Published online Sep 27, 2023. doi: 10.4240/wjgs.v15.i9.1841
Peer-review started: May 14, 2023
First decision: July 4, 2023
Revised: July 17, 2023
Accepted: July 31, 2023
Article in press: July 31, 2023
Published online: September 27, 2023
Processing time: 131 Days and 3.5 Hours
Indocyanine green (ICG) is a water-soluble fluorescent dye that is minimally toxic and widely used in gastrointestinal surgery. ICG facilitates anatomical identification of structures (e.g., ureters), assessment of lymph nodes, biliary mapping, organ perfusion and anastomosis assessment, and aids in determining the adequacy of oncological margins. In addition, ICG can be conjugated to artificially created antibodies for tumour markers, such as carcinoembryonic antigen for colorectal, breast, lung, and gastric cancer, prostate-specific antigen for prostate cancer, and cancer antigen 125 for ovarian cancer. Although ICG has shown promising results, the optimization of patient factors, dye factors, equipment, and the method of assessing fluorescence intensity could further enhance its utility. This review summarizes the clinical application of ICG in gastrointestinal surgery and discusses the emergence of novel dyes such as ZW-800 and VM678 that have demonstrated appropriate pharmacokinetic properties and improved target-to-background ratios in animal studies. With the emergence of robotic technology and the increasing reporting of ICG utility, a comprehensive review of clinical application of ICG in gastrointestinal surgery is timely and this review serves that aim.
Core Tip: Indocyanine green (ICG) is a safe and widely-used fluorescent dye for anatomy delineation, tumour identification and lymph node mapping. ICG has demonstrated superior results in organ perfusion and anastomosis assessment. However, there is still room for further optimization of patient factors, dye factors, and fluorescence intensity assessment. Other dyes, such as ZW-800 and VM678, have shown better pharmacokinetic properties and target-to-background ratios in animal studies, and novel contrast agents that target unique pathology, such as conjugating ICG to artificially created antibodies, are being developed for disease detection and management.
- Citation: Lim ZY, Mohan S, Balasubramaniam S, Ahmed S, Siew CCH, Shelat VG. Indocyanine green dye and its application in gastrointestinal surgery: The future is bright green. World J Gastrointest Surg 2023; 15(9): 1841-1857
- URL: https://www.wjgnet.com/1948-9366/full/v15/i9/1841.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i9.1841
Indocyanine green (ICG) was first developed during World War II for colour imaging, and later in the 1950s, used in the medical field to quantify cardiac and renal function. It is a minimally toxic, water-soluble fluorescent dye that is rapidly taken up by the liver and excreted into the bile ducts within minutes after injection, making it ideal for such applications[1,2]. ICG is a favourable contrast agent for in vivo application due to its 820 nm near-infrared (NIR) emission wavelength, minimising interference from blood and tissue autofluorescence at 500-600 nm[3]. After intravenous injection, ICG binds to plasma proteins and has a half-life of three minutes. As the lymph is rich in protein content, lymphatics and lymph nodes (LNs) can be easily mapped after ICG injection. In general, ICG is safe at doses below 0.5 mg/kg body weight, however adverse reactions like nausea, pyrexia, and anaphylaxis may occur[1-3].
As early as 1959, ICG quantification was used to assess hepatic function. Given ICG’s affinity for the blood, ICG levels in the blood corresponded directly with hepatic function[2]. It was also used to determine cardiac output, and for videoangiography for assessment of choroidal neovascularization[4,5].
Recently, fuelled by the emergence of robotic technology, ICG has gained widespread usage in the identification of tumours, lymphatic mapping, and evaluation of organ perfusion and anastomosis[6]. With its increasing application in general surgery, novel uses for ICG are continuously being uncovered. Therefore, the present review aims to provide a summary and critical analysis of the established applications of ICG in general surgery, as well as emerging avenues for future research and development.
An electronic search of PubMed (MEDLINE), Embase (Ovid), and Google Scholar was performed for the concepts of (“Indocyanine Green” [MeSH Terms]), (“Esophagus” [MeSH Terms]), (“Stomach” [MeSH Terms]), (“Liver” [MeSH Terms]), (“Gallbladder” [MeSH Terms]), (“Pancreas” [MeSH Terms]), (“Adrenal Glands” [MeSH Terms]), (“Spleen” [MeSH Terms]), (“Intestine, Small” [MeSH Terms]), (“Colon” [MeSH Terms]), (“Rectum” [MeSH Terms]), (“Peritoneum” [MeSH Terms]), (“Blood Vessels” [MeSH Terms]), (“Abdomen” [MeSH Terms]), (“General Surgery” [MeSH Terms]) in January 2023. Relevant articles published in English were identified and summarised to produce an up-to-date review on the history, present and future use of ICG in abdominal surgery. We discuss clinical application of ICG in individual organs with a cranial to caudal approach of human anatomy.
Lymphatic mapping in oesophageal cancer: Oesophageal cancer is a biologically aggressive disease with poor prognosis despite treatment, endoscopic or surgical, with the intent to cure[7]. Lymphadenectomy significantly improves accuracy of tumour staging and impacts long-term survival of patients with oesophageal cancer. However, at present, most lymphadenectomies are performed based on anatomical territory understanding and surgeons’ experience and expertise with wide variation in the extent of nodal harvest. Current American Joint Committee on Cancer (AJCC) guidelines recommend the removal of ≥ 20 LNs for T2 disease, or ≥ 30 for T3 and T4 disease, while National Comprehensive Cancer Network guidelines recommend the removal of at least 15 LNs to ensure adequate nodal staging[8,9].
Studies have proposed the use of radiocolloid tracers for sentinel LN (SLN) mapping, but these largely require open procedures with back table dissection of the specimen and radiation exposure[10]. Radioisotope methods are unable to predict locations of primary SLNs perioperatively with high accuracy. This can be attributed to poor spatial resolution and low detail regarding surrounding anatomy, for reasons including the shine-through phenomenon, where the radiation flare of the primary tumour outshines the SLN near to the primary tumour[11,12]. A feasibility study by Yuasa et al[12] proposed the use of NIR fluorescence imaging (FI) using ICG, together with preoperative computed tomography (CT) lymphography for SLN localisation[10]. This involved the injection of ICG in 2 regions around the tumour after thoracotomy, and the oesophagus and LNs that fluoresced were harvested.
A first in human pilot trial by Hachey et al[10] demonstrated the feasibility of using NIR guided lymphatic mapping as the sole modality for SLN identification in minimal access oesophagectomy. Regional LNs distinct from the oesophagus specimen were identified in 66.7% (6/9) of the patients where ICG diluted in human serum albumin (HSA) was used, as compared to 40% (2/5) of the patients with ICG only. In both groups, ICG was injected peritumourally via 4-corner submucosal injections adjacent to each lesion[10]. The dilution of ICG with HSA increases the quantum yield, which is the efficacy at which fluorescent molecules convert absorbed photons into emitted photons, and also the SLN retention[13,14]. Furthermore, the combination of ICG with neomannosyl HSA, which targets the macrophage mannose receptor CD206, was trialled by Kim et al[15]. This combination was used on porcine models for oesophageal SLN identification and demonstrated higher fluorescence signal, LN retention and allowed for more precise real-time SLN detection in surgery. The use of ICG for lymphatic mapping may allow for targeted lymphadenectomy, decreased operative time, and hence decreased postoperative complications while ensuring the completeness of resection and improving cancer-free survival[16].
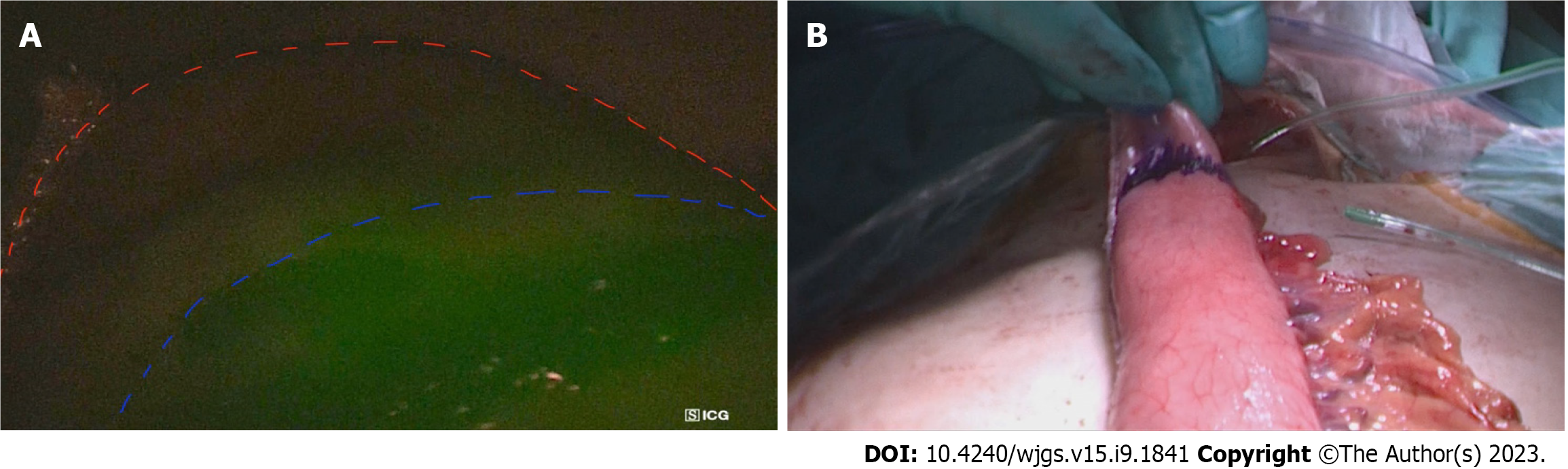
Evaluation of oesophago-gastric anastomosis: The evaluation of gastrointestinal-oesophageal anastomosis is the most common application of ICG FI for oesophageal pathologies. There is significant postoperative morbidity and mortality associated with anastomotic leak (AL) post-oesophagectomy. A major factor contributing to oesophago-gastric AL is ischaemia at the tip of the gastric conduit, due to insufficient perfusion from the isolated right gastroepiploic artery[17]. Figure 1 below illustrate this. Therefore, the use of ICG FI intra-operatively to assess perfusion can be valuable as it allows for live monitoring of conduit perfusion, early detection of reversible conduit ischaemia, and hence better selection of the optimal site for anastomosis. Other optical techniques such as optical coherence tomography and NIR spectroscopy have been assessed by authors, but ICG remains the most widely used given the safety, reliability, and ease of use[18].
However, the use of ICG fluoroscopy for assessment of perfusion does not provide surgeons with a quantitative assessment of perfusion but is instead estimated based on the time from initial ICG enhancement at the root of the gastro-epiploic artery until gastric tube tip. Noma et al[19] suggested that anastomosis be performed proximal to the point of fluorescence reached in 30 s, or the 90 s rule established by Kumagai et al[20]. Noma et al[19] reported significant reduction in leakage rate and duration of postoperative intensive care unit (ICU) stay for the ICG group, with no increase in other complications such as pneumonia. In a meta-analysis including 5 studies and 616 patients, Slooter et al[21] concluded that ICG reduces the risk of AL and graft necrosis [odds ratio (OR) = 0.30, 95% confidence interval (CI): 0.14-0.63]. Based on this, we computed the number needed to treat (NNT) for ICG to reduce 1 case of AL or graft necrosis as 6.6 oesophagectomies.
Identification of chylothorax post-oesophagectomy: Besides the use of ICG in oesophageal surgery for assessment of perfusion, a new and upcoming use of ICG is for the detection of chyle leak post-oesophagectomy. The incidence of chylothorax ranges from 1.1%-21% in oesophagectomy patients, with extensive LN dissection and en bloc resection of the thoracic duct for oncological reasons as risk factors[22]. Traditionally, the ingestion of milk immediately before surgery, or the intraoperative administration of milk into the duodenum were techniques used to identify the site of chyle leak[23].
Kaburagi et al[24] however reported the successful use of intraoperative ICG fluorescence lymphography for the identification of the chyle leak, and to confirm ligation of the thoracic duct transabdominally. Kamiya et al[23] similarly achieved this through the injection of 1.5 mL of ICG subcutaneously at the inguinal region bilaterally, and obtained fluorescence images of lymph flow 14 min after injection using a NIR camera. This is in contrast to other techniques such as lymphoscintigraphy, which can identify chyle leak, but cannot delineate the exact site of leak without the use of a single-photon emission computerized tomography scan[25]. Management of the chyle leak reduces the need for postoperative nutritional interventions, infectious morbidity, and reduces the length of hospital stay[22].
ICG guided LN dissection: Gastrectomy with D2 lymphadenectomy is a technically demanding surgery requiring experience and expertise to achieve radical lymphadenectomy. With advances in minimal access technology, adoption of training curricula and fellowship programs, laparoscopic gastrectomy is routine in many institutions. ICG can help to improve LN harvest while minimizing complications. Chen et al[8] reported a randomized control trial with 266 gastric cancer patients comparing ICG use in gastrectomy with conventional gastrectomy. The ICG group had significantly greater LNs retrieved compared to the non-ICG group (49.6 LNs vs 41.7 LNs respectively; P < 0.001). In addition, in a matched cohort study of 37 patients who underwent robotic gastrectomy with D2 LN dissection demonstrated higher mean total number of harvested LNs in the ICG group than the control (50.8 vs 40.1, P = 0.03)[26]. Higher nodal yield aids accurate staging and potentially contributes to improved survival outcomes. The iGreenGO study is a prospective multicentre study which seeks to determine if the use of ICG necessitates a change in surgical conduct, such as performing more extensive dissection after the surgeon has already completed D2 lymphadenectomy without ICG aid[27]. ICG remains a useful surgical adjunct for a surgeon early in their learning curve and for advanced gastric cancers.
Sentinel LN mapping: The stomach has a complex lymphatic drainage system. Gastrectomy with D2 lymphadenectomy remains the gold standard for resectable gastric cancer, however this has higher morbidity than D1 lymphadenectomy therefore may be excessive in clinical T1/T2 N0 gastric cancers where LN metastasis maybe limited. SLN mapping may be a solution to this conundrum where radical lymphadenectomy may be carried out only if SLN is positive. In a prospective multicentre trial by Kitagawa et al[28], 397 patients underwent SLN biopsy (SLNB), and the method showed high accuracy in detecting sentinel nodes and metastatic SLNs, with a false negative rate of 1%. Future studies should compare long-term oncologic outcomes of SLN guided surgery vs conventional surgery, but this has the potential to change surgical management of gastric cancer as what SLNB has done for breast cancer surgery.
Localisation of gastric tumour to guide resection in early gastric cancer: Early gastric cancer may not be visible to the surgeons on the serosal surface. Injection of ICG submucosally around the tumour will emit fluoresce on the serosal surface and aid to ensure adequacy of resection margins when performing subtotal gastrectomy. In a retrospective study including more than 500 patients with early gastric cancers in the body of the stomach, Cho et al[29] demonstrated that ICG diffusion area along the gastric wall secured a resection margin of > 28 mm.
Leak tests after sleeve gastrectomy and other anastomosis based bariatric surgeries: ICG has been used by bariatric surgeons for leak test after sleeve gastrectomy and other bariatric surgeries. ICG is instilled via nasogastric or orogastric tubes after the sleeve gastrectomy or after anastomosis is completed. Kalmar et al[30] reported a sensitivity of 100.0% and specificity of 98.3% for ICG based leak tests. Hagen et al[31] reported a series of 95 patients who had Roux-en-Y gastric bypass who had leak tests with air and with a mix of methylene blue and ICG. In their series, no patients had a positive leak test with air, no patients showed methylene blue excretion, and an ICG leak was observed in 4.2% (4/95) patients, suggesting that ICG maybe more sensitive for small ALs. These results need to be validated by others.
ICG in revisional bariatric surgery: ICG has proven it’s utility in revisional bariatric surgery. Anatomy of the stomach is distorted in cases of previous gastric surgery especially if complications such as ulcers or perforations have occurred. In addition, in cases where records of previous surgeries are also not available makes deciphering the exact procedure the patient had underdone, vascular pedicles taken etc. challenging. This makes the surgery technically challenging with potential for increased morbidity. ICG helps to highlight areas of poor vascularity, identify old staple lines to enable better surgical planning to prevent crossing of staples lines, leaving blind gastric pouches and performing anastomosis in areas of good vascularity[32].
Tumour visualization: Hepatectomy remains the gold standard in treatment of liver malignancies and some benign masses. However, the key to a successful oncological resection is negative margins, which requires clear segment demarcations based on vascular and lymphatic supply[33].
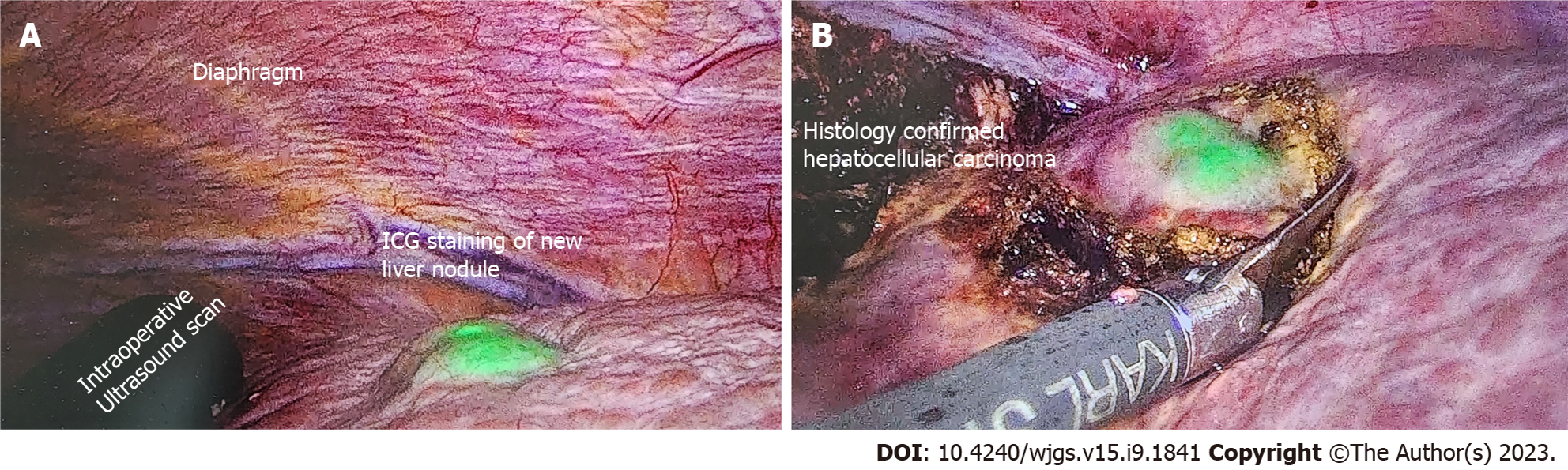
ICG is typically administered intravenously several hours or days before surgery and will be taken up by hepatocytes, which illuminate under an infrared source. ICG is then excreted in the bile and disappears from healthy hepatocytes within a few hours before the surgery begins. However, as the cancerous hepatocytes are underactive and metabolize the ICG slowly, these will be the only areas that illuminate during the operation. Figure 2 shows the use of ICG for the resection in a patient with hepatocellular carcinoma.
In non-hepatocellular cancers, the areas around the tumour will retain the ICG instead. This is termed tumour and peritumoural fluorescence and helps differentiate between hepatocellular and non-hepatocellular cancers intraoperatively[34]. However, since ICG is metabolized by the liver, further studies need to be conducted with regards to dose adjustment for cirrhotic patients, who constitute a large proportion of liver cancer patients[35].
In addition, in a prospective study of 54 patients who underwent robotic assisted liver resections with ICG demonstrated that ICG use decreased operative time and achieved more resections with no histopathologically proven macro- or microscopic tumour residual[36].
Liver function assessment: Proper patient selection is vital for hepatectomies as even healthy patients without underlying liver disease can have severe postoperative liver dysfunction. For patients with pre-existing liver disease, even a minor resection could lead to posthepatectomy liver dysfunction or failure. ICG clearance has been noted as a valuable tool to identify patients that are at risk of developing posthepatectomy liver failure (PHLF)[37,38].
The ICG retention test after 15 min (ICG-R15) is used conventionally. A single bolus of ICG is administered intravenously, and venous blood samples are drawn and read with a pulse spectrophotometer at 15 min[39]. Literature suggests that ICG-R15 of more than 14% is prognostic of PHLF[38-40]. A study by Schwarz et al[37] comprising 698 patients similarly showed that patients with impaired ICG clearance were twice as likely to have postoperative liver dysfunction. A recent retrospective study however highlighted that in patients treated with associating liver partition and portal vein ligation for staged hepatectomy, ICG-R15 overestimated the true liver function increase post-operatively[41]. These results remain to be validated, and are essential in tailoring treatment to prevent PHLF.
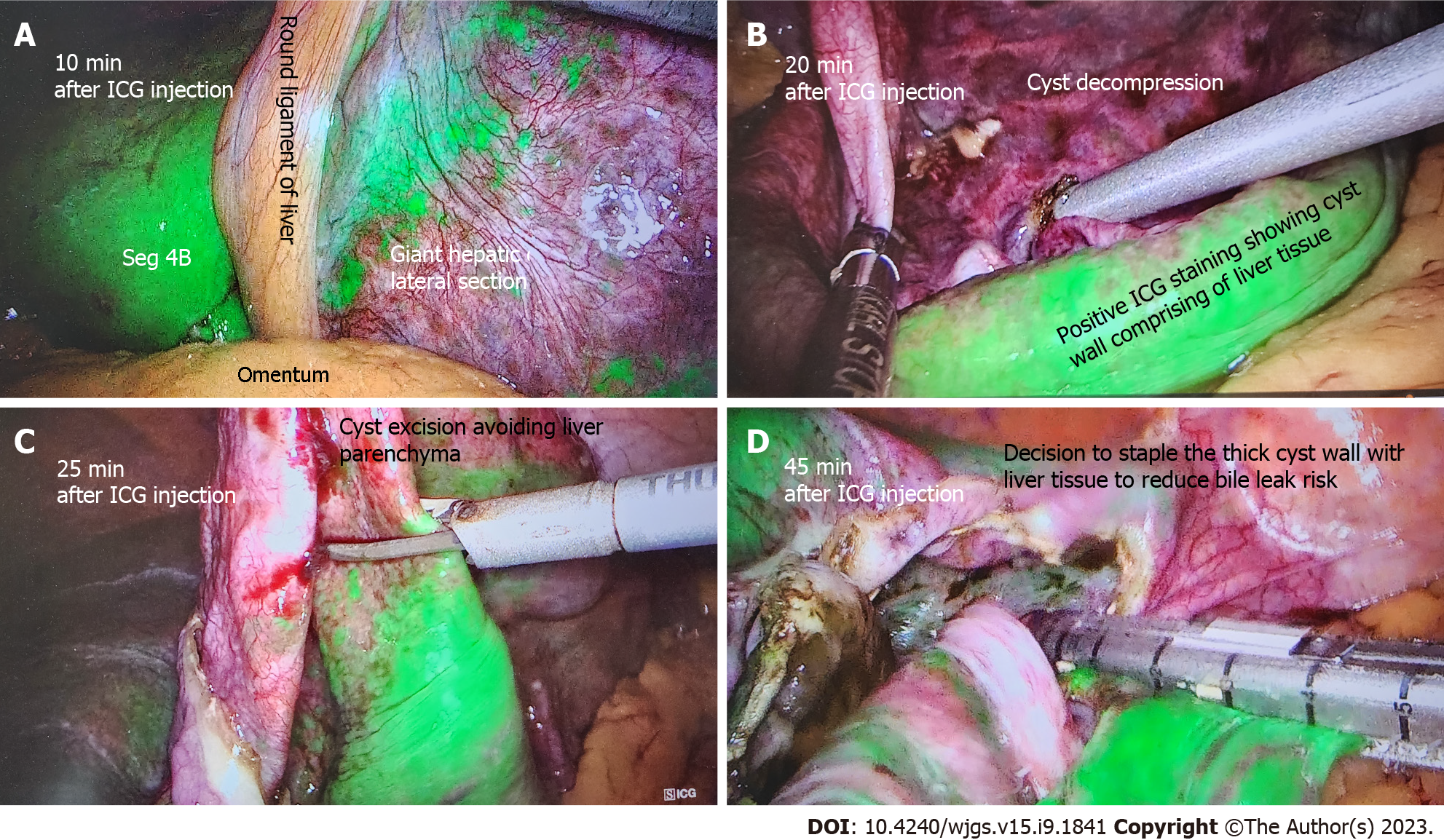
Liver cyst: Several studies have reported the use of ICG FI for liver cyst fenestrations performed laparoscopically. Une et al[42] reported the successful implementation of ICG FI to allow for clear distinguishment of cyst from liver parenchyma to guide resection. Hanaki et al[43] also reported that ICG FI allowed for visualisation of small bile ducts located within the cyst wall to decrease the risk of bile leaks and prevent iatrogenic bile duct injury (BDI). Authors injected ICG intravenously 1-h prior to surgery. In addition, ICG can be administered via endoscopic nasal biliary drain during hepatic cyst deroofing procedures to allow for immediate visualisation, and can also allow for assessment of minor biliary leakage from resection margins or staple lines, preventing postoperative biliary leakage[44]. Figure 3 illustrates the use of ICG FI for liver cyst deroofing.
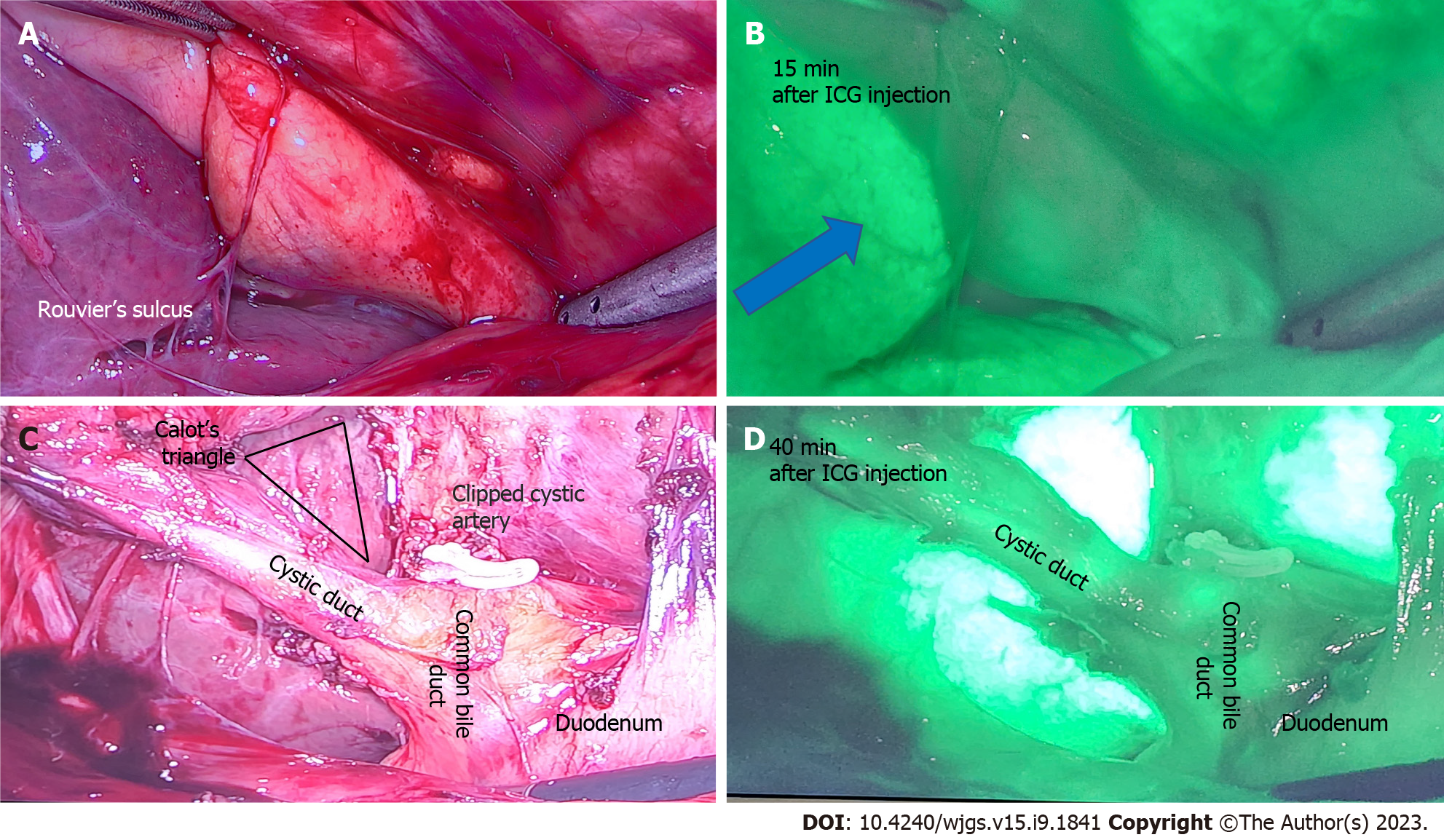
Biliary mapping during laparoscopic cholecystectomy: Laparoscopic cholecystectomy is one of the most frequently performed operations worldwide. BDI is an uncommon but significant complication associated with cholecystectomy as it reduces patients’ quality of life and exposes surgeon to litigation[45]. The common cause of BDI are misidentification of anatomy, severe scarring and fibrosis due to chronic pathology and surgical experience. In estimated 10%-15% patients, it is not possible to obtain critical view of safety to expose Calot’s triangle and a surgeon has to determine the next course of action that may include calling for help[46] and conversion to a bail-out procedure like subtotal cholecystectomy[47]. ICG NIR fluorescence instead provides detailed and real time anatomical mapping of the biliary structures to reduce BDI risk[48]. Yong et al[49] highlighted in his case study of a 40-year-old male undergoing laparoscopic cholecystectomy, that the cannabidiol (CBD) and cystic duct were only discernible via ICG FI and not at all under white light.
While intraoperative cholangiography remains the gold standard for laparoscopic cholecystectomies, intraoperative ultrasound and ICG NIR FI are often considered as good alternatives. ICG NIR FI has been found to only be useful in discerning the extrahepatic biliary tree, while intraoperative cholangiography is useful for evaluating the intrahepatic biliary tree[50]. However, ICG NIR FI is superior in terms of causing less radiation exposure[49]. Figure 4 below demonstrates the use of ICG in laparoscopic cholecystectomy.
ICG can be administered through either the intravenous or intrabiliary route. For the intravenous route, ICG is administered 30 min before the surgery. Since ICG is metabolized by the liver and excreted in bile, the biliary structures are visualized intraoperatively immediately after dissection of the Calot’s triangle[51,52]. For the intrabiliary route, the gallbladder is punctured with cholangiogram or pigtail catheter mid-surgery, and the bile is aspirated and mixed with ICG solution, and then re-injected into the gallbladder[45]. Currently, the intrabiliary route is proven to be more efficacious in mapping the biliary tree. In a retrospective study of 24 patients by Shibata et al[53], ICG was administered intravenously in 12 patients and intrabiliary for 12 patients. The biliary tree was well-identified in 100% (12/12) of the patients in the intrabiliary group, as compared to only 83.3% (10/12) of the patients in the intravenous group. Ambe et al[52] reported no statistically significant differences in the duration of operation, length of stay in hospital, and risk of BDI when comparing between ICG guided and non-ICG guided laparoscopic cholecystectomy. For this study, the median duration of operation was 53 vs 54 min in the group with and without ICG respectively. Median length of stay was 2 d and no BDI occurred for both groups.
Additionally, studies have also evaluated the use of ICG cholangiography for use in robotic cholecystectomies. In a retrospective study of 184 robotic cholecystectomies by Esposito et al[54] demonstrated this with ICG FI allowing visualization of minimally 1 biliary structure in 99% (182/184) cases, with no laparoscopic or open conversions required.
Gallbladder cancer: Gallbladder cancer (GBC) is associated with high mortality, with a 5-year survival rate of less than 5%[55]. The mainstay of treatment for GBC remains radical resection of the gallbladder, including a central hepatectomy and regional lymphadenectomy. Recent advancements in this area include the increasing use of minimally invasive robotic surgery[56]. Ahmad reported the use of ICG FI in robotic radical resections for GBC in 10 patients, for the purposes of identifying the cystic duct junction with the CBD. This was made easy as NIR FI is a standard feature in daVinciâ surgical robots[56]. In addition, AJCC guidelines recommend removal and evaluation of 6 LNs in GBC resection, however this is rarely achieved[57]. The use of ICG guided regional lymphadenectomies may hence improve our ability to achieve this while reducing the risk of bile duct devascularization, and overcome visualization challenges from scarring and adhesions from previous operations[58,59].
Choledochal cyst excision: The utility of ICG is also explored in identification of pancreatico-biliary junction and distal end of bile duct in a patient with choledochal cyst scheduled for laparoscopic excision[60]. The authors innovated a novel method of exploiting the protein affinity of ICG by mixing ICG with the patient’s own bile juice aspirated from the gallbladder during surgery.
Bilio-enteric anastomosis: In patients undergoing hepaticojejunostomy for a variety of indications, ICG is shown to increase the detection of intra-operative bile leak from the anastomosis, thus allowing surgeons to reinforce the suture line and reducing the risk of post-operative biliary fistulas[61].
Tumour detection: During pancreatic tumour surgery, the extent of the tumour is typically evaluated intraoperatively through visual inspection or, in some cases, with the aid of intraoperative ultrasound. However, accurately delineating tumour boundaries can be difficult due to the presence of inflamed surrounding tissue[62]. Insufficient identification of tumour margins can lead to incomplete tumour resection, a predicament that has been shown to contribute to high recurrence rates ranging from 68% to 72%, as reported in a study by Griffin et al[63].
Novel NIR fluorescent agents have been developed that target tumour-specific cell surface markers, enzymatic activity, or increased glucose metabolism[64-66]. However, these tumour-specific agents are not yet available for clinical use. ICG on the other hand, can identify tumours based on the enhanced permeability and retention (EPR) effect. This effect refers to the dye’s ability to accumulate in tumour spaces for prolonged periods due to the highly porous vessels and poorly developed lymphatics, despite not being tumour specific[67]. However, the EPR effect has been found to be less effective in identifying pancreatic tumours compared to other malignancies such as breast cancer. A study conducted by Hutteman et al[62] revealed that only 12.5% (1/8) patients had a clear fluorescence hotspot corresponding to an adenocarcinoma, with no other useful results noted for the remaining patients. This can be attributed to healthy pancreatic cells having almost equal ICG uptake as tumour cells. The COLPAN study concluded that single-bolus intraoperative ICG was effective in delimiting the area of high fluorescence corresponding to functional pancreatic neuroendocrine tumours. Peak tumour fluorescence was obtained 20 min post administration, and ICG also concentrated in peripancreatic LNs[68].
Assessment of pancreatic perfusion post-pancreaticoduodenectomy: ICG dye can be utilised to confirm adequate perfusion of the pancreatic remnant during surgery. Traditional methods for assessing perfusion include clinical inspection of normal bleeding from the cut surface of the pancreas or Doppler ultrasonography for real-time arterial flow[69,70]. However, ultrasonography has limited spatial resolution and is not proficient in identifying concealed arteries, venous perfusion, or microperfusion[71]. In contrast, ICG binds to plasma lipoproteins, remaining within the intravascular space. ICG is administered intravenously during surgery, and its fluorescence in the remnant confirms adequate perfusion, as demonstrated in a case study by Iguchi et al[72]. Therefore, it is an effective method for evaluating all vascular supply means of the remnant pancreas.
Use in adrenalectomy: Laparoscopic and robotic techniques are now the gold-standard for adrenalectomies, but it hampers surgeons’ ability to receive tactile feedback, which is important for discerning tumour edges and vascular structures[73]. The use of ICG enables differentiation between the hyperfluorescent adrenocortical tissue and hypofluorescent retroperitoneal tissue, facilitating dissection[74]. The best contrast between the adrenal and retroperitoneal fatty tissues was observed 5 min post-injection of ICG[75].
Moreover, ICG guided cortical-sparing adrenalectomy allows for intraoperative visualisation of the boundaries between the normal adrenal cortex and medullary tumour[74]. Phaeochromocytomas were non-fluorescent while healthy cortical tissue was brightly fluorescent, and hence Kahramangil et al[76] reported how when the phaeochromocytoma was small and did not penetrate the cortex, the whole adrenal appeared heterogeneously fluorescent and hence ICG usage was not helpful. It was only when the tumour was large, was the non-fluorescence appreciable for guiding resection.
Following the intravenous administration of ICG, the sequence of enhancement was the arterial anatomy, followed by the adrenal parenchyma, and lastly the adrenal vein. The identification of the vasculature is important, particularly for cases with distorted anatomy such as large adrenal neoplasms, and potentially allows for decreased blood loss[77]. Of note however, the identification of the adrenal vein was inconsistent in a larger prospective study of 100 patients[76].
Laparoscopic splenectomy, as compared to open, has been shown to improve outcomes including blood loss, length of stay and reduction in wound complications[78]. It is unlikely that routine use of ICG would be indicated in straightforward cases. However, it could be useful in the identification and division of the splenic artery and vein in cases where there is anatomic distortion or adhesions from prior inflammation[79]. This is important as bleeding from these vessels can be substantial, and it is more difficult to obtain control in laparoscopic or robotic surgery compared to open surgery. ICG has been shown to be useful in selected cases during splenic surgery as described below.
Splenic aneurysmectomy: ICG has been reported to be helpful in the treatment of splenic artery aneurysms, an extremely rare disorder[80]. Bertolucci et al[81] reported a case where ICG was used in a laparoscopic splenic artery aneurysmectomy to confirm successful clip and resection of aneurysm. The use of ICG FI also enabled assessment of splenic blood supply, allowing for laparoscopic partial splenectomy in 4 patients[79].
Splenic cysts: Dome resection for splenic cysts allows for the preservation of splenic immunological function and has become the primary technique to treat splenic cysts. Masuya et al[82] reported the successful use of ICG fluorescence to assess for the thinning area of the cyst to be punctured. This is beneficial to allow preservation of normal parenchyma and avoid unnecessary splenectomy.
Perfusion assessment: There has been growing use of minimally invasive surgery for the treatment of small bowel pathology in recent years, but laparoscopy reduces the ability to discern signs of irreversible vascular insufficiency such as absence of peristaltic movements, mesenteric pulsations, and discolouration of the bowel wall. ICG angiography for assessment of bowel perfusion aids in determining need and extent of bowel resection.
Use in small bowel obstruction: In the setting of small bowel obstruction, Guerra et al[83] reported the use of ICG fluorescence in 7 patients for assessment of bowel viability. ICG was administered intravenously and in small 2 mL boluses to assess the intestinal microcirculation. Bowel segments that demonstrated patchy fluorescence or non-fluorescence were then resected. ICG as an adjunct for assessment of bowel perfusion is important, as inability to assess bowel viability is the second most common reason for conversion to open surgery in patients with small bowel obstruction[84]. Likewise, Ganguly et al[85] reported the use of ICG FI in 2 patients with incarcerated inguinal hernias containing small bowel. The involved bowel presented dusky areas but ICG administration revealed sufficient fluorescence and bowel resection was avoided.
Use in small bowel ischemia: In mesenteric ischemia, it can be challenging to macroscopically differentiate between reversible and irreversible ischaemic bowel. Intraoperative ICG FI makes it possible to detect non-viable intestine that is not apparent to the naked eye. This may reduce the need for repeated laparotomies to reassess bowel viability[86]. In occlusive mesenteric ischemia, it is logical to determine the region of bowel to resect based on the vascular supply as evident on CT angiogram[87]. However, in non-occlusive mesenteric ischemia, hypoperfusion is due to mesenteric vasoconstriction which makes identifying the precise segment of non-viable bowel difficult. ICG plays a crucial role in helping surgeons determine intraoperatively which regions of the bowel are adequately perfused, and hence decide on the need or extent of resection[86].
In colorectal surgery, ICG’s applications are varied including fluorescent tumour localisation, LN mapping and intraoperative angiography for anastomosis perfusion assessment[88]. Fluorescence guided visualisation continues to gain popularity amongst colorectal surgeons due to its reliability, safety, and ease of use. A survey of 37 centres in the Italian ColoRectal Anastomotic Leakage study group reported that 78.4% (29/37) of centres used fluorescence in all laparoscopic colorectal resections, and 65.5% of surgeons strongly believed the use of FI will become a minimum requirement in the future[89]. Studies have also demonstrated the use of ICG FI in robotic colorectal surgeries[90].
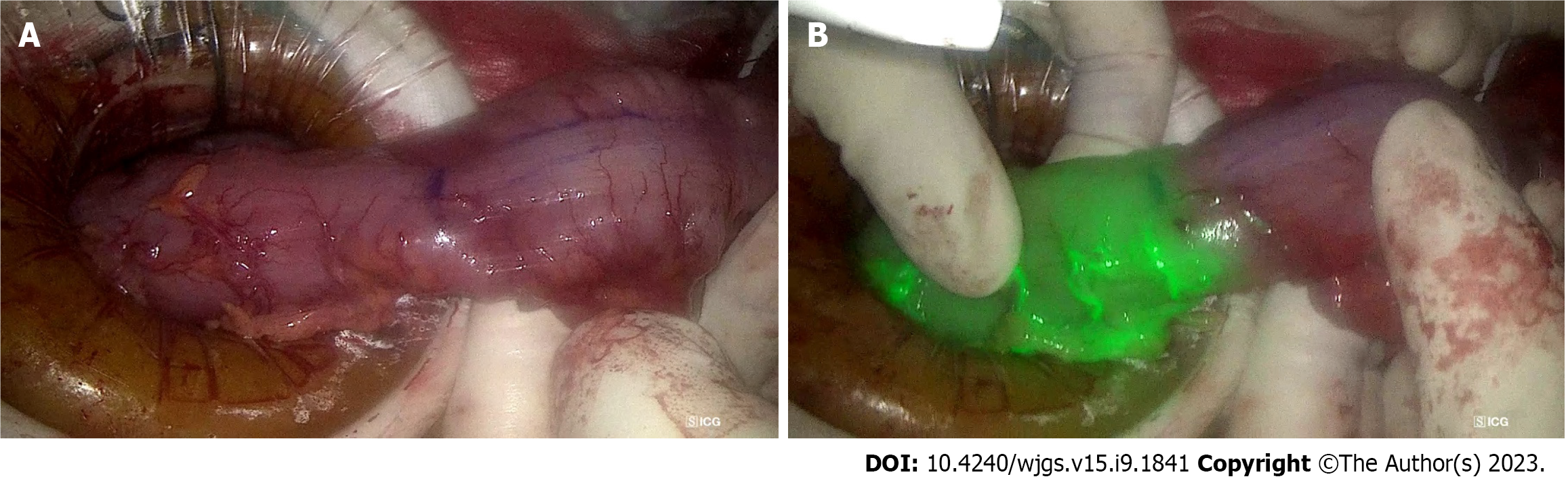
Assessment of bowel perfusion at site of intended anastomosis: ALs are a known complication of colorectal surgery with incidence between 3%-19%[91]. This is associated with increased morbidity and mortality, prolonged hospital stay, and a potential association with an increased risk of cancer recurrence, translating to worse long-term outcomes[92,93]. Bowel vascularity is a modifiable risk factor for anastomotic healing, hence the utility of ICG fluorescence angiography for intraoperative confirmation of favourable bowel perfusion prior to anastomosis. A retrospective matched-pairs analysis has demonstrated that ICG angiography suggested a change of proximal colonic resection line location in 16.4% and significantly reduced AL rates by 4%[94]. A recent meta-analysis of 4037 patients comparing AL rates between colorectal surgery with and without ICG showed that ICG angiography significantly reduced the AL rate by 4%, which translated to a reduced risk of reoperation and 5.6% reduction in overall complications[95]. This is confirmed by a larger meta-analysis of 25 studies with 7735 patients by Trastulli et al[96], which found that ICG angiography led to a reduction in AL rate compared to standard methods of anastomosis perfusion assessment (OR = 0.39, 95%CI: 0.31-0.49, P < 0.001). The NNT for ICG to prevent 1 additional AL is 23 patients. Figure 5 illustrates the use of ICG to confirm well vascularised bowel at the site of intended bowel transection and subsequent anastomosis.
Some limitations include the qualitative nature of the assessment for ICG fluorescence in the bowel which can be subjective, with no standard on dose of ICG and observation time. Research has hence been conducted on the quantitative analysis of colonic perfusion, with an evaluation of fluorescence intensity and perfusion time factors. A Korean study has determined that factors related to perfusion time, such as time from first fluorescence increase to maximum fluorescence, are significant predictors of anastomotic complications[97]. At present there is no consensus on the routine use of ICG for assessment of anastomotic perfusion in colorectal surgery. In spite of this, a recent cost analysis by Liu et al[98] on routine ICG use for anastomotic perfusion assessment found it cost-effective.
Perfusion assessment of other structures: Perfusion assessment using ICG has also been performed for pedicled omentoplasty in pelvic surgery, gracilis muscle flaps and anal advancement flaps for perianal fistula[99]. In a study assessing the role of ICG dye in pedicled opemtoplasties, 80% (12/15) of patients had a larger resection than intended as ICG was able to identify areas of malperfused omentum that was not visible under standard white light. While this added an extra median of 8 min (range 3-39 min) to the surgical time, it can be argued that this is a worthwhile limitation[100].
Tumour localisation: Preoperative endoscopic tattooing of colonic lesions using India ink was first described in 1975 by Ponsky and King[101] for the purposes of intraoperative localisation. This is necessary in the setting of minimally invasive surgery in view of the inability to palpate the colorectum intraoperatively to allow identification of lesions. ICG tumour marking has been employed to allow precise intraoperative identification of small lesions without affecting the visibility of the surgical field and tissue planes with colour dye while in conventional viewing mode. The preferred interval between endoscopic submucosal injection of ICG and surgery varies. Lee et al[102] endoscopically injected 1-1.5 mL of ICG preoperatively and found that tattoos placed within 2 d of surgery were more often visualised (95%) than if they were placed earlier (40%). In contrast, a Japanese study injecting 0.5 mg of ICG submucosally described 100% intraoperative detection rates within 6 d and significant decrease after 7 d[103]. Furthermore, a prospective case series by Orsi et al[104] on 10 patients who underwent robotic colorectal resections also demonstrated the utility of ICG as a preoperative tumour marking dye for robotic surgeries.
Lymphatic mapping: ICG can further be used for LN mapping in colorectal cancer (CRC) patients, similar to that for other gastrointestinal malignancies. ICG spreads through lymphatic drainage from distal perivascular space with slow interstitial fluid reabsorption when ICG is injected into the colonic wall[88]. Concentration and dosing of ICG utilised in the literature varies, with injections performed either subserosal laparoscopically or submucosal endoscopically[105]. In patients with CRC, ICG is useful for two purposes. Firstly, ICG dye injection guides lymphatic mapping to facilitate harvesting of the draining LNs for oncological resection during colorectal resection. Secondly, ICG dye injection helps identify the SLN and provide information to surgeons for resection and is an area of ongoing research initiatives.
A systematic review of 12 studies found the rate of SLN accuracy in T1 CRC to be between 89%-100% when various dyes are used, including ICG and patent blue[106]. However, there is no consensus on the applicability of SLN identification in colorectal cancer. Current practice of complete mesocolic excision and total mesorectal excision ensures enbloc lymphovascular clearance. The role of lymphatic mapping in colorectal cancer could potentially be in early tumour stages to allow for conservative surgical resections but more research is required in this aspect[107].
Lateral pelvic LN dissection: Lateral pelvic LN dissection (LPLD) is recommended for patients diagnosed with mid-to-low advanced rectal cancer, due to the estimated 11%-22% incidence of lateral pelvic LN metastases (LPNM) in patients with T3/4 rectal cancer[108]. LPNM is an important factor for local recurrence, and is treated as a systemic disease due to common occurrence of distant metastasis[109,110]. Zhou et al[109] evaluated the use of ICG FI for LPLD, and found significantly reduced blood loss and a greater number of LNs harvested, but no difference in operative time nor postoperative complications. In another longer-term propensity score-matched cohort study, Watanabe et al[111] reported decreased 3-year cumulative lateral local recurrence rate in the ICG-FI group. In addition, Yasui et al[112] and Noura et al[113] proposed the use of ICG FI to identify SLNs in patients without suspected LPNM. However, further prospective studies are required in this regard.
Ureteral visualization: Ureteral injuries, while rare with an incidence of around 0.28% of colorectal surgeries, are associated with increased mortality, morbidity, length of stay, and healthcare costs[114]. Intraureteral ICG administration has been used for intraoperative ureteral identification to reduce iatrogenic injuries, and also allows for the early identification of any ureteral injury for immediate repair. Administration requires cystoscopy and ureteral catheterisation, and allows for 4 to 12 h of ureteral visualisation[115]. Most studies used 5 mL of 2.5 mg/mL ICG for each ureter. A systematic review of 7 retrospective studies found this safe and effective, although the risks of ureteral catheterisation include ureteral injury itself and infectious complications[116,117].
Urethral identification: Urethral injury is a dreaded complication in transanal total mesorectal excision and abdominoperineal resection, and is increasing in incidence with more minimally invasive transanal surgery being performed[118]. Studies have demonstrated successful visualisation of the urethra with ICG mixed with Instillagel® and ICG-silicon coated Foley catheters, albeit in cadavers[99].
Identification of nerves: The pelvic autonomic nerves are crucial for regulation of anorectal and urogenital function, but may be damaged during colorectal surgery. A pilot study by Jin et al[119] demonstrated that intravenous administration of 5 mg/kg ICG 24 h preoperatively allowed for the visualisation of the splanchnic, inferior mesenteric artery and sacral plexus during laparoscopic colorectal resection. This technique still requires further research, but could potentially aid in identification and protection of the pelvic autonomic nerves during laparoscopic colorectal resections.
Peritoneal metastases occur in up to 30% of colorectal cancer patients (metachronous more than synchronous), and 75% of ovarian cancer patients present with peritoneal disease on diagnosis[120,121]. Conventional imaging modalities such as CT and magnetic resonance imaging have poor sensitivity in detecting small peritoneal nodules, requiring surgical exploration or cytological examination of peritoneal washings for complete evaluation of the peritoneal cavity[122,123]. However, small nodules may remain undetected during the surgeon’s visual and tactile assessment. In the context of a diagnostic exploration, this can impact staging and management. In the therapeutic setting, this can affect the completeness of cytoreduction and subsequent long term outcomes. ICG offers a potential solution to this diagnostic challenge, with its theoretical ability to detect micro peritoneal implants using the EPR effect[124]. In a systematic review of 71 patients with 322 peritoneal nodules assessed, ICG demonstrated promising sensitivity and specificity in detecting nodules at 88.2% and 77.8%, respectively[125]. However, there are restrictions to its utility in mucinous colorectal carcinomas, which have poor affinity for ICG. There is a possible role for ICG fluorescence as an adjunct to improve detection of peritoneal metastases in colon and ovarian cancer, but more studies are warranted.
Wound healing post-amputation in patients with peripheral artery disease or chronic limb threatening ischaemia is often poor due to the poor vascular status and underlying comorbidities including diabetes mellitus or smoking[126]. ICG NIR FI post-amputation or post-revascularization is one proposed method for assessing regional tissue perfusion in predicting wound healing, determining level of amputation and to assess global limb perfusion. Van Den Hoven et al[127] performed a pilot study where ICG NIR FI was performed in 15 patients post-amputation, and noted that impaired wound healing corresponded to regions of low fluorescence in patients, and accurately predicted postoperative skin necrosis in 4 cases.
Bowel ischaemia is a known postoperative complication of abdominal aortic aneurysm (AAA) repair due to malperfusion of the peripheral arteries, with its associated mortality up to 50%[128,129]. ICG angiography provides visualization of peripheral intestinal blood flow, which can be used to determine whether there is sufficient vascular supply to perfuse the bowels. This information can help to guide decisions regarding whether the inferior mesenteric arteries (IMA) and internal iliac arteries (IIA) need to be reconstructed or preserved. In a study conducted by Yamamoto et al[129] involving 10 open AAA repairs, the use of ICG angiography resulted in at least 1 IMA or IIA being reconstructed in 8 cases that would not have been done otherwise. This approach helps to ensure that postoperative bowel ischemia, which would require a second surgery, is minimized.
Beyond the organs discussed above, ICG is also used in other abdominal organs beyond the purview of a gastrointestinal surgeon. For example, ICG has been used to define tumour margins from normal kidney, identify branches of the main renal artery in partial nephrectomies, and assess microperfusion to predict early graft function in kidney transplant patients[130-132]. In gynaecological surgery, similar applications were noted in identifying SLNs in endometrial, cervical and vulvar malignancies[133]. It also is used for ureteral identification and localizing endometriosis nodules[134].
ICG plays a crucial role in the field of gastrointestinal surgery, specifically in the optimization of oncological resections and comprehension of vascular supply. The key factors that contribute to successful cancer resections with low recurrence rates involve precise identification and localisation of the tumour, adequate resection of the tumour with ample margins, and complete removal of the lymphatics[33]. ICG serves as a useful tool in facilitating these steps, enhancing their efficiency and accuracy.
In oncological resections of various organs such as the oesophagus, stomach, hepatobiliary system, and the bowels, lymphatic mapping through ICG is widely employed. This method ensures the precise identification of SLNs and aids in determining the extent of LN dissection[135]. Literature also confirms that ICG can be used to identify tumours intraoperatively, specifically via the EPR effect. This helps to assure surgeons that they have resected sufficient tissue to prevent positive margins that may mandate a second operation. This, in turn, enables surgeons to operate with greater confidence that the cancer has been adequately removed, while simultaneously reducing the need for more extensive surgeries when they are not necessary.
ICG also provides surgeons with a better understanding of vascular supply, thereby preventing intraoperative accidental injuries, especially in cases where vessels are difficult to visualize or have aberrant anatomy[135]. Additionally, it facilitates complete vessel anastomoses to prevent leaks. Furthermore, ICG aids in ensuring sufficient perfusion of organs following resections, thereby decreasing the risk of postoperative ischemia. In summary, ICG provides surgeons with valuable insights into the vessels involved in surgery, which significantly reduces surgical morbidity, leading to shorter postoperative complications and ICU stays.
Given these applications of ICG in gastrointestinal surgery, it is only natural that ICG FI is primarily used in minimally invasive surgery or robotic surgery. ICG enables the mitigation of traditional drawbacks such as the lack of tactile feedback and subjective judgment error for tissue perfusion and viability. It remains used in open surgery still in more oncological contexts, such as SLN mapping.
ICG has a myriad of clinical applications and many emerging applications. Despite this, the accessibility, availability, affordability, and adoption remain an unmet need that needs to be met by collaborative initiatives of the medico-industrial complex. To begin with, standardized evidence base guidelines need to be developed, disseminated, and implemented for safe adoption in routine clinical practice.
Optimising ICG: Patient factors, dye factors, equipment, and method of assessing fluorescence intensity are factors that implicate and affect the utility of ICG. Patient factors include obesity and inflammation. Eriksson et al[136] showed a decreased rate of successful SLN mapping with increased patient body mass index.
Dye factors include the dose and concentration, timing, and route of administration, and increasingly also whether the dye is mixed with any other substances. For the purpose of SLN identification, prolonged accumulation of ICG in the sentinel nodes is crucial. By complexing ICG with HSA in the optimal molar composition, a higher fluorescence can be obtained to aid in this[137].
In addition, other dyes such as ZW-800 and VM678, among many others, have been tested in animal studies, with results showing better pharmacokinetic properties and target-to-background ratio. However, cost remains a barrier for these dyes[138]. ICG coating of the tubes and stents can be made possible with potential future clinical application in surgery. For example, ICG-coated ureteral stents can be useful in colorectal, gynecological, and urological procedures.
Fundamentally, there remains no widely accepted protocols for the use of ICG in most applications, with decisions such as dosing regimens left up to the surgeons’ expertise. Further research and study should focus on this area to optimise protocols to ensure the successful use of ICG.
Targeted contrast agents: It would also be useful to look beyond ICG, and develop new contrast agents that better target unique pathologies. This can be done via identifying antibodies or ligands for proteins and receptors on cancer cell surfaces, and substrates for cancer specific metabolic pathways. A large proportion of these dyes are ICG-based, as they can be incorporated into hardware that are already in operative rooms. Other cyanine based dyes can also be incorporated with minor modifications in these machinery[139].
There are already several tumour specific dyes produced clinically. LUM015 is a cyanine based dye that targets cathepsin, which is a protease secreted by cancer cells at a higher level than healthy cells. LUM015 targets breast cancer and sarcomas specifically and is not affected by breast density, as compared to ICG, making it more accurate[140].
Studies have also shown that ICG-like fluorescent dyes can be tagged to artificially created antibodies of cell-surface tumour markers. Promising antibodies have been developed for carcinoembryonic antigen (CEA) for colorectal, breast, lung, and gastric cancer, prostate-specific antigen for prostate cancer, and cancer antigen 125 for ovarian cancer[139]. For example, XenoLight CF750 is an anti-CEA antibody conjugated to ICG and NIR probe. It was able to detect peritoneal tumour deposits in all 4 gastric cancer cell lines, including micrometastases < 2 mm in mouse models[141].
The ability to target cancers specifically allows for better cancer detection and surgical margins, and hence this is an area of research that shows great promise. Regardless, further research should be conducted for all applications of ICG to confirm the improvement in outcomes.
ICG has wide clinical utility to enhance safety and accuracy of gastrointestinal surgery to improve patient outcomes, both in surgical oncology and in general. With the ongoing advancements in technology and research, the future of FI remains promising and will continue to revolutionize surgery. However, ICG should not be considered as a panacea to guide surgical conduct, and surgeons need to exercise own’s informed judgment based on individual skills, experience and training.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bains L, India; Komatsu S, Japan S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
| 1. | Lu CH, Hsiao JK. Indocyanine green: An old drug with novel applications. Tzu Chi Med J. 2021;33:317-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Reinhart MB, Huntington CR, Blair LJ, Heniford BT, Augenstein VA. Indocyanine Green: Historical Context, Current Applications, and Future Considerations. Surg Innov. 2016;23:166-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 331] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 3. | Kraft JC, Ho RJ. Interactions of indocyanine green and lipid in enhancing near-infrared fluorescence properties: the basis for near-infrared imaging in vivo. Biochemistry. 2014;53:1275-1283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 126] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 4. | Lund-Johansen P. The dye dilution method for measurement of cardiac output. Eur Heart J. 1990;11 Suppl I:6-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Destro M, Puliafito CA. Indocyanine green videoangiography of choroidal neovascularization. Ophthalmology. 1989;96:846-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 119] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Peltrini R, Podda M, Castiglioni S, Di Nuzzo MM, D'Ambra M, Lionetti R, Sodo M, Luglio G, Mucilli F, Di Saverio S, Bracale U, Corcione F. Intraoperative use of indocyanine green fluorescence imaging in rectal cancer surgery: The state of the art. World J Gastroenterol. 2021;27:6374-6386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 7. | Short MW, Burgers KG, Fry VT. Esophageal Cancer. Am Fam Physician. 2017;95:22-28. [PubMed] |
| 8. | Chen QY, Xie JW, Zhong Q, Wang JB, Lin JX, Lu J, Cao LL, Lin M, Tu RH, Huang ZN, Lin JL, Zheng HL, Li P, Zheng CH, Huang CM. Safety and Efficacy of Indocyanine Green Tracer-Guided Lymph Node Dissection During Laparoscopic Radical Gastrectomy in Patients With Gastric Cancer: A Randomized Clinical Trial. JAMA Surg. 2020;155:300-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 212] [Article Influence: 42.4] [Reference Citation Analysis (1)] |
| 9. | National Comprehensive Cancer Network. Guidelines Detail – NCCN Guidelines. [cited 21 Apr 2023]. Available from: https://www.nccn.org/guidelines/guidelines-detail. |
| 10. | Hachey KJ, Gilmore DM, Armstrong KW, Harris SE, Hornick JL, Colson YL, Wee JO. Safety and feasibility of near-infrared image-guided lymphatic mapping of regional lymph nodes in esophageal cancer. J Thorac Cardiovasc Surg. 2016;152:546-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | den Toom IJ, Mahieu R, van Rooij R, van Es RJJ, Hobbelink MGG, Krijger GC, Tijink BM, de Keizer B, de Bree R. Sentinel lymph node detection in oral cancer: a within-patient comparison between [(99m)Tc]Tc-tilmanocept and [(99m)Tc]Tc-nanocolloid. Eur J Nucl Med Mol Imaging. 2021;48:851-858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Yuasa Y, Seike J, Yoshida T, Takechi H, Yamai H, Yamamoto Y, Furukita Y, Goto M, Minato T, Nishino T, Inoue S, Fujiwara S, Tangoku A. Sentinel lymph node biopsy using intraoperative indocyanine green fluorescence imaging navigated with preoperative CT lymphography for superficial esophageal cancer. Ann Surg Oncol. 2012;19:486-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Ohnishi S, Lomnes SJ, Laurence RG, Gogbashian A, Mariani G, Frangioni JV. Organic alternatives to quantum dots for intraoperative near-infrared fluorescent sentinel lymph node mapping. Mol Imaging. 2005;4:172-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 138] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 14. | Wall KP, Dillon R, Knowles MK. Fluorescence quantum yield measurements of fluorescent proteins: a laboratory experiment for a biochemistry or molecular biophysics laboratory course. Biochem Mol Biol Educ. 2015;43:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Kim HK, Quan YH, Oh Y, Park JY, Park JH, Choi Y, Lee YS, Jeong JM, Choi YH, Kim BM. Macrophage-Targeted Indocyanine Green-Neomannosyl Human Serum Albumin for Intraoperative Sentinel Lymph Node Mapping in Porcine Esophagus. Ann Thorac Surg. 2016;102:1149-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Schlottmann F, Patti MG. Esophageal Adenocarcinoma Lymphatic Drainage with ICG Fluorescence Imaging. J Gastrointest Surg. 2019;23:384-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Chandler P, Wiesel O, Sherwinter DA. Fluorescence-guided surgery of the esophagus. Ann Transl Med. 2021;9:908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Fabbi M, Hagens ERC, van Berge Henegouwen MI, Gisbertz SS. Anastomotic leakage after esophagectomy for esophageal cancer: definitions, diagnostics, and treatment. Dis Esophagus. 2021;34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 79] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 19. | Noma K, Shirakawa Y, Kanaya N, Okada T, Maeda N, Ninomiya T, Tanabe S, Sakurama K, Fujiwara T. Visualized Evaluation of Blood Flow to the Gastric Conduit and Complications in Esophageal Reconstruction. J Am Coll Surg. 2018;226:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 20. | Kumagai Y, Hatano S, Sobajima J, Ishiguro T, Fukuchi M, Ishibashi KI, Mochiki E, Nakajima Y, Ishida H. Indocyanine green fluorescence angiography of the reconstructed gastric tube during esophagectomy: efficacy of the 90-second rule. Dis Esophagus. 2018;31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 21. | Slooter MD, Eshuis WJ, Cuesta MA, Gisbertz SS, van Berge Henegouwen MI. Fluorescent imaging using indocyanine green during esophagectomy to prevent surgical morbidity: a systematic review and meta-analysis. J Thorac Dis. 2019;11:S755-S765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 22. | Yang YH, Park SY, Kim DJ. Chyle Leakage after Esophageal Cancer Surgery. Korean J Thorac Cardiovasc Surg. 2020;53:191-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Kamiya K, Unno N, Konno H. Intraoperative indocyanine green fluorescence lymphography, a novel imaging technique to detect a chyle fistula after an esophagectomy: report of a case. Surg Today. 2009;39:421-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Kaburagi T, Takeuchi H, Oyama T, Nakamura R, Takahashi T, Wada N, Saikawa Y, Kamiya S, Tanaka M, Wada T, Kitagawa Y. Intraoperative fluorescence lymphography using indocyanine green in a patient with chylothorax after esophagectomy: report of a case. Surg Today. 2013;43:206-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Das J, Thambudorai R, Ray S. Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. Indian J Nucl Med. 2015;30:177-179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Cianchi F, Indennitate G, Paoli B, Ortolani M, Lami G, Manetti N, Tarantino O, Messeri S, Foppa C, Badii B, Novelli L, Skalamera I, Nelli T, Coratti F, Perigli G, Staderini F. The Clinical Value of Fluorescent Lymphography with Indocyanine Green During Robotic Surgery for Gastric Cancer: a Matched Cohort Study. J Gastrointest Surg. 2020;24:2197-2203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 27. | Lombardi PM, Mazzola M, Nicastro V, Giacopuzzi S, Baiocchi GL, Castoro C, Rosati R, Fumagalli Romario U, Bonavina L, Staderini F, Gockel I, Gregori D, De Martini P, Gualtierotti M, Danieli M, Beretta S, Mutignani M, Forti E, Ferrari G. The iGreenGO Study: The Clinical Role of Indocyanine Green Imaging Fluorescence in Modifying the Surgeon's Conduct During the Surgical Treatment of Advanced Gastric Cancer-Study Protocol for an International Multicenter Prospective Study. Front Oncol. 2022;12:854754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Kitagawa Y, Takeuchi H, Takagi Y, Natsugoe S, Terashima M, Murakami N, Fujimura T, Tsujimoto H, Hayashi H, Yoshimizu N, Takagane A, Mohri Y, Nabeshima K, Uenosono Y, Kinami S, Sakamoto J, Morita S, Aikou T, Miwa K, Kitajima M. Sentinel node mapping for gastric cancer: a prospective multicenter trial in Japan. J Clin Oncol. 2013;31:3704-3710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 231] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 29. | Cho M, Kim KY, Park SH, Kim YM, Kim HI, Hyung WJ. Securing Resection Margin Using Indocyanine Green Diffusion Range on Gastric Wall during NIR Fluorescence-Guided Surgery in Early Gastric Cancer Patients. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 30. | Kalmar CL, Reed CM, Peery CL, Salzberg AD. Intraluminal indocyanine green for intraoperative staple line leak testing in bariatric surgery. Surg Endosc. 2020;34:4194-4199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Hagen ME, Diaper J, Douissard J, Jung MK, Buehler L, Aldenkortt F, Barcelos GK, Morel P. Early Experience with Intraoperative Leak Test Using a Blend of Methylene Blue and Indocyanine Green During Robotic Gastric Bypass Surgery. Obes Surg. 2019;29:949-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Sánchez-Pernaute A, López-Antoñanzas L, Torres AJ, Dziakova J, Rubio MA, Pérez-Aguirre E. Avoiding Complications During Revisional Bariatric Surgery with Indocyanine Green Fluorescence Imaging. Obes Surg. 2023;33:972-974. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 33. | Schrembs D, Rosenberg R. [Principles of modern oncologic surgery]. Ther Umsch. 2019;76:199-207. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 34. | Rossi G, Tarasconi A, Baiocchi G, De' Angelis GL, Gaiani F, Di Mario F, Catena F, Dalla Valle R. Fluorescence guided surgery in liver tumors: applications and advantages. Acta Biomed. 2018;89:135-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 35. | Franz M, Arend J, Wolff S, Perrakis A, Rahimli M, Negrini VR, Stockheim J, Lorenz E, Croner R. Tumor visualization and fluorescence angiography with indocyanine green (ICG) in laparoscopic and robotic hepatobiliary surgery - valuation of early adopters from Germany. Innov Surg Sci. 2021;6:59-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 36. | Mehdorn AS, Richter F, Hess K, Beckmann JH, Egberts JH, Linecker M, Becker T, Braun F. The Role of ICG in Robot-Assisted Liver Resections. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Schwarz C, Plass I, Fitschek F, Punzengruber A, Mittlböck M, Kampf S, Asenbaum U, Starlinger P, Stremitzer S, Bodingbauer M, Kaczirek K. The value of indocyanine green clearance assessment to predict postoperative liver dysfunction in patients undergoing liver resection. Sci Rep. 2019;9:8421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 38. | Sheriff S, Madhavan S, Lei GY, Chan YH, Junnarkar SP, Huey CW, Low JK, Shelat VG. Predictors of mortality within the first year post-hepatectomy for hepatocellular carcinoma. J Egypt Natl Canc Inst. 2022;34:14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 39. | Li M, Wang J, Song J, Shen F, Song L, Ni X, Suo T, Liu H, Zhong M. Preoperative ICG Test to Predict Posthepatectomy Liver Failure and Postoperative Outcomes in Hilar Cholangiocarcinoma. Biomed Res Int. 2021;2021:8298737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Pind ML, Bendtsen F, Kallemose T, Møller S. Indocyanine green retention test (ICG-r15) as a noninvasive predictor of portal hypertension in patients with different severity of cirrhosis. Eur J Gastroenterol Hepatol. 2016;28:948-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 41. | Chan KS, Shelat VG, Low HM, Low JK. Is the extent of functional liver remnant increase truly "functional"? A single-institution case series of patients with Associating Liver Partition and Portal vein ligation for Staged hepatectomy (ALPPS). Clin Exp Hepatol. 2023;9:28-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Une N, Fujio A, Mitsugashira H, Kanai N, Saitoh Y, Ohta M, Sasaki K, Miyazawa K, Kashiwadate T, Nakanishi W, Tokodai K, Miyagi S, Unno M, Kamei T. Laparoscopic liver cyst fenestration with real-time indocyanine green fluorescence-guided surgery: a case report. J Surg Case Rep. 2021;2021:rjab196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Hanaki T, Yagyu T, Uchinaka E, Morimoto M, Watanabe J, Tokuyasu N, Takano S, Sakamoto T, Honjo S, Fujiwara Y. Avoidance of bile duct injury during laparoscopic liver cyst fenestration using indocyanine green: A case report. Clin Case Rep. 2020;8:1419-1424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 44. | Umemura A, Nitta H, Suto T, Fujiwara H, Takahara T, Hasegawa Y, Katagiri H, Kanno S, Ando T, Sasaki A. Indocyanine green fluorescence imaging via endoscopic nasal biliary drainage during laparoscopic deroofing of liver cysts. J Minim Access Surg. 2021;17:131-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 45. | Graves C, Ely S, Idowu O, Newton C, Kim S. Direct Gallbladder Indocyanine Green Injection Fluorescence Cholangiography During Laparoscopic Cholecystectomy. J Laparoendosc Adv Surg Tech A. 2017;27:1069-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 46. | Chan KS, Hwang E, Low JK, Junnarkar SP, Huey CWT, Shelat VG. On-table hepatopancreatobiliary surgical consults for difficult cholecystectomies: A 7-year audit. Hepatobiliary Pancreat Dis Int. 2022;21:273-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 47. | Koo JGA, Chan YH, Shelat VG. Laparoscopic subtotal cholecystectomy: comparison of reconstituting and fenestrating techniques. Surg Endosc. 2021;35:1014-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 48. | Polom W, Markuszewski M, Rho YS, Matuszewski M. Usage of invisible near infrared light (NIR) fluorescence with indocyanine green (ICG) and methylene blue (MB) in urological oncology. Part 1. Cent European J Urol. 2014;67:142-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | Yong CC, Yin SM, Sng YP, Chen CL. Prevent bile duct injury by indocyanine green guide fluorescent imaging during laparoscopic cholecystectomy in liver transplantation recipient. Hepatobiliary Surg Nutr. 2020;9:817-819. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 50. | Lim SH, Tan HTA, Shelat VG. Comparison of indocyanine green dye fluorescent cholangiography with intra-operative cholangiography in laparoscopic cholecystectomy: a meta-analysis. Surg Endosc. 2021;35:1511-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 51. | Bandari M, Pai MV, Acharya A, Augustine AJ, Murlimanju BV. Anatomical mapping of the biliary tree during laparoscopic cholecystectomy by using indocyanine green dye. J Minim Access Surg. 2022;18:218-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 52. | Ambe PC, Plambeck J, Fernandez-Jesberg V, Zarras K. The role of indocyanine green fluoroscopy for intraoperative bile duct visualization during laparoscopic cholecystectomy: an observational cohort study in 70 patients. Patient Saf Surg. 2019;13:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 53. | Shibata H, Aoki T, Koizumi T, Kusano T, Yamazaki T, Saito K, Hirai T, Tomioka K, Wada Y, Hakozaki T, Tashiro Y, Nogaki K, Yamada K, Matsuda K, Fujimori A, Enami Y, Murakami M. The Efficacy of Intraoperative Fluorescent Imaging Using Indocyanine Green for Cholangiography During Cholecystectomy and Hepatectomy. Clin Exp Gastroenterol. 2021;14:145-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 54. | Esposito C, Alberti D, Settimi A, Pecorelli S, Boroni G, Montanaro B, Escolino M. Indocyanine green (ICG) fluorescent cholangiography during laparoscopic cholecystectomy using RUBINA™ technology: preliminary experience in two pediatric surgery centers. Surg Endosc. 2021;35:6366-6373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 55. | Rakić M, Patrlj L, Kopljar M, Kliček R, Kolovrat M, Loncar B, Busic Z. Gallbladder cancer. Hepatobiliary Surg Nutr. 2014;3:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 99] [Reference Citation Analysis (0)] |
| 56. | Ahmad A. Use of indocyanine green (ICG) augmented near-infrared fluorescence imaging in robotic radical resection of gallbladder adenocarcinomas. Surg Endosc. 2020;34:2490-2494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 57. | Papageorge MV, de Geus SWL, Woods AP, Ng SC, Drake FT, Merrill A, Cassidy MR, McAneny D, Tseng JF, Sachs TE. Lymphadenectomy in gallbladder adenocarcinoma: Are we doing enough? Am J Surg. 2022;224:423-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | Anselmo A, Siragusa L, Materazzo M, Sforza D, Bacchiocchi G, Sensi B, Tisone G. ASO Author Reflections: Can Indocyanine Green Increase the Safety of Bile Duct Dissection and Thus Improve Regional Lymphadenectomy in Re-Do Surgery for Incidental Gallbladder Cancer? Ann Surg Oncol. 2022;29:5554. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 59. | Luján J, Almeida A, López-Olaondo L, Rotellar F. Laparoscopic radical hepatectomy and lymphadenectomy for incidental gallbladder cancer. Surgical technique with ICG fluorescence enhancement. Surg Oncol. 2022;42:101756. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 60. | Onishi S, Yamada K, Murakami M, Kedoin C, Muto M, Ieiri S. Co-injection of Bile and Indocyanine Green for Detecting Pancreaticobiliary Maljunction of Choledochal Cyst. European J Pediatr Surg Rep. 2022;10:e127-e130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 61. | Gijsen A, Vries RD, Liem M, Lips D. The Use of Indocyanine Green Fluorescence Imaging in Preventing Postoperative Bile Leakage of the Hepaticojejunostomy in Robot-assisted Pancreatic Surgery. HPB. 2022;24:S368-S369. [DOI] [Full Text] |
| 62. | Hutteman M, van der Vorst JR, Mieog JS, Bonsing BA, Hartgrink HH, Kuppen PJ, Löwik CW, Frangioni JV, van de Velde CJ, Vahrmeijer AL. Near-infrared fluorescence imaging in patients undergoing pancreaticoduodenectomy. Eur Surg Res. 2011;47:90-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 63. | Griffin JF, Smalley SR, Jewell W, Paradelo JC, Reymond RD, Hassanein RE, Evans RG. Patterns of failure after curative resection of pancreatic carcinoma. Cancer. 1990;66:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 64. | Lee SB, Hassan M, Fisher R, Chertov O, Chernomordik V, Kramer-Marek G, Gandjbakhche A, Capala J. Affibody molecules for in vivo characterization of HER2-positive tumors by near-infrared imaging. Clin Cancer Res. 2008;14:3840-3849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 135] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 65. | Jiang T, Olson ES, Nguyen QT, Roy M, Jennings PA, Tsien RY. Tumor imaging by means of proteolytic activation of cell-penetrating peptides. Proc Natl Acad Sci U S A. 2004;101:17867-17872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 641] [Cited by in RCA: 651] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 66. | Zhou H, Luby-Phelps K, Mickey BE, Habib AA, Mason RP, Zhao D. Dynamic near-infrared optical imaging of 2-deoxyglucose uptake by intracranial glioma of athymic mice. PLoS One. 2009;4:e8051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 67. | Intes X, Ripoll J, Chen Y, Nioka S, Yodh AG, Chance B. In vivo continuous-wave optical breast imaging enhanced with Indocyanine Green. Med Phys. 2003;30:1039-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 157] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 68. | Paiella S, De Pastena M, Landoni L, Esposito A, Casetti L, Miotto M, Ramera M, Salvia R, Secchettin E, Bonamini D, Manzini G, D'Onofrio M, Marchegiani G, Bassi C. Is there a role for near-infrared technology in laparoscopic resection of pancreatic neuroendocrine tumors? Results of the COLPAN "colour-and-resect the pancreas" study. Surg Endosc. 2017;31:4478-4484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 69. | Sperti C, Polizzi ML, Moro M, Beltrame V, Pedrazzoli S. Middle-preserving pancreatectomy: an interesting procedure for pancreas-sparing resection. JOP. 2010;11:258-261. [PubMed] |
| 70. | Ohzato H, Yamamoto T, Fukunaga M, Imamura H, Furukawa H. Middle-preserving pancreatectomy for multifocal metastatic renal cell carcinoma located in the head, body and tail of the pancreas. A case report. JOP. 2010;11:633-637. [PubMed] |
| 71. | Hide T, Yano S, Shinojima N, Kuratsu J. Usefulness of the indocyanine green fluorescence endoscope in endonasal transsphenoidal surgery. J Neurosurg. 2015;122:1185-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 72. | Iguchi T, Iseda N, Hirose K, Ninomiya M, Honboh T, Maeda T, Sawada F, Tachibana YI, Akashi T, Sekiguchi N, Sadanaga N, Matsuura H. Indocyanine green fluorescence to ensure perfusion in middle segment-preserving pancreatectomy: a case report. Surg Case Rep. 2021;7:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 73. | Palomba G, Dinuzzi VP, Pegoraro F, Troisi RI, Montalti R, De Palma GD, Aprea G. The Role of Intraoperative Indocyanine Green (ICG) and Preoperative 3-Dimensional (3D) Reconstruction in Laparoscopic Adrenalectomy: A Propensity Score-matched Analysis. Surg Laparosc Endosc Percutan Tech. 2022;32:643-649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 74. | Moore EC, Berber E. Fluorescence techniques in adrenal surgery. Gland Surg. 2019;8:S22-S27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 75. | Colvin J, Zaidi N, Berber E. The utility of indocyanine green fluorescence imaging during robotic adrenalectomy. J Surg Oncol. 2016;114:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 76. | Kahramangil B, Kose E, Berber E. Characterization of fluorescence patterns exhibited by different adrenal tumors: Determining the indications for indocyanine green use in adrenalectomy. Surgery. 2018;164:972-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 77. | DeLong JC, Chakedis JM, Hosseini A, Kelly KJ, Horgan S, Bouvet M. Indocyanine green (ICG) fluorescence-guided laparoscopic adrenalectomy. J Surg Oncol. 2015;112:650-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 78. | Aloysius TMN, Shelat VG. Laparoscopic splenectomy for splenic rupture secondary to metastatic choriocarcinoma. Ann Hepatobiliary Pancreat Surg. 2018;22:79-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 79. | Bada-Bosch I, Mata DP, de la Torre M, Ordóñez J, Blanco MD, de Agustin J. Laparoscopic Partial Splenectomy Assisted by Fluorescence in a 13-Year-Old Girl. European J Pediatr Surg Rep. 2020;8:e81-e85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 80. | Chia C, Pandya GJ, Kamalesh A, Shelat VG. Splenic Artery Pseudoaneurysm Masquerading as a Pancreatic Cyst-A Diagnostic Challenge. Int Surg. 2015;100:1069-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 81. | Bertolucci A, Tartaglia D, Cremonini C, Ginesini M, Cengeli I, Galatioto C, Coccolini F, Chiarugi M. Indocyanine Green (ICG) for the assessment of splenic perfusion during laparoscopic splenic artery aneurysmectomy. A case report. Ann Ital Chir. 2021;10. [PubMed] |
| 82. | Masuya R, Nakame K, Tahira K, Kai K, Hamada T, Yano K, Imamura N, Hiyoshi M, Nanashima A, Ieiri S. Laparoscopic dome resection for pediatric nonparasitic huge splenic cyst safely performed using indocyanine green fluorescence and percutaneous needle grasper. Asian J Endosc Surg. 2022;15:693-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 83. | Guerra F, Coletta D, Greco PA, Eugeni E, Patriti A. The use of indocyanine green fluorescence to define bowel microcirculation during laparoscopic surgery for acute small bowel obstruction. Colorectal Dis. 2021;23:2189-2194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 84. | Quah GS, Eslick GD, Cox MR. Laparoscopic versus open surgery for adhesional small bowel obstruction: a systematic review and meta-analysis of case-control studies. Surg Endosc. 2019;33:3209-3217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 85. | Ganguly A, Acharya A, Pai MV, Augustine AJ. Assessment of bowel vascularity using indocyanine green fluorescence in incarcerated hernia. Int Surg J. 2021;8:2834. [DOI] [Full Text] |
| 86. | Karampinis I, Keese M, Jakob J, Stasiunaitis V, Gerken A, Attenberger U, Post S, Kienle P, Nowak K. Indocyanine Green Tissue Angiography Can Reduce Extended Bowel Resections in Acute Mesenteric Ischemia. J Gastrointest Surg. 2018;22:2117-2124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 87. | Shih MC, Hagspiel KD. CTA and MRA in mesenteric ischemia: part 1, Role in diagnosis and differential diagnosis. AJR Am J Roentgenol. 2007;188:452-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 88. | Son GM, Ahn HM, Lee IY, Ha GW. Multifunctional Indocyanine Green Applications for Fluorescence-Guided Laparoscopic Colorectal Surgery. Ann Coloproctol. 2021;37:133-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 89. | Baiocchi GL, Guercioni G, Vettoretto N, Scabini S, Millo P, Muratore A, Clementi M, Sica G, Delrio P, Longo G, Anania G, Barbieri V, Amodio P, Di Marco C, Baldazzi G, Garulli G, Patriti A, Pirozzi F, De Luca R, Mancini S, Pedrazzani C, Scaramuzzi M, Scatizzi M, Taglietti L, Motter M, Ceccarelli G, Totis M, Gennai A, Frazzini D, Di Mauro G, Capolupo GT, Crafa F, Marini P, Ruffo G, Persiani R, Borghi F, de Manzini N, Catarci M. ICG fluorescence imaging in colorectal surgery: a snapshot from the ICRAL study group. BMC Surg. 2021;21:190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 90. | Belloni E, Muttillo EM, Di Saverio S, Gasparrini M, Brescia A, Nigri G. The Role of Indocyanine Green Fluorescence in Rectal Cancer Robotic Surgery: A Narrative Review. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 91. | Slieker JC, Daams F, Mulder IM, Jeekel J, Lange JF. Systematic review of the technique of colorectal anastomosis. JAMA Surg. 2013;148:190-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 119] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 92. | Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253:890-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 747] [Cited by in RCA: 679] [Article Influence: 48.5] [Reference Citation Analysis (0)] |
| 93. | Kverneng Hultberg D, Svensson J, Jutesten H, Rutegård J, Matthiessen P, Lydrup ML, Rutegård M. The Impact of Anastomotic Leakage on Long-term Function After Anterior Resection for Rectal Cancer. Dis Colon Rectum. 2020;63:619-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 94. | Kudszus S, Roesel C, Schachtrupp A, Höer JJ. Intraoperative laser fluorescence angiography in colorectal surgery: a noninvasive analysis to reduce the rate of anastomotic leakage. Langenbecks Arch Surg. 2010;395:1025-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 236] [Article Influence: 15.7] [Reference Citation Analysis (1)] |
| 95. | Liu D, Liang L, Liu L, Zhu Z. Does intraoperative indocyanine green fluorescence angiography decrease the incidence of anastomotic leakage in colorectal surgery? A systematic review and meta-analysis. Int J Colorectal Dis. 2021;36:57-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 96. | Trastulli S, Munzi G, Desiderio J, Cirocchi R, Rossi M, Parisi A. Indocyanine green fluorescence angiography versus standard intraoperative methods for prevention of anastomotic leak in colorectal surgery: meta-analysis. Br J Surg. 2021;108:359-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 97. | Son GM, Kwon MS, Kim Y, Kim J, Kim SH, Lee JW. Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc. 2019;33:1640-1649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 141] [Article Influence: 20.1] [Reference Citation Analysis (1)] |
| 98. | Liu RQ, Elnahas A, Tang E, Alkhamesi NA, Hawel J, Alnumay A, Schlachta CM. Cost analysis of indocyanine green fluorescence angiography for prevention of anastomotic leakage in colorectal surgery. Surg Endosc. 2022;36:9281-9287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 99. | Garoufalia Z, Wexner SD. Indocyanine Green Fluorescence Guided Surgery in Colorectal Surgery. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 29] [Reference Citation Analysis (1)] |
| 100. | Slooter MD, Blok RD, Wisselink DD, Buskens CJ, Bemelman WA, Tanis PJ, Hompes R. Near-infrared fluorescence angiography for intra-operative assessment of pedicled omentoplasty for filling of a pelvic cavity: a pilot study. Tech Coloproctol. 2019;23:723-728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 101. | Ponsky JL, King JF. Endoscopic marking of colonic lesions. Gastrointest Endosc. 1975;22:42-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 100] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 102. | Lee SJ, Sohn DK, Han KS, Kim BC, Hong CW, Park SC, Kim MJ, Park BK, Oh JH. Preoperative Tattooing Using Indocyanine Green in Laparoscopic Colorectal Surgery. Ann Coloproctol. 2018;34:206-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 103. | Satoyoshi T, Okita K, Ishii M, Hamabe A, Usui A, Akizuki E, Okuya K, Nishidate T, Yamano H, Nakase H, Takemasa I. Timing of indocyanine green injection prior to laparoscopic colorectal surgery for tumor localization: a prospective case series. Surg Endosc. 2021;35:763-769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 104. | Orsi AM, Dias SM, Moreira JE, Camilli JA. [Morphological development of the seminiferous epithelium of the pig at different ages (Sus scrofa of the Landrace strain)]. Anat Histol Embryol. 1987;16:97-102. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 105. | Emile SH, Elfeki H, Shalaby M, Sakr A, Sileri P, Laurberg S, Wexner SD. Sensitivity and specificity of indocyanine green near-infrared fluorescence imaging in detection of metastatic lymph nodes in colorectal cancer: Systematic review and meta-analysis. J Surg Oncol. 2017;116:730-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 106. | Di Berardino S, Capolupo GT, Caricato C, Caricato M. Sentinel lymph node mapping procedure in T1 colorectal cancer: A systematic review of published studies. Medicine (Baltimore). 2019;98:e16310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 107. | Carrara A, Motter M, Amabile D, Pellecchia L, Moscatelli P, Pertile R, Barbareschi M, Decarli NL, Ferrari M, Tirone G. Predictive value of the sentinel lymph node procedure in the staging of non-metastatic colorectal cancer. Int J Colorectal Dis. 2020;35:1921-1928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 108. | Kim MJ, Oh JH. Lateral Lymph Node Dissection With the Focus on Indications, Functional Outcomes, and Minimally Invasive Surgery. Ann Coloproctol. 2018;34:229-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 109. | Zhou SC, Tian YT, Wang XW, Zhao CD, Ma S, Jiang J, Li EN, Zhou HT, Liu Q, Liang JW, Zhou ZX, Wang XS. Application of indocyanine green-enhanced near-infrared fluorescence-guided imaging in laparoscopic lateral pelvic lymph node dissection for middle-low rectal cancer. World J Gastroenterol. 2019;25:4502-4511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 63] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 110. | Ogawa S, Itabashi M, Inoue Y, Ohki T, Bamba Y, Koshino K, Nakagawa R, Tani K, Aihara H, Kondo H, Yamaguchi S, Yamamoto M. Lateral pelvic lymph nodes for rectal cancer: A review of diagnosis and management. World J Gastrointest Oncol. 2021;13:1412-1424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 111. | Watanabe J, Ohya H, Sakai J, Suwa Y, Goto K, Nakagawa K, Ozawa M, Ishibe A, Suwa H, Kunisaki C, Endo I. Long-term outcomes of indocyanine green fluorescence imaging-guided laparoscopic lateral pelvic lymph node dissection for clinical stage II/III middle-lower rectal cancer: a propensity score-matched cohort study. Tech Coloproctol. 2023;27:759-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 21] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 112. | Yasui M, Ohue M, Noura S, Miyoshi N, Takahashi Y, Matsuda C, Nishimura J, Haraguchi N, Ushigome H, Nakai N, Fujino S, Sugimura K, Wada H, Takahashi H, Omori T, Miyata H. Exploratory analysis of lateral pelvic sentinel lymph node status for optimal management of laparoscopic lateral lymph node dissection in advanced lower rectal cancer without suspected lateral lymph node metastasis. BMC Cancer. 2021;21:911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 113. | Noura S, Ohue M, Seki Y, Yamamoto T, Idota A, Fujii J, Yamasaki T, Nakajima H, Murata K, Kameyama M, Yamada T, Miyashiro I, Ohigashi H, Yano M, Ishikawa O, Imaoka S. Evaluation of the lateral sentinel node by indocyanine green for rectal cancer based on micrometastasis determined by reverse transcriptase-polymerase chain reaction. Oncol Rep. 2008;20:745-750. [PubMed] |
| 114. | Halabi WJ, Jafari MD, Nguyen VQ, Carmichael JC, Mills S, Pigazzi A, Stamos MJ. Ureteral injuries in colorectal surgery: an analysis of trends, outcomes, and risk factors over a 10-year period in the United States. Dis Colon Rectum. 2014;57:179-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 100] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 115. | White LA, Joseph JP, Yang DY, Kelley SR, Mathis KL, Behm K, Viers BR. Intraureteral indocyanine green augments ureteral identification and avoidance during complex robotic-assisted colorectal surgery. Colorectal Dis. 2021;23:718-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 116. | Geskin AA, Westney OL, Graber WJ, Smith Iii TG, Chapin BF, Gregg JR. Complications Of Peri-Operative Ureteral Catheter Placement: Experience at A Major Cancer Center. Urology. 2022;164:88-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 117. | Rodríguez-Zentner H, Cukier M, Montagne V, Arrue E. Ureteral identification with indocyanine green in laparoscopic colorectal surgery. Asian J Endosc Surg. 2023;16:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 118. | Ferrara M, Kann BR. Urological Injuries during Colorectal Surgery. Clin Colon Rectal Surg. 2019;32:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 119. | Jin H, Zheng L, Lu L, Cui M. Near-infrared intraoperative imaging of pelvic autonomic nerves: a pilot study. Surg Endosc. 2022;36:2349-2356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 120. | Liberale G, Vankerckhove S, Caldon MG, Ahmed B, Moreau M, Nakadi IE, Larsimont D, Donckier V, Bourgeois P; Group R&D for the Clinical Application of Fluorescence Imaging of the Jules Bordetʼs Institute. Fluorescence Imaging After Indocyanine Green Injection for Detection of Peritoneal Metastases in Patients Undergoing Cytoreductive Surgery for Peritoneal Carcinomatosis From Colorectal Cancer: A Pilot Study. Ann Surg. 2016;264:1110-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 121. | Veys I, Pop FC, Vankerckhove S, Barbieux R, Chintinne M, Moreau M, Nogaret JM, Larsimont D, Donckier V, Bourgeois P, Liberale G; Group R&D for the Clinical Application of Fluorescence Imaging of the Jules Bordet Institute. ICG-fluorescence imaging for detection of peritoneal metastases and residual tumoral scars in locally advanced ovarian cancer: A pilot study. J Surg Oncol. 2018;117:228-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 122. | Low RN, Barone RM, Lucero J. Comparison of MRI and CT for predicting the Peritoneal Cancer Index (PCI) preoperatively in patients being considered for cytoreductive surgical procedures. Ann Surg Oncol. 2015;22:1708-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 123. | Ikoma N, Blum M, Chiang YJ, Estrella JS, Roy-Chowdhuri S, Fournier K, Mansfield P, Ajani JA, Badgwell BD. Yield of Staging Laparoscopy and Lavage Cytology for Radiologically Occult Peritoneal Carcinomatosis of Gastric Cancer. Ann Surg Oncol. 2016;23:4332-4337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 124. | Kobayashi H, Ogawa M, Alford R, Choyke PL, Urano Y. New strategies for fluorescent probe design in medical diagnostic imaging. Chem Rev. 2010;110:2620-2640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1878] [Cited by in RCA: 1572] [Article Influence: 104.8] [Reference Citation Analysis (0)] |
| 125. | Baiocchi GL, Gheza F, Molfino S, Arru L, Vaira M, Giacopuzzi S. Indocyanine green fluorescence-guided intraoperative detection of peritoneal carcinomatosis: systematic review. BMC Surg. 2020;20:158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 126. | Eneroth M. Factors affecting wound healing after major amputation for vascular disease: a review. Prosthet Orthot Int. 1999;23:195-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 127. | Van Den Hoven P, Van Den Berg SD, Van Der Valk JP, Van Der Krogt H, Van Doorn LP, Van De Bogt KEA, Van Schaik J, Schepers A, Vahrmeijer AL, Hamming JF, Van Der Vorst JR. Assessment of Tissue Viability Following Amputation Surgery Using Near-Infrared Fluorescence Imaging With Indocyanine Green. Ann Vasc Surg. 2022;78:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 128. | Ultee KH, Zettervall SL, Soden PA, Darling J, Bertges DJ, Verhagen HJ, Schermerhorn ML; Vascular Study Group of New England. Incidence of and risk factors for bowel ischemia after abdominal aortic aneurysm repair. J Vasc Surg. 2016;64:1384-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 129. | Yamamoto M, Orihashi K, Nishimori H, Wariishi S, Fukutomi T, Kondo N, Kihara K, Sato T, Sasaguri S. Indocyanine green angiography for intra-operative assessment in vascular surgery. Eur J Vasc Endovasc Surg. 2012;43:426-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 130. | Mitsui Y, Shiina H, Arichi N, Hiraoka T, Inoue S, Sumura M, Honda S, Yasumoto H, Igawa M. Indocyanine green (ICG)-based fluorescence navigation system for discrimination of kidney cancer from normal parenchyma: application during partial nephrectomy. Int Urol Nephrol. 2012;44:753-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 131. | Gadus L, Kocarek J, Chmelik F, Matejkova M, Heracek J. Robotic Partial Nephrectomy with Indocyanine Green Fluorescence Navigation. Contrast Media Mol Imaging. 2020;2020:1287530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 132. | Gerken ALH, Nowak K, Meyer A, Weiss C, Krüger B, Nawroth N, Karampinis I, Heller K, Apel H, Reissfelder C, Schwenke K, Keese M, Lang W, Rother U. Quantitative Assessment of Intraoperative Laser Fluorescence Angiography With Indocyanine Green Predicts Early Graft Function After Kidney Transplantation. Ann Surg. 2022;276:391-397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 133. | Ferreira H, Smith AV, Wattiez A. Application of Indocyanine Green in Gynecology: Review of the Literature. Surg Technol Int. 2019;34:282-292. [PubMed] |
| 134. | Bar-Shavit Y, Jaillet L, Chauvet P, Canis M, Bourdel N. Use of indocyanine green in endometriosis surgery. Fertil Steril. 2018;109:1136-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 135. | Schaafsma BE, Mieog JS, Hutteman M, van der Vorst JR, Kuppen PJ, Löwik CW, Frangioni JV, van de Velde CJ, Vahrmeijer AL. The clinical use of indocyanine green as a near-infrared fluorescent contrast agent for image-guided oncologic surgery. J Surg Oncol. 2011;104:323-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 661] [Cited by in RCA: 614] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 136. | Eriksson AG, Montovano M, Beavis A, Soslow RA, Zhou Q, Abu-Rustum NR, Gardner GJ, Zivanovic O, Barakat RR, Brown CL, Levine DA, Sonoda Y, Leitao MM Jr, Jewell EL. Impact of Obesity on Sentinel Lymph Node Mapping in Patients with Newly Diagnosed Uterine Cancer Undergoing Robotic Surgery. Ann Surg Oncol. 2016;23:2522-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 137. | Markuszewski M, Buszewska-Forajta M, Artymowicz M, Połom W, Roslan M, Markuszewski M. Binding indocyanine green to human serum albumin potentially enhances the detection of sentinel lymph nodes. An initial step for facilitating the detection of first-station nodes in penile and other urological cancers. Arch Med Sci. 2022;18:719-725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 138. | van den Bos J, Wieringa FP, Bouvy ND, Stassen LPS. Optimizing the image of fluorescence cholangiography using ICG: a systematic review and ex vivo experiments. Surg Endosc. 2018;32:4820-4832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 139. | Woo Y, Chaurasiya S, O'Leary M, Han E, Fong Y. Fluorescent imaging for cancer therapy and cancer gene therapy. Mol Ther Oncolytics. 2021;23:231-238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 140. | Linders DGJ, Bijlstra OD, Fallert LC, Hilling DE, Walker E, Straight B, March TL, Valentijn ARPM, Pool M, Burggraaf J, Basilion JP, Vahrmeijer AL, Kuppen PJK. Cysteine Cathepsins in Breast Cancer: Promising Targets for Fluorescence-Guided Surgery. Mol Imaging Biol. 2023;25:58-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 141. | Turner MA, Lwin TM, Amirfakhri S, Nishino H, Hoffman RM, Yazaki PJ, Bouvet M. The Use of Fluorescent Anti-CEA Antibodies to Label, Resect and Treat Cancers: A Review. Biomolecules. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |