endosc. 2012;75:965-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Wu P, Wang F, Wu X, Nie J, Ge X, Li Q, Lin J, Miao L. Comparison of esophageal stent placement versus endoscopic incision method for treatment of refractory esophageal anastomotic stricture. Ann Palliat Med. 2019;8:462-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Li J, Zhao H, Ma Z, Liu B. Endoscopic incision and selective cutting for primary treatment of benign esophageal anastomotic stricture: outcomes of 5 cases with a minimum follow-up of 12 month. Ann Palliat Med. 2020;9:1206-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Hordijk ML, Siersema PD, Tilanus HW, Kuipers EJ. Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc. 2006;63:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Fuccio L, Hassan C, Frazzoni L, Miglio R, Repici A. Clinical outcomes following stent placement in refractory benign esophageal stricture: a systematic review and meta-analysis. Endoscopy. 2016;48:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 13. |
Xie YX, Guo JY, Yao H, Shi GQ.
Progress in endoscopic prevention and treatment of benign gastrointestinal stenosis |
| 14. | Mahawongkajit P, Tomtitchong P, Boochangkool N, Mingmalairak C, Awsakulsutthi S, Havanond C. A prospective randomized controlled trial of omeprazole for preventing esophageal stricture in grade 2b and 3a corrosive esophageal injuries. Surg Endosc. 2021;35:2759-2764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Khan A, Chakravarty A, Naqishbandi R, Qamar S. Atypical presentation of acquired tracheo-oesophageal fistula in an adolescent girl with pulmonary tuberculosis. BMJ Case Rep. 2022;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |